Association between Obesity and Short-Term Patient-Reported Outcomes following Total Knee Arthroplasty: A Retrospective Cohort Study in Japan
Abstract
1. Introduction
2. Materials and Methods
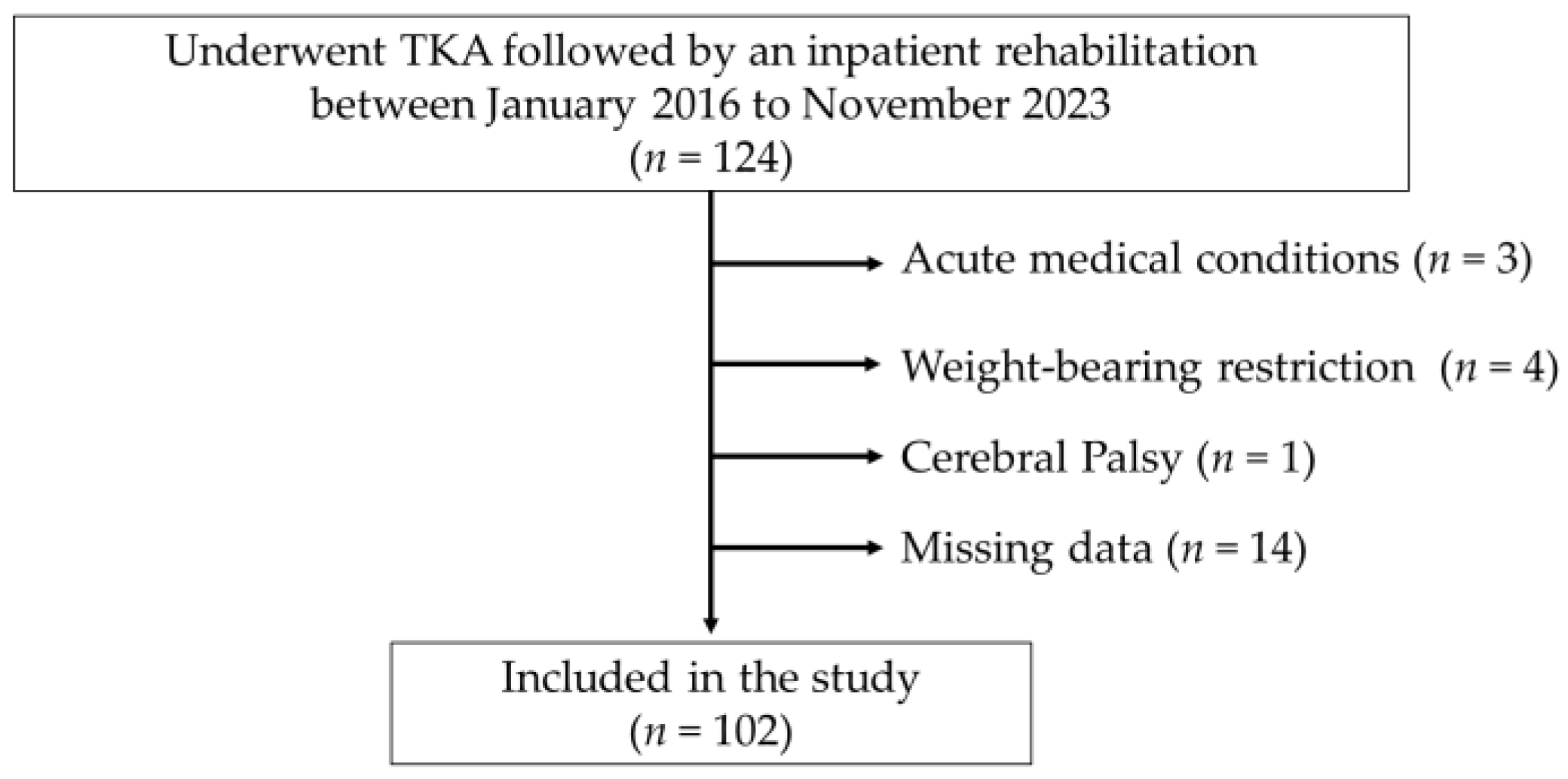
2.1. Participants and Setting
2.2. Surgery and Postoperative Rehabilitation
2.3. Study Design and Data Collection
2.4. Outcome Measures
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Participants
3.2. Surgery and Rehabilitation
3.3. WOMAC Pain and Function Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Neogi, T. The Epidemiology and Impact of Pain in Osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1145–1153. [Google Scholar] [CrossRef]
- Allen, K.D.; Thoma, L.M.; Golightly, Y.M. Epidemiology of Osteoarthritis. Osteoarthr. Cartil. 2022, 30, 184–195. [Google Scholar] [CrossRef]
- Felson, D.T.; Naimark, A.; Anderson, J.; Kazis, L.; Castelli, W.; Meenan, R.F. The Prevalence of Knee Osteoarthritis in the Elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987, 30, 914–918. [Google Scholar] [CrossRef]
- Hong, J.W.; Noh, J.H.; Kim, D.J. The Prevalence of and Demographic Factors Associated with Radiographic Knee Osteoarthritis in Korean Adults Aged ≥ 50 Years: The 2010-2013 Korea National Health and Nutrition Examination Survey. PLoS ONE 2020, 15, e0230613. [Google Scholar] [CrossRef]
- Li, D.; Li, S.; Chen, Q.; Xie, X. The Prevalence of Symptomatic Knee Osteoarthritis in Relation to Age, Sex, Area, Region, and Body Mass Index in China: A Systematic Review and Meta-analysis. Front. Med. 2020, 7, 304. [Google Scholar] [CrossRef]
- Driban, J.B.; Bannuru, R.R.; Eaton, C.B.; Spector, T.D.; Hart, D.J.; McAlindon, T.E.; Lu, B.; Lo, G.H.; Arden, N.K. The Incidence and Characteristics of Accelerated Knee Osteoarthritis Among Women: The Chingford Cohort. BMC Musculoskelet. Disord. 2020, 21, 60. [Google Scholar] [CrossRef]
- Losina, E.; Weinstein, A.M.; Reichmann, W.M.; Burbine, S.A.; Solomon, D.H.; Daigle, M.E.; Rome, B.N.; Chen, S.P.; Hunter, D.J.; Suter, L.G.; et al. Lifetime Risk and Age at Diagnosis of Symptomatic Knee Osteoarthritis in the US. Arthritis Care Res. 2013, 65, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N.; Muraki, S.; Nakamura, K.; Tanaka, S. Epidemiology of the Locomotive Syndrome: The Research on Osteoarthritis/Osteoporosis Against Disability Study 2005–2015. Mod. Rheumatol. 2017, 27, 1–7. [Google Scholar] [CrossRef]
- Matsuoka, H.; Nanmo, H.; Nojiri, S.; Nagao, M.; Nishizaki, Y. Projected Numbers of Knee and Hip Arthroplasties up to the Year 2030 in Japan. J. Orthop. Sci. 2023, 28, 161–166. [Google Scholar] [CrossRef]
- Ikeda, N.; Nakaya, T.; Bennett, J.; Ezzati, M.; Nishi, N. Trends and Disparities in Adult Body Mass Index Across the 47 Prefectures of Japan, 1975–2018: A Bayesian Spatiotemporal Analysis of National Household Surveys. Front. Public Health 2022, 10, 830578. [Google Scholar] [CrossRef]
- Hunter, D.J.; Schofield, D.; Callander, E. The Individual and Socioeconomic Impact of Osteoarthritis. Nat. Rev. Rheumatol. 2014, 10, 437–441. [Google Scholar] [CrossRef]
- Giorgino, R.; Albano, D.; Fusco, S.; Peretti, G.M.; Mangiavini, L.; Messina, C. Knee Osteoarthritis: Epidemiology, Pathogenesis, and Mesenchymal Stem Cells: What Else Is New? An Update. Int. J. Mol. Sci. 2023, 24, 6405. [Google Scholar] [CrossRef]
- Skou, S.T.; Roos, E.M.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Simonsen, O.; Rasmussen, S.A. Randomized, Controlled Trial of Total Knee Replacement. N. Engl. J. Med. 2015, 373, 1597–1606. [Google Scholar] [CrossRef]
- Feng, J.E.; Novikov, D.; Anoushiravani, A.A.; Schwarzkopf, R. Total Knee Arthroplasty: Improving Outcomes with a Multidisciplinary Approach. J. Multidiscip. Healthc. 2018, 11, 63–73. [Google Scholar] [CrossRef]
- Mizner, R.L.; Petterson, S.C.; Snyder-Mackler, L. Quadriceps Strength and the Time Course of Functional Recovery After Total Knee Arthroplasty. J. Orthop. Sports Phys. Ther. 2005, 35, 424–436. [Google Scholar] [CrossRef]
- Pua, Y.H.; Seah, F.J.; Seet, F.J.; Tan, J.W.; Liaw, J.S.; Chong, H.C. Sex Differences and Impact of Body Mass Index on the Time Course of Knee Range of Motion, Knee Strength, and Gait Speed After Total Knee Arthroplasty. Arthritis Care Res. 2015, 67, 1397–1405. [Google Scholar] [CrossRef]
- Pua, Y.H.; Seah, F.J.; Clark, R.A.; Lian-Li Poon, C.; Tan, J.W.; Chong, H.C. Factors Associated with Gait Speed Recovery after Total Knee Arthroplasty: A Longitudinal Study. Semin. Arthritis Rheum. 2017, 46, 544–551. [Google Scholar] [CrossRef]
- Papakostidou, I.; Dailiana, Z.H.; Papapolychroniou, T.; Liaropoulos, L.; Zintzaras, E.; Karachalios, T.S.; Malizos, K.N. Factors Affecting the Quality of Life After Total Knee Arthroplasties: A Prospective Study. BMC Musculoskelet. Disord. 2012, 13, 116. [Google Scholar] [CrossRef]
- Collins, J.E.; Donnell-Fink, L.A.; Yang, H.Y.; Usiskin, I.M.; Lape, E.C.; Wright, J.; Katz, J.N.; Losina, E. Effect of Obesity on Pain and Functional Recovery Following Total Knee Arthroplasty. J. Bone Joint Surg. Am. 2017, 99, 1812–1818. [Google Scholar] [CrossRef]
- Baghbani-Naghadehi, F.; Armijo-Olivo, S.; Prado, C.M.; Gramlich, L.; Woodhouse, L.J. Does Obesity Affect Patient-Reported Outcomes Following Total Knee Arthroplasty? BMC Musculoskelet. Disord. 2022, 23, 55. [Google Scholar] [CrossRef]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D. Patient Satisfaction After Total Knee Arthroplasty: Who Is Satisfied and Who Is Not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Luna, I.E.; Kehlet, H.; Peterson, B.; Wede, H.R.; Hoevsgaard, S.J.; Aasvang, E.K. Early Patient-Reported Outcomes Versus Objective Function After Total Hip and Knee Arthroplasty: A Prospective Cohort Study. Bone Joint J. 2017, 99-B, 1167–1175. [Google Scholar] [CrossRef]
- Van Egmond, J.C.; Hesseling, B.; Verburg, H.; Mathijssen, N.M.C. Short-Term Functional Outcome After Fast-Track Primary Total Knee Arthroplasty: Analysis of 623 Patients. Acta Orthop. 2021, 92, 602–607. [Google Scholar] [CrossRef]
- Boyce, L.; Prasad, A.; Barrett, M.; Dawson-Bowling, S.; Millington, S.; Hanna, S.A.; Achan, P. The outcomes of total knee arthroplasty in morbidly obese patients: A systematic review of the literature. Arch. Orthop. Trauma Surg. 2019, 139, 553–560. [Google Scholar] [CrossRef]
- Bonasia, D.E.; Palazzolo, A.; Cottino, U.; Saccia, F.; Mazzola, C.; Rosso, F.; Rossi, R. Modifiable and Nonmodifiable Predictive Factors Associated with the Outcomes of Total Knee Arthroplasty. Joints 2019, 7, 13–18. [Google Scholar] [CrossRef][Green Version]
- Pozzobon, D.; Ferreira, P.H.; Blyth, F.M.; Machado, G.C.; Ferreira, M.L. Can obesity and physical activity predict outcomes of elective knee or hip surgery due to osteoarthritis? A meta-analysis of cohort studies. BMJ Open 2018, 8, e017689. [Google Scholar] [CrossRef]
- Baker, P.; Petheram, T.; Jameson, S.; Reed, M.; Gregg, P.; Deehan, D. The association between body mass index and the outcomes of total knee arthroplasty. J. Bone Joint Surg. Am. 2012, 94, 1501–1508. [Google Scholar] [CrossRef]
- Giesinger, J.M.; Loth, F.L.; MacDonald, D.J.; Giesinger, K.; Patton, J.T.; Simpson, A.H.R.W.; Howie, C.R.; Hamilton, D.F. Patient-Reported Outcome Metrics Following Total Knee Arthroplasty Are Influenced Differently by Patients' Body Mass Index. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3257–3264. [Google Scholar] [CrossRef]
- Başdelioğlu, K. Effects of Body Mass Index on Outcomes of Total Knee Arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 595–600. [Google Scholar] [CrossRef]
- Baum, G.; Jacobs, H.; Lazovic, D.; Maus, U.; Hoffmann, F.; Seeber, G.H. The Influence of Obesity on Functional Outcomes and Patient Satisfaction 8 Weeks After Total Knee Arthroplasty: Results of the Prospective FInGK Study. BMC Musculoskelet. Disord. 2022, 23, 949. [Google Scholar] [CrossRef]
- Giesinger, K.; Giesinger, J.M.; Hamilton, D.F.; Rechsteiner, J.; Ladurner, A. Higher Body Mass Index Is Associated with Larger Postoperative Improvement in Patient-Reported Outcomes Following Total Knee Arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 635. [Google Scholar] [CrossRef]
- Maniar, R.N.; Maniar, P.R.; Singhi, T.; Gangaraju, B.K. WHO Class of Obesity Influences Functional Recovery Post-TKA. Clin. Orthop. Surg. 2018, 10, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Chen, J.Y.; Lo, N.N.; Chia, S.L.; Tay, D.K.J.; Pang, H.N.; Hao, Y.; Yeo, S.J. The Influence of Obesity on Functional Outcome and Quality of Life After Total Knee Arthroplasty: A Ten-Year Follow-Up Study. Bone Joint J. 2018, 100-B, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Lo, N.N.; Chong, H.C.; Bin Abd Razak, H.R.; Pang, H.N.; Tay, D.K.; Chia, S.L.; Yeo, S.J. The Influence of Body Mass Index on Functional Outcome and Quality of Life After Total Knee Arthroplasty. Bone Joint J. 2016, 98-B, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Yoshiike, N.; Matsumura, Y.; Zaman, M.M.; Yamaguchi, M. Descriptive Epidemiology of Body Mass Index in Japanese Adults in a Representative Sample from the National Nutrition Survey 1990–1994. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 684–687. [Google Scholar] [CrossRef] [PubMed]
- Yuji, M. Examination Committee of Criteria for ‘Obesity Disease’ in Japan; Japan Society for the Study of Obesity. New Criteria for ‘Obesity Disease’ in Japan. Circ. J. 2002, 66, 987–992. [Google Scholar] [CrossRef]
- Yoshiike, N.; Miyoshi, M. Epidemiological Aspects of Overweight and Obesity in Japan--International Comparisons. Nihon Rinsho Jpn. J. Clin. Med. 2013, 71, 207–216. [Google Scholar]
- den Hertog, A.; Gliesche, K.; Timm, J.; Muhlbauer, B.; Zebrowski, S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: A randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch. Orthop. Trauma Surg. 2012, 132, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Burn, E.; Edwards, C.J.; Murray, D.W.; Silman, A.; Cooper, C.; Arden, N.K.; Pinedo-Villanueva, R.; Prieto-Alhambra, D. Trends and determinants of length of stay and hospital reimbursement following knee and hip replacement: Evidence from linked primary care and NHS hospital records from 1997 to 2014. BMJ Open 2018, 8, e019146. [Google Scholar] [CrossRef]
- Kuwakado, S.; Kawaguchi, K.; Sakugawa, A.; Takahashi, M.; Oda, T.; Shimamoto, N.; Motomura, G.; Hamai, S.; Nakashima, Y. Factors Affecting the Length of Convalescent Hospital Stay Following Total Hip and Knee Arthroplasty. Prog. Rehabil. Med. 2021, 6, 20210033. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organization Technical Report Series; World Health Organization: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. [Google Scholar]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation Study of WOMAC: A Health Status Instrument for Measuring Clinically Important Patient Relevant Outcomes to Antirheumatic Drug Therapy in Patients with Osteoarthritis of the Hip or Knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Hashimoto, H.; Hanyu, T.; Sledge, C.B.; Lingard, E.A. Validation of a Japanese Patient-Derived Outcome Scale for Assessing Total Knee Arthroplasty: Comparison with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). J. Orthop. Sci. 2003, 8, 288–293. [Google Scholar] [CrossRef]
- Copsey, B.; Thompson, J.Y.; Vadher, K.; Ali, U.; Dutton, S.J.; Fitzpatrick, R.; Lamb, S.E.; Cook, J.A. Problems Persist in Reporting of Methods and Results for the WOMAC Measure in Hip and Knee Osteoarthritis Trials. Qual. Life Res. 2019, 28, 335–343. [Google Scholar] [CrossRef]
- Singh, J.; Sloan, J.A.; Johanson, N.A. Challenges with Health-Related Quality of Life Assessment in Arthroplasty Patients: Problems and Solutions. J. Am. Acad. Orthop. Surg. 2010, 18, 72–82. [Google Scholar] [CrossRef]
- Angst, F.; Benz, T.; Lehmann, S.; Aeschlimann, A.; Angst, J. Multidimensional Minimal Clinically Important Differences in Knee Osteoarthritis After Comprehensive Rehabilitation: A Prospective Evaluation from the Bad Zurzach Osteoarthritis Study. RMD Open 2018, 4, e000685. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Bardgett, M.; Weir, D.; Holland, J.; Gerrand, C.; Deehan, D.J. What Is the Minimum Clinically Important Difference for the WOMAC Index After TKA? Clin. Orthop. Relat. Res. 2018, 476, 2005–2014. [Google Scholar] [CrossRef] [PubMed]
- Green, P.; MacLeod, C.J.; Nakagawa, S. SIMR: An R package for power analysis of generalized linear mixed models by simulation. Methods Ecol. Evol. 2016, 7, 493–498. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Science; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1998. [Google Scholar]
- Hofstede, S.N.; Gademan, M.G.J.; Stijnen, T.; Nelissen, R.G.H.H.; Marang-van de Mheen, P.J.; ARGON-OPTIMA study group. The Influence of Preoperative Determinants on Quality of Life, Functioning and Pain After Total Knee and Hip Replacement: A Pooled Analysis of Dutch Cohorts. BMC Musculoskelet. Disord. 2018, 19, 68. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.K.; Vincent, K.R. Obesity and Inpatient Rehabilitation Outcomes Following Knee Arthroplasty: A Multicenter Study. Obesity 2008, 16, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Conner-Spady, B.; Estey, A.; Arnett, G.; Ness, K.; McGurran, J.; Bear, R.; Noseworthy, T. Prioritization of patients on waiting lists for hip and knee replacement: Validation of a priority criteria tool. Int. J. Technol. Assess. Health Care 2004, 20, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 102) | Normal Weight (n = 30) | Overweight (n = 49) | Obese (n = 23) | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age | 75.00 | (71.75, 78.00) | 77.00 | (72.00, 79.25) | 75.00 | (73.00, 77.50) | 73.00 | (68.00, 77.00) | 0.068 b |
| Sex, number of women | 87 | 85.29% | 24 | 80% | 41 | 83.67% | 22 | 95.65% | 0.254 c |
| BMI (kg/m2) | 27.37 | ±4.11 | 23.39 | (22.05, 24.26) | 27.16 | (26.09, 28.75) | 31.63 | (30.83, 36.05) | <0.001 b * |
| Etiology, frequency of OA/RA | 94/8 | 92.16%/7.84% | 25/5 | 83.33%/16.57% | 46/3 | 93.88%/6.12% | 23/0 | 100% | 0.068 c |
| Number of comorbidities | 2.00 | (1.00, 3.00) | 2.00 | (1.00, 3.00) | 2.00 | (1.50, 3.00) | 2.00 | (1.00, 3.00) | 0.653 b |
| CCI | 1.00 | (0.00, 1.00) | 1.00 | (0.00, 1.00) | 1.00 | (0.00, 1.00) | 0.00 | (0.00, 1.00) | 0.196 b |
| Preoperative walking status | |||||||||
| Self-reliant | 66 | 64.71% | 20 | 66.67% | 32 | 65.31% | 14 | 60.87% | 0.902 c |
| Reliance on assistive devices | 36 | 35.29% | 10 | 33.33% | 17 | 34.69% | 9 | 39.13% | |
| FIM motor score | 85.00 | (79.75, 88.00) | 85.00 | (81.50, 88.00) | 85.00 | (79.00, 89.00) | 83.00 | (79.00, 87.00) | 0.510 b |
| FIM cognition score | 35.00 | (35.00, 35.00) | 35.00 | (33.75, 35.00) | 35.00 | (34.00, 35.00) | 35.00 | (35.00, 35.00) | 0.073 b |
| WOMAC pain score † | 40.10 | ±19.47 | 42.50 | ±20.67 | 39.18 | ±18.10 | 38.91 | ±21.26 | 0.727 a |
| WOMAC functional score † | 26.47 | (16.18, 38.60) | 30.88 | (19.85, 41.18) | 19.12 | (16.18, 37.50) | 27.94 | (17.65, 50.00) | 0.277 b |
| Duration of surgery (minutes) | 99.50 | (90.00, 101.25) | 95.00 | (85.50, 106.00) | 98.00 | (90.00, 109.50) | 106.00 | (100.00, 127.00) | 0.007 b |
| Duration of daily rehabilitation (hours) | 1.66 | (1.52, 1.84) | 1.66 | ±0.21 | 1.65 | ±0.24 | 1.66 | ±0.18 | 1.000 b |
| Normal Weight | Overweight | Obese | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WOMAC | n | Estimated Mean | (95% CI) | n | Estimated Mean | (95% CI) | n | Estimated Mean | (95% CI) | |
| Pain † | Pre | 30 | 40.85 | (33.16, 48.53) | 49 | 36.83 | (29.59, 44.08) | 23 | 35.22 | (25.53, 44.91) |
| 2w | 25 | 28.15 | (19.90, 36.40) | 46 | 26.67 | (19.35, 33.99) | 21 | 24.30 | (14.38, 34.21) | |
| 4w | 24 | 21.64 | (13.28, 30.00) | 45 | 17.92 | (10.55, 25.29) | 21 | 14.54 | (4.62, 24.45) | |
| Time effect (with respect to preoperative score): 2w, p = 0.001 *; 4w, p < 0.001 *. | ||||||||||
| Group effect (relating to normal weight group): Overweight, p = 0.344; Obese, p = 0.280. | ||||||||||
| Group-by-time interaction effect (relating to normal weight group by preoperative score): | ||||||||||
| Overweight × 2w, p = 0.603; Obese × 2w, p = 0.953. | ||||||||||
| Overweight × 4w, p = 0.760; Obese × 4w, p = 0.800. | ||||||||||
| Normal weight | Overweight | Obese | ||||||||
| WOMAC | n | Estimated mean | (95% CI) | n | Estimated mean | (95% CI) | n | Estimated mean | (95% CI) | |
| Function † | Pre | 30 | 28.34 | (22.17, 34.51) | 49 | 24.13 | (18.37, 29.90) | 23 | 30.41 | (22.67, 38.15) |
| 2w | 25 | 24.78 | (18.12, 31.45) | 46 | 24.08 | (18.25, 29.91) | 21 | 25.35 | (17.42, 33.28) | |
| 4w | 24 | 13.34 | (6.59, 20.10) | 45 | 11.28 | (5.41, 17.16) | 21 | 14.29 | (6.35, 22.22) | |
| Time effect (with respect to preoperative score): 2w, p = 0.288; 4w, p < 0.001 *. | ||||||||||
| Group effect (relating to normal weight group): Overweight, p = 0.221; Obese, p = 0.792. | ||||||||||
| Group-by-time interaction effect (relating to normal weight group by preoperative score): | ||||||||||
| Overweight × 2w, p = 0.402; Obese × 2w, p = 0.611. | ||||||||||
| Overweight × 4w, p = 0.763; Obese × 4w, p = 0.823. | ||||||||||
| Total | Normal Weight | Overweight | Obese | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔWOMAC | n | Mean or Median | ±SD or (IQR) | n | Mean or Median | ±SD or (IQR) | n | Mean or Median | ±SD or (IQR) | n | Mean or Median | ±SD or (IQR) | p | η2 or r | |
| Pain | 2w | 92 | −10.65 | ±22.75 | 25 | −12.40 | ±24.80 | 46 | −9.67 | ±22.59 | 21 | −10.71 | ±21.52 | 0.892 a | 0.003 |
| 4w | 90 | −18.72 | ±21.22 | 24 | −17.92 | ±23.63 | 45 | −18.33 | ±21.32 | 21 | −20.48 | ±18.90 | 0.910 a | 0.002 | |
| Function | 2w | 92 | −1.81 | ±19.47 | 25 | −2.71 | ±23.14 | 46 | 0.13 | ±18.07 | 21 | −4.97 | ±18.10 | 0.593 a | 0.012 |
| 4w | 90 | −11.76 | (−23.90, −1.47) | 24 | −16.18 | (−26.47, 2.21) | 45 | −10.29 | (−21.32, −2.94) | 21 | −11.76 | (−28.68, −2.94) | 0.769 b | 0.056 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishimoto, R.; Mutsuzaki, H.; Shimizu, Y.; Yoshikawa, K.; Koseki, K.; Takeuchi, R.; Matsumoto, S.; Hada, Y. Association between Obesity and Short-Term Patient-Reported Outcomes following Total Knee Arthroplasty: A Retrospective Cohort Study in Japan. J. Clin. Med. 2024, 13, 1291. https://doi.org/10.3390/jcm13051291
Ishimoto R, Mutsuzaki H, Shimizu Y, Yoshikawa K, Koseki K, Takeuchi R, Matsumoto S, Hada Y. Association between Obesity and Short-Term Patient-Reported Outcomes following Total Knee Arthroplasty: A Retrospective Cohort Study in Japan. Journal of Clinical Medicine. 2024; 13(5):1291. https://doi.org/10.3390/jcm13051291
Chicago/Turabian StyleIshimoto, Ryu, Hirotaka Mutsuzaki, Yukiyo Shimizu, Kenichi Yoshikawa, Kazunori Koseki, Ryoko Takeuchi, Shuji Matsumoto, and Yasushi Hada. 2024. "Association between Obesity and Short-Term Patient-Reported Outcomes following Total Knee Arthroplasty: A Retrospective Cohort Study in Japan" Journal of Clinical Medicine 13, no. 5: 1291. https://doi.org/10.3390/jcm13051291
APA StyleIshimoto, R., Mutsuzaki, H., Shimizu, Y., Yoshikawa, K., Koseki, K., Takeuchi, R., Matsumoto, S., & Hada, Y. (2024). Association between Obesity and Short-Term Patient-Reported Outcomes following Total Knee Arthroplasty: A Retrospective Cohort Study in Japan. Journal of Clinical Medicine, 13(5), 1291. https://doi.org/10.3390/jcm13051291





