The Long-Term Efficacy of Computed Tomography-Navigated Total Hip Arthroplasty: An 18-Year Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statements
2.2. Study Design and Population
2.3. Data Collection
2.4. Follow-Up
2.5. Data Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Sugano, N.; Takao, M.; Sakai, T.; Nishii, T.; Miki, H. Does CT-based navigation improve the long-term survival in ceramic-on-ceramic THA. Clin. Orthop. Relat. Res. 2012, 470, 3054–3059. [Google Scholar] [CrossRef]
- Shon, W.Y.; Baldini, T.; Peterson, M.G.; Wright, T.M.; Salvati, E.A. Impingement in total hip arthroplasty a study of retrieved acetabular components. J. Arthroplast. 2005, 20, 427–435. [Google Scholar] [CrossRef]
- Wroblewski, B.M.; Siney, P.D.; Fleming, P.A. Effect of reduced diameter neck stem on incidence of radiographic cup loosening and revisions in Charnley low-frictional torque arthroplasty. J. Arthroplast. 2009, 24, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Furmanski, J.; Anderson, M.; Bal, S.; Greenwald, A.S.; Halley, D.; Penenberg, B.; Ries, M.; Pruitt, L. Clinical fracture of cross-linked UHMWPE acetabular liners. Biomaterials 2009, 30, 5572–5582. [Google Scholar] [CrossRef] [PubMed]
- DiGioia, A.M.; Jaramaz, B.; Blackwell, M.; Simon, D.A.; Morgan, F.; Moody, J.E.; Nikou, C.; Colgan, B.D.; Aston, C.A.; Labarca, R.S.; et al. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin. Orthop. Relat. Res. 1998, 355, 8–22. [Google Scholar] [CrossRef] [PubMed]
- Sugano, N.; Sasama, T.; Sato, Y.; Nakajima, Y.; Nishii, T.; Yonenobu, K.; Tamura, S.; Ochi, T. Accuracy evaluation of surface-based registration methods in a computer navigation system for hip surgery performed through a posterolateral approach. Comput. Aided Surg. 2001, 6, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Nakahara, I.; Takao, M.; Sakai, T.; Nishii, T.; Yoshikawa, H.; Sugano, N. Gender differences in 3D morphology and bony impingement of human hips. J. Orthop. Res. 2011, 29, 333–339. [Google Scholar] [CrossRef]
- Imai, N.; Takubo, R.; Suzuki, H.; Shimada, H.; Miyasaka, D.; Tsuchiya, K.; Endo, N. Accuracy of acetabular cup placement using CT-based navigation in total hip arthroplasty: Comparison between obese and non-obese patients. J. Orthop. Sci. 2019, 24, 482–487. [Google Scholar] [CrossRef]
- Nozaki, A.; Imai, N.; Funayama, K.; Horigome, Y.; Suzuki, H.; Minato, I.; Kobayashi, K.; Kawashima, H. Accuracy of ZedView, the software for three-dimensional measurement and preoperative planning: A basic study. Medicina 2023, 59, 1030. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef] [PubMed]
- DeLee, J.G.; Charnley, J. Radiological demarcation of cemented sockets in total hip replacement. Clin. Orthop. Relat. Res. 1976, 121, 20–32. [Google Scholar] [CrossRef]
- Nogler, M.; Kessler, O.; Prassl, A.; Donnelly, B.; Streicher, R.; Sledge, J.B.; Krismer, M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin. Orthop. Relat. Res. 2004, 426, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Miki, H.; Yamanashi, W.; Nishii, T.; Sato, Y.; Yoshikawa, H.; Sugano, N. Anatomic hip range of motion after implantation during total hip arthroplasty as measured by a navigation system. J. Arthroplast. 2007, 22, 946–952. [Google Scholar] [CrossRef] [PubMed]
- González Della Valle, A.; Comba, F.; Zoppi, A.; Salvati, E.A. Favourable mid-term results of the VerSys CT polished cemented femoral stem for total hip arthroplasty. Int. Orthop. 2006, 30, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Kawaji, H.; Uematsu, T.; Hoshikawa, N.; Watanabe, H.; Takai, S. Mid-term clinical results of VerSys Hip System (Zimmer) uncemented total hip replacement arthroplasty. J. Nippon. Med. Sch. 2016, 83, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Surdam, J.W.; Archibeck, M.J.; Schultz, S.C.; Junick, D.W.; White, R.E. A second-generation cementless total hip arthroplasty mean 9-year results. J. Arthroplast. 2007, 22, 204–209. [Google Scholar] [CrossRef]
- Phillips, C.B.; Barrett, J.A.; Losina, E.; Mahomed, N.N.; Lingard, E.A.; Guadagnoli, E.; Baron, J.A.; Harris, W.H.; Poss, R.; Katz, J.N. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J. Bone Joint Surg. Am. 2003, 85, 20–26. [Google Scholar] [CrossRef]
- Bistolfi, A.; Crova, M.; Rosso, F.; Titolo, P.; Ventura, S.; Massazza, G. Dislocation rate after hip arthroplasty within the first postoperative year: 36 mm versus 28 mm femoral heads. Hip Int. 2011, 21, 559–564. [Google Scholar] [CrossRef]
- Sierra, R.J.; Raposo, J.M.; Trousdale, R.T.; Cabanela, M.E. Dislocation of primary THA done through a posterolateral approach in the elderly. Clin. Orthop. Relat. Res. 2005, 441, 262–267. [Google Scholar] [CrossRef]
- Higgins, B.T.; Barlow, D.R.; Heagerty, N.E.; Lin, T.J. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J. Arthroplast. 2015, 30, 419–434. [Google Scholar] [CrossRef]
- Widmer, K.H.; Zurfluh, B. Compliant positioning of total hip components for optimal range of motion. J. Orthop. Res. 2004, 22, 815–821. [Google Scholar] [CrossRef]
- Widmer, K.H. The impingement-free, prosthesis-specific, and anatomy-adjusted combined target zone for component positioning in THA depends on design and implantation parameters of both components. Clin. Orthop. Relat. Res. 2020, 478, 1904–1918. [Google Scholar] [CrossRef] [PubMed]
- Loppini, M.; Pisano, A.; Ruggeri, R.; Della Rocca, A.; Grappiolo, G. Pelvic tilt and functional acetabular position after total hip arthroplasty: An EOS 2D/3D radiographic study. Hip Int. 2023, 33, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Berry, D.J.; von Knoch, M.; Schleck, C.D.; Harmsen, W.S. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J. Bone Joint Surg. Am. 2005, 87, 2456–2463. [Google Scholar] [CrossRef]
- Kwon, M.S.; Kuskowski, M.; Mulhall, K.J.; Macaulay, W.; Brown, T.E.; Saleh, K.J. Does surgical approach affect total hip arthroplasty dislocation rates. Clin. Orthop. Relat. Res. 2006, 447, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Howie, D.W.; Holubowycz, O.T.; Middleton, R.; Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: A randomized controlled trial. J. Bone Joint Surg. Am. 2012, 94, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Lübbeke, A.; Suvà, D.; Perneger, T.; Hoffmeyer, P. Influence of preoperative patient education on the risk of dislocation after primary total hip arthroplasty. Arthritis Rheum. 2009, 61, 552–558. [Google Scholar] [CrossRef]




| Age (Years) | 57.3 ± 9.6 |
|---|---|
| Sex (men/women) | 14/131 |
| Right/left hip | 69/76 |
| Follow-up period (years) | 18.4 ± 1.7 |
| Body mass index (kg/m2) | 23.4 ± 3.1 |
| Surgical approach | Direct lateral, 109 Anterolateral supine, 11 Orthopädische Chirurgie of München approach, 25 |
| Cause | Hip osteoarthritis, 117 Idiopathic osteonecrosis of the femoral head, 21 Rheumatoid arthritis, 6 Pigmented villonodular synovitis, |
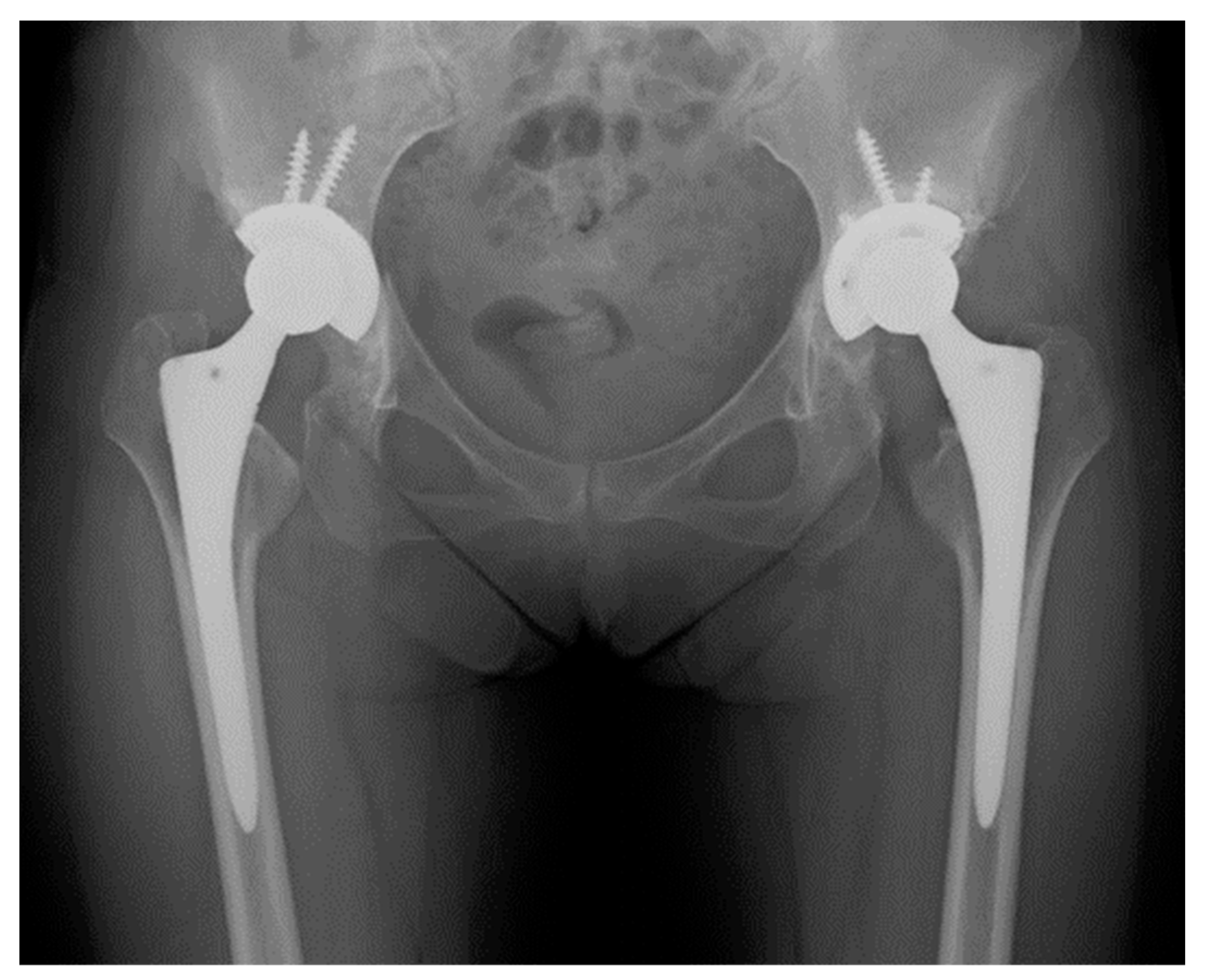
| Acetabular component | Trilogy®, 145 |
| Femoral component | VerSys Midcoat collarless stem®, 89 Fiber metal taper®, 48 Cemented®, 8 |
| Head size (mm) | 22, 7 26, 103 28, 35 |
| Intra-Observer Reliability | Inter-Observer Reliability | |||||||
|---|---|---|---|---|---|---|---|---|
| MAD | ICC | 95% CI | p-Value | MAD | ICC | 95% CI | p-Value | |
| Radiographic anteversion (°) | 1.4 ± 0.8 | 0.971 | 0.962–0.978 | <0.001 | 1.9 ± 1.4 | 0.932 | 0.912–0.945 | <0.001 |
| Radiographic inclination (°) | 1.3 ± 0.9 | 0.974 | 0.963–0.980 | <0.001 | 2.3 ± 1.8 | 0.941 | 0.922–0.956 | <0.001 |
| Stem anteversion (°) | 1.6 ± 1.6 | 0.956 | 0.934–0.978 | <0.001 | 2.2 ± 2.1 | 0.950 | 0.933–0.962 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imai, N.; Miyasaka, D.; Ibuchi, S.; Kimura, K.; Hirano, Y.; Horigome, Y.; Kawashima, H. The Long-Term Efficacy of Computed Tomography-Navigated Total Hip Arthroplasty: An 18-Year Follow-Up Study. J. Clin. Med. 2024, 13, 1374. https://doi.org/10.3390/jcm13051374
Imai N, Miyasaka D, Ibuchi S, Kimura K, Hirano Y, Horigome Y, Kawashima H. The Long-Term Efficacy of Computed Tomography-Navigated Total Hip Arthroplasty: An 18-Year Follow-Up Study. Journal of Clinical Medicine. 2024; 13(5):1374. https://doi.org/10.3390/jcm13051374
Chicago/Turabian StyleImai, Norio, Dai Miyasaka, Shinya Ibuchi, Keishi Kimura, Yuki Hirano, Yoji Horigome, and Hiroyuki Kawashima. 2024. "The Long-Term Efficacy of Computed Tomography-Navigated Total Hip Arthroplasty: An 18-Year Follow-Up Study" Journal of Clinical Medicine 13, no. 5: 1374. https://doi.org/10.3390/jcm13051374






