Buried Autologous Breast Reconstruction: Outcomes and Technical Considerations
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Pre-Operative
2.3. Intra-Operative
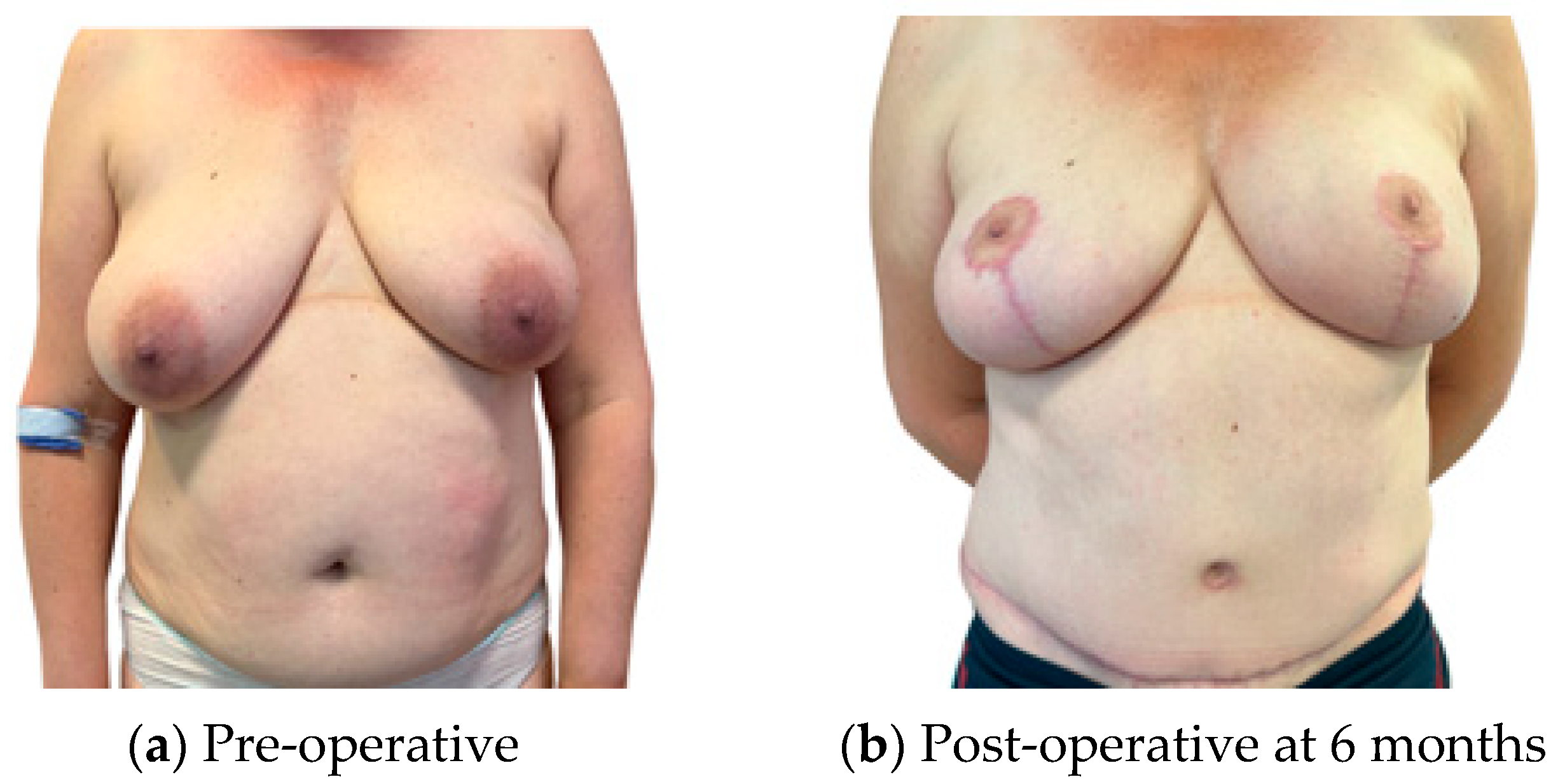
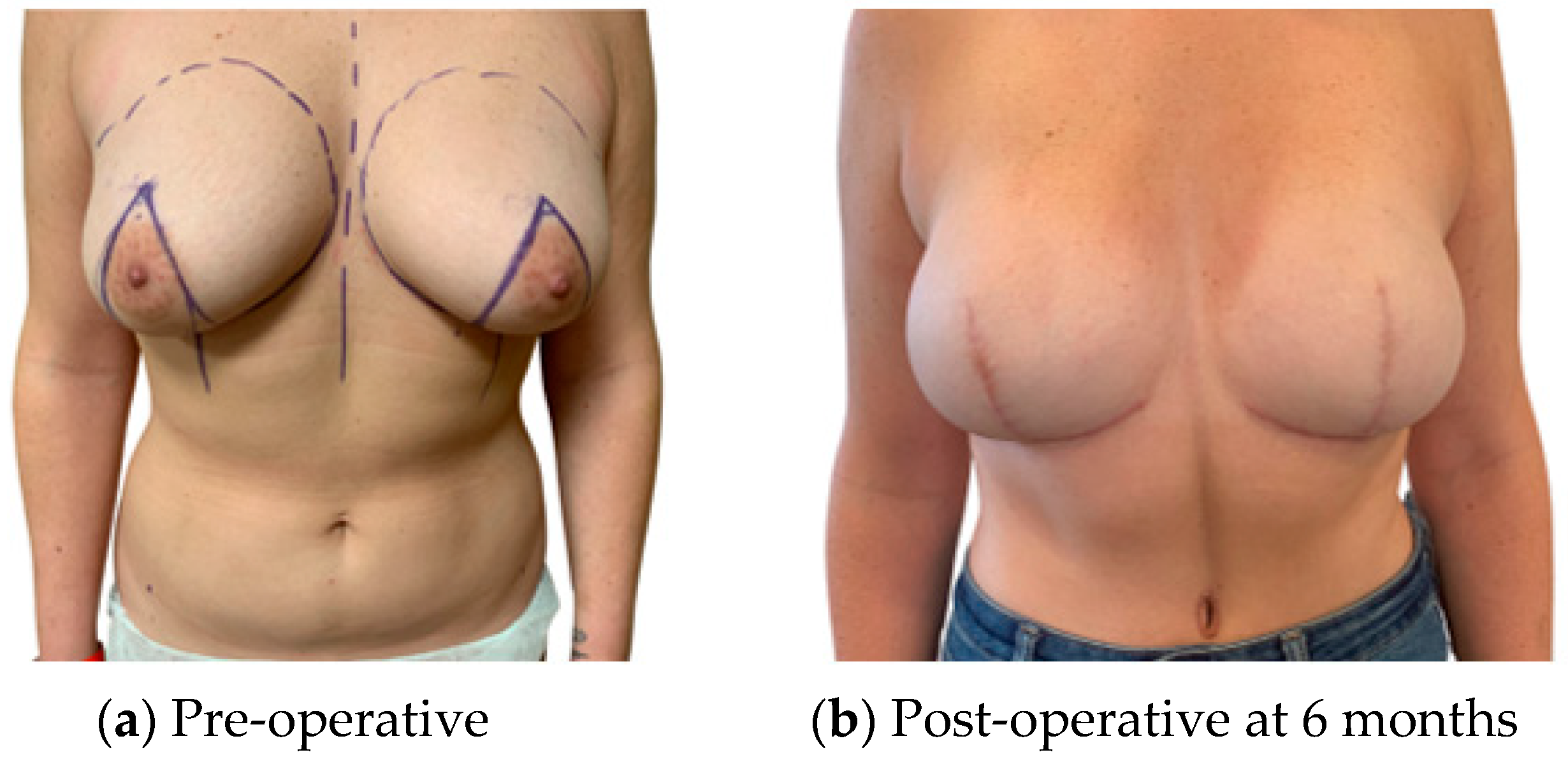
Skin Envelope
2.4. Post-Operative
2.5. Statistical Tests
3. Results
3.1. Demographics and Flap Details
3.2. Intra-Operative Results
3.3. Complications
3.4. Additional Procedures
4. Discussion
5. Limitations
Summary and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panchal, H.; Matros, E. Current Trends in Post-Mastectomy Breast Reconstruction. Plast. Reconstr. Surg. 2017, 140, 7S. [Google Scholar] [CrossRef] [PubMed]
- Headon, H.L.; Kasem, A.; Mokbel, K. The Oncological Safety of Nipple-Sparing Mastectomy: A Systematic Review of the Literature with a Pooled Analysis of 12,358 Procedures. Arch. Plast. Surg. 2016, 43, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Mota, B.S.; Riera, R.; Ricci, M.D.; Barrett, J.; de Castria, T.B.; Atallah, Á.N.; Bevilacqua, J.L.B. Nipple-and Areola-sparing Mastectomy for the Treatment of Breast Cancer. Cochrane Database Syst. Rev. 2016, 2016, CD008932. [Google Scholar] [CrossRef] [PubMed]
- Valero, M.G.; Muhsen, S.; Moo, T.-A.; Zabor, E.C.; Stempel, M.; Pusic, A.; Gemignani, M.L.; Morrow, M.; Sacchini, V.S. Increase in Utilization of Nipple-Sparing Mastectomy for Breast Cancer: Indications, Complications, and Oncologic Outcomes. Ann. Surg. Oncol. 2020, 27, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Frey, J.D.; Stranix, J.T.; Chiodo, M.V.; Alperovich, M.; Ahn, C.Y.; Allen, R.J.; Choi, M.; Karp, N.S.; Levine, J.P. Evolution in Monitoring of Free Flap Autologous Breast Reconstruction after Nipple-Sparing Mastectomy: Is There a Best Way? Plast. Reconstr. Surg. 2018, 141, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Rose, V.; Cooper, L.; Pafitanis, G.; Hogben, K.; Sharma, A.; Din, A.H. Single-Stage Buried Autologous Breast Reconstruction (BABR). J. Plast. Reconstr. Aesthetic Surg. 2022, 75, 2960–2969. [Google Scholar] [CrossRef] [PubMed]
- Halani, S.H.; Jones, K.; Liu, Y.; Teotia, S.S.; Haddock, N.T. Reconstructive Burnout after Mastectomy: Implications for Patient Selection. Plast. Reconstr. Surg. 2023, 151, 13e–19e. [Google Scholar] [CrossRef]
- Romanoff, A.; Zabor, E.C.; Stempel, M.; Sacchini, V.; Pusic, A.; Morrow, M. A Comparison of Patient-Reported Outcomes after Nipple-Sparing Mastectomy and Conventional Mastectomy with Reconstruction. Ann. Surg. Oncol. 2018, 25, 2909–2916. [Google Scholar] [CrossRef]
- Clarijs, M.E.; Peeters, N.J.M.C.V.; van Dongen, S.A.F.; Koppert, L.B.; Pusic, A.L.; Mureau, M.A.M.; Rijken, B.F.M. Quality of Life and Complications after Nipple-versus Skin-Sparing Mastectomy Followed by Immediate Breast Reconstruction: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2023, 152, 12e–24e. [Google Scholar] [CrossRef]
- Levine, S.M.; Snider, C.; Gerald, G.; Tanna, N.; Broer, P.N.; Stolier, A.; Sadeghi, A.; Allen Sr, R.J. Buried Flap Reconstruction after Nipple-Sparing Mastectomy: Advancing toward Single-Stage Breast Reconstruction. Plast. Reconstr. Surg. 2013, 132, 489e–497e. [Google Scholar] [CrossRef]
- Creasy, M.H.; Citron, M.I.; O’Connor, M.E.F.; Rose, M.V.; Din, M.A.H. Reply to ‘Early Experience with Synovis Flow Coupler and Major Pitfalls in Its Use in 18 Microsurgical Free Flaps’ Snapshot Review of Greater than 100 Free Flaps in 1 Year Using Venous Flow Couplers for Monitoring. J. Plast. Reconstr. Aesthetic Surg. 2023. [Google Scholar] [CrossRef]
- Zhang, T.; Dyalram-Silverberg, D.; Bui, T.; Caccamese, J.F., Jr.; Lubek, J.E. Analysis of an Implantable Venous Anastomotic Flow Coupler: Experience in Head and Neck Free Flap Reconstruction. Int. J. Oral Maxillofac. Surg. 2012, 41, 751–755. [Google Scholar] [CrossRef]
- Chadwick, S.L.; Khaw, R.; Duncan, J.; Wilson, S.W.; Highton, L.; O’Ceallaigh, S. The Use of Venous Anastomotic Flow Couplers to Monitor Buried Free DIEP Flap Reconstructions Following Nipple-Sparing Mastectomy. JPRAS Open 2020, 23, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Shtarbanov, P.; Kodama, H.; Nikkhah, D. Early Experience with Synovis Flow Coupler and Major Pitfalls in Its Use in 18 Microsurgical Free Flaps. J. Plast. Reconstr. Aesthetic Surg. 2023. [Google Scholar] [CrossRef] [PubMed]
- Sindali, K.; Harries, V.; Borges, A.; Simione, S.; Patel, S.; Vorster, T.; Lawrence, C.; Jones, M. Improved Patient Outcomes Using the Enhanced Recovery Pathway in Breast Microsurgical Reconstruction: A UK Experience. JPRAS Open 2019, 19, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Haddock, N.T.; Kayfan, S.; Pezeshk, R.A.; Teotia, S.S. Co-surgeons in Breast Reconstructive Microsurgery: What Do They Bring to the Table? Microsurgery 2018, 38, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Escandón, J.M.; Mascaro-Pankova, A.; DellaCroce, F.J.; Escandón, L.; Christiano, J.G.; Langstein, H.N.; Manrique, O.J. The Value of a Co-Surgeon in Microvascular Breast Reconstruction: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. Glob. Open 2024, 12, e5624. [Google Scholar] [CrossRef] [PubMed]
- MacNeill, F.; Irvine, T. Breast Surgery. GIRFT Programme National Speciality Report. 2021. Available online: https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/09/BreastSurgeryReport-Jul21p.pdf (accessed on 12 December 2023).
- Hazari, A.; Cole, R.; Fowler, C.; Schache, S.; Ho, M.; Nugent, M.; Kinsman, R.; Walton, P. First UK National Flap Registry Report. 2019. Available online: https://bahno.org.uk/_userfiles/pages/files/uknfr_first_report_4dec_2019.pdf (accessed on 12 December 2023).
- Heidekrueger, P.I.; Moellhoff, N.; Horch, R.E.; Lohmeyer, J.A.; Marx, M.; Heitmann, C.; Fansa, H.; Geenen, M.; Gabka, C.J.; Handstein, S. Overall Complication Rates of DIEP Flap Breast Reconstructions in Germany—A Multi-Center Analysis Based on the DGPRÄC Prospective National Online Registry for Microsurgical Breast Reconstructions. J. Clin. Med. 2021, 10, 1016. [Google Scholar] [CrossRef]
- Moller, L.; Berner, J.E.; Dheansa, B. The Reconstructive Journey: Description of the Breast Reconstruction Pathway in a High-Volume UK-Based Microsurgical Centre. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1930–1935. [Google Scholar] [CrossRef]
- NHS England. Delivery Plan for Tackling the COVID-19 Backlog of Elective Care. Available online: https://www.england.nhs.uk/coronavirus/publication/delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care/ (accessed on 12 December 2023).
- Shen, A.Y.; Lonie, S.; Lim, K.; Farthing, H.; Hunter-Smith, D.J.; Rozen, W.M. Free Flap Monitoring, Salvage, and Failure Timing: A Systematic Review. J. Reconstr. Microsurg. 2021, 37, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Paprottka, F.J.; Klimas, D.; Krezdorn, N.; Schlarb, D.; Trevatt, A.E.J.; Hebebrand, D. Cook–Swartz Doppler Probe Surveillance for Free Flaps—Defining Pros and Cons. Surg. J. 2020, 6, e42–e46. [Google Scholar] [CrossRef] [PubMed]
- Swartz, W.M.; Izquierdo, R.; Miller, M.J. Implantable Venous Doppler Microvascular Monitoring: Laboratory Investigation and Clinical Results. Plast. Reconstr. Surg. 1994, 93, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Kempton, S.J.; Poore, S.O.; Chen, J.T.; Afifi, A.M. Free Flap Monitoring Using an Implantable Anastomotic Venous Flow Coupler: Analysis of 119 Consecutive Abdominal-based Free Flaps for Breast Reconstruction. Microsurgery 2015, 35, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Salibian, A.A.; Bekisz, J.M.; Frey, J.D.; Thanik, V.D.; Levine, J.P.; Karp, N.S.; Choi, M. Comparing Incision Choices in Immediate Microvascular Breast Reconstruction after Nipple-Sparing Mastectomy: Unique Considerations to Optimize Outcomes. Plast. Reconstr. Surg. 2021, 148, 1173–1185. [Google Scholar] [CrossRef] [PubMed]
- Mughal, M.; Berner, J.E.; Ho-Asjoe, M.; See, M.; Roblin, P.; Rose, V.; Mohanna, P.-N. One-Stop Autologous Breast Reconstruction: A Safe and Effective Cost-Saving Pathway. J. Plast. Reconstr. Aesthetic Surg. 2023. [Google Scholar] [CrossRef]
- Perez, K.; Steppe, C.; Teotia, S.S.; Haddock, N.T. Does Fitzpatrick Score Predict Flap Loss? Microsurgical Breast Reconstruction Outcomes of Varying Skin Color. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4637. [Google Scholar] [CrossRef]
- Pusic, A.L.; Klassen, A.F.; Scott, A.M.; Klok, J.A.; Cordeiro, P.G.; Cano, S.J. Development of a New Patient-Reported Outcome Measure for Breast Surgery: The BREAST-Q. Plast. Reconstr. Surg. 2009, 124, 345–353. [Google Scholar] [CrossRef]






| Buried | Non-Buried | p Value | |||
|---|---|---|---|---|---|
| n (%) | % | n (%) | % | ||
| Total patients | 113 | 141 | |||
| Total flaps | 153 | 47.5% | 169 | 52.0% | |
| Age | 48.3 | 49.8 | 0.337 | ||
| Co-morbidities | p value | ||||
| Hypertension | 10 | 8.8% | 17 | 12.1% | 0.410 |
| BMI | 9 | 8.0% | 11 | 7.8% | 0.962 |
| Smoking | 4 | 3.5% | 14 | 9.9% | 0.049 |
| Ex smoker | 4 | 3.5% | 1 | 0.7% | 0.107 |
| Diabetes | 5 | 4.4% | 9 | 6.4% | 0.497 |
| Asthma | 9 | 8.0% | 6 | 4.3% | 0.213 |
| Other | 11 | 9.7% | 23 | 16.3% | 0.126 |
| Flaps | |||||
| DIEP | 120 | 78.4% | 143 | 84.6% | 0.129 |
| PAP | 27 | 17.6% | 18 | 10.7% | 0.056 |
| SGAP | 5 | 3.2% | 5 | 3.0% | 0.890 |
| SIEA | 1 | 0.65% | 2 | 1.2% | 0.613 |
| ALT | 0 | 0.0% | 1 | 0.6% | 0.337 |
| Unilateral vs. bilateral | |||||
| Unilateral | 52 | 34.0% | 87 | 51.5% | 0.001 |
| Bilateral | 54 | 35.3% | 43 | 27.2% | 0.138 |
| Bilateral: one buried/one non-buried | 3 | 2.0% | 3 | 1.8% | 0.915 |
| Unilateral—stacked | 16 | 10.5% | 10 | 5.9% | 0.135 |
| Unilateral—bipedicle | 20 | 13.1% | 25 | 14.8% | 0.656 |
| Bilateral—stacked | 7 | 4.6% | 0 | 0.0% | 0.005 |
| Immediate vs. delayed | |||||
| Immediate | 124 | 82.4% | 103 | 60.9% | <0.001 |
| Delayed | 29 | 19.0% | 66 | 39.1% | <0.001 |
| Immediate symmetrisation procedure | 28 | 31.9% | 26 | 21.3% | 0.085 |
| Mastectomy | |||||
| Nipple sparing | 88 | 57.5% | 13 | 7.7% | <0.001 |
| Skin reducing | 46 | 30.1% | 8 | 4.7% | <0.001 |
| Free nipple graft | 9 | 5.9% | 1 | 0.6% | 0.007 |
| Buried | Non-Buried | p Value | |||
|---|---|---|---|---|---|
| Time (min) | SD | Time (min) | SD | ||
| Ischaemia time | 62.6 | ±24.7 | 69.0 | ±24.9 | 0.036 |
| Flap weight | 509.1 | ±284.8 | 621.6 | ±287.8 | 0.002 |
| Operating time | 416.4 | ±117.9 | 383.6 | ±287.8 | 0.031 |
| Buried | Non-Buried | p Values | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Flap | |||||
| Haematoma | 7 | 4.6% | 7 | 4.1% | 0.849 |
| Fat necrosis | 2 | 1.3% | 4 | 2.4% | 0.483 |
| Flap loss | 3 | 2.0% | 3 | 1.8% | 0.902 |
| Negative takeback | 3 | 2.0% | 1 | 0.6% | 0.268 |
| RTT vein | 1 | 0.7% | 2 | 1.2% | 0.621 |
| Partial flap loss | 0 | 0% | 1 | 0.6% | 0.341 |
| Intra-operative flap issues | |||||
| Cephalic turndown | 2 | 1.3% | 3 | 1.8% | 0.734 |
| Arterial issue | 1 | 0.7% | 0 | 0% | 0.293 |
| SIEV supercharge | 2 | 1.3% | 0 | 0% | 0.136 |
| Mastectomy skin/nipple | |||||
| Wound—conservation | 10 | 6.5% | 11 | 6.5% | 0.992 |
| Wound—re-admission/re-operation | 7 | 4.6% | 6 | 3.6% | 0.641 |
| NAC loss | 4 | 2.6% | 2 | 1.2% | 0.343 |
| Donor site | |||||
| Wound—conservative | 4 | 2.6% | 11 | 6.5% | 0.098 |
| Wound—infection | 4 | 2.6% | 2 | 1.2% | 0.343 |
| Wound dehiscence—RTT | 3 | 2.0% | 6 | 3.6% | 0.388 |
| Seroma | 3 | 2.0% | 3 | 1.8% | 0.902 |
| Bulge | 0 | 0% | 1 | 0.6% | 0.341 |
| Buried | Non-Buried | p | ||||
|---|---|---|---|---|---|---|
| Additional Procedures | n | % | n | % | ||
| Lipofilling | 34 | 30.1% | 68 | 48.2% | 0.003 | |
| Nipple reconstruction | 21 | 18.6% | 72 | 51.1% | <0.001 | |
| Scar revision | 7 | 6.2% | 7 | 5.0% | 0.669 | |
| Symmetrisation | 15 | 13.3% | 23 | 16.3% | 0.500 | |
| Dog ear excision | 2 | 1.8% | 5 | 3.5% | 0.390 | |
| FTSG to mastectomy wound | 2 | 1.8% | 0 | 0% | 0.113 | |
| Total additional procedures for breast appearance | ||||||
| No further procedures | 59 | 52.2% | 36 | 25.5% | <0.001 | |
| 1 | 44 | 38.9% | 72 | 51.1% | ||
| 2 | 6 | 5.3% | 19 | 13.5% | ||
| 3 | 3 | 2.7% | 5 | 3.5% | ||
| >3 | 1 | 0.9% | 5 | 3.5% | ||
| Average | 0.62 | 1 | 1.12 | <0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Creasy, H.; Citron, I.; Davis, T.P.; Cooper, L.; Din, A.H.; Rose, V. Buried Autologous Breast Reconstruction: Outcomes and Technical Considerations. J. Clin. Med. 2024, 13, 1463. https://doi.org/10.3390/jcm13051463
Creasy H, Citron I, Davis TP, Cooper L, Din AH, Rose V. Buried Autologous Breast Reconstruction: Outcomes and Technical Considerations. Journal of Clinical Medicine. 2024; 13(5):1463. https://doi.org/10.3390/jcm13051463
Chicago/Turabian StyleCreasy, Henrietta, Isabelle Citron, Timothy P. Davis, Lilli Cooper, Asmat H. Din, and Victoria Rose. 2024. "Buried Autologous Breast Reconstruction: Outcomes and Technical Considerations" Journal of Clinical Medicine 13, no. 5: 1463. https://doi.org/10.3390/jcm13051463
APA StyleCreasy, H., Citron, I., Davis, T. P., Cooper, L., Din, A. H., & Rose, V. (2024). Buried Autologous Breast Reconstruction: Outcomes and Technical Considerations. Journal of Clinical Medicine, 13(5), 1463. https://doi.org/10.3390/jcm13051463





