Evaluation of Esthetic Results after Mass Removal with Elliptical Skin Excision Using Ultrasonography to Measure Skin Thickness
Abstract
1. Introduction
2. Materials and Methods
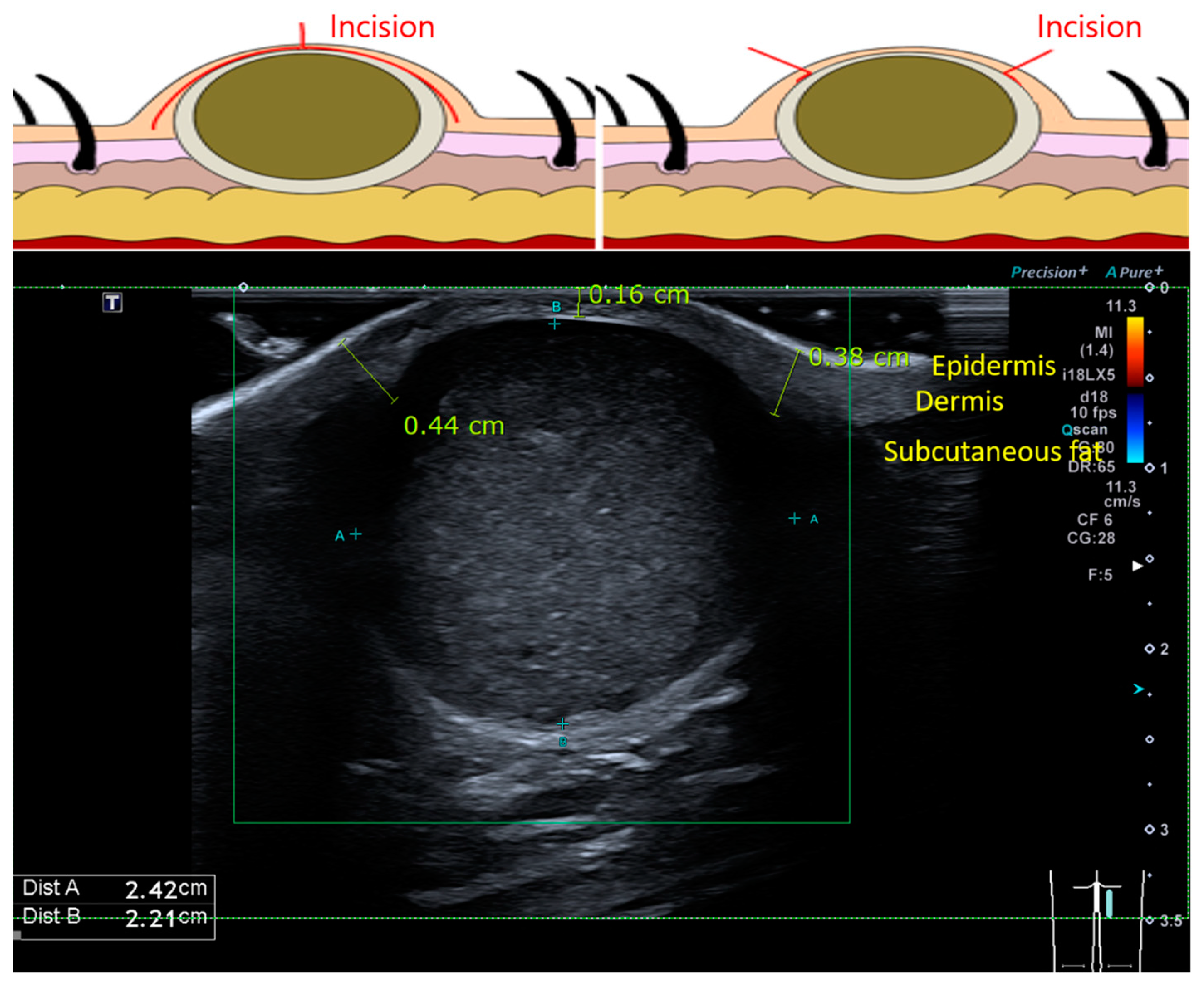
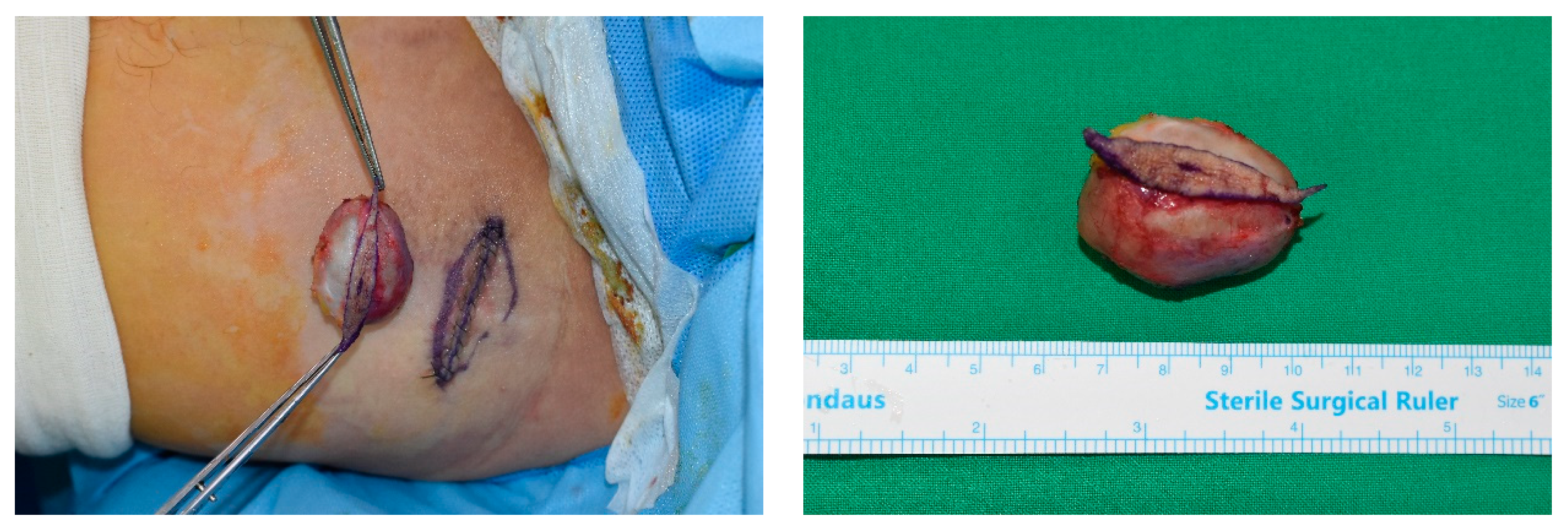
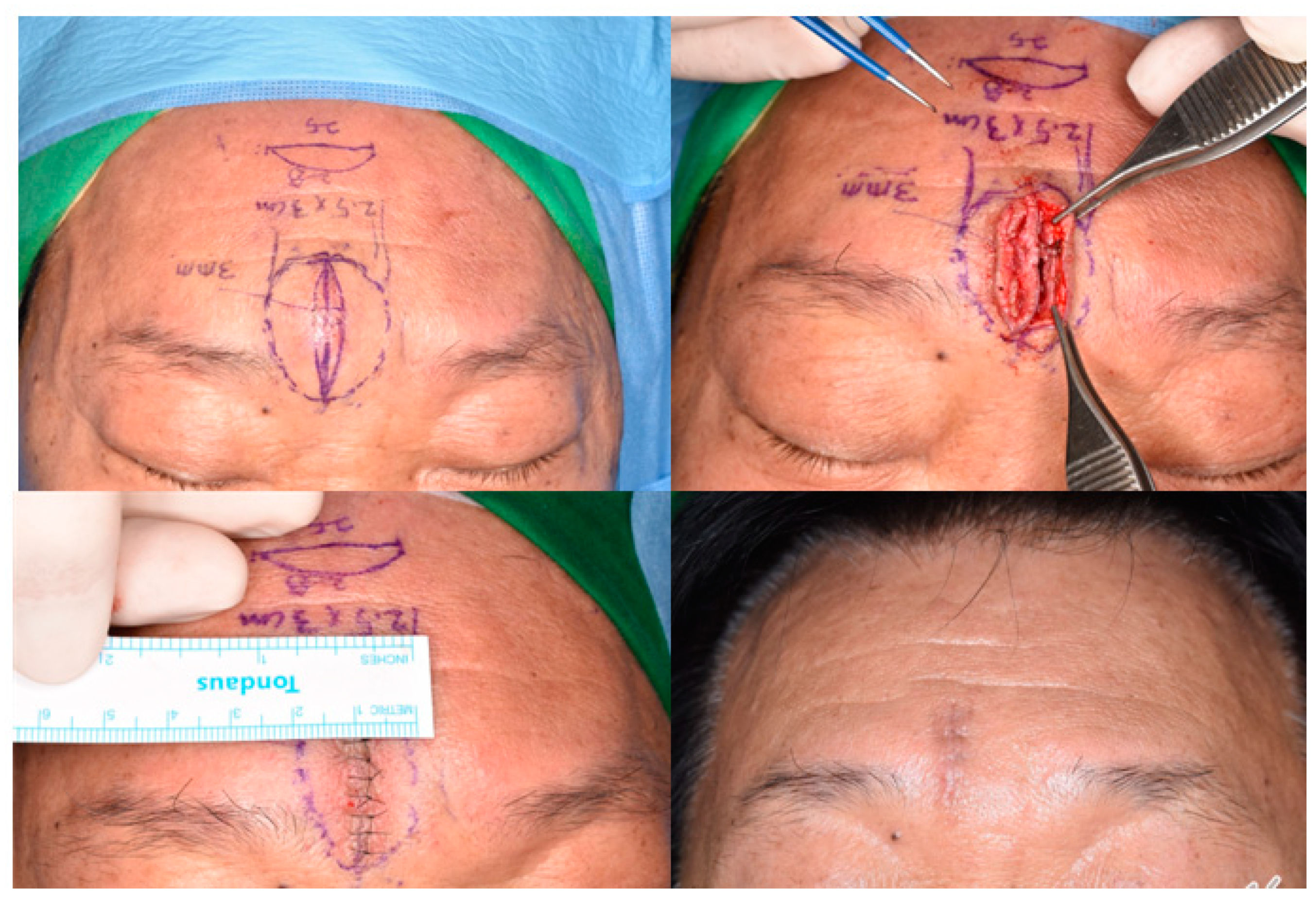
2.1. Patient Selection and Surgical Methods
2.2. Outcome Assessment
2.3. Cutometer
2.4. mVSS
2.5. Statistical Analysis
3. Results
3.1. Patients
3.2. Quantitative Evaluation (Objective)
3.3. mVSS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fitzpatrick, T.B.; Freedberg, I.M. Fitzpatrick’s Dermatology in General Medicine, 6th ed.; McGraw-Hill: New York, NY, USA, 2003; pp. 774–775. [Google Scholar]
- Cillo, J.E., Jr.; Caloss, R.; Wendelken, J.A. Excision of subcutaneous facial cysts and lipomas using cosmetic approaches. J. Oral. Maxillofac. Surg. 2006, 64, 1603–1616. [Google Scholar] [CrossRef] [PubMed]
- Shalom, A.; Persitz, A.; Westreich, M. A surgical technique for excision of epidermal cysts. Dermatol. Surg. 2012, 38, 1856–1858. [Google Scholar] [CrossRef] [PubMed]
- Itoh, Y.; Watanabe, Y.; Henta, T.; Ishibashi, A. Endoscopic extraction and curettage of epidermal cysts on the face. Br. J. Plast. Surg. 1999, 52, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M. Treating a sebaceous cyst: An incisional technique. Aesthetic Plast. Surg. 2001, 25, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, B.; Douglas, S.; Mirza, S. Skin incisions for the excision of spherical cutaneous and subcutaneous lesions. J. Laryngol. Otol. 2009, 123, 1250–1251. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Yang, K.C. A new method for facial epidermoid cyst removal with minimal incision. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 887–890. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.C.; Hao, L.M.; Tan, J.X.; Huang, Y.B.; Huang, H.F.; Hu, J.; Bi, M.Y. Efficacy of the combination of minimally invasive CO(2) laser incision with photodynamic therapy for infected epidermoid cysts. Photodiagnosis Photodyn. Ther. 2020, 30, 101791. [Google Scholar] [CrossRef]
- Lee, H.E.; Yang, C.H.; Chen, C.H.; Hong, H.S.; Kuan, Y.Z. Comparison of the surgical outcomes of punch incision and elliptical excision in treating epidermal inclusion cysts: A prospective, randomized study. Dermatol. Surg. 2006, 32, 520–525. [Google Scholar] [CrossRef]
- Cheeley, J.; Delong Aspey, L.; MacKelfresh, J.; Pennie, M.; Chen, S. Comparison of elliptical excision versus punch incision for the treatment of epi-dermal inclusion cysts: A prospective, randomized study. J. Am. Acad. Dermatol. 2018, 79, 360–361. [Google Scholar] [CrossRef]
- Ikizoglu, G.; Kaya, T.I.; Tursen, U.; Baz, K. The use of the freer dissector for the removal of trichilemmal cysts. Int. J. Dermatol. 2003, 42, 405–407. [Google Scholar] [CrossRef]
- Salasche, S.J.; Orengo, I. Surgical pearl: The retraction suture. J. Am. Acad. Dermatol. 1994, 30, 118–120. [Google Scholar] [CrossRef] [PubMed]
- Mizunuma, M.; Yanai, A.; Tsutsumi, S.; Yoshida, H.; Seno, H.; Inoue, M.; Nishida, M. Can dog-ear formation be decreased when an S-shaped skin resection is used instead of a spindle skin resection? A three-dimensional analysis of skin surgery techniques using the finite element method. Plast. Reconstr. Surg. 2000, 106, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Raveh Tilleman, T.; Tilleman, M.M.; Krekels, G.A.; Neumann, M.H. Skin waste, vertex angle, and scar length in excisional biopsies: Comparing five excision patterns—Fusiform ellipse, fusiform circle, rhomboid, mosque, and S-shaped. Plast. Reconstr. Surg. 2004, 113, 857–861. [Google Scholar] [CrossRef]
- Tilleman, T.R. Direct closure of round skin defects: A four-step technique with multiple subcutaneous and cutaneous “figure-of-8” sutures alleviating dog-ears. Plast. Reconstr. Surg. 2004, 114, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.H.; Kim, M.; Shin, J.W.; Na, J.I.; Huh, C.H. Comparison of Surgical Outcomes of Rectangular Lid Excision Versus Elliptical Excision for the Treatment of Epidermal Cysts. Dermatol. Surg. 2019, 45, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.R. Use of the inverted parachute retraction suture for epidermal cyst removal. J. Am. Acad. Dermatol. 2018, 78, e7–e8. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Lee, S.J.; Kim, H.J.; Lee, J.H.; Jeong, H.S.; Suh, I.S. Aging-related changes in the mid-face skin elasticity in East Asian women. Arch. Craniofac. Surg. 2019, 20, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Draaijers, L.J.; Botman, Y.A.; Tempelman, F.R.; Kreis, R.W.; Middelkoop, E.; van Zuijlen, P.P. Skin elasticity meter or subjective evaluation in scars: A reliability assessment. Burns 2004, 30, 109–114. [Google Scholar] [CrossRef]
- Nedelec, B.; Correa, J.A.; Rachelska, G.; Armour, A.; LaSalle, L. Quantitative measurement of hypertrophic scar: Interrater reliability and con-current validity. J. Burn. Care Res. 2008, 29, 501–511. [Google Scholar] [CrossRef]
- Verhaegen, P.; van der Wal, M.B.A.; Middelkoop, E.; van Zuijlen, P.P.M. Objective scar assessment tools: A clinimetric appraisal. Plast. Reconstr. Surg. 2011, 127, 1561–1570. [Google Scholar] [CrossRef]
- Busche, M.N.; Thraen, A.J.; Gohritz, A.; Rennekampff, H.O.; Vogt, P.M. Burn Scar Evaluation Using the Cutometer® MPA 580 in Comparison to “Patient and Observer Scar Assessment Scale” and “Vancouver Scar Scale”. J. Burn. Care Res. 2018, 39, 516–526. [Google Scholar] [CrossRef]
- Abbas, D.B.; Lavin, C.V.; Fahy, E.J.; Griffin, M.; Guardino, N.; King, M.; Chen, K.; Lorenz, P.H.; Gurtner, G.C.; Longaker, M.T.; et al. Standardizing Dimensionless Cutometer Parameters to Determine In Vivo Elasticity of Human Skin. Adv. Wound Care 2022, 11, 297–310. [Google Scholar] [CrossRef]
- Yoon, C.S.; Kim, H.B.; Kim, Y.K.; Kim, H.; Kim, K.N. Keystone-design perforator island flaps for the management of complicated epi-dermoid cysts on the back. Sci. Rep. 2019, 9, 14699. [Google Scholar] [CrossRef]
- Kim, H.; Ryu, W.C.; Yoon, C.S.; Kim, K.N. Keystone-designed buried de-epithelialized flap: A novel technique for obliterating small to moderately sized dead spaces. Medicine 2017, 96, e7008. [Google Scholar] [CrossRef] [PubMed]
- Zuber, T.J. Minimal excision technique for epidermoid (sebaceous) cysts. Am. Fam. Physician 2002, 65, 1409–1412. [Google Scholar]
- Gierek, M.; Bergler-Czop, B.; Słaboń, A.; Łabuś, W.; Ochała-Gierek, G. Laser speckle contrast analysis (LASCA): A new device in the diagnosis and monitoring of surgical treatment of hidradenitis suppurativa. Adv. Dermatol. Allergol. Postępy Dermatol. I Alergol. 2023, 40, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Klama-Baryła, A.; Łabuś, W.; Bergler-Czop, B.; Pietrauszka, K.; Niemiec, P. Platelet-Rich Plasma and Acellular Dermal Matrix in the Surgical Treatment of Hidradenitis Suppurativa: A Comparative Retrospective Study. J. Clin. Med. 2023, 12, 2112. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Łabuś, W.; Słaboń, A.; Ziółkowska, K.; Ochała-Gierek, G.; Kitala, D.; Szyluk, K.; Niemiec, P. Co-Graft of Acellular Dermal Matrix and Split Thickness Skin Graft—A New Reconstructive Surgical Method in the Treatment of Hidradenitis Suppurativa. Bioengineering 2022, 9, 389. [Google Scholar] [CrossRef]
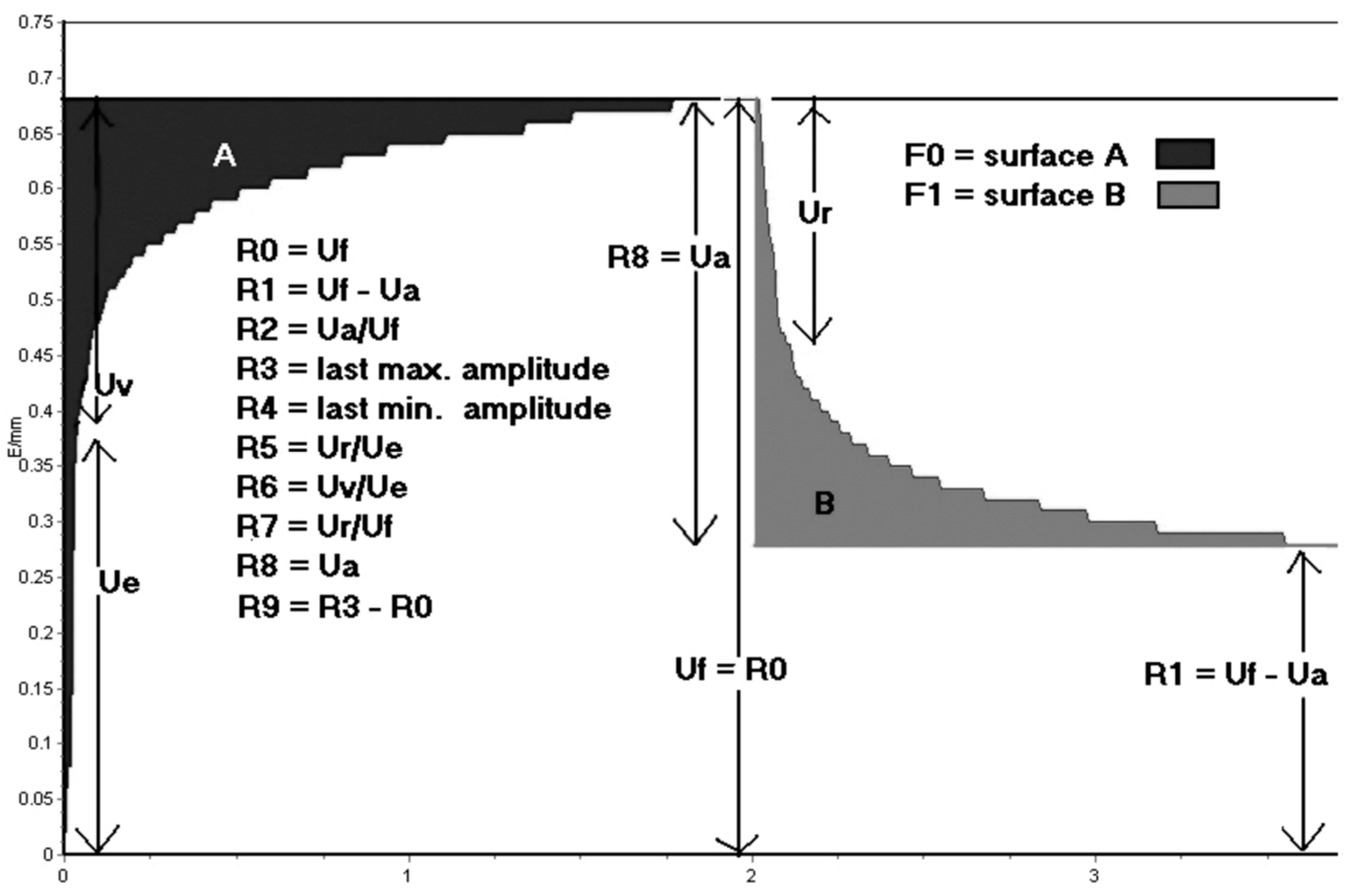

| Parameters | Representation | Equivalent |
|---|---|---|
| R0 | The final distension of the first curve | Uf |
| R1 | The ability to return to the original state | Uf-Ua |
| R2 | The overall elasticity of the skin, including creep and creep recovery | Ua/Uf |
| R3 | The last maximum highest point of the last curve | Last Uf |
| R4 | The last minimal lowest point of the last curve | Last R |
| R5 | The net elasticity | Ur/Ue |
| R6 | The ratio of viscoelastic to elastic extension, also called the viscoelastic ratio | Uv/Ue |
| R7 | The ratio of elastic recovery to the total deformation | Ur/Uf |
| R8 | The Ua of the first curve | First Ua |
| R9 | The residual deformation at the end of the measuring cycle | R3–R0 |
| Male (n = 524) | Female (n = 456) | Total (n = 980) | |
|---|---|---|---|
| Age (years) | 58.1 (13–84) | 43.2 (4–75) | 53.5 (4–84) |
| Location, n (%) | |||
| Head and neck | 386 (73.7) | 309 (67.8) | 695 (70.9) |
| Trunk | 90 (17.2) | 83 (18.2) | 173 (17.7) |
| Extremities | 48 (9.2) | 64 (14.0) | 112 (11.4) |
| Pathology, n (%) | |||
| Epidermal cyst | 278 (53.1) | 193 (42.3) | 471 (48.1) |
| Lipoma | 71 (13.5) | 60 (13.2) | 131 (13.4) |
| Pilomatricoma | 22 (4.2) | 34 (7.5) | 56 (5.7) |
| Dermoid cyst | 8 (1.5) | 15 (3.3) | 23 (2.3) |
| Other benign masses | 145 (27.7) | 154 (33.8) | 299 (30.5) |
| Surgical Time | |
|---|---|
| Size (mm) (long axis × short axis) | 14.21 ± 7.50 × 11.33 ± 6.93 |
| Incision line (mm) (length × width) | 14.77 ± 7.15 × 2.17 ± 1.24 |
| Surgical time (min) | 17.48 ± 3.46 |
| Cutometer MPA 580 | |||
|---|---|---|---|
| Parameters | Suture Line | Normal Skin | p-Value |
| R0 | 1.33 ± 0.30 | 1.52 ± 0.30 | <0.05 |
| R1 | 0.42 ± 0.25 | 0.39 ± 0.24 | <0.05 |
| R2 | 0.70 ± 0.15 | 0.75 ± 0.12 | <0.05 |
| R3 | 1.49 ± 0.30 | 1.65 ± 0.31 | <0.05 |
| R4 | 1.19 ± 0.32 | 1.24 ± 0.33 | <0.05 |
| R5 | 1.48 ± 0.31 | 1.27 ± 0.30 | <0.05 |
| R6 | 0.75 ± 0.17 | 0.65 ± 0.16 | <0.05 |
| R7 | 0.64 ± 0.21 | 0.52 ± 0.20 | <0.05 |
| R8 | 0.92 ± 0.26 | 1.13 ± 0.25 | <0.05 |
| R9 | 0.16 ± 0.02 | 0.12 ± 0.04 | <0.05 |
| mVSS | |||
|---|---|---|---|
| Postoperative | 1 Month | 3 Months | p-Value |
| Vascularity | 0.61 ± 0.75 | 0.35± 0.44 | <0.05 |
| Pigmentation | 1.38 ± 0.82 | 0.88 ± 0.60 | <0.05 |
| Pliability | 1.85 ± 1.10 | 1.58 ± 1.12 | <0.05 |
| Height | 0.30 ± 0.47 | 0.41 ± 0.52 | <0.05 |
| Pain | 0.76 ± 0.83 | 0.45 ± 0.30 | <0.05 |
| Total | 5.06 ± 3.97 | 3.67 ± 2.98 | <0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woo, S.S.; Gwak, H.; Kim, K.H.; Lee, J.W.; Choi, J.K.; Suh, I.; Kim, S.H. Evaluation of Esthetic Results after Mass Removal with Elliptical Skin Excision Using Ultrasonography to Measure Skin Thickness. J. Clin. Med. 2024, 13, 1467. https://doi.org/10.3390/jcm13051467
Woo SS, Gwak H, Kim KH, Lee JW, Choi JK, Suh I, Kim SH. Evaluation of Esthetic Results after Mass Removal with Elliptical Skin Excision Using Ultrasonography to Measure Skin Thickness. Journal of Clinical Medicine. 2024; 13(5):1467. https://doi.org/10.3390/jcm13051467
Chicago/Turabian StyleWoo, Sang Seok, Hongki Gwak, Ki Hyun Kim, Jun Won Lee, Jai Koo Choi, Insuck Suh, and Seong Hwan Kim. 2024. "Evaluation of Esthetic Results after Mass Removal with Elliptical Skin Excision Using Ultrasonography to Measure Skin Thickness" Journal of Clinical Medicine 13, no. 5: 1467. https://doi.org/10.3390/jcm13051467
APA StyleWoo, S. S., Gwak, H., Kim, K. H., Lee, J. W., Choi, J. K., Suh, I., & Kim, S. H. (2024). Evaluation of Esthetic Results after Mass Removal with Elliptical Skin Excision Using Ultrasonography to Measure Skin Thickness. Journal of Clinical Medicine, 13(5), 1467. https://doi.org/10.3390/jcm13051467






