The Effect of Severe Varus Deformity on Clinical and Radiographic Outcomes in Mechanical Aligned Total Knee Arthroplasty with Medial Stabilizing Technique
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Surgical Technique
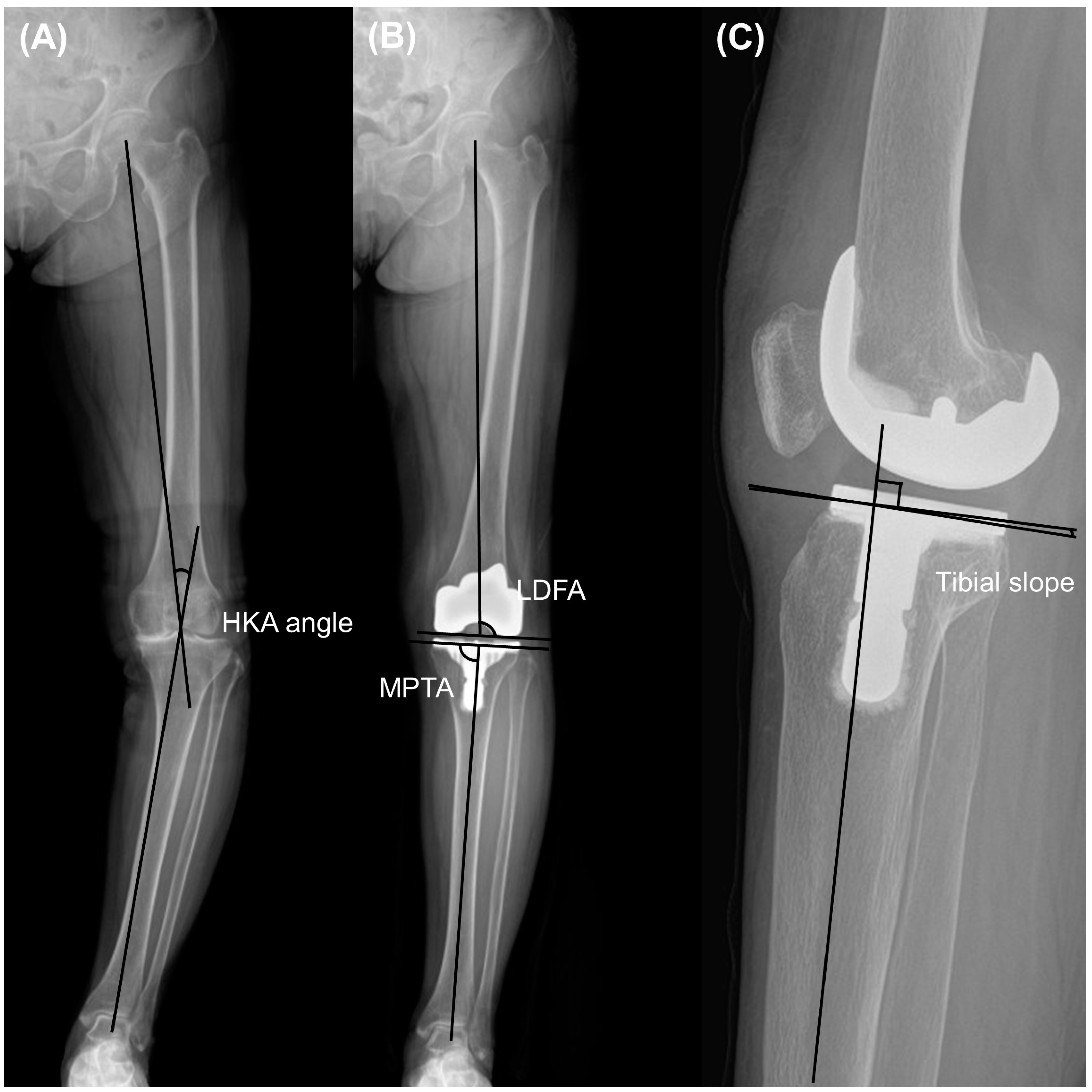
2.3. Clinical and Radiographic Assessments
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, H.J.; Kim, S.H.; Park, Y.B. Selective medial release using multiple needle puncturing with a spacer block in situ for correcting severe varus deformity during total knee arthroplasty. Arch. Orthop. Trauma. Surg. 2020, 140, 1523–1531. [Google Scholar] [CrossRef]
- Herschmiller, T.; Grosso, M.J.; Cunn, G.J.; Murtaugh, T.S.; Gardner, T.R.; Geller, J.A. Step-wise medial collateral ligament needle puncturing in extension leads to a safe and predictable reduction in medial compartment pressure during TKA. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1759–1766. [Google Scholar] [CrossRef]
- Toyooka, S.; Masuda, H.; Nishihara, N.; Miyamoto, W.; Kobayashi, T.; Kawano, H.; Nakagawa, T. Assessing the Role of Minimal Medial Tissue Release during Navigation-Assisted Varus Total Knee Arthroplasty Based on the Degree of Preoperative Varus Deformity. J. Knee Surg. 2022, 35, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Zambianchi, F.; Giorgini, A.; Ensini, A.; Lombari, V.; Daffara, V.; Catani, F. Navigated, soft tissue-guided total knee arthroplasty restores the distal femoral joint line orientation in a modified mechanically aligned technique. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 966–974. [Google Scholar] [CrossRef]
- Ishibashi, K.; Sasaki, E.; Sasaki, S.; Kimura, Y.; Yamamoto, Y.; Ishibashi, Y. Medial stabilizing technique preserves anatomical joint line and increases range of motion compared with the gap-balancing technique in navigated total knee arthroplasty. Knee 2020, 27, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Tsubosaka, M.; Muratsu, H.; Nakano, N.; Kamenaga, T.; Kuroda, Y.; Inokuchi, T.; Miya, H.; Kuroda, R.; Matsumoto, T. Knee Stability following Posterior-Stabilized Total Knee Arthroplasty: Comparison of Medial Preserving Gap Technique and Measured Resection Technique. J. Knee Surg. 2021, 36, 95–104. [Google Scholar] [CrossRef]
- Puliero, B.; Favreau, H.; Eichler, D.; Adam, P.; Bonnomet, F.; Ehlinger, M. Total knee arthroplasty in patients with varus deformities greater than ten degrees: Survival analysis at a mean ten year follow-up. Int. Orthop. 2019, 43, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.M.; Bin, S.I.; Kim, J.Y.; Cho, H.I.; Lee, B.S.; Kim, J.M. Does the Preoperative Varus Deformity Influence the Survival of Postoperative Neutral-Aligned TKAs? An Analysis With a Minimum 5-Year Follow-Up. J. Arthroplast. 2018, 33, 3181–3185. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Bin, S.I.; Kim, J.M.; Lee, B.S.; Lee, C.R.; Kwon, Y.H. Using a Tibial Short Extension Stem Reduces Tibial Component Loosening After Primary Total Knee Arthroplasty in Severely Varus Knees: Long-term Survival Analysis With Propensity Score Matching. J. Arthroplast. 2018, 33, 2512–2517. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.S.; Lee, S.J.; Kim, J.M.; Lee, D.H.; Cha, E.J.; Bin, S.I. No impact of severe varus deformity on clinical outcome after posterior stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 960–966. [Google Scholar] [CrossRef]
- Lee, S.S.; Lee, J.; Alharthi, H.; Moon, Y.W. Effect of mediolateral gap difference on postoperative outcomes in navigation-assisted total knee arthroplasty using an ultracongruent insert and the medial stabilising technique. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3745–3754. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar] [PubMed]
- Insall, J.N.; Dorr, L.D.; Scott, R.D.; Scott, W.N. Rationale of the Knee Society clinical rating system. Clin. Orthop. Relat. Res. 1989, 248, 13–14. [Google Scholar] [CrossRef]
- Choi, B.S.; Kim, J.M.; Han, H.S. Decision-making factors and their thresholds for total knee arthroplasty in lateral tibiofemoral osteoarthritis patients: A retrospective cohort study. Knee Surg. Relat. Res. 2022, 34, 41. [Google Scholar] [CrossRef] [PubMed]
- Miralles-Munoz, F.A.; Gonzalez-Parreno, S.; Martinez-Mendez, D.; Gonzalez-Navarro, B.; Ruiz-Lozano, M.; Lizaur-Utrilla, A.; Alonso-Montero, C. A validated outcome categorization of the knee society score for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1266–1272. [Google Scholar] [CrossRef]
- Pawar, P.; Naik, L.; Sahu, D.; Bagaria, V. Comparative Study of Pinless Navigation System versus Conventional Instrumentation in Total Knee Arthroplasty. Clin. Orthop. Surg. 2021, 13, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Shon, O.J.; Kim, G.B. Does the degree of intraoperatively identified cartilage loss affect the outcomes of primary total knee arthroplasty without patella resurfacing? A prospective comparative cohort study. Knee Surg. Relat. Res. 2022, 34, 36. [Google Scholar] [CrossRef] [PubMed]
- Piovan, G.; Farinelli, L.; Screpis, D.; Iacono, V.; Povegliano, L.; Bonomo, M.; Auregli, L.; Zorzi, C. Distal femoral osteotomy versus lateral unicompartmental arthroplasty for isolated lateral tibiofemoral osteoarthritis with intra-articular and extra-articular deformity: A propensity score-matched analysis. Knee Surg. Relat. Res. 2022, 34, 34. [Google Scholar] [CrossRef] [PubMed]
- Hess, S.; Moser, L.B.; Robertson, E.L.; Behrend, H.; Amsler, F.; Iordache, E.; Leclercq, V.; Hirschmann, M.T. Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientations in a cross-sectional study based on 3D reconstructed CT images. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 407–418. [Google Scholar] [CrossRef]
- Song, E.K.; Agrawal, P.R.; Kim, S.K.; Seo, H.Y.; Seon, J.K. A randomized controlled clinical and radiological trial about outcomes of navigation-assisted TKA compared to conventional TKA: Long-term follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3381–3386. [Google Scholar] [CrossRef]
- Lee, S.S.; Kim, J.H.; Heo, J.W.; Moon, Y.W. Gradual change in knee extension following total knee arthroplasty using ultracongruent inserts. Knee 2019, 26, 905–913. [Google Scholar] [CrossRef]
- Okamoto, S.; Okazaki, K.; Mitsuyasu, H.; Matsuda, S.; Mizu-Uchi, H.; Hamai, S.; Tashiro, Y.; Iwamoto, Y. Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 3174–3180. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Moon, J.Y.; Song, E.K.; Lim, H.A.; Seon, J.K. Minimum Two-year Results of Revision Total Knee Arthroplasty Following Infectious or Non-infectious Causes. Knee Surg. Relat. Res. 2012, 24, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Bae, D.K.; Baek, J.H.; Yoon, K.T.; Son, H.S.; Song, S.J. Comparison of patellofemoral outcomes after TKA using two prostheses with different patellofemoral design features. Knee Surg. Sports Traumatol. Arthrosc. 2016, 25, 747–3754. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Bardgett, M.; Weir, D.; Holland, J.; Gerrand, C.; Deehan, D.J. What is the Minimum Clinically Important Difference for the WOMAC Index After TKA? Clin. Orthop. Relat. Res. 2018, 476, 2005–2014. [Google Scholar] [CrossRef] [PubMed]
- An, V.V.G.; Twiggs, J.; Leie, M.; Fritsch, B.A. Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 2019, 26, 466–476. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Howell, S.M.; Won, Y.Y.; Lee, O.S.; Lee, S.H.; Vahedi, H.; Teo, S.H. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3467–3479. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Campanelli, V.; Howell, S.; Hull, M. Kinematic alignment more closely restores the groove location and the sulcus angle of the native trochlea than mechanical alignment: Implications for prosthetic design. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1504–1513. [Google Scholar] [CrossRef]
- Zambianchi, F.; Bazzan, G.; Marcovigi, A.; Pavesi, M.; Illuminati, A.; Ensini, A.; Catani, F. Joint line is restored in robotic-arm-assisted total knee arthroplasty performed with a tibia-based functional alignment. Arch. Orthop. Trauma. Surg. 2021, 141, 2175–2184. [Google Scholar] [CrossRef]
- Seo, J.G.; Moon, Y.W.; Kim, S.M.; Park, S.H.; Lee, B.H.; Chang, M.J.; Jo, B.C. Prevention of pseudo-patella baja during total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3601–3606. [Google Scholar] [CrossRef]
- Azukizawa, M.; Kuriyama, S.; Nakamura, S.; Nishitani, K.; Lyman, S.; Morita, Y.; Furu, M.; Ito, H.; Matsuda, S. Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch. Orthop. Trauma. Surg. 2018, 138, 1143–1150. [Google Scholar] [CrossRef]
- Tanaka, Y.; Nakamura, S.; Kuriyama, S.; Nishitani, K.; Ito, H.; Lyman, S.; Matsuda, S. Intraoperative physiological lateral laxity in extension and flexion for varus knees did not affect short-term clinical outcomes and patient satisfaction. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3888–3898. [Google Scholar] [CrossRef]
- Nagai, K.; Muratsu, H.; Kanda, Y.; Tsubosaka, M.; Kamenaga, T.; Miya, H.; Matsushita, T.; Niikura, T.; Kuroda, R.; Matsumoto, T. Intraoperative soft tissue balance using novel medial preserving gap technique in posterior-stabilized total knee arthroplasty: Comparison to measured resection technique. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3474–3481. [Google Scholar] [CrossRef]
- Kim, J.S.; Cho, C.H.; Lee, M.C.; Han, H.S. Risk factors of de novo hyperextension developed after posterior cruciate ligament substituting total knee arthroplasty: A matched case-control study. Knee Surg. Sports Traumatol. Arthrosc. 2021, 31, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Sekiya, H.; Takatoku, K.; Takada, H.; Sasanuma, H.; Sugimoto, N. Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin. Orthop. Relat. Res. 2009, 467, 1582–1586. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Lee, C.R.; Gwak, H.C.; Kim, J.H.; Kwon, Y.U.; Kim, D.Y. The Effects of Surgical Technique in Total Knee Arthroplasty for Varus Osteoarthritic Knee on the Rotational Alignment of Femoral Component: Gap Balancing Technique versus Measured Resection Technique. J. Knee Surg. 2020, 33, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.; Baker, K.; Hommel, H.; Bernard, M.; Kopf, S. No correlation between rotation of femoral components in the transverse plane and clinical outcome after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1456–1462. [Google Scholar] [CrossRef]





| Age, year | 71.1 ± 5.2 (57–82) |
| Sex, male:female | 0:158 |
| Body mass index, kg/m2 | 26.7 ± 3.1 (20–37.5) |
| Direction, right:left | 80:78 |
| Mean follow up period, months | 29.6 ± 8.8 (23.7–56.7) |
| Preoperative HKA angle, ° | 9.9 ± 4.3 (0.6–23) |
| Preoperative LDFA, ° | 83.4 ± 2.5 (78.5–89.9) |
| Preoperative MPTA, ° | 84.0 ± 3.3 (73–90) |
| Preoperative tibial slope, ° | 9.1 ± 3.0 (1–16.2) |
| Preoperative patellar tilt angle, ° | 9.8 ± 5.1 (−0.9–22.3) |
| Preoperation | Postoperation | p Value | |
|---|---|---|---|
| Range of motion, ° | 132.6 ± 21.3 | 142.3 ± 13.3 | <0.001 |
| WOMAC index | 55.3 ± 16.6 | 8.3 ± 4.9 | <0.001 |
| KSKS | 58.8 ± 5.6 | 93.9 ± 7.1 | <0.001 |
| KSFS | 51.7 ± 7.4 | 81.7 ± 15.6 | <0.001 |
| HKA angle, ° | 9.9 ± 4.3 | 1.2 ± 1.7 | <0.001 |
| LDFA, ° | 83.4 ± 2.5 | 89.8 ± 2.2 | <0.001 |
| MPTA, ° | 84.0 ± 3.3 | 89.5 ± 1.8 | <0.001 |
| Tibial slope, ° | 9.1 ± 3.0 | 4.0 ± 2.2 | <0.001 |
| Patellar tilt angle, ° | 9.8 ± 5.1 | 9.2 ± 4.6 | 0.07 |
| Extension angle on full extension lateral radiographs, ° | 4.4 ± 2.9 | 3.0 ± 2.4 | <0.001 |
| Femoral condylar offset, mm | 28.8 ± 3.4 | 31.3 ± 3.0 | <0.001 |
| Joint line distance, mm | 17.2 ± 3.8 | 18.4 ± 2.8 | <0.001 |
| Mild Varus Group | Severe Varus Group | p Value | |
|---|---|---|---|
| Number of knees | 131 | 27 | |
| Age, year | 71.3 ± 5.3 | 70.0 ± 4.9 | 0.215 |
| Body mass index, kg/m2 | 26.6 ± 3.2 | 26.9 ± 2.7 | 0.632 |
| Direction, right:left | 68:63 | 12:15 | 0.53 |
| Range of motion, ° | 133.2 ± 20.8 | 129.6 ± 24.0 | 0.429 |
| WOMAC index | 55.9 ± 17.5 | 53.9 ± 11.2 | 0.637 |
| KSKS | 59.1 ± 5.7 | 57.1 ± 5.1 | 0.102 |
| KSFS | 50.7 ± 7.3 | 50.4 ± 6.6 | 0.786 |
| HKA angle, ° | 8.4 ± 2.9 | 16.9 ± 2.4 | <0.001 |
| LDFA, ° | 83.3 ± 2.6 | 83.9 ± 1.9 | 0.225 |
| MPTA, ° | 84.7 ± 2.8 | 80.7 ± 3.2 | <0.001 |
| Tibial slope, ° | 9.1 ± 2.9 | 9.0 ± 3.3 | 0.897 |
| Patellar tilt angle, ° | 9.8 ± 5.1 | 9.8 ± 5.5 | 0.997 |
| Extension angle on full extension lateral radiographs, ° | 4.5 ± 3.0 | 4.0 ± 2.6 | 0.384 |
| Femoral condylar offset, mm | 28.7 ± 3.4 | 29.4 ± 3.1 | 0.304 |
| Joint line distance, mm | 17.2 ± 3.8 | 17.2 ± 3.7 | 0.99 |
| Mild Varus Group | Severe Varus Group | p Value | |
|---|---|---|---|
| Range of motion, ° | 142.2 ± 13.8 | 142.6 ± 10.6 | 0.882 |
| WOMAC index | 8.6 ± 5.0 | 7.1 ± 4.1 | 0.181 |
| KSKS | 94.2 ± 7.0 | 92.3 ± 7.2 | 0.133 |
| KSFS | 81.3 ± 16.0 | 83.9 ± 13.5 | 0.215 |
| HKA angle, ° | 1.0 ± 1.4 | 2.2 ± 2.6 | 0.001 |
| Outlier of HKA angle, % (n) | 8.4% (11) | 14.8% (4) | 0.47 |
| LDFA, ° | 89.6 ± 2.1 | 90.4 ± 1.8 | 0.088 |
| Outlier of LDFA angle, % (n) | 6.9% (9) | 7.4% (2) | 0.92 |
| MPTA, ° | 89.6 ± 1.6 | 89.2 ± 1.5 | 0.232 |
| Outlier of MPTA angle, % (n) | 4.6% (6) | 3.7% (1) | 0.84 |
| Tibial slope, ° | 3.9 ± 2.2 | 4.3 ± 2.3 | 0.419 |
| Patellar tilt angle, ° | 9.0 ± 4.7 | 10.1 ± 4.0 | 0.263 |
| Extension angle on full extension lateral radiographs, ° | 3.2 ± 2.3 | 2.0 ± 2.9 | 0.02 |
| Femoral condylar offset, mm | 31.2 ± 3.0 | 32.0 ± 2.6 | 0.142 |
| Joint line distance, mm | 18.4 ± 2.8 | 18.6 ± 2.7 | 0.676 |
| Change of joint line distance, mm | 1.1 ± 4.0 | 1.4 ± 3.4 | 0.756 |
| Femoral component rotation angle, ° | −1.7 ± 1.0 | −1.0 ± 1.3 | 0.018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-S.; Jung, J.; Kim, H.; Kim, J.; Jung, I.G.; Kim, J.; Moon, Y.-W. The Effect of Severe Varus Deformity on Clinical and Radiographic Outcomes in Mechanical Aligned Total Knee Arthroplasty with Medial Stabilizing Technique. J. Clin. Med. 2024, 13, 1595. https://doi.org/10.3390/jcm13061595
Lee S-S, Jung J, Kim H, Kim J, Jung IG, Kim J, Moon Y-W. The Effect of Severe Varus Deformity on Clinical and Radiographic Outcomes in Mechanical Aligned Total Knee Arthroplasty with Medial Stabilizing Technique. Journal of Clinical Medicine. 2024; 13(6):1595. https://doi.org/10.3390/jcm13061595
Chicago/Turabian StyleLee, Sung-Sahn, Jewon Jung, Hanbit Kim, Jinwoo Kim, In Geol Jung, Jiin Kim, and Young-Wan Moon. 2024. "The Effect of Severe Varus Deformity on Clinical and Radiographic Outcomes in Mechanical Aligned Total Knee Arthroplasty with Medial Stabilizing Technique" Journal of Clinical Medicine 13, no. 6: 1595. https://doi.org/10.3390/jcm13061595





