Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection Criteria
- -
- Patients under 18 years old;
- -
- Rheumatoid arthritis or other inflammatory diseases;
- -
- Neurological disorders or other lower limb disruptions;
- -
- Symptomatic abnormal metatarsal formula with relatively longer second or third metatarsals;
- -
- Prior hallux surgery;
- -
- First metatarsophalangeal joint osteoarthritis that was more than grade 2 according to the Regnauld classification [19].
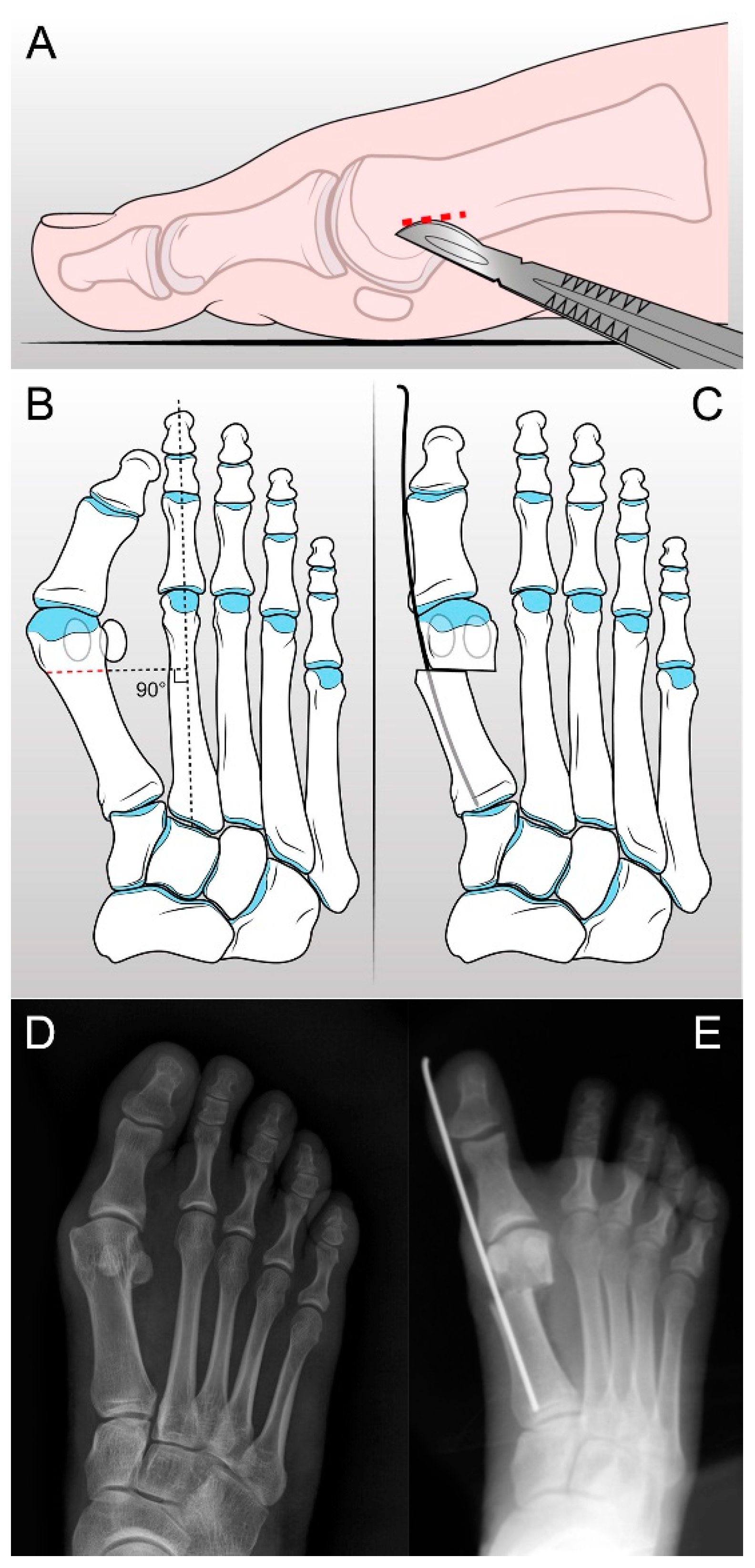
2.2. S.E.R.I. Operative Technique and Postoperative Management
2.3. Clinical and Radiological Assessments
2.4. PP Measurement
2.5. Statistical Analysis
3. Results
3.1. Population
3.2. Clinical and Radiological Results
3.3. Differences in Plantar Pressure Parameters before and after HV Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacob, H.A. Forces acting in the forefoot during normal gait—An estimate. Clin. Biomech. 2001, 16, 783–792. [Google Scholar] [CrossRef]
- Rodgers, M.M. Dynamic biomechanics of the normal foot and ankle during walking and running. Phys. Ther. 1988, 68, 1822–1830. [Google Scholar] [CrossRef]
- Myerson, M.S.; Badekas, A. Hypermobility of the first ray. Foot Ankle Clin. 2000, 5, 469–484. [Google Scholar] [PubMed]
- Coughlin, M.J.; Jones, C.P. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007, 28, 759–777. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Faldini, C.; Nanni, M.; Di Martino, A.; Luciani, D.; Vannini, F. A minimally invasive technique for surgical treatment of hallux valgus: Simple, effective, rapid, inexpensive (SERI). Int. Orthop. 2013, 37, 1805–1813. [Google Scholar] [CrossRef] [PubMed]
- Deschamps, K.; Birch, I.; Desloovere, K.; Matricali, G.A. The impact of hallux valgus on foot kinematics: A cross-sectional, comparative study. Gait Posture 2010, 32, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Hida, T.; Okuda, R.; Yasuda, T.; Jotoku, T.; Shima, H.; Neo, M. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J. Orthop. Sci. 2017, 22, 1054–1059. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Faldini, C.; Vannini, F.; Digennaro, V.; Bevoni, R.; Luciani, D. The minimally invasive osteotomy “S.E.R.I.” (simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int. 2008, 29, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Tsujinaka, S.; Shima, H.; Yasuda, T.; Mori, K.; Kizawa, M.; Togei, K.; Neo, M. Comparison of Plantar Pressure Distribution between Postoperative Hallux Valgus Feet and Healthy Feet. Foot Ankle Int. 2019, 40, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Verdu-Roman, C.; Sanz-Reig, J.; Martinez-Gimenez, E.; Carratala-Munuera, C.; Lopez-Pineda, A.; Quesada, J.A.; Gil-Guillen, V.F.; Orozco-Beltran, D. Plantar pressure improvement in moderate hallux valgus with modified chevron osteotomy: Clinical and radiographic outcomes. Foot Ankle Surg. 2020, 26, 205–208. [Google Scholar] [CrossRef]
- Brodsky, J.W.; Beischer, A.D.; Robinson, A.H.N.; Westra, S.; Negrine, J.P.; Shabat, S. Surgery for hallux valgus with proximal crescentic osteotomy causes variable postoperative pressure patterns. Clin. Orthop. Relat. Res. 2006, 443, 280–286. [Google Scholar] [CrossRef]
- Cancilleri, F.; Marinozzi, A.; Martinelli, N.; Ippolito, M.; Spiezia, F.; Ronconi, P.; Denaro, V. Comparison of plantar pressure, clinical, and radiographic changes of the forefoot after biplanar Austin osteotomy and triplanar Boc osteotomy in patients with mild hallux valgus. Foot Ankle Int. 2008, 29, 817–824. [Google Scholar]
- Kernozek, T.W.; Sterriker, S.A. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: Comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002, 23, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Schuh, R.; Hofstaetter, S.G.; Adams, S.B.; Pichler, F.; Kristen, K.-H.; Trnka, H.-J. Rehabilitation after hallux valgus surgery: Importance of physical therapy to restore weight bearing of the first ray during the stance phase. Phys. Ther. 2009, 89, 934–945. [Google Scholar] [CrossRef] [PubMed]
- Lorei, T.J.; Kinast, C.; Klärner, H.; Rosenbaum, D. Pedographic, clinical, and functional outcome after scarf osteotomy. Clin. Orthop. Relat. Res. 2006, 451, 161–166. [Google Scholar] [CrossRef] [PubMed]
- King, C.M.; Hamilton, G.A.; Ford, L.A. Effects of the lapidus arthrodesis and chevron bunionectomy on plantar forefoot pressures. J. Foot. Ankle Surg. 2014, 53, 415–419. [Google Scholar] [CrossRef]
- Bryant, A.R.; Tinley, P.; Cole, J.H. Plantar pressure and radiographic changes to the forefoot after the Austin bunionectomy. J. Am. Podiatr. Med. Assoc. 2005, 95, 357–365. [Google Scholar] [CrossRef]
- Saro, C.; Andrén, B.; Felländer-Tsai, L.; Lindgren, U.; Arndt, A. Plantar pressure distribution and pain after distal osteotomy for hallux valgus: A prospective study of 22 patients with 12-month follow-up. Foot 2007, 17, 84–93. [Google Scholar] [CrossRef][Green Version]
- Regnauld, B. The Foot: Pathology, Aetiology, Semiology, Clinical Investigation and Therapy; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Thong, I.S.K.; Jensen, M.P.; Miró, J.; Tan, G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scand J. Pain. 2018, 18, 99–107. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Saltzman, C.L.; Nunley, J.A. Angular measurements in the evaluation of hallux valgus deformities: A report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002, 23, 68–74. [Google Scholar]
- Claverie, L.; Ille, A.; Moretto, P. Discrete sensors distribution for accurate plantar pressure analyses. Med. Eng. Phys. 2016, 38, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Claverie, L.; Ille, A.; Moretto, P. Validation of a method for dispatching discrete sensors on an insole for plantar pressure analysis. Comput. Methods Biomech. Biomed. Eng. 2015, 18 (Suppl. S1), 1908–1909. [Google Scholar] [CrossRef] [PubMed]
- Pinloche, L.; Zhang, Q.; Berthouze, S.E.; Monteil, K.; Hautier, C. Physical ability, cervical function, and walking plantar pressure in frail and pre-frail older adults: An attentional focus approach. Front. Aging 2022, 3, 1063320. [Google Scholar] [CrossRef] [PubMed]
- Botín-Córdoba, J.A.; Oballe-Peinado, Ó.; Sánchez-Durán, J.A.; Hidalgo-López, J.A. Quasi Single Point Calibration Method for High-Speed Measurements of Resistive Sensors. Micromachines 2019, 10, 664. [Google Scholar] [CrossRef] [PubMed]
- Casado-Hernández, I.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Soriano-Medrano, A.; López-López, D.; Navarro-Flores, E.; Pérez-Boal, E.; Martínez-Jiménez, E.M. The Effectiveness of Hard Insoles for Plantar Pressure in Cycling: A Crossover Study. Bioengineering 2023, 10, 816. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Karim, H.; Wali, N.; Naraghi, R. The inter- and intra-rater reliability of the Maestro and Barroco metatarsal length measurement techniques. J. Foot Ankle Res. 2018, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Cavallo, M.; Faldini, C.; Luciani, D.; Vannini, F. The SERI distal metatarsal osteotomy and Scarf osteotomy provide similar correction of hallux valgus. Clin. Orthop. Relat. Res. 2013, 471, 2305–2311. [Google Scholar] [CrossRef] [PubMed]
- Rocca, G.; De Venuto, A.; Mazzotti, A.; Zielli, S.O.; Artioli, E.; Brognara, L.; Traina, F.; Faldini, C. The Minimally Invasive SERI Osteotomy for Pediatric Hallux Valgus. Children 2023, 10, 94. [Google Scholar] [CrossRef]
- Almalki, T.; Alatassi, R.; Alajlan, A.; Alghamdi, K.; Abdulaal, A. Assessment of the efficacy of SERI osteotomy for hallux valgus correction. J. Orthop. Surg. Res. 2019, 14, 28. [Google Scholar] [CrossRef]
- Brognara, L.; Mazzotti, A.; Arceri, A.; Artioli, E.; Casadei, G.; Bonelli, S.; Traina, F.; Faldini, C. Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures. Diseases 2023, 11, 57. [Google Scholar] [CrossRef] [PubMed]
- Abdul Razak, A.H.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot Plantar Pressure Measurement System: A Review. Sensors 2012, 12, 9884–9912. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Muneta, T.; Asahina, S.; Furuya, K. Forefoot pressures during walking in feet afficted with hallux valgus. Clin. Orthop. Relat. Res. 1996, 323, 247–253. [Google Scholar] [CrossRef]
- Nyska, M.; Liberson, A.; McCabe, C.; Linge, K.; Klenerman, L. Plantar foot pressure distribution in patients with Hallux valgus treated by distal soft tissue procedure and proximal metatarsal osteotomy. Foot Ankle Surg. 1998, 4, 35–41. [Google Scholar] [CrossRef]
- Mazzotti, A.; Arceri, A.; Martini, B.; Bonelli, S.; Zielli, S.; Artioli, E.; Brognara, L.; Faldini, C. Hallux Valgus Plantar Pressure Distribution before and after Surgery. J. Am. Podiatr. Med. Assoc. 2023, 113, 22–177. [Google Scholar] [CrossRef] [PubMed]
- Orlin, M.N.; McPoil, T.G. Plantar pressure assessment. Phys. Ther. 2000, 80, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Monteagudo, M.; Martínez-de-Albornoz, P. Management of Complications after Hallux Valgus Reconstruction. Foot Ankle Clin. 2020, 25, 151–167. [Google Scholar] [CrossRef]
- Biz, C.; Corradin, M.; Kuete Kanah, W.T.; Dalmau-Pastor, M.; Zornetta, A.; Volpin, A.; Ruggieri, P. Medium-Long-Term Clinical and Radiographic Outcomes of Minimally Invasive Distal Metatarsal Metaphyseal Osteotomy (DMMO) for Central Primary Metatarsalgia: Do Maestro Criteria Have a Predictive Value in the Preoperative Planning for This Percutaneous Technique? BioMed Res. Int. 2018, 2018, 1947024. [Google Scholar]
- Togei, K.; Shima, H.; Yasuda, T.; Tsujinaka, S.; Nakamura, G.; Neo, M. Plantar pressure distribution in hallux valgus feet after a first metatarsal proximal crescentic osteotomy with a lesser metatarsal proximal shortening osteotomy. Foot Ankle Surg. 2021, 27, 665–672. [Google Scholar] [CrossRef]
- Vandeputte, G.; Dereymaeker, G.; Steenwerckx, A.; Peeraer, L. The Weil Osteotomy of the Lesser Metatarsals: A Clinical and Pedobarographic Follow-up Study. Foot Ankle Int. 2000, 21, 370–374. [Google Scholar] [CrossRef]


| Patients | 15 (24 Halluces) |
|---|---|
| Side | 2 left, 4 right, 9 bilateral |
| Age | 53.9 ± 17.3 (18–78) |
| Gender | 14 F/1 M |
| BMI | 24.1 ± 3.2 |
| Baseline | Follow-Up (12 Months) | p-Value | |
|---|---|---|---|
| AOFAS | 46.7 ± 15.6 | 84.8 ± 15.2 | <0.001 * |
| Pain | 20.8 ± 10.8 | 36.7 ± 6.5 | <0.001 * |
| Function | 21.4 ± 8.8 | 34.3 ± 8.7 | <0.001 * |
| Alignment | 4.5 ± 6.0 | 13.8 ± 2.7 | <0.001 * |
| NRS | 6.4 ± 1.3 | 2.2 ± 2.4 | <0.001 * |
| IMA | 12.9° ± 2.2 | 5.6° ± 2.2 | <0.001 * |
| HVA | 34.1° ± 7.2 | 11.4° ± 3.8 | <0.001 * |
| Peak-P | Baseline | Follow-Up (12 Months) | p-Value |
|---|---|---|---|
| Region 1 | 773.1 ± 663.5 (66.2–2148.2) | 1088.8 ± 236.7 (582.7–1545.5) | 0.027 * |
| Region 2 | 552.2 ± 256.7 (139.4–1290.5) | 844.1 ± 317.6 (260.8–1424.5) | 0.005 * |
| Region 3 | 714.71 ± 366.6 (118.5–1483.2) | 999.6 ± 383.1 (345.6–1858.1) | 0.024 * |
| Region 4 | 515.9 ± 402.8 (67.0–1586.1) | 631.7 ± 304.8 (31.7–1267.9) | 0.266 |
| Region 5 | 264.8 ± 316.0 (35.6–1419.3) | 415.7 ± 324.5 (0.5–1153.4) | 0.107 |
| Region 6 | 134.7 ± 166.5 (14.4–779.9) | 162.4 ± 128.8 (37.2–479.9) | 0.474 |
| Region 7 | 116.3 ± 195.7 (0.7–732.4) | 78.0 ± 121.8 (0.4–454.4) | 0.472 |
| Region 8 | 516.7 ± 274.3 (145.4–1293.2) | 528.9 ± 305.9 (13.0–1136.8) | 0.896 |
| Region 9 | 269.7 ± 280.9 (1.2–1158.2) | 228.6 ± 212.6 (1.2–926.5) | 0.394 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzotti, A.; Arceri, A.; Artioli, E.; Langone, L.; Zielli, S.O.; Martini, B.; Traina, F.; Faldini, C.; Brognara, L. Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy. J. Clin. Med. 2024, 13, 1731. https://doi.org/10.3390/jcm13061731
Mazzotti A, Arceri A, Artioli E, Langone L, Zielli SO, Martini B, Traina F, Faldini C, Brognara L. Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy. Journal of Clinical Medicine. 2024; 13(6):1731. https://doi.org/10.3390/jcm13061731
Chicago/Turabian StyleMazzotti, Antonio, Alberto Arceri, Elena Artioli, Laura Langone, Simone Ottavio Zielli, Beatrice Martini, Francesco Traina, Cesare Faldini, and Lorenzo Brognara. 2024. "Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy" Journal of Clinical Medicine 13, no. 6: 1731. https://doi.org/10.3390/jcm13061731
APA StyleMazzotti, A., Arceri, A., Artioli, E., Langone, L., Zielli, S. O., Martini, B., Traina, F., Faldini, C., & Brognara, L. (2024). Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy. Journal of Clinical Medicine, 13(6), 1731. https://doi.org/10.3390/jcm13061731












