Abstract
Background: Anterior cervical discectomy and fusion (ACDF) is a standard procedure for degenerative diseases of the cervical spine, providing nerve decompression and spinal stabilization. However, it limits cervical spine motility, restricts fused segment activity, and may lead to adjacent degeneration. Cervical disc arthroplasty (CDA) is an accepted alternative that preserves the structure and flexibility of the cervical spine. This study aimed to explore the dynamic changes in the range of motion (ROM) of the cervical spine after CDA using a viscoelastic artificial disc, as well as the factors affecting mobility restoration. Methods: A retrospective analysis was conducted on 132 patients who underwent single-level anterior cervical discectomy and CDA from January 2015 to June 2022. Result: Analysis of data from 132 patients revealed a significant improvement in clinical outcomes. The mean ROM of C2–C7 and functional spinal unit (FSU) segments significantly increased from 2 to 36 months post-operatively. Cervical spine flexibility was preserved and enhanced after prosthesis implantation. However, it took six months for the cervical spine motility to stabilize. In addition, sex and age were found to impact motility restoration, with female and younger patients exhibiting larger ROMs post-surgery. Additionally, CDA at the C5–C6 level resulted in the greatest increase in ROM, potentially improving overall kinematic ability. Conclusions: Single-segment artificial disc arthroplasty effectively restores the ROM in degenerative cervical spine conditions.
1. Introduction
The cervical spine in humans serves not only to support the weight of the head but also to facilitate multi-directional activities. As we age, the flexibility of the cervical spine decreases, which may lead to degenerative diseases [1]. These conditions, such as disc herniation, narrowed foramina, osteophyte formation, and endplate sclerosis, can potentially cause cervical myelopathy or radiculopathy [2]. Among these, cervical disc herniation is the most common degenerative cervical disease, particularly affecting individuals over 40 years of age [3].
Surgical intervention becomes an option for patients whose symptoms and neurological deficits cannot be alleviated by non-invasive or minimally invasive treatments [4,5]. Anterior cervical discectomy and fusion (ACDF) has been widely adopted as the gold standard treatment for cervical disc herniation and was first described in 1958 by Smith and Robinson. However, the fusion-based reconstructive procedures used in ACDF sacrifice the motility of the cervical spine and may result in future adjacent degenerative diseases. Therefore, numerous dynamic cervical implants have been developed since 2002, with several studies highlighting the benefits and complications of these devices [6,7].
Cervical disc arthroplasty (CDA) has gained acceptance as a reliable surgical alternative over the past decade [8]. The superiority of CDA over ACDF has been demonstrated by randomized controlled trials, with advantages including higher long-term clinical success rates, improved motion flexibility, reduced incidence of adjacent syndrome, lower reoperation rates, and shorter hospital stays [9,10,11,12]. In a recent systematic review evaluating the cost effectiveness of CDA and ACDF, the findings suggested that CDA may be a more cost-effective treatment approach [13].
The existing literature highlights the benefit of CDA in restoring the physiological biomechanical properties of the cervical spine [14,15,16]. Range of motion (ROM), which reflects cervical flexibility, is a well-studied biomechanical parameter for evaluating motion preservation. However, there is still a lack of comprehensive understanding regarding the dynamic changes in ROM after CDA with a viscoelastic artificial disc, particularly those that provide motion in 6 degrees of freedom (6-DOF). These new-generation prostheses are expected to resemble natural discs and hold promise for future CDA procedures [17].
The present study was designed as a three-year follow-up to investigate the mobility of the cervical spine after arthroplasty with a semi-constrained cervical disc prosthesis (Baguera®C, Spineart Geneva SA, Geneva, Switzerland). By analyzing the changes in ROM, which was measured by radiographic outcomes, this retrospective study aimed to elucidate whether age, sex, and operative level had an impact on mobility restoration after CDA with a viscoelastic disc.
2. Materials and Methods
2.1. Study Design and Patient Population
This study conducted a retrospective analysis of patients who underwent single-level anterior cervical discectomy and cervical disc arthroplasty (CDA) from January 2015 to June 2022 at our institute. All patients had cervical degenerative diseases with radiculopathy and/or myelopathy and underwent surgeries by the same surgeon. A total of 132 patients (60 males and 72 females) were enrolled in the study. The ages of the patients ranged from 32 to 88 years, with a mean age of 58.03 years at the time of surgery. The minimum follow-up period was six months.
The inclusion criteria specified that patients must have symptomatic cervical disc disease at a single level between C3–C4 and C6–C7. Conservative treatments had failed for all patients with herniated discs or bony osteophytes, as observed in their magnetic resonance imaging studies. The exclusion criteria comprised osteoporosis, rheumatoid arthritis or other autoimmune diseases, ossification of the posterior longitudinal ligament, active infection, structural instability, disc space collapse, known allergy to titanium, neoplasia, and metabolic bone diseases. All patients included in this study provided informed consent by accepting and signing a consent form. This study was approved by the Institutional Review Board of Shin Kong Wu Ho-Su Memorial Hospital (approval code: 20200202R) before data collection and analysis.
2.2. Device Description
All patients underwent CDA using the Baguera®C prosthesis (Spineart Inc., Plan-Les-Ouates, Switzerland), which enables motion in 6-DOF. The Baguera®C is a semi-constrained cervical disc prosthesis consisting of a high-density polyethylene nucleus that serves as an articulation between two titanium endplate components. It has a porous coated exterior and a diamond-like carbon-coated interior, as well as three fins on each endplate, providing immediate stability after implantation.
2.3. Surgical Procedures
The surgical procedure involved a modified Smith-Robinson anterior approach to the cervical spine. The same neurosurgeon performed the procedures for all 132 of the patients. The patient was placed in a supine position on the operating table with a soft pad placed under the shoulder to slightly extend the neck. A transverse skin incision of 2.5 cm was made on either the right or left side of the neck, depending on the laterality of the patient’s symptoms. Through this incision, the target level was reached and confirmed using intra-operative lateral fluoroscopy. A self-retractor was used to push the trachea and esophagus across the midline to the opposite direction and the carotid sheath laterally, exposing the anterior border of the cervical spine.
Discectomy was performed, removing all cartilaginous endplates, hard spurs, and the disc itself. The posterior longitudinal ligaments were opened in all cases to ensure sufficient decompression. Bilateral uncovertebral joints (Luschka’s joints) were also released. A properly sized Baguera®C cervical prosthesis was then implanted into the intervertebral space, guided by lateral fluoroscopy. An implant with dimensions close to the original disc space was selected. Any bone dust was irrigated out with regular saline, and bone edges were sealed with bone wax. The wound was closed in layers, and no drainage tube was left. Patients were able to move independently immediately after recovering from anesthesia. The use of a cervical collar post-operatively was not necessary. Patients were allowed to attempt oral intake on the same day. After a review by the medical team, they could be discharged on post-operative day 2 or 3.
2.4. Clinical Evaluation
All patients diagnosed with single-level cervical herniated disc disease underwent a comprehensive neurological examination and completed an extensive questionnaire that included the Visual Analogue Scale (VAS) to assess pain in the neck and limbs, the Neck Disability Index (NDI) to evaluate disability, and the Japanese Orthopedic Association (JOA) score. These assessments were conducted both pre-operatively and on post-operative day 2 or 3.
2.5. Radiological Evaluation
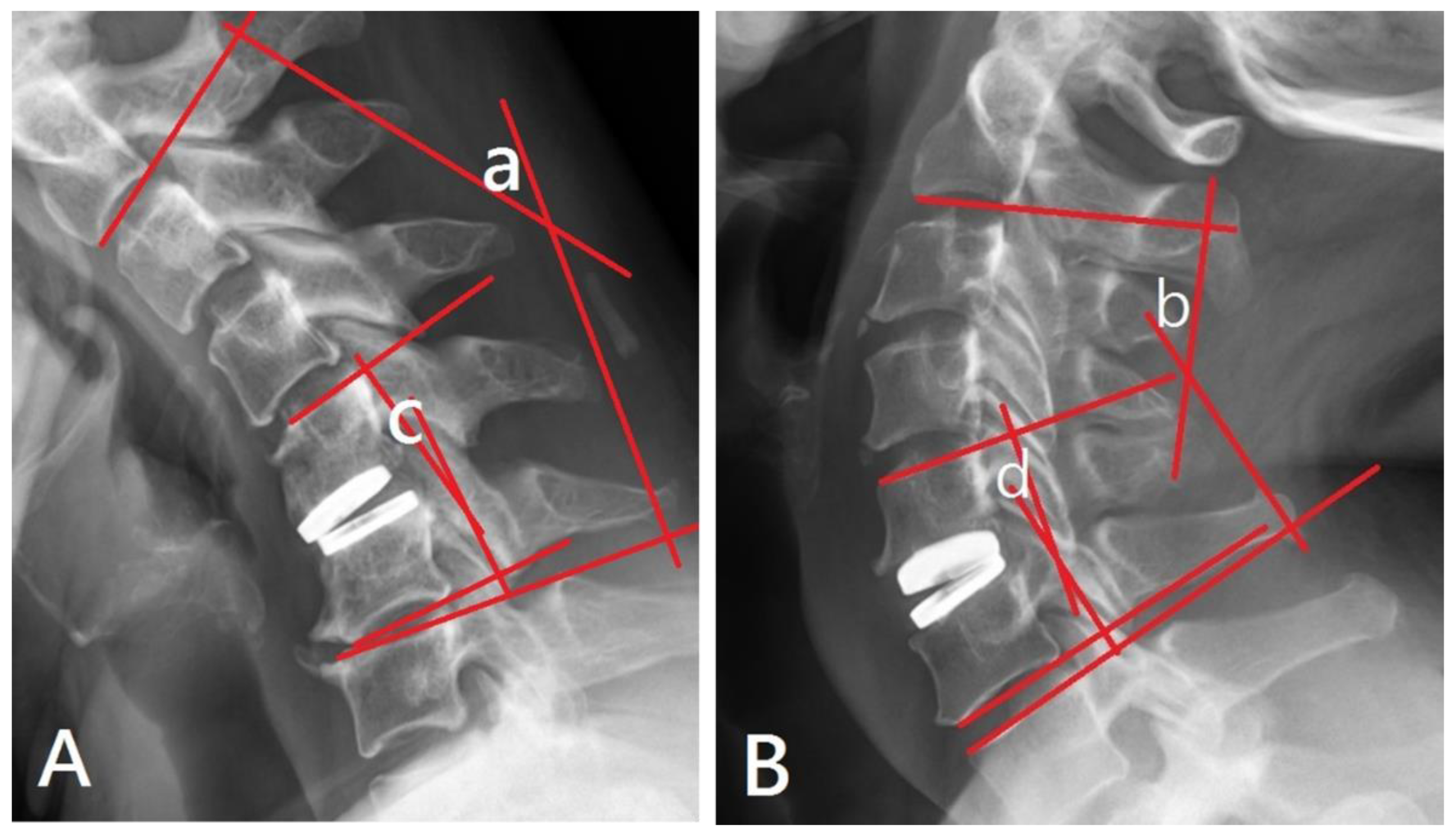
To evaluate the ROM of the cervical spine, dynamic studies were conducted to assess its motility. The ROM of the C2–C7 segment represents the overall motility of the entire cervical spine, while the ROM of the functional spinal unit (FSU), a combination of two adjacent vertebrae and the intervertebral disc, represents the motility specific to the CDA procedure.
The angles between the superior endplate of the upper vertebra and the inferior endplate of the lower vertebra were measured using Cobb’s technique on flexion and extension lateral cervical radiographs [18]. The sum of these two angles provided the ROM of the measured vertebrae. The ROM of C2–C7 extended from the inferior endplate of C2 to the superior endplate of C7, while the ROM of the FSU spanned from the superior endplate of the upper vertebra to the inferior endplate of the lower vertebra at the level of the lesioned disc (Figure 1).
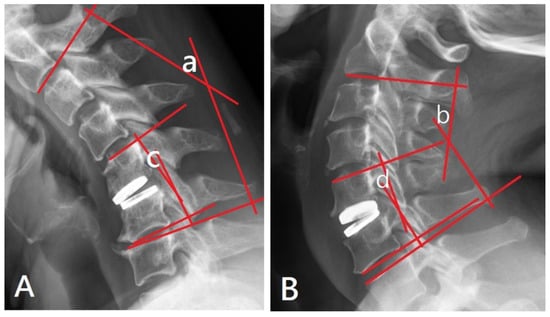
Figure 1.
(A) (flexion view) and 1 (B) (extension view): Evaluation of the ROM of C2–C7 and FSU using flexion and extension lateral cervical radiographs. The angle of “a+b” represents the ROM of C2–C7. The angle of “c+d” represents the ROM of FSU.
Cervical spine radiographs in the anterior–posterior and lateral projections were taken on post-operative day 1 to assess the location of the implant. Dynamic studies, consisting of flexion and extension views in lateral projection radiographs, were performed at specific intervals (1 week, 1 month, 2 months, 3 months, 6 months, 12 months, 18 months, 24 months, and 36 months) to evaluate the motility of the cervical spine. To ensure consistency and minimize observer bias, two independent technicians evaluated the radiographs and calculated the angles to determine the ROM.
2.6. Radiological Evaluation
Statistical analyses were performed using SPSS version 26 (SPSS Inc., Chicago, IL, USA). The data were presented as mean ± SD. Comparisons between the two groups were performed using the Mann–Whitney U test, paired t-test, or Chi-square test. One-way analysis of variance (ANOVA) was used to compare the ROMs during the pre-operation period and the follow-up periods. To evaluate the effects of two different factors and their interaction, the general linear model (GLM) univariate analysis was employed. p values were set at p ≤ 0.05 to determine statistical significance.
3. Results
A total of 132 patients (60 females and 72 males) who underwent single-level surgery between January 2015 and June 2022 were included in this study. The surgical levels at which the patients underwent the procedure were C3–C4 (n = 25), C4–C5 (n = 15), C5–C6 (n = 50), and C6–C7 (n = 42). No significant differences between sexes were found at baseline (Table 1) with respect to age, mean pre-operative VAS scores, and ROM of the FSU and overall cervical spine (C2–C7).

Table 1.
Comparison of age, VAS, and angles of ROM by sex at baseline (n = 132)
3.1. Clinical Outcomes
Cervical disc arthroplasty surgery resulted in significant improvements in clinical outcomes, as evidenced by decreased VAS scores and NDI, and increased JOA scores (Table 2).

Table 2.
Comparison of VAS, NDI, and JOA at pre-operation and post-operation stages (n = 132).
3.2. Radiological Evaluation
Radiological evaluations were conducted on each patient before surgery and at regular post-operative intervals (1 week, 1 month, 2 months, 3 months, 6 months, 12 months, 18 months, 24 months, and 36 months) for a period of three years. All patients completed the radiological evaluations, resulting in a follow-up rate of 100%.
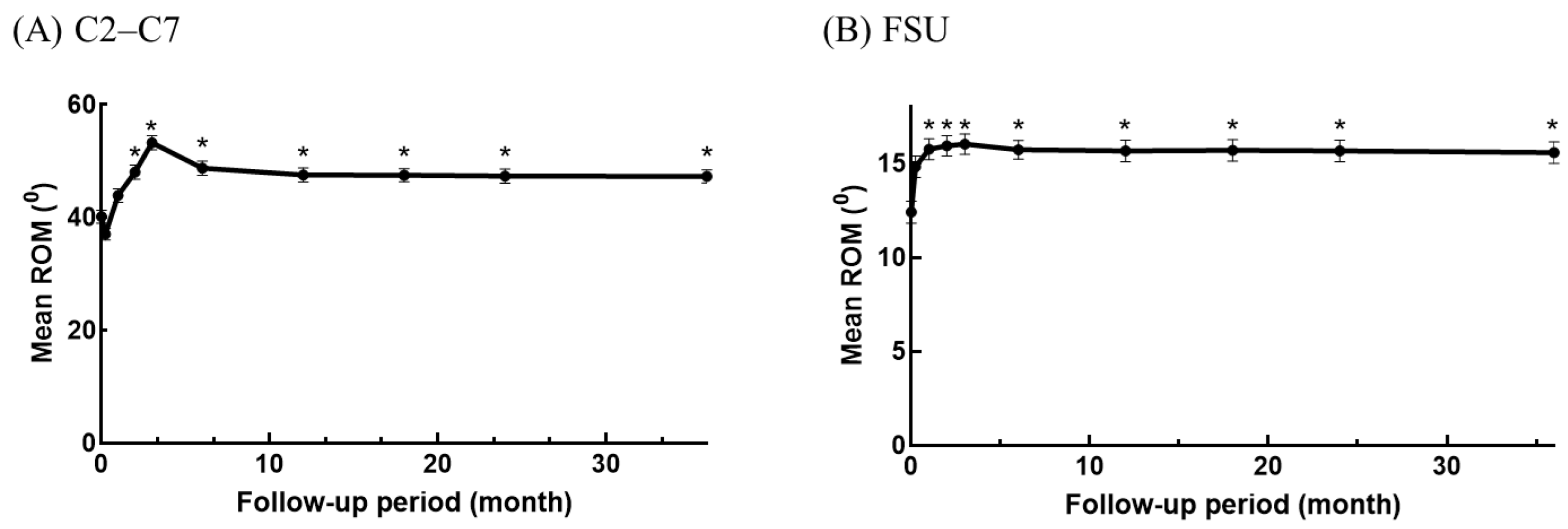
3.2.1. Improvement in ROM
The ROM showed significant improvement, indicating enhanced mobility of the cervical spine. Prior to surgery, the mean ROM for C2–C7 was 40.17° ± 13.37°, and for the FSU, it was 12.41° ± 6.77°. At the 36-month follow-up, these values increased to 47.31° ± 13.18° and 15.58° ± 6.52°, respectively. Compared with the pre-operative period, statistically significant upregulation of ROM for the FSU and C2–C7 was observed post-operatively from the 2-month follow-up and continued throughout the 36-month follow-up period.
The highest mean ROM values were recorded at the 3-month follow-up (overall cervical spine: 53.3°, FSU: 16.02°). The ROM of the FSU remained well-maintained with less than 1° difference at any point from the 3-month throughout the 36-month follow-up. Although the mean ROM of the overall cervical spine slightly decreased at the 6-month follow-up (48.76°), the difference was not statistically significant compared to the 3-month follow-up. Subsequently, the ROM remained stable with a difference of less than 1.5° throughout the remaining follow-up period (Figure 2).
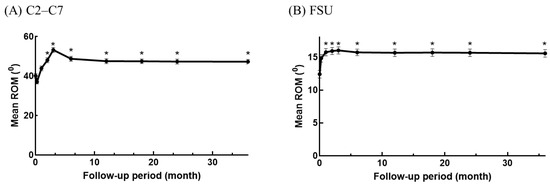
Figure 2.
Dynamic changes in ROM of C2–C7 (A) and FSU (B). * p ≤ 0.05 compared to pre-operative baseline. The point on the y-axis is the ROM of the pre-operative period.
Compared to the pre-operative baseline measurements, the ROM of both C2–C7 and FSU increased significantly from the 2-month follow-up and continued throughout the 36-month follow-up. The radiological findings indicated that the ROM of both C2–C7 and FSU remained significantly improved from the 2-month follow-up to the last follow-up, suggesting sustained improvement over time. To further explore the factors influencing the improvement in cervical motility, longitudinal data were analyzed to examine the potential impact of age, sex, and the operated segment.
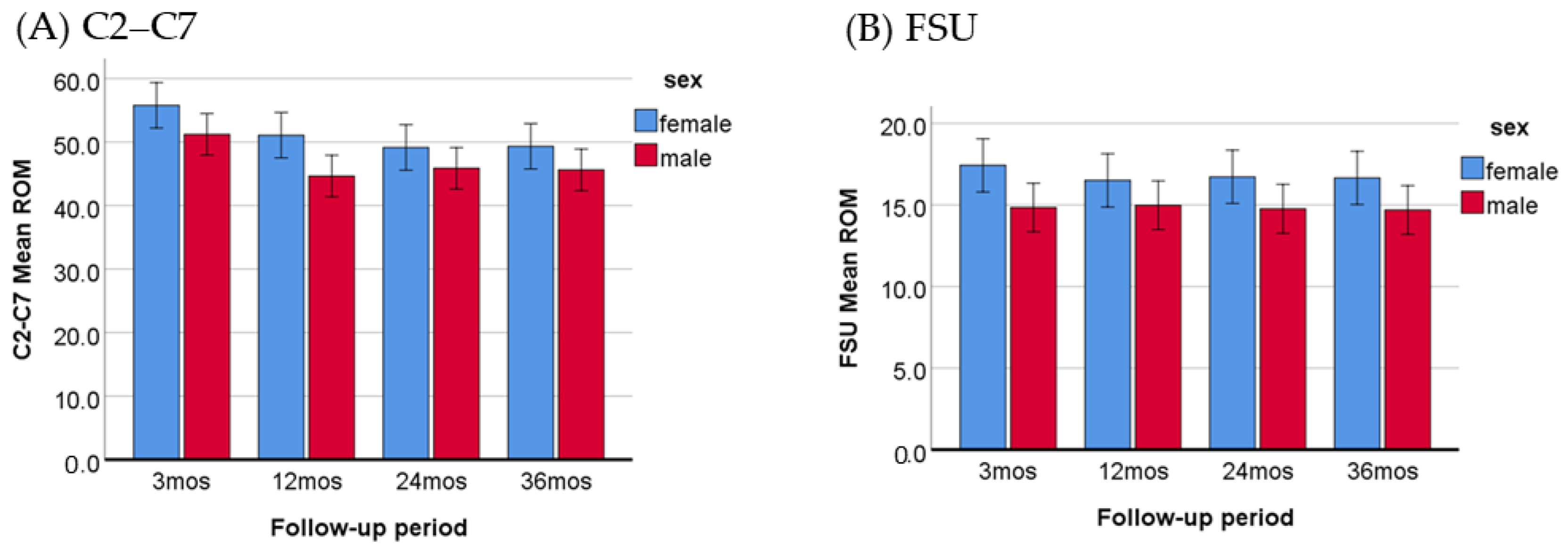
3.2.2. Comparing the Improvement in ROM between Males and Females
To evaluate potential differences in post-operative ROM between males and females, the ROM measurements at the 3-, 12-, 24-, and 36-month follow-ups were analyzed. As presented in Table 3 and Figure 3, the ROM of C2–C7 and FSU both increased significantly in females compared to males. Additionally, no interaction was observed between the time intervals and sex groups, indicating that the ROM improvements were consistent across the follow-up periods for both sexes.

Table 3.
Comparison of ROM by time interval and sex within 3–36 months post-operatively (Females = 60, Males = 72).
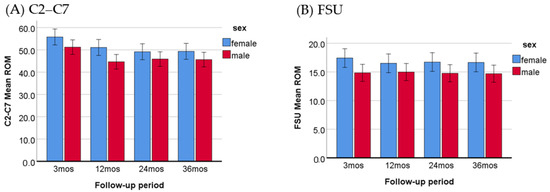
Figure 3.
Comparison of C2–C7 (A) and FSU (B) ROM between females and males within 3–36 months post-operatively, with a p-value less than 0.001 for both ROM.
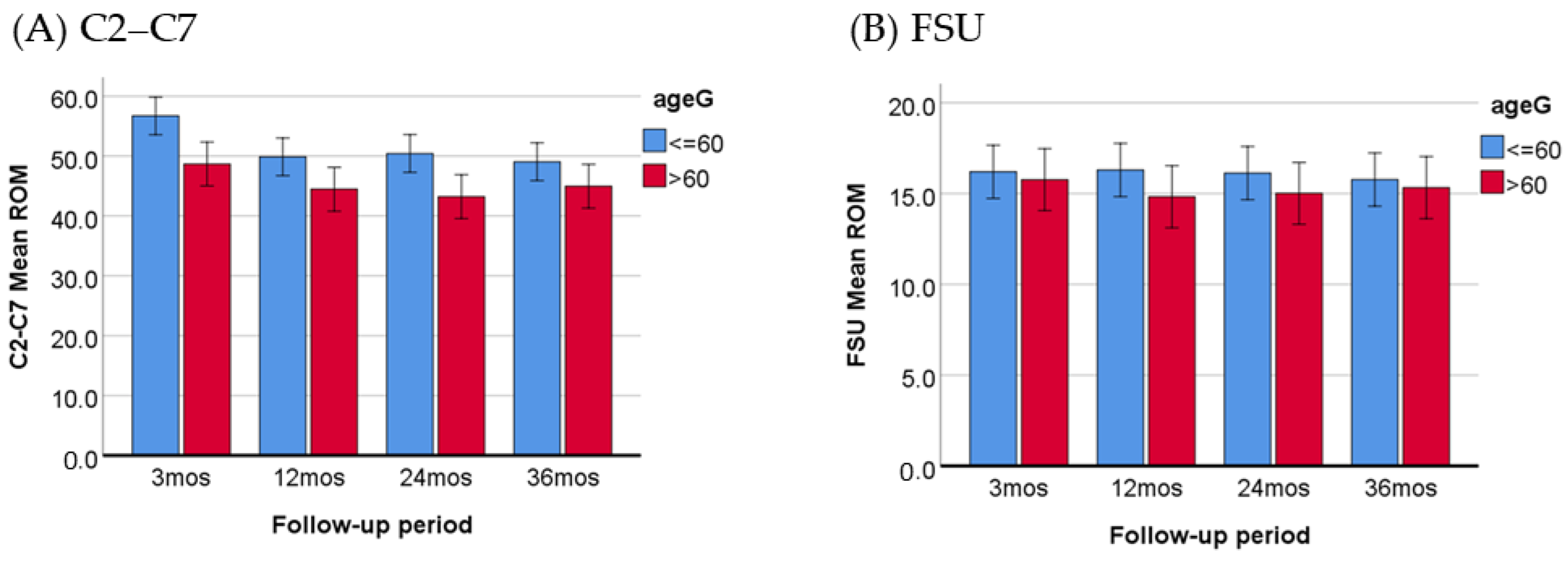
3.2.3. Comparing the Improvement in ROM between Older and Younger Patients
This study aimed to investigate whether age has an impact on the improvement in post-operative ROM. For the purpose of our analysis, we defined individuals aged 60 years or older as the “older adults” group, ensuring a relatively equal distribution of patients in both age groups (≤60, n = 76; >60, n = 56). The ROM measurements at the 3-, 12-, 24-, and 36-month follow-ups were analyzed. The mean pre-operative ROM of C2–C7 was 41.96 ± 13.73 (≤60 group) and 37.74 ± 12.57 (>60 group), showing no significant difference between the two groups (p = 0.072). However, there was a significant difference in the pre-operative ROM of the FSU, with values of 13.44 ± 7.49 (≤60 group) and 11.01 ± 5.41 (>60 group) (p = 0.042). Notably, the age difference was only observed in the ROM of C2–C7 after surgery, and there was no interaction between time and age groups (Table 4, Figure 4).

Table 4.
Comparison of ROM by time and age group within 3–36 months post-operatively (≤60, n = 76, >60, n = 56).
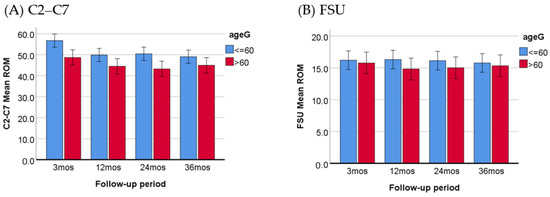
Figure 4.
Comparison of C2–C7 (A) and FSU (B) ROM between younger patients and older patients within 3–36 months post-operatively, with a p-value less than 0.001 for C2–C7 ROM.
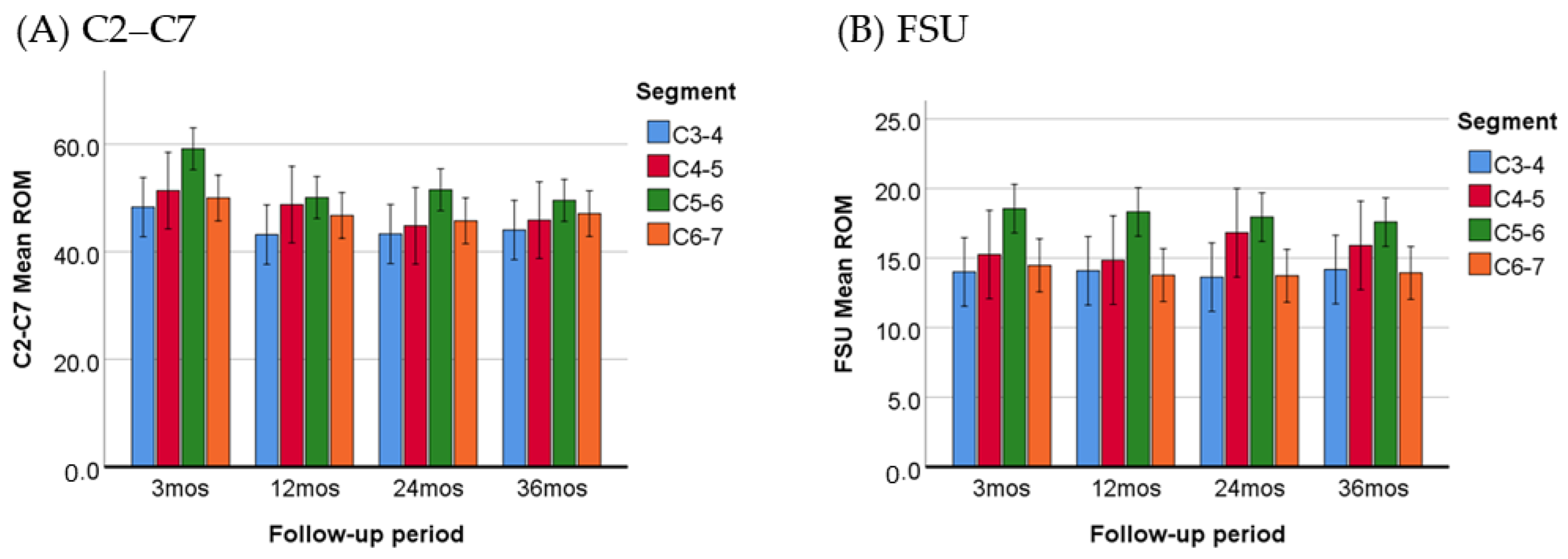
3.2.4. Comparing the Improvement in ROM between Patients with Different Levels of Surgery
The ROM was evaluated at various time intervals, including the 3-, 12-, 24-, and 36-month follow-ups. The results, presented in Table 5 and Figure 5, indicate that the increase in ROM was most pronounced in patients who were operated at the C5–C6 level. The ROM for both C2–C7 and FSU were significantly larger (p ≤ 0.05) than the other segments, with the exception of the ROM for C2–C7 at the C4–C5 operated level (p = 0.117).

Table 5.
Comparisons of mean ROM by operated level within 3–36 months post-operatively.
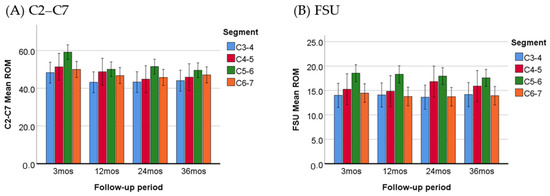
Figure 5.
Comparison of C2–C7 (A) and FSU (B) ROM between patients treated on different segments. The increase in ROM was most pronounced in patients who were operated at the C5–C6 level.
In addition, heterotopic ossification (HO), which refers to the abnormal formation of bone tissue growing into the disc space and partially blocking the ROM, was found in 11 of the 132 patients (8.3%) at the final follow-up.
4. Discussion
The patient cohort examined in the current study demonstrated significant improvements in all clinical outcome parameters (NDI, VAS, and JOA) in comparison to baseline levels. Previous studies have also verified similar favorable clinical outcomes at different observation periods, irrespective of the type of prosthesis implanted [19,20,21,22]. It has been suggested that higher pre-operative NDI scores are associated with a more pronounced C2–C7 sagittal vertical axis and reduced cervical lordosis [23]. Following surgical reconstruction, which led to a decrease in NDI and VAS scores, CDA not only alleviates pain but also restores sagittal balance in the cervical spine.
A literature review has revealed that CDA preserves the motility of the cervical spine, especially at these operative levels [24,25,26]. However, there are inconsistent findings in clinical trials using different types of prostheses and varying follow-up periods regarding changes in ROM before and after surgery [27,28,29,30]. A study cohort using Baguera®C, which is the same type of prosthesis used in this study, reported a non-significant decrease in mean ROM of the FSU and a non-significant increase in ROM of C2–C7 two years after surgery [31]. A recent study on the longitudinal changes in ROM at the operated segments following CDA with the Mobi-C prosthesis, a semi-constrained artificial disc classified under the same category as the artificial disc used in our study, found a significant decrease in ROM starting 24 months after the operation [32].
In the present study, the mean ROM of C2–C7 and FSU increased at all follow-up points, with the exception of the ROM of C2–C7 at the first follow-up (one week after surgery). This temporary decrease was attributed to discomfort caused by the non-healing wound, which affected the patient’s ability to extend and flex their neck. All ROM upregulations were statistically significant in comparison to baseline levels from 2 months post-operatively to the final follow-up (Figure 1). The ROM remained relatively stable after the 6-month follow-up, indicating that the improved flexibility of the operated segment and the cervical spine was preserved well by the implanted viscoelastic prosthesis.
Additionally, this finding demonstrates that the stability of the motor function after intervertebral disc replacement requires a 6-month period of adaptation before reaching a stable plateau. Therefore, a 6-month follow-up is sufficient to assess the influence of CDA on cervical spine motility. The substantial improvement observed for three years after CDA, as well as the low ratio of HO in our cases, may be attributed to specific surgical techniques employed in this study. These techniques involved the decompression of bilateral Luschka’s joints (uncovertebral joints), thorough normal saline irrigation to remove bone dust, and the use of bone wax to seal bone edges after implantation.
Sex plays an influential role in determining the total ROM in the cervical spine of asymptomatic individuals, with females generally exhibiting significantly larger ROM compared to males [33,34]. In our patient cohort, no significant sex differences in ROM were observed at the baseline assessment (Table 1). However, the post-operative ROM of the total cervical spine and FSU increased significantly in females compared to males (Table 3, Figure 3). This finding suggests that the reconstruction of degenerative levels in female patients may lead to better cervical motility restoration, resulting in significantly larger ROM, which is in line with observations in the asymptomatic population. Thus, even after surgery, females are able to retain their innate advantages in cervical motility. In contrast to our study, Wu, T.K. et al. reported that sex and age did not have a significant effect on post-operative ROM [21]. Their study enrolled patients who underwent 1-level CDA (48.41%) and 2-level CDA (51.59%). The higher complexity of the study population may interfere with the analysis results.
The total cervical ROM tends to decrease with increasing age, primarily caused by the degeneration of the intervertebral discs [34,35]. In our study, the patients were divided into two groups: older (>60 years old) and younger patients (≤60 years old). Prior to surgery, there was no significant difference in the total cervical ROM between the two groups. This lack of difference may be due to neck pain or stiffness, which could limit the motility of the cervical spine. However, the post-operative ROM of the C2–C7 segment increased in both groups, but the values of ROM were significantly larger in the younger group (Table 4), indicating that the flexibility of the cervical spine was markedly improved by the implanted viscoelastic prosthesis in young individuals. Therefore, single-segment CDA appears to be particularly beneficial for younger patients.
It is noteworthy that the pre-operative ROM of the FSU at the operated level was significantly smaller in the older group, but this difference became non-significant after the implantation of the prosthesis (Table 4). A radiographic assessment performed on 212 asymptomatic volunteers found that age has a significant negative association with segmental ROM at all cervical levels, with segmental ROM decreasing at the degenerated disc levels [33]. The non-significant post-operative difference indicates that our patients, regardless of their age, were able to preserve segmental motility well after receiving the prosthesis replacement at the diseased segment. On the other hand, a comparative study found that younger patients (≤40 years old) had a significant post-operative segmental ROM than elderly patients (≥65) [36]. The reason for the disparity between this study’s findings and our own should be attributed to differences in the study cohort and prosthesis implanted.
Given the distinct differences in motion characteristics among different segments of the cervical spine during neck motion [37], it is expected that the outcomes of patients with implants at different levels would vary in terms of cervical motility. Although there was no significant difference in the pre-operative ROM of the C2–C7 segment among patients with different operative levels, the analysis of the longitudinal changes in ROM from three months to three years post-operatively revealed that the most significant increase in ROM occurred in patients treated at the C5–C6 level (Table 5, Figure 5). These patients demonstrated the greatest improvement in cervical spine flexibility post-operatively. Biomechanical and kinematic investigations have shown that the C5–C6 motion segment exhibits the maximum ROM for flexion/extension motion in healthy young adults [38]. Furthermore, a single-level degenerative condition at the C5–C6 segment leads to a substantial decrease of approximately 32% in flexion and 33% in extension in segmental ROM [15]. Moreover, in symptomatic patients with severely degenerated segments, the contribution of the C5–C6 motion segment to the total angular ROM decreases significantly [39]. Unfortunately, C5–C6 is one of the most commonly affected levels in degenerative disc disease. This indicates that degenerative cervical diseases affect the C5–C6 level frequently. After CDA at the diseased C5–C6 level, the function of the C5–C6 motion segment could be restored, and so could the contribution to ROM. It is rational to expect that patients treated at the C5–C6 level would have better post-operative ROM than others. According to our findings, patients who were operated at the C5–C6 level experienced the most significant improvement in ROM. The motility restoration in the C5–C6 motor segment appears to elevate the overall kinematic ability of the cervical spine more effectively than other segments.
While CDA is a more physiological surgical option for cervical degenerative diseases compared to ACDF, its high medical expenses limit its widespread adoption. For patients with multi-level cervical degenerative diseases, some surgeons have advocated for hybrid surgeries, which combine fusion and non-fusion procedures, as a cost-effective alternative for replacing diseased cervical discs [40]. Considering the pivotal role of the C5–C6 level in cervical spine motility, whether it is through single-segment CDA or hybrid surgeries, the replacement of the C5–C6 disc with an artificial disc proves to be the most cost-effective approach and should be given the highest priority in terms of restoring cervical spine ROM.
In addition, HO is a common post-operative complication in cervical spine arthroplasty, with reported incidences ranging from 5% to 63%. The occurrence of HO can vary depending on the type of prosthesis used and the length of the follow-up period [41,42]. HO may have a significant impact on the motility of the cervical spine after CDA, particularly in cases classified as McAfee’s class III and IV, where the ROM is severely restricted [41]. This suggests that the motility of the cervical spine may be preserved in cases classified as class 0 to II. Furthermore, it is challenging to evaluate the grading of HO accurately using plain radiographs alone. In our study, the occurrence of HO was approximately 8.3%. However, it is possible that this figure may be underestimated, and the incidence may increase with further long-term follow-up.
A survey estimating the incidence of cervical spine surgery from 2020 to 2040 in the United States predicts an increase in cervical spinal disease and a subsequent rise in surgical volumes in the near future [43]. Given the allowance for 6-DOF motion, viscoelastic devices have been recommended as ideal artificial discs that resemble the physiological motion patterns of natural discs [44]. The results of this study provide valuable insights into the changes in ROM that occur over a three-year period following CDA with a viscoelastic device. It highlights the significance of the C5–C6 segment for cervical spine ROM and suggests that a 6-month adaptation period is required to reach a stable ROM status. Single-segment artificial disc replacement had the potential to restore ROM in the cervical spine. However, additional prospective investigations with longer follow-ups are warranted to gain a deeper understanding of the precise motion characteristics of viscoelastic device implantation.
5. Limitations
Although the present study reveals important findings, it is not without limitations. One limitation is the three-year follow-up period, which limits the ability to draw conclusions regarding the long-term performance of viscoelastic devices. Additionally, there may be a risk of selection bias as the study only included patients from a single institution who were treated with a specific type of viscoelastic device by the same neurosurgeon. The heterogeneity in surgical indications among patients may also influence post-operative outcomes.
Author Contributions
Conceptualization, M.-C.T. and M.-C.L.; methodology, M.-C.T. and M.-C.L.; software, Y.-F.L. and W.-H.L.; validation, M.-C.T. and M.-C.L.; formal analysis, M.-C.T.; data curation, Y.-F.L. and W.-H.L.; writing—original draft preparation, M.-C.L.; writing—review and editing, M.-C.T.; visualization, Y.-F.L.; supervision, M.-C.L.; project administration, M.-C.T. and M.-C.L.; funding acquisition, M.-C.T. and M.-C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Shin-Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan.
Institutional Review Board Statement
The study was approved by the Institutional Review Board of Shin-Kong Wu Ho-Su Memorial Hospital before data collection and analysis (approval code: 20200202R).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author. The data are not publicly available for to the privacy of the patients.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Tao, Y.; Galbusera, F.; Niemeyer, F.; Samartzis, D.; Vogele, D.; Wilke, H.J. Radiographic cervical spine degenerative findings: A study on a large population from age 18 to 97 years. Eur. Spine J. 2021, 30, 431–443. [Google Scholar] [CrossRef]
- Choi, S.H.; Kang, C.N. Degenerative Cervical Myelopathy: Pathophysiology and Current Treatment Strategies. Asian Spine J. 2020, 14, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Hammer, C.; Heller, J.; Kepler, C. Epidemiology and pathophysiology of cervical disc herniation. Semin. Spine Surg. 2016, 28, 64–67. [Google Scholar] [CrossRef]
- Theodore, N. Degenerative Cervical Spondylosis. N. Engl. J. Med. 2020, 383, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Buser, Z.; Ortega, B.; D’Oro, A.; Pannell, W.; Cohen, J.R.; Wang, J.; Golish, R.; Reed, M.; Wang, J.C. Spine degenerative conditions and their treatments: National trends in the United States of America. Glob. Spine J. 2018, 8, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Nunley, P.D.; Coric, D.; Jawahar, A.; Kerr, E.; Gordon, C.; Utter, P. Total Disc Replacement in Cervical Spine: 4–7 Years Follow-Up for Primary Outcomes and Symptomatic Adjacent Segment Disease; Cervical Spine Research Society: New York, NY, USA, 2011. [Google Scholar]
- Price, R.L.; Coric, D.; Ray, W.Z. Cervical Total Disc Replacement: Complications and Complication Avoidance. Neurosurg. Clin. N. Am. 2021, 32, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Koreckij, T.D.; Gandhi, S.D.; Park, D.K. Cervical Disk Arthroplasty. J. Am. Acad. Orthop. Surg. 2019, 27, e96–e104. [Google Scholar] [CrossRef]
- Nunez, J.H.; Escudero, B.; Omiste, I.; Martinez-Penas, J.; Surroca, M.; Alonzo-Gonzalez, F.; Bosch-Garcia, D. Outcomes of cervical arthroplasty versus anterior cervical arthrodesis: A systematic review and meta-analysis of randomized clinical trials with a minimum follow-up of 7-year. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.J.; Liu, Y.F.; Hsiao, Y.M.; Huang, Y.H.; Liu, K.C.; Lin, R.M.; Lin, C.L. Comparison of anterior cervical discectomy and fusion versus artificial disc replacement for cervical spondylotic myelopathy: A meta-analysis. J. Neurosurg. Spine 2022, 37, 569–578. [Google Scholar] [CrossRef]
- Zhang, Y.; Lv, N.; He, F.; Pi, B.; Liu, H.; Chen, A.C.; Yang, H.; Liu, M.; Zhu, X. Comparison of cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical disc degenerative diseases on the basis of more than 60 months of follow-up: A systematic review and meta-analysis. BMC Neurol. 2020, 20, 143. [Google Scholar] [CrossRef]
- Wang, Q.L.; Tu, Z.M.; Hu, P.; Kontos, F.; Li, Y.W.; Li, L.; Dai, Y.L.; Lv, G.H.; Wang, B. Long-term Results Comparing Cervical Disc Arthroplasty to Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Orthop. Surg. 2020, 12, 16–30. [Google Scholar] [CrossRef]
- Schuermans, V.N.E.; Smeets, A.; Boselie, A.F.M.; Zarrouk, O.; Hermans, S.M.M.; Droeghaag, R.; Curfs, I.; Evers, S.; van Santbrink, H. Cost-effectiveness of anterior surgical decompression surgery for cervical degenerative disk disease: A systematic review of economic evaluations. Eur. Spine J. 2022, 31, 1206–1218. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, A.A.; Kode, S.; DeVries, N.A.; Grosland, N.M.; Smucker, J.D.; Fredericks, D.C. Biomechanical Analysis of Cervical Disc Replacement and Fusion Using Single Level, Two Level, and Hybrid Constructs. Spine 2015, 40, 1578–1585. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, A.A.; Grosland, N.M.; Kallemeyn, N.A.; Kode, S.; Fredericks, D.C.; Smucker, J.D. Biomechanical Analysis of the Cervical Spine Following Disc Degeneration, Disc Fusion, and Disc Replacement: A Finite Element Study. Int. J. Spine Surg. 2019, 13, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.G.; Havey, R.M. Biomechanics of Cervical Disc Arthroplasty—A Review of Concepts and Current Technology. Int. J. Spine Surg. 2020, 14, S14–S28. [Google Scholar] [CrossRef]
- Jacobs, C.A.M.; Siepe, C.J.; Ito, K. Viscoelastic cervical total disc replacement devices: Design concepts. Spine J. 2020, 20, 1911–1924. [Google Scholar] [CrossRef]
- COBB, J.R. Outline for the study of scoliosis. Instr. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Shin, J.J.; Kim, K.R.; Son, D.W.; Shin, D.A.; Yi, S.; Kim, K.N.; Yoon, D.H.; Ha, Y. Radiological Changes in Adjacent and Index Levels after Cervical Disc Arthroplasty. Yonsei Med. J. 2022, 63, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Rong, X.; Liu, X.J.; Liu, H. Clinical and radiological outcomes of dynamic cervical implant arthroplasty: A 5-year follow-up. World J. Clin. Cases 2021, 9, 3869–3879. [Google Scholar] [CrossRef]
- Wu, T.K.; Liu, H.; Ding, C.; Rong, X.; He, J.B.; Huang, K.K.; Hong, Y.; Wang, B.Y. Effect of preoperative segmental range of motion on patient outcomes in cervical disc arthroplasty. BMC Musculoskelet. Disord. 2020, 21, 457. [Google Scholar] [CrossRef]
- Song, Q.; He, D.; Han, X.; Zhang, N.; Wang, J.; Tian, W. Clinical and radiological outcomes of cervical disc arthroplasty: Ten year follow-up study. Int. Orthop. 2018, 42, 2389–2396. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Chen, P.; Wang, Z.; Chen, G.; Liu, W. Does Cervical Sagittal Balance Affect the Preoperative Neck Disability Index in Patients with Cervical Myelopathy? Clin. Spine Surg. 2020, 33, E21–E25. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Janssen, T.; Arts, M.P.; Peul, W.C.; Vleggeert-Lankamp, C.L.A. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: A systematic review. Spine J. 2018, 18, 1678–1693. [Google Scholar] [CrossRef] [PubMed]
- Zavras, A.G.; Dandu, N.; Nolte, M.T.; Butler, A.J.; Federico, V.P.; Sayari, A.J.; Sullivan, T.B.; Colman, M.W. Segmental range of motion after cervical total disc arthroplasty at long-term follow-up: A systematic review and meta-analysis. J. Neurosurg. Spine 2022, 37, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.J.; Kim, K.R.; Son, D.W.; Shin, D.A.; Yi, S.; Kim, K.N.; Yoon, D.H.; Ha, Y.; Riew, K.D. Cervical disc arthroplasty: What we know in 2020 and a literature review. J. Orthop. Surg. 2021, 29, 23094990211006934. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.K.; Basantani, N.; Carvalho, A.S.; Gupta, E. Long-Term Clinicoradiological Outcomes of Cervical Fusion with Polyether Ether Ketone versus Cervical Disc Arthroplasty in a Double-Blinded Randomized Control Trial. Asian J. Neurosurg. 2021, 16, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Lauryssen, C.; Coric, D.; Dimmig, T.; Musante, D.; Ohnmeiss, D.D.; Stubbs, H.A. Cervical total disc replacement using a novel compressible prosthesis: Results from a prospective Food and Drug Administration-regulated feasibility study with 24-month follow-up. Int. J. Spine Surg. 2012, 6, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Hui, N.; Phan, K.; Lee, M.Y.; Kerferd, J.; Singh, T.; Mobbs, R.J. The Changes in Cervical Biomechanics After CTDR and Its Association with Heterotopic Ossification: A Systematic Review and Meta-analysis. Global. Spine J. 2021, 11, 565–574. [Google Scholar] [CrossRef]
- Hou, Y.; Nie, L.; Pan, X.; Si, M.; Han, Y.; Li, J.; Zhang, H. Effectiveness and safety of Mobi-C for treatment of single-level cervical disc spondylosis: A randomised control trial with a minimum of five years of follow-up. Bone Jt. J. 2016, 98 Pt B, 829–833. [Google Scholar] [CrossRef]
- Fransen, P.; Hansen-Algenstaedt, N.; Chatzisotiriou, A.; Noriega, D.; Verheyden, J.; Van Hecke, W.; Pointillart, V. Radiographic outcome and adjacent segment evaluation two years after cervical disc replacement with the Baguera® C prosthesis as treatment of degenerative cervical disc disease. J. Spine 2016, 5, 1–7. [Google Scholar] [CrossRef]
- Moon, J.H.; Chung, C.K.; Kim, C.H.; Lee, C.H.; Park, S.B.; Heo, W. Longitudinal change of cervical artificial disc motion following replacement. PLoS ONE 2020, 15, e0228628. [Google Scholar] [CrossRef]
- Liu, B.; Wu, B.; Van Hoof, T.; Okito, J.P.; Liu, Z.; Zeng, Z. Are the standard parameters of cervical spine alignment and range of motion related to age, sex, and cervical disc degeneration? J. Neurosurg. Spine 2015, 23, 274–279. [Google Scholar] [CrossRef]
- Machino, M.; Yukawa, Y.; Imagama, S.; Ito, K.; Katayama, Y.; Matsumoto, T.; Inoue, T.; Ouchida, J.; Tomita, K.; Ishiguro, N.; et al. Age-Related and Degenerative Changes in the Osseous Anatomy, Alignment, and Range of Motion of the Cervical Spine: A Comparative Study of Radiographic Data From 1016 Patients with Cervical Spondylotic Myelopathy and 1230 Asymptomatic Subjects. Spine 2016, 41, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Yukawa, Y.; Kato, F.; Suda, K.; Yamagata, M.; Ueta, T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Chang, H.K.; Huang, W.C.; Tu, T.H.; Fay, L.Y.; Kuo, C.H.; Chang, C.C.; Wu, C.L.; Chang, H.C.; Cheng, H. Radiological and clinical outcomes of cervical disc arthroplasty for the elderly: A comparison with young patients. BMC Musculoskelet. Disord. 2019, 20, 115. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Wang, H.; Wang, C.; Tsai, T.Y.; Yu, Y.; Ostergaard, P.; Li, G.; Cha, T. Intervertebral range of motion characteristics of normal cervical spinal segments (C0-T1) during in vivo neck motions. J. Biomech. 2020, 98, 109418. [Google Scholar] [CrossRef] [PubMed]
- Anderst, W.J.; Donaldson, W.F., 3rd; Lee, J.Y.; Kang, J.D. Three-dimensional intervertebral kinematics in the healthy young adult cervical spine during dynamic functional loading. J. Biomech. 2015, 48, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, M.; Hong, S.W.; Yoon, S.H.; Zou, J.; Tow, B.; Alanay, A.; Abitbol, J.-J.; Wang, J.C. Kinematic Analysis of the Relationship Between the Grade of Disc Degeneration and Motion Unit of the Cervical Spine. Spine 2008, 33, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, G.M.; Assietti, R.; Corbino, L.; Olindo, G.; Foti, P.V.; Russo, V.; Albanese, V. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: Opposite or complementary techniques? Eur. Spine J. 2009, 18 (Suppl. S1), 29–39. [Google Scholar] [CrossRef]
- McAfee, P.C.; Cunningham, B.W.; Devine, J.; Williams, E.; Yu-Yahiro, J. Classification of heterotopic ossification (HO) in artificial disk replacement. J. Spinal Disord. Tech. 2003, 16, 384–389. [Google Scholar] [CrossRef]
- Dowdell, J.E.; Kim, J.S.; Mikhail, C.; Overley, S.C.; Levin, J.M.; McAnany, S.J.; Mroz, T.E.; Hecht, A.C. The Rate of Heterotopic Ossification Following Cervical Disc Arthroplasty: A Systematic Review and Comparison of Data. Spine 2020, 45, E1197–E1202. [Google Scholar] [CrossRef] [PubMed]
- Neifert, S.N.; Martini, M.L.; Yuk, F.; McNeill, I.T.; Caridi, J.M.; Steinberger, J.; Oermann, E.K. Predicting Trends in Cervical Spinal Surgery in the United States from 2020 to 2040. World Neurosurg. 2020, 141, e175–e181. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y. Lumbar and cervical viscoelastic disc replacement: Concepts and current experience. World J. Orthop. 2020, 11, 345–356. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).