Abstract
Background: Postoperative physical therapy emerges as a pivotal element of the rehabilitation process, aimed at enhancing functional recovery, managing pain, and mitigating the risk of further complications. The debate concerning the optimal timing of physical therapy intervention post-surgery remains unresolved; in particular, whether to initiate physical therapy immediately or to wait weeks is of particular interest. The aim of this study is to review the available literature regarding the optimal timing of physical therapy initiation and the outcomes obtained. Methods: This review was carried out in accordance with the Preferential Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines. This search was carried out in February 2024. Only peer-reviewed articles were considered for inclusion. Results: Fourteen studies were included. The primary outcomes assessed in the included studies were the following: 12-week and 12-month low back pain, return to work, function and disability, psychological status, patient satisfaction, and complications associated with early physical therapy. A meta-analysis was performed concerning low back pain after lumbar discectomy at 12 weeks and 12 months and complications after early physical therapy after lumbar discectomy and lumbar interbody fusion. A significant difference was found between early and standard physical therapy in terms of low back pain at 12–18 months (p = 0.0062); no significant differences were found in terms of complications, both for discectomy and arthrodesis. Conclusions: This review indicates that employing early rehabilitation strategies for intervertebral disc disease could enhance results in terms of pain and disability without an enhanced risk of complications.
1. Introduction
The ongoing demographic transformation towards a more aged global population is set to profoundly reshape healthcare priorities, particularly in the realm of managing degenerative spine diseases [1]. The World Health Organization’s projection states that by 2030, one in every six individuals worldwide will be over the age of 60, bringing to the forefront the urgent need to address the burgeoning health challenges associated with this shift [2].
Among these challenges, degenerative conditions such as lumbar disc herniation (LDH), degenerative scoliosis, and lumbar stenosis are increasingly prevalent, driven by factors including aging, lifestyle, and genetic predisposition. These conditions, characterized by the progressive degeneration of spinal structures, significantly impact patients’ quality of life, often necessitating surgical treatment for relief [3,4,5].
Postoperative physical therapy emerges as a pivotal element of the rehabilitation process, aimed at enhancing functional recovery, managing pain, and mitigating the risk of further complications [6,7]. However, the debate concerning the optimal timing of physical therapy intervention post-surgery remains unresolved; in particular, whether to initiate physical therapy immediately or to wait weeks is of particular interest. Contemporary research supports initiating physical therapy within two weeks postoperatively for lumbar discectomy [8] and between three and six weeks postoperatively for single-level lumbar interbody fusion [9]. This timing has been shown to effectively reduce postoperative low back pain, enhance functional recovery, and decrease disability. Early physical therapy should be integrated into multimodal Enhanced Recovery After Surgery (ERAS) programs, which have been shown through empirical evidence to significantly improve outcomes. These programs not only relieve postoperative pain and speed up functional recovery but also have the added benefit of increasing patient turnover in hospitals. By shortening hospital stays, early physical therapy allows for a quicker return to daily activities and work, thus offering distinct advantages over traditional rehabilitation protocols. Hospital managers should investigate the importance of early physical therapy to further enhance the efficiency of patient management and support faster recovery processes [10].
This review endeavors to synthesize the existing literature, focusing on the timing of physical therapy initiation and the outcomes obtained. A comprehensive review of the literature was conducted to determine the optimal timing for initiating physical therapy following surgery. This includes an analysis of early vs. delayed initiation of physical therapy interventions with the aim of understanding their impact on patient outcomes such as functional recovery, pain management, and complications.
The goal is to identify which timing of physical therapy initiation is most effective in improving functional capacity, alleviating pain, and facilitating a return to daily activities, while also considering the potential risks of initiating therapy too early. By addressing these two critical aspects, this review aims to furnish clinical practice by identifying the most effective strategies for physical therapy intervention post-surgery for degenerative intervertebral disc disease and ensuring that recommendations are tailored to meet the individual needs of patients.
2. Materials and Methods
2.1. Review Design
A systematic review of the literature regarding the optimal timing of postoperative physical therapy after spine surgery for degenerative disc disease was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11]. The Oxford Centre for Evidence-Based Medicine (OCEBM) [12] was used to assess the level of evidence in the included studies (full version for randomized and non-randomized clinical trials, modified version for all other studies).
The considered inclusion criteria were the following: papers describing the optimal timing of postoperative physical therapy after elective lumbar spine procedures in degenerative intervertebral disc disease, either discectomy or one-level lumbar interbody fusion.
The applied exclusion criteria were the following: Isolated case reports/series with less than 5 patients, technical notes, expert opinions, literature reviews, meta-analyses, and biomechanical and/or in vitro studies; papers providing incomplete data or not providing data regarding optimal timing for postoperative physical therapy; papers describing outcomes in cervical spine, tumoral or metastatic spine, trauma, infection, and revision surgery. Papers reporting results in patients with a diagnosis of rheumatologic disease, connective tissue disease, or malabsorptive disorder were also excluded because these conditions can affect bone and muscle quality, confounding the results. Studies not indicating the diagnosis but excluding patients undergoing cervical or thoracic spine, tumoral or metastatic spine, trauma, and revision surgery were also included. Articles in English in peer-reviewed journals that met the population, intervention, comparison, and outcome criteria on systematic reviews were considered for inclusion. Randomized controlled trials, prospective and retrospective cohort studies, and case series (CS) were considered for inclusion.
2.2. Search Strategy
An electronic systematic search of the available English literature on three large electronic databases (Pubmed-MEDLINE, Scopus, and Google Scholar) was performed over the years 1994–2024 to identify eligible studies. The online literature search was conducted in February 2024 by two authors. The authors stated the following research questions: “Is there an optimal time for starting physical therapy after degenerative disc disease surgery?”; “Is early physical therapy beneficial when compared to standard physical therapy?”; and “Is early physical therapy safe, or does it bring more complications when compared to standard physical therapy?”.
The search was conducted using combinations of the following keywords: “lumbar disc disease”, “discectomy”, “exercise therapy”, “rehabilitation”, “intervertebral disc degeneration”, “lumbar spine fusion”, “physical therapy”, “lumbar pain”, “lumbar physical therapy”, “visual analogue scale”, “timing”, “low back pain”, “optimal timing”, “early physical therapy”, “ODI”, “outcomes”, “complications”, “exercises”, “pain”, and “disability”.
2.3. Study Selection
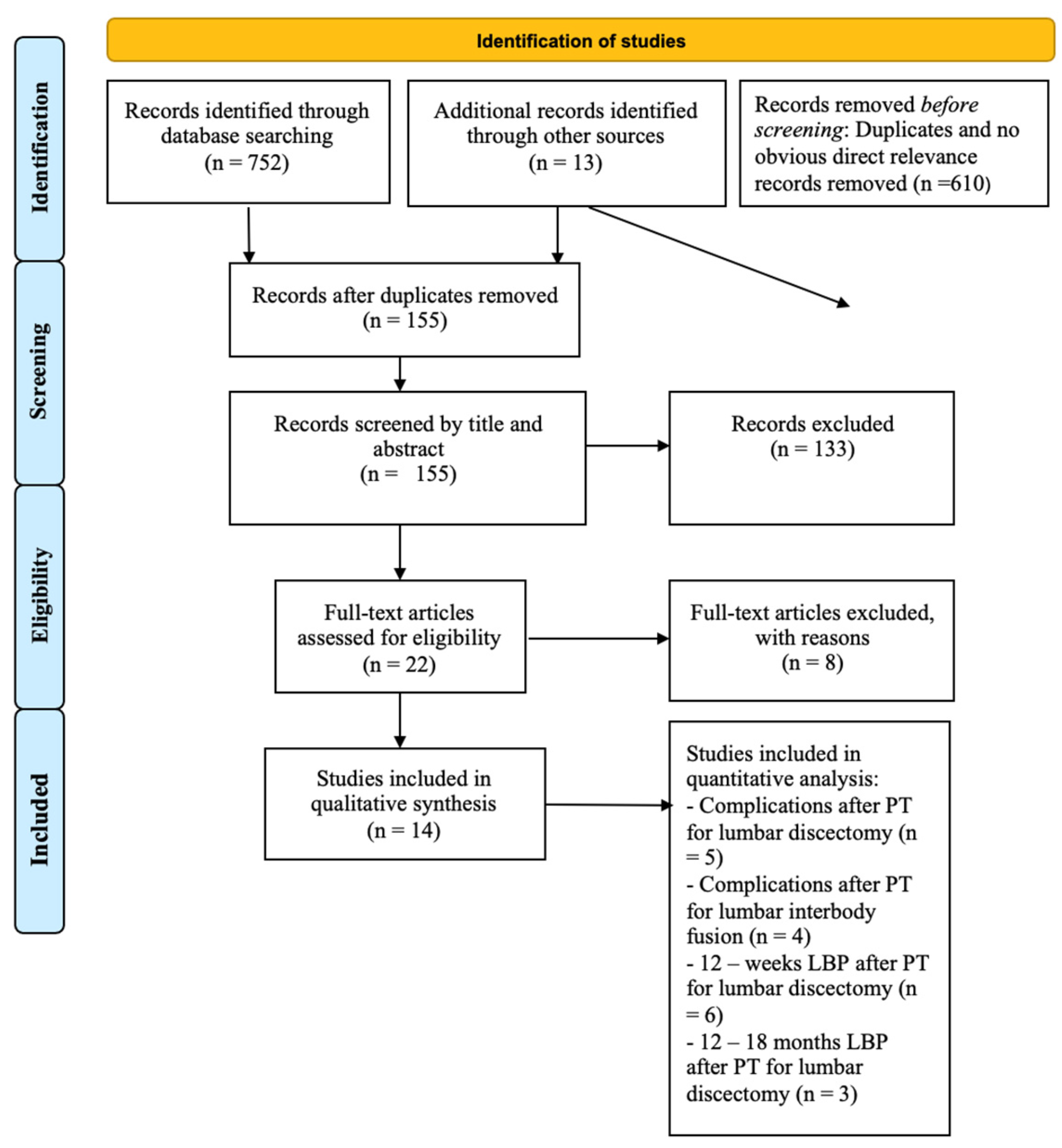
After screening the titles and abstracts, the full-text articles were obtained and reviewed. A manual search of the bibliography of each of the relevant articles was also performed to identify potentially missed eligible papers. Reviews and meta-analyses were also analyzed to potentially broaden the search for studies that might have been missed through the electronic search. Duplicates were removed. The study selection process was carried out in accordance with the PRISMA flowchart [11] (Figure 1).

Figure 1.
Prisma 2009 flow diagram of the included studies; LBP = low back pain; PT = physical therapy.
The present systematic review was accepted for registration in the PROSPERO database for systematic reviews [13] (ID: CRD42024523304). Ethical approval and institutional review board approval were not required because this study retrieved and synthesized data from already published studies.
2.4. Data Extraction
Two authors extracted the data through a standardized data collection form. Three authors checked the data for accuracy, and inconsistent results were discussed. Data concerning study design, number and demographics of patients, surgical procedure, timing of physical therapy, intervention type, control, results, and complications were extracted and summarized in Table 1.

Table 1.
Details of the included studies; NS = non-specified; RMQ = Roland Morriss Questionnaire; DRI = Disability Rating Index; VAS = visual analogue scale.
Post-physical-therapy pain, disability, function, return to work, patient satisfaction, and complications at different timings of physical therapy initiation were considered as outcome measures. When studies involved patients with early timing of postoperative physical therapy not solely limited to degenerative disc disease patients (such as tumors or fractures), data about patients with degenerative disc disease were pooled; if this was not possible, the study was excluded.
2.5. Methodological Quality Assessment of Included Studies
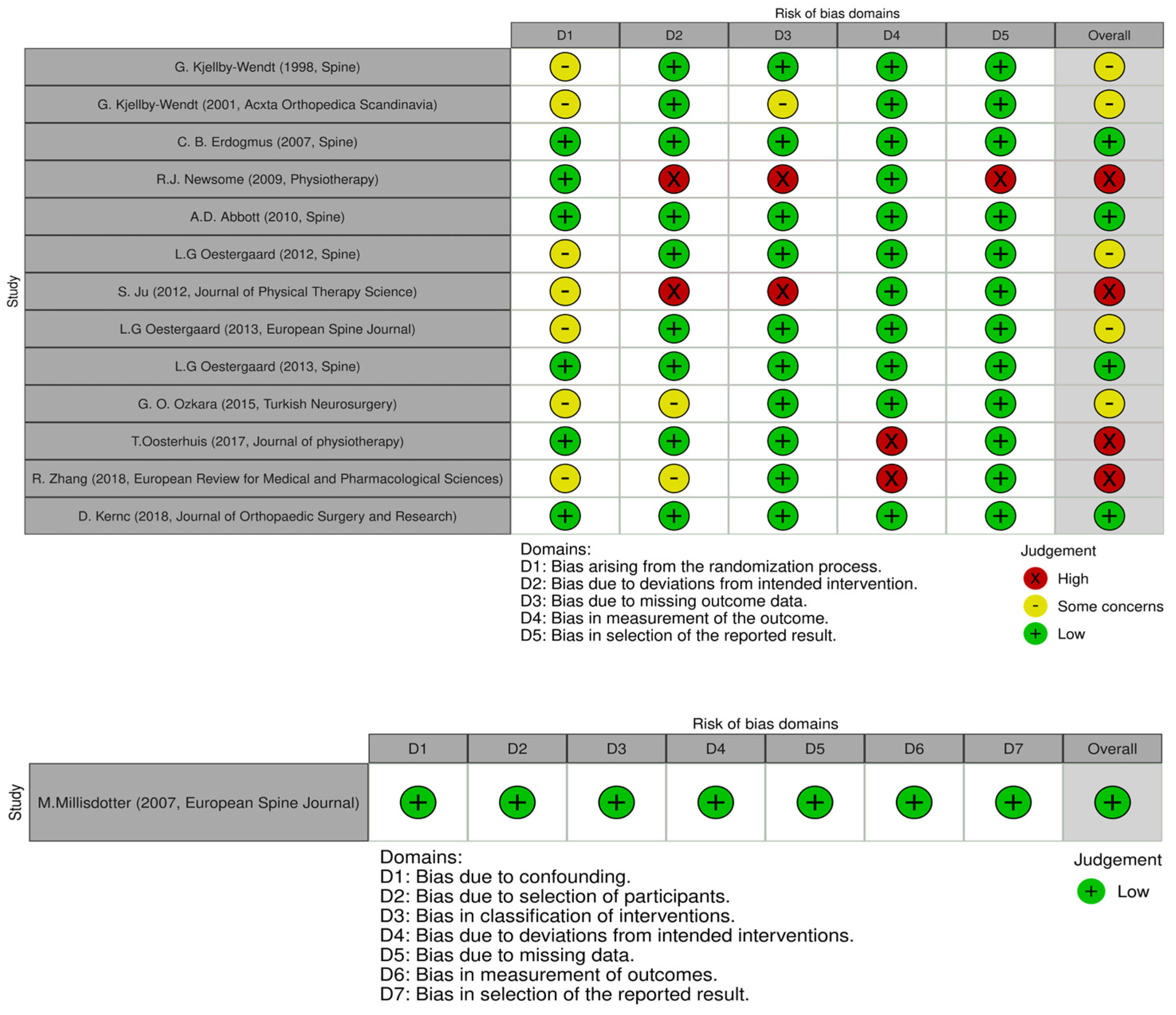
The Revised Cochrane Risk of Bias tool for randomized trials (RoB 2.0) [14] was used to assess the methodological quality of the included studies. The quality of each study was reported by assessing 5 domains: randomization process, deviation from intended interventions, missing outcomes, measurement of the outcomes, and selection of the reported results. Each domain can present a low, some-concern, or high risk of bias; these combined together form an overall risk of bias. For each included study, the total risk of bias was categorized as low risk with 5 low-risk domains, some-concern risk with at least one some-concern domain, and high risk with ≥1 high-risk domain or multiple some-concern domains. A similar tool, the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) tool, was used for evaluating the methodological quality of only the non-randomized studies included [8]. As with the evaluation of titles and abstracts, any disagreement was solved by a senior author. Details on the quality of the studies included are summarized in Figure 2 and Figure 3.
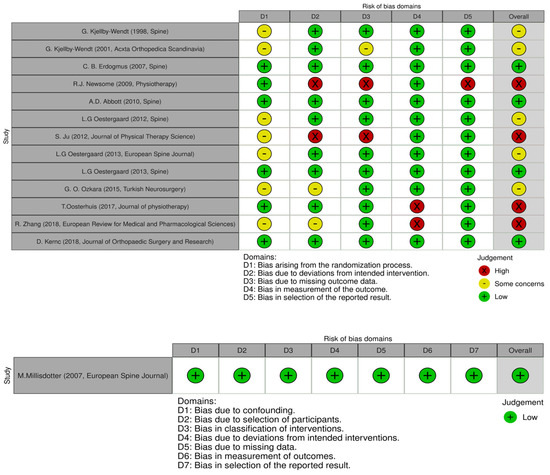
Figure 2.
ROB 2.0 and ROBINS-I tools used for the included studies [8,9,14,15,16,17,18,19,20,21,22,23,24,25].

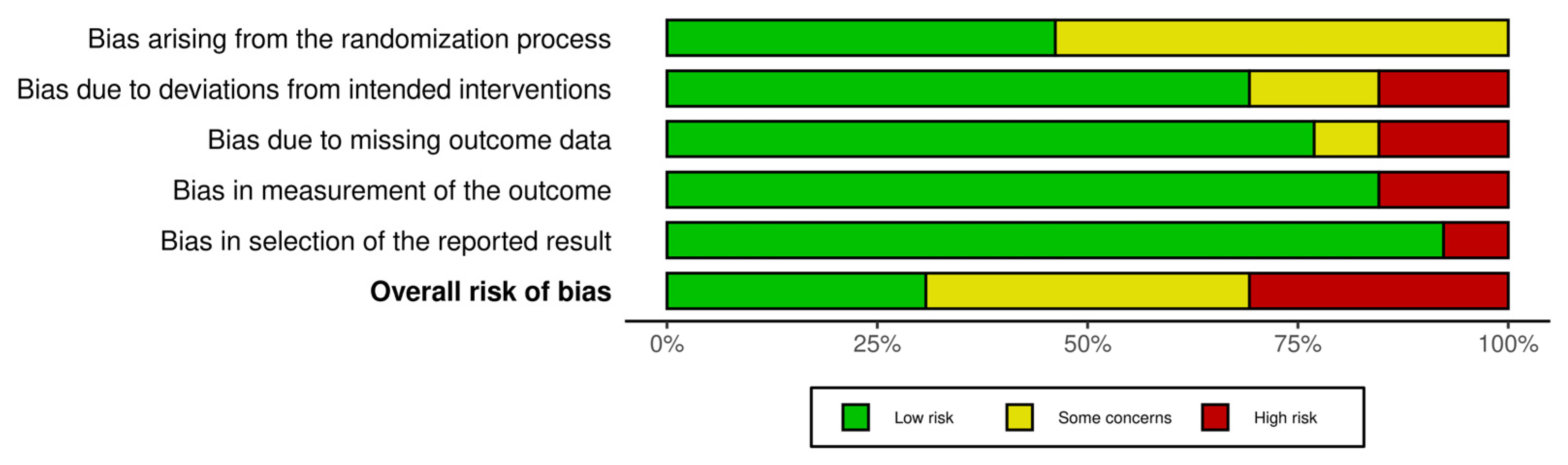
Figure 3.
ROB2 tool plot summary.
2.6. Statistical Analysis
Meta-analyses were performed when at least three studies were comparable. This was possible for complications after physical therapy for lumbar discectomy and interbody lumbar fusion, for 1-year residual back pain after physical therapy for lumbar discectomy, and for 12-week residual back pain after physical therapy for lumbar discectomy.
For complication rates, dichotomous models were evaluated; for post-physical therapy back pain, a standardized mean difference evaluation was performed. The analysis was carried out using the log odds ratio with 95% CI and p value as the outcome measure of effect size. A random-effects model was fitted to the data. The amount of heterogeneity (i.e., tau2) was estimated using the restricted maximum likelihood estimator. In addition to the estimate of tau2, the Q-test for heterogeneity and the I2 statistic were reported. In cases where any amount of heterogeneity was detected (i.e., tau2 > 0, regardless of the results of the Q-test), a prediction interval for the true outcomes was also provided. Studentized residuals and Cook’s distances were used to examine whether studies may be outliers and/or influential in the context of the model. Studies with a studentized residual larger than the 100 × (1 − 0.05/(2 × k))th percentile of a standard normal distribution were considered potential outliers (i.e., using a Bonferroni correction with two-sided alpha = 0.05 for k studies included in the meta-analysis). Studies with a Cook’s distance larger than the median plus six times the interquartile range of the Cook’s distances were considered to be influential. The rank correlation test and the regression test, using the standard error of the observed outcomes as a predictor, were used to check for funnel plot asymmetry. All statistical analyses were conducted with Jamovi version 2.2 (The Jamovi Project, Sydney, Australia) software. A p value < 0.05 was considered to be significant.
3. Results
3.1. Included Studies and Population
Initially, a total of 752 studies were found through an electronic search. Before title screening, 610 articles were excluded after duplication removal or for having no obvious direct relevance to the topic. A total of 155 records were screened by title and abstract, leading to the exclusion of 133 records. After screening, 22 studies were assessed for eligibility. The inclusion criteria were not met by eight studies, such as those that included revision surgery patients; those with traumatic, neoplastic, or cervical spine diseases; or those that reported no or insufficient postoperative physical therapy timing data or surgical procedure data.
Eventually, 14 studies [8,9,15,16,17,18,19,20,21,22,23,24,25,26] met the inclusion criteria and were included in this systematic review for qualitative synthesis. Five different studies [8,15,21,23,26] were considered for quantitative analysis regarding complications after physical therapy for lumbar discectomy, four [9,16,19,24] for complications after physical therapy for lumbar interbody fusion, six [8,15,21,22,25,26] for 12-week residual back pain after physical therapy for lumbar discectomy, and three studies [8,15,21] for 1-year residual back pain after physical therapy for lumbar discectomy (Figure 1).
All of the included studies were designed in a randomized control trial fashion, except for one, which utilized prospectively collected data and enrolled patients using single-institution databases from various years of recruitment. The included studies reported data on a total of 993 patients (596 females, 60%), and the median age at surgery ranged from 32.5 ± 7.3 to 61.1 ± 8 years. In all the analyzed studies, each group of early physical therapy patients in which outcomes were evaluated was matched with a relatively homogeneous group composed of non-early physical therapy patients in which outcomes were evaluated. The included studies analyzed both small- and large-sized populations and were heterogeneous in the description of complications after physical therapy (Table 1).
3.2. Risk of Bias Assessment
Two authors assessed the risk of bias for each study using the ROB 2.0 and ROBINS-I tools; the results are shown in Figure 2. The studies indicated an overall risk of bias that was categorized as low, presenting some concerns, or high (respectively, 35.7%, 35.7%, and 28.6%). Four studies [18,22,23,26] had a high risk of bias due to the bias caused by the randomization process, deviations from the intended interventions, measurement of the outcomes, and selection of the reported results. Since most studies described outcome measurement well with clear definitions of the results, accurate and reliable outcome measurements, and low missing outcomes, they demonstrated low measurement outcome and low missing outcome data and low bias in the selection of the reported result items (<80%). Furthermore, the randomization process item was consistently moderate for most studies (~50%) since the randomization process may be skewed by the described procedure for randomization (Figure 3).
3.3. Timing of Physical Therapy
All the included studies evaluated the timing of the initiation of postoperative rehabilitation in their populations. Six distinct timings of early physical therapy (2 h, 1 day, 1 week, and 2 weeks postoperatively for lumbar discectomy; and 3 and 6 weeks postoperatively for lumbar interbody fusion) were discussed in this review.
Kjellby and colleagues [15] randomized two groups of patients who started an early active training program (EAT) at either postoperative day 1 or week 6 after a lumbar microdiscectomy. The EAT group patients had significantly less intense pain compared to the control group patients at 6 and 12 weeks after surgery. The range of motion of the lumbar spine was significantly more increased in the EAT group at 12 weeks after surgery compared to the controls. However, this trend was not replicated one year after surgery.
Erdogmus et al. [21] confirmed the importance of early physical therapy, starting from postoperative week 1 after lumbar discectomy. In this prospective randomized study, the authors randomized 120 patients into three groups of interventions (early physical therapy, sham therapy, and no treatment) and compared the results at 12 weeks and 1.5 years. There was a significant difference in low back pain at 12 weeks in early physical therapy patients compared to the untreated patients, which was not replicated at 1.5 years. These results are in contrast with those obtained by other studies [23,26], where early physical therapy was neither more effective nor more cost-effective than no referral.
Oestergaard et al. [9] performed a randomization of two groups of patients who had undergone lumbar fusion to initiate physical therapy early, at 6 weeks, or standard, at 12 weeks postoperatively. An early start of rehabilitation (6 weeks vs. 12 weeks) resulted in inferior outcomes; moreover, the improvement in the 12-week group was four times better compared to the 6-week group.
These results are in contrast with those obtained by Abbott et al. [24], where early physical therapy at postoperative week 3 improved pain, functional disability, self-efficacy, outcome expectancy, and fear of movement when compared with no physical therapy for the first 3 postoperative weeks.
In another study [19], the randomization between early physical therapy at 3 weeks and a control group with no physical therapy for 3 months showed that early initiation of postoperative rehabilitation had better results in terms of muscle strength and walking speed.
3.4. Outcomes Evaluated
This systematic review examined the primary outcomes assessed in the included studies: 12-week and 12-month low back pain, return to work, function and disability, psychological status, patient satisfaction, and complications associated with early physical therapy.
The intensity of low back pain at 12 weeks and 12 months following physical therapy, both post-lumbar interbody fusion and post-lumbar discectomy, has been analyzed. Merely two studies [9,24] specifically examined low back pain following physical therapy for lumbar interbody fusion, yielding contradictory results.
Abbott et al. [24], in their randomized control trial, demonstrated that early postoperative rehabilitation can be safely administered after lumbar fusion, significantly reducing the VAS score for low back pain in comparison to control subjects at 3, 6, and 12 months, with no further differences noted at 2–3 years.
These findings starkly contrast with those of another study [9], in which, at a 12-month follow-up, the early physical therapy group exhibited outcomes four times worse in terms of back pain when compared to the control group, suggesting that an early initiation of physical therapy may adversely affect overall outcomes.
When comparing early physical therapy with sham or no physical therapy in patients who have undergone lumbar discectomy, there is reasonable evidence that early physical therapy reduces pain at 12 weeks, as stated by the included studies.
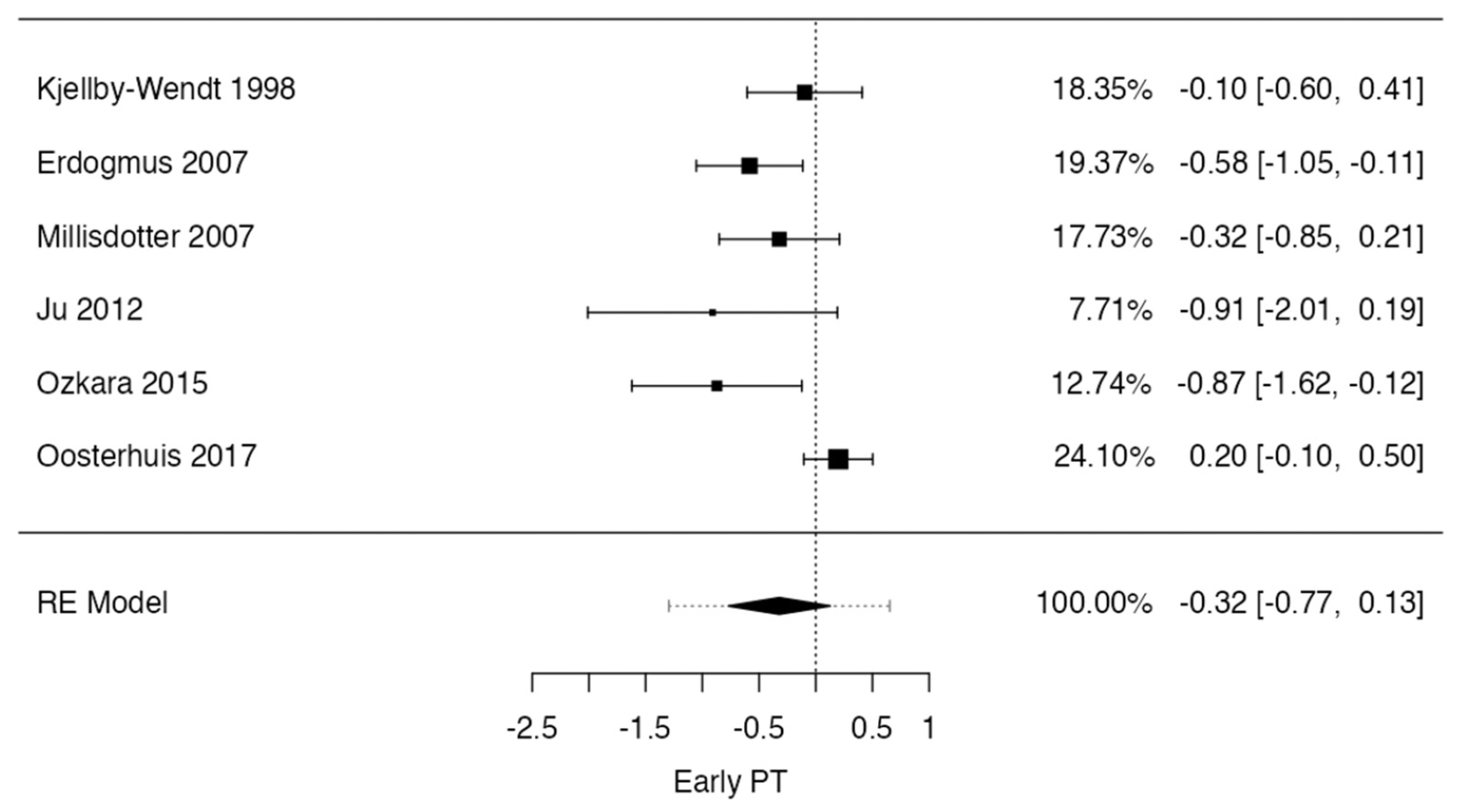
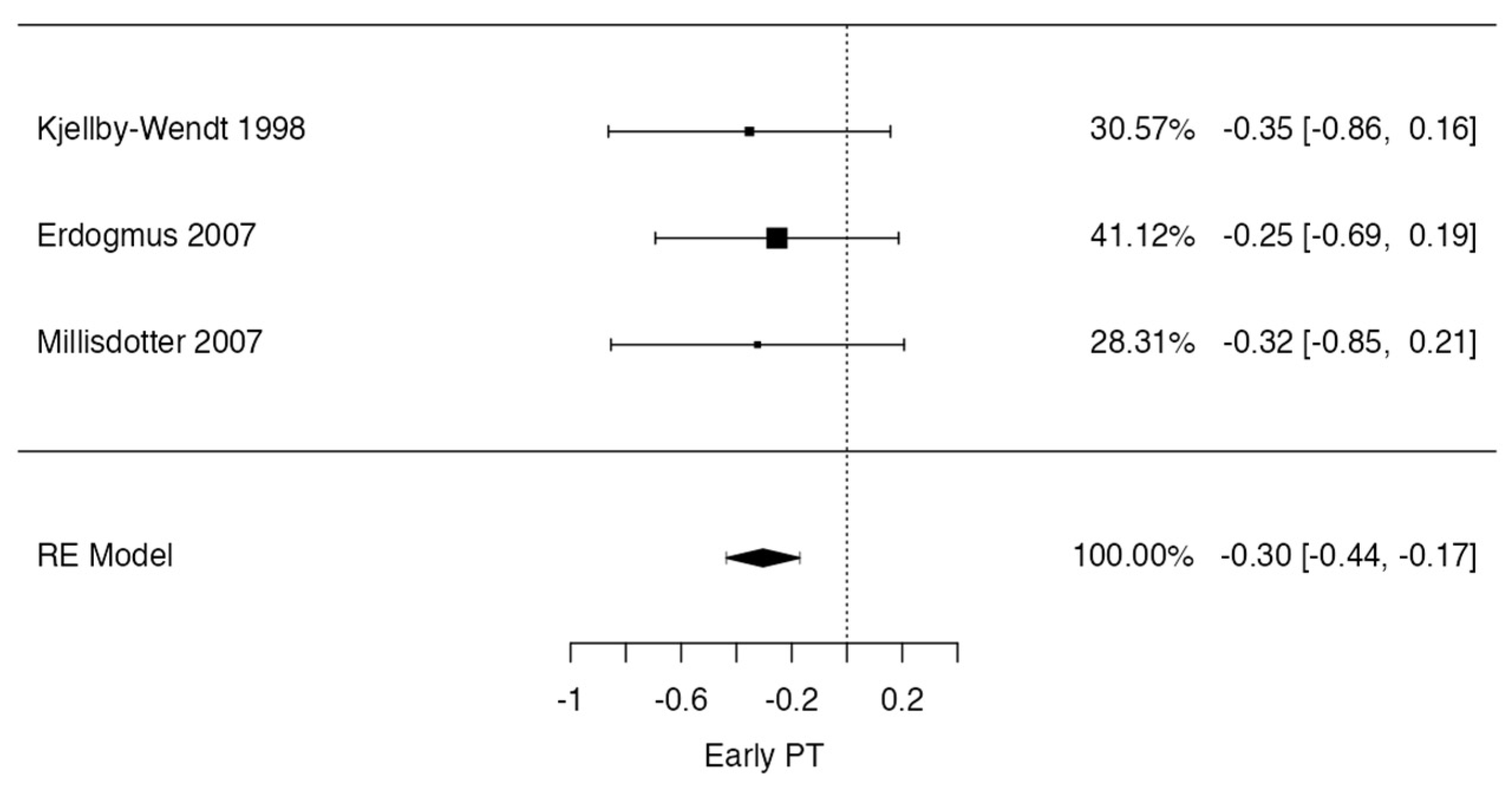
However, a meta-analysis was performed on studies in which data regarding patients with low back pain after early or standard physical therapy could be pooled. This was possible for six studies that quantified low back pain at 12 weeks postoperatively [8,15,21,22,25,26] and for three studies that quantified low back pain at 12–18 months [8,15,21] postoperatively after lumbar discectomy.
In the low back pain at 12 weeks case, the observed standardized mean differences ranged from −0.9092 to 0.1991, with most estimates being negative (83%). The estimated average standardized mean difference based on the random-effects model was −0.3210 (95% CI: −0.7706 to 0.1287). Therefore, the average outcome did not differ significantly from zero (t (5) = −1.8349, p = 0.1260). According to the Q-test, the true outcomes appeared to be heterogeneous (Q (5) = 14.1591, p = 0.0146, tau2 = 0.1129, I2 = 61.9562%). A 95% prediction interval for the true outcomes was given as −1.2948 to 0.6529. Hence, although the average outcome was estimated to be negative, in some studies, the true outcome may in fact be positive. An examination of the studentized residuals revealed that one study [26] had a value larger than ± 2.6383 and may be a potential outlier in the context of this model. According to Cook’s distances, none of the studies could be overly influential. The regression test indicated funnel plot asymmetry (p = 0.0410), but not the rank correlation test (p = 0.4694) (Figure 4).

Figure 4.
Forrest plot representation of the meta-analysis for low back pain at 12–week follow-up after lumbar discectomy [8,14,16,19,22,23].
In the low back pain at 12–18 months case, the observed standardized mean differences ranged from −0.3529 to −0.2531, with the majority of estimates being negative (100%). The estimated average standardized mean difference based on the random-effects model was −0.3036 (95% CI: −0.4364 to −0.1709). Therefore, the average outcome differed significantly from zero (t(2) = −9.8411, p = 0.0102). According to the Q-test, there was no significant amount of heterogeneity in the true outcomes (Q(2) = 0.0919, p = 0.9551, tau2 = 0.0000, I2 = 0.0000%). An examination of the studentized residuals revealed that one [21] of the studies had a value larger than ± 2.3940 and may be a potential outlier of this model. According to Cook’s distances, none of the studies could be considered to be overly influential. Neither the rank correlation nor the regression test indicated any funnel plot asymmetry (p = 1.0000 and p = 0.2881, respectively) (Figure 5).
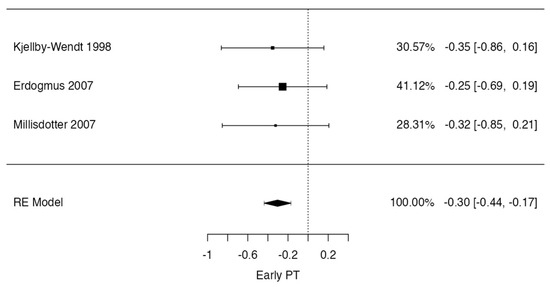
Figure 5.
Forrest plot representation of the meta-analysis for low back pain at 12–18-month follow-up after lumbar discectomy [8,14,16].
Five trials [9,15,21,23,25] evaluated return-to-work differences between early physical therapy and controls. All trails, except for one [23], agree on the non-significant influence of early physical therapy on return to work. In one trial, more than 80% of participants returned to work after 1.5 years without any significant difference between groups [15]. On the other hand, Newsome and colleagues [23] reported that patients in the early physical therapy group showed a significantly more rapid return to work when compared to the control group. Unfortunately, a meta-analysis could not be conducted due to the impossibility of pooling data resulting from the heterogeneity in the timing of the return-to-work evaluation or due to missing data.
All studies included in this review, except for two [18,20], reported outcomes related to either functionality or disability following early physical therapy. The current literature trend suggests that there is evidence of significant differences in disability and function among patients who commence physical therapy early. Nevertheless, these significant differences become less pronounced when examining studies in which patients underwent single-level lumbar fusion. Indeed, Oestergaard and colleagues [9,16,17] have described in their investigations that early physical therapy does not outperform standard physical therapy regarding disability and function. Rather, it may demonstrate inferior results at a one-year follow-up when compared to standard physical therapy. These results are in contrast with those obtained by Abbott et al. [24], where patients who underwent early physical therapy treatment at 3 weeks significantly improved their disability and function scores when compared to the controls. Despite this, a meta-analysis could not be conducted due to the impossibility of pooling data. This was the result of either the heterogeneity in the timing of function and disability evaluations and the tools used for these evaluations or due to missing data.
Three trials reported on patient satisfaction [15,21,25] and four on the psychological status after early physical therapy [20,24,25,26]. Regarding patient satisfaction, one study [15] indicated that there was no significant difference in treatment outcome satisfaction among participants across different groups at any evaluated time point. In contrast, a separate investigation [21] conducted a follow-up two years post-surgery, revealing that 88% of the individuals who had undergone early, comprehensive physical therapy expressed satisfaction with their functional outcomes. This is in comparison to 67% of the participants in the control group reporting similar satisfaction levels.
The psychological well-being was meticulously delineated by Kjelby et al. in their randomized controlled trial [20], wherein patients who underwent early physical therapy showed significant improvement in anxiety levels and pain coping in their daily activities when compared with the controls. This finding received corroboration through the studies conducted by Abbott [24] and Ozakara [25]. Despite this, a meta-analysis could not be conducted due to the impossibility of pooling data. This was the result of either the heterogeneity in the timing of patient satisfaction and psychological status evaluations and the tools used for these evaluations or due to missing data.
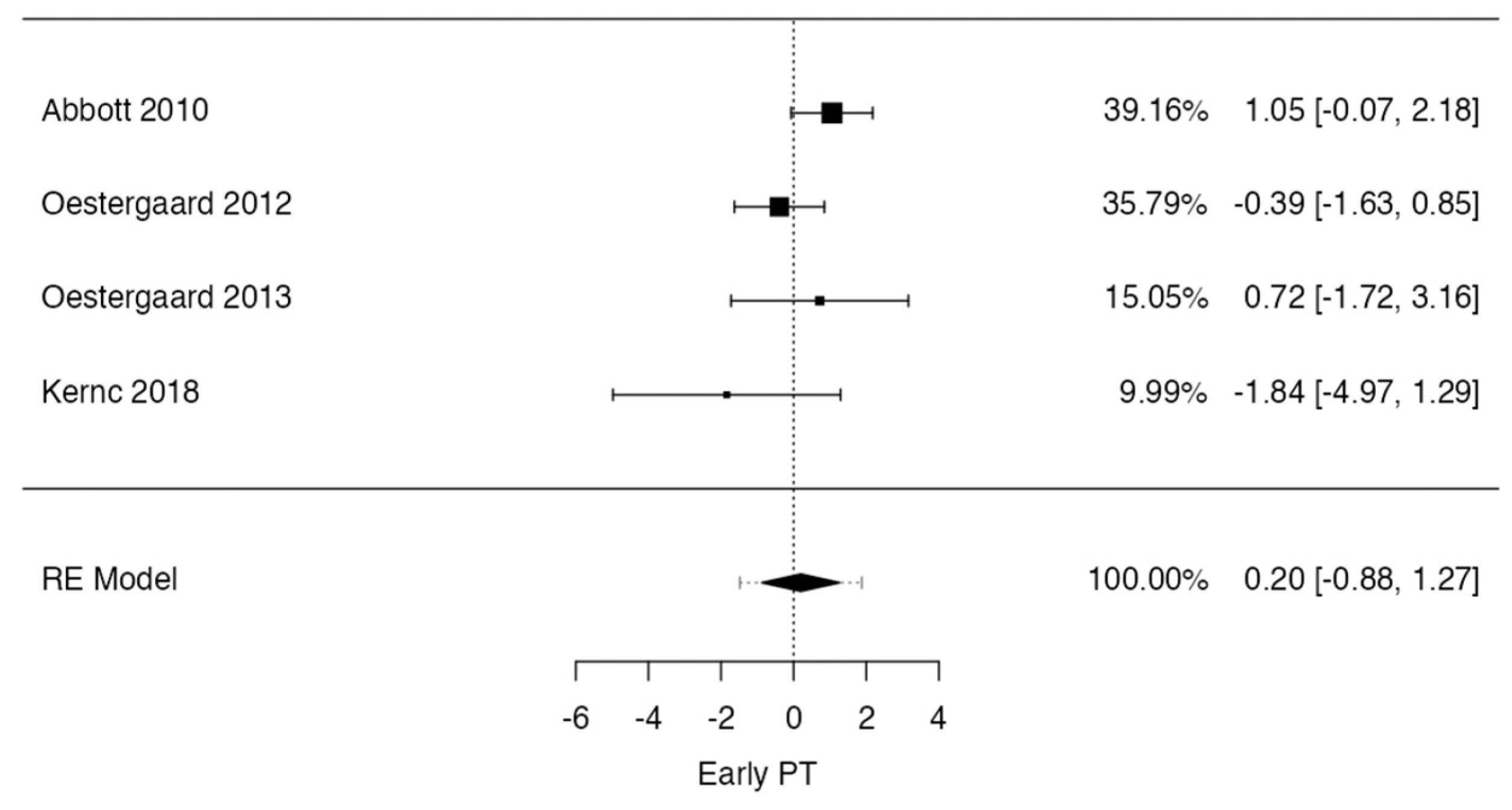
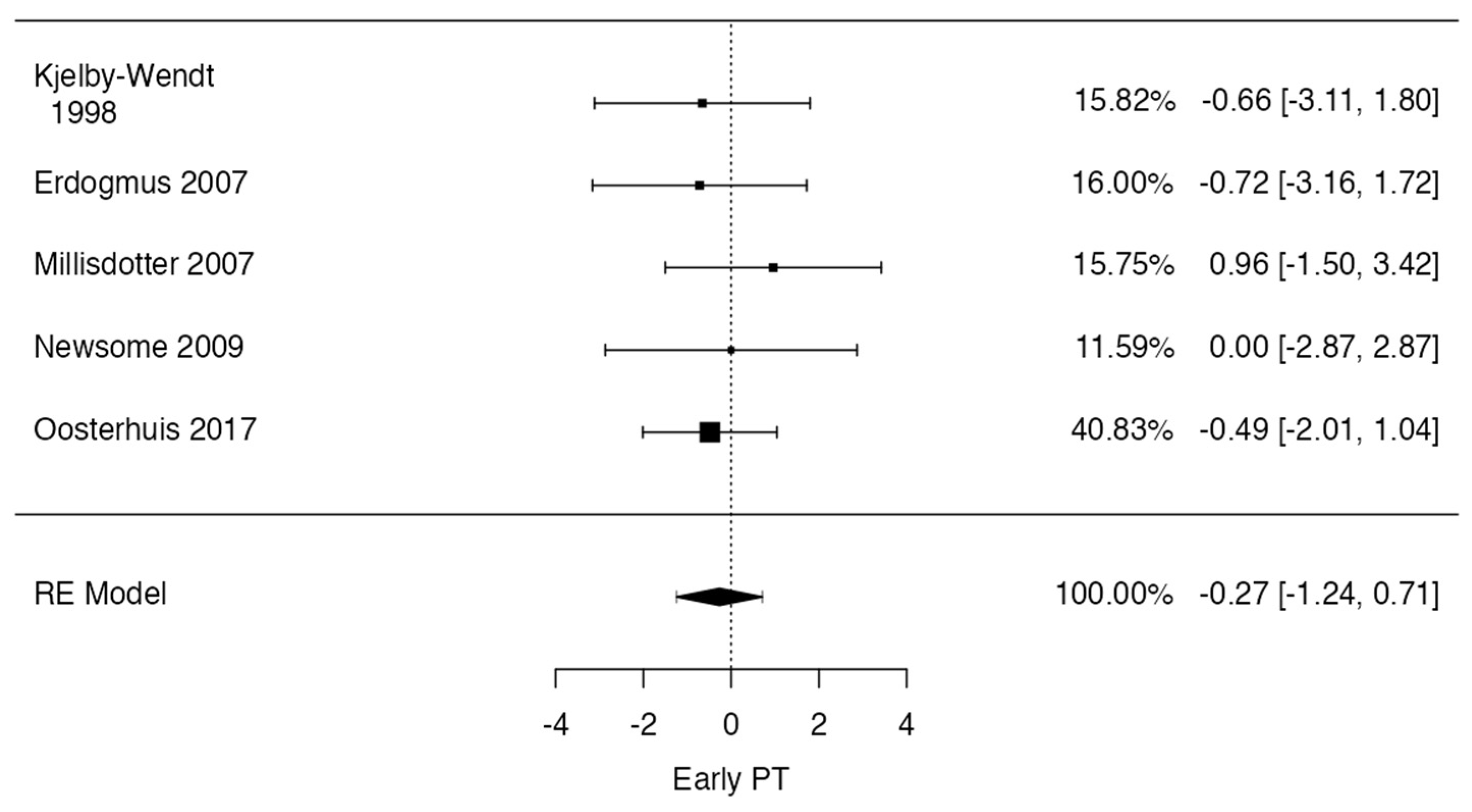
When comparing early physical therapy with sham or no physical therapy, there is reasonable evidence to suggest that early physical therapy is safe and does not increase the risk of complications, as stated by the included studies. Four trials [9,17,24] reported complications in patients who underwent lumbar interbody fusion. Conversely, five trials [8,15,16,17,23] reported complications in patients who underwent lumbar discectomy. The adverse events reported included re-herniation, reoperation at a different or the same level, pseudarthrosis, loosening of the implant, and revision surgery. A meta-analysis was performed on studies in which data regarding patients with complications after early or standard physical therapy could be pooled; this was possible for four trials [9,17,24] that reported complications in patients who underwent lumbar interbody fusion and for five trials [8,20,21,23,26] that reported complications in patients who underwent lumbar discectomy.
In the lumbar interbody fusion case, the observed log odds ratios ranged from −1.8412 to 1.0537, with the majority of estimates being negative (50%). The estimated average log odds ratio based on the random-effects model was 0.1959 (95% CI: −0.8756 to 1.2675). Therefore, the average outcome did not differ significantly from zero (z = 0.3584, p = 0.7201). According to the Q-test, there was no significant amount of heterogeneity in the true outcomes (Q(3) = 4.8407, p = 0.1838, tau2 = 0.4351, I2 = 37.4998%). A 95% prediction interval for the true outcomes was given as −1.4832 to 1.8751. Hence, although the average outcome was estimated to be positive, in some studies, the true outcome may in fact be negative. An examination of the studentized residuals revealed that none of the studies had a value larger than ± 2.4977, and hence there was no indication of outliers in the context of this model. According to Cook’s distances, none of the studies could be considered to be overly influential. Neither the rank correlation nor the regression test indicated any funnel plot asymmetry (p = 0.7500 and p = 0.3939, respectively) (Figure 6).
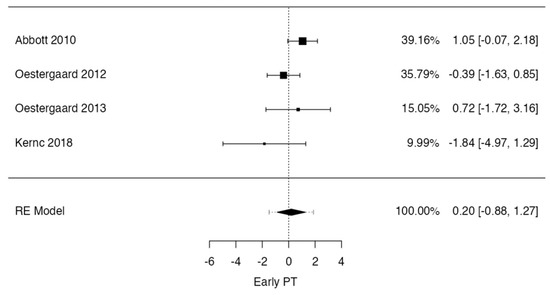
Figure 6.
Forrest plot representation of the meta–analysis for complications after lumbar interbody fusion and physical therapy [9,18,20,24].
In the lumbar discectomy case, the observed log odds ratios ranged from −0.7191 to 0.9589, with the majority of estimates being negative (60%). The estimated average log odds ratio based on the random-effects model was −0.2665 (95% CI: −1.2433 to 0.7103). Therefore, the average outcome did not differ significantly from zero (z = −0.5348, p = 0.5928). According to the Q-test, there was no significant amount of heterogeneity in the true outcomes (Q(4) = 1.2941, p = 0.8624, tau2 = 0.0000, I2 = 0.0000%). An examination of the studentized residuals revealed that none of the studies had a value larger than ±2.5758, and hence there was no indication of outliers in the context of this model. According to Cook’s distances, none of the studies could be considered to be overly influential. Neither the rank correlation nor the regression test indicated any funnel plot asymmetry (p = 0.2333 and p = 0.7005, respectively) (Figure 7).
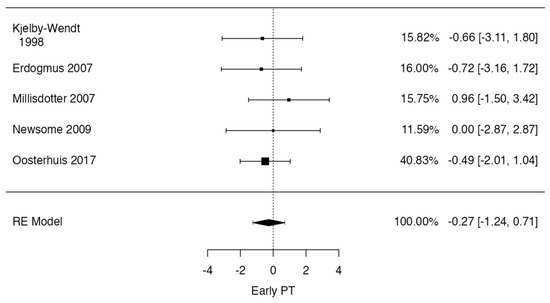
Figure 7.
Forrest plot representation of the meta–analysis for complications after lumbar discectomy and physical therapy [8,14,16,17,23].
4. Discussion
Postoperative rehabilitation encompasses a diverse assortment of practices across different contexts. For certain practitioners, it consists merely in distributing a brochure accompanied by patient education to engage in walking. In contrast, European institutions frequently adopt a “Back Café” methodology [27], integrating psychosocial support alongside physical exercises. Alternatively, some propose a rigorous regimen of isometric strengthening exercises [18,19,22]. This work has analyzed the limited literature specifically dedicated to rehabilitation subsequent to lumbar discectomy or spinal fusion for intervertebral disc disease, seeking to determine the outcomes of early physical therapy after surgery for intervertebral disc disease. The timing for the optimal initiation of physical therapy was limited to a maximum of 4 weeks postoperatively for lumbar discectomy and 6 weeks for lumbar interbody fusion, obtaining moderate-quality evidence that comprehensive early rehabilitation is both safe and effective.
In instances where adverse events are not invariably predictable, factors including patient characteristics, surgical procedures, indications, the type of physical therapy, and the timing of its initiation can be modulated and have a considerable impact on patient outcomes. This meta-analysis shows that early physical therapy does not present a significantly major risk of adverse events, both for lumbar discectomy and lumbar interbody fusion, when compared to the standard initiation of psychical therapy. These results can be highlighted by the relatively consistent direction of the outcomes shown among the included studies. Specifically, certain studies [15,23,26] suggested that complications were almost evenly distributed across the groups or slightly in favor of early physical therapy, yet never achieving a statistically significant difference. The dichotomous models in the meta-analysis indeed confirm this trend, both for lumbar discectomy and lumbar interbody fusion.
Post-physical therapy low back pain can represent a challenge for patients undergoing lumbar discectomy or lumbar intervertebral fusion procedures, manifesting with a highly variable incidence rate ranging from 3% to 43% [28,29]. Indeed, the surgical treatment involves subperiosteal decortication and the removal of bone segments from the vertebrae. This can induce muscular atrophy, weakness [30], diminished range of motion [31], and pain, leading to a fear of movement, stiffness, and an increased level of disability [32]. Hence, the impact on postoperative physical and mental health may extend beyond the initial expectations. Consequently, various rehabilitation programs have been developed to hasten symptom resolution, particularly pain, facilitate functional recovery and a return to employment, offer reassurance to patients, and, ultimately, prevent chronic pain, complications, and recurrences [33]. Our work reported discordant results in terms of low back pain after early physical therapy for lumbar interbody fusion, showing the need for more randomized control trials on this topic to provide clear guidance on the optimal timing for initiating physical therapy. Conversely, when considering early physical therapy after lumbar discectomy, there is moderate evidence that early physical therapy reduces pain at 12 weeks and 12 months postoperatively. These findings are consistent with those obtained by other reviews, which suggested that therapeutic programs should start between 4 and 6 weeks postoperatively [34].
4.1. Limitations of the Study
This work does not come without limitations. One is that we found quite consistent heterogeneity in the duration, intensity, type, and timing of initiation of the physical therapy interventions. The heterogeneity in the timing of initiation can potentially cause a significant limitation. However, the majority of the included studies [8,15,18,20,21,22,23,25,26] began within the first two postoperative weeks, and four [15,18,23,25] began within the first postoperative day, thereby reducing the impact of heterogeneity on our results. Nevertheless, it is imperative to exercise caution when acknowledging that the studies included in this review employed a diverse array of physical therapy protocols, extending from basic muscle strengthening exercises to sophisticated regimes incorporating both physical therapy and psychomotor education.
Overall, the effectiveness of postoperative physical therapy in improving patient outcomes after lumbar surgery can greatly depend on the healthcare context of the region, highlighting the need for adaptable and resource-sensitive approaches in global spinal care. In developed countries, especially those with robust healthcare infrastructures close to metropolitan areas, postoperative rehabilitation programs are often comprehensive and standardized, featuring the latest in physiotherapeutic techniques and equipment. Patients in these areas typically have access to a range of specialists and multimodal therapies, which can lead to faster and more effective recovery outcomes.
Conversely, in developing countries or rural regions distant from large cities, physical therapy protocols post-surgery can be less consistent, with variations in the availability of specialized care and resources. Rehabilitation services might be more generic, less frequent, or rely heavily on patient self-management due to limited access to specialized healthcare facilities and professionals. This discrepancy can affect the speed and quality of recovery, potentially leading to longer periods of disability and higher rates of complications.
Despite this variability, a unifying philosophical approach was evident across all the included studies. Specifically, they conducted comparisons between cohorts that engaged in early initiation of any form of physical therapy and those patients who either commenced physical therapy at a later stage or did not participate in any physical therapy interventions. Another limitation is that only a small number of reported complications were reported by all the included studies, limiting the potential of picturing all adverse events that a patient can experience starting early physical therapy, particularly if these complications are unrelated to the surgical technique or spine exposure. However, the strength of this work is that it focused on clinically relevant parameters for patients, such as pain, function and disability, return to work, and possible complications, offering moderate evidence that early physical therapy could be beneficial for different aspects relevant to the patients.
4.2. Conclusions of the Study
This review indicates that employing early rehabilitation strategies for intervertebral disc disease could enhance results in terms of pain and disability without an enhanced risk of complications. However, it is evident there is a lack of randomized controlled trials (RCTs) on post-surgery rehabilitation for lumbar interbody fusion procedures, along with a significant diversity in the interventions proposed. There is a need for more research into the efficacy of integrative pre- and post-surgery rehabilitation programs to identify the most opportune moment to commence physical therapy following surgical procedures and understand the long-term impacts of these programs. Enhancing the quality of research in this area is crucial.
Author Contributions
Conceptualization, M.M. and A.R.; methodology, G.V.; software, M.I.; validation, M.T., A.R., and M.M.; formal analysis, M.M.; investigation, M.M.; resources, F.V.; data curation, A.C.; writing—original draft preparation, A.C. and I.S.G.; writing—review and editing, M.M., G.V., and M.T.; visualization, I.S.G.; supervision, C.F.; project administration, C.F.; funding acquisition, C.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Institutional review board approval was not required because this study retrieved and synthesized data from already published studies.
Informed Consent Statement
Patient consent was not required because this study retrieved and synthesized data from already published studies.
Data Availability Statement
Data are available, with adequate reason, upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fehlings, M.G.; Tetreault, L.; Nater, A.; Choma, T.; Harrop, J.; Mroz, T.; Santaguida, C.; Smith, J.S. The Aging of the Global Population: The Changing Epidemiology of Disease and Spinal Disorders. Neurosurgery 2015, 77, S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) Approach to Healthy Ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, S.; Pumberger, M.; Hughes, A.; Girardi, F. Degenerative Scoliosis: A Review. HSS J. 2011, 7, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Zimmerman, Z.E.; Mass, H.; Makhni, M.C. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. Jama 2022, 327, 1688–1699. [Google Scholar] [CrossRef] [PubMed]
- Aebi, M. The Adult Scoliosis. Eur. Spine J. 2005, 14, 925–948. [Google Scholar] [CrossRef]
- Ostelo, R.W.; De Vet, H.C.; Waddell, G.; Kerckhoffs, M.R.; Leffers, P.; Van Tulder, M. Rehabilitation Following First-Time Lumbar Disc Surgery. Spine 2003, 28, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Snowdon, M.; Peiris, C.L. Physiotherapy Commenced Within the First Four Weeks Post-Spinal Surgery Is Safe and Effective: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2016, 97, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Millisdotter, M.; Strömqvist, B. Early Neuromuscular Customized Training after Surgery for Lumbar Disc Herniation: A Prospective Controlled Study. Eur. Spine J. 2007, 16, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Oestergaard, L.G.; Nielsen, C.V.; Bünger, C.E.; Sogaard, R.; Fruensgaard, S.; Helmig, P.; Christensen, F.B. The Effect of Early Initiation of Rehabilitation after Lumbar Spinal Fusion: A Randomized Clinical Study. Spine 2012, 37, 1803–1809. [Google Scholar] [CrossRef]
- Zaed, I.; Bossi, B.; Ganau, M.; Tinterri, B.; Giordano, M.; Chibbaro, S. Current State of Benefits of Enhanced Recovery After Surgery (ERAS) in Spinal Surgeries: A Systematic Review of the Literature. Neurochirurgie 2022, 68, 61–68. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Hodgkinson, M. The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. Available online: http://www.cebm.net/index.aspx?o=5653 (accessed on 3 March 2024).
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the International Prospective Register of Systematic Reviews (PROSPERO) of Systematic Review Protocols Was Associated with Increased Review Quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Crocker, T.F.; Lam, N.; Jordão, M.; Brundle, C.; Prescott, M.; Forster, A.; Ensor, J.; Gladman, J.; Clegg, A. Risk-of-Bias Assessment Using Cochrane’s Revised Tool for Randomized Trials (RoB 2) Was Useful but Challenging and Resource-Intensive: Observations from a Systematic Review. J. Clin. Epidemiol. 2023, 161, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Kjellby-Wendt, G.; Styf, J. Early Active Training after Lumbar Discectomy: A Prospective, Randomized, and Controlled Study. Spine 1998, 23, 2345–2351. [Google Scholar] [CrossRef] [PubMed]
- Oestergaard, L.G.; Nielsen, C.V.; Bünger, C.E.; Svidt, K.; Christensen, F.B. The Effect of Timing of Rehabilitation on Physical Performance after Lumbar Spinal Fusion: A Randomized Clinical Study. Eur. Spine J. 2013, 22, 1884–1890. [Google Scholar] [CrossRef] [PubMed]
- Oestergaard, L.G.; Christensen, F.B.; Nielsen, C.V.; Bünger, C.E.; Fruensgaard, S.; Sogaard, R. Early versus Late Initiation of Rehabilitation after Lumbar Spinal Fusion: Economic Evaluation alongside a Randomized Controlled Trial. Spine 2013, 38, 1979–1985. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Zhang, S.J.; Wang, X.J. Postoperative Functional Exercise for Patients Who Underwent Percutaneous Transforaminal Endoscopic Discectomy for Lumbar Disc Herniation. Eur. Rev. Med. Pharmacol. Sci. 2021, 22, 15–22. [Google Scholar] [CrossRef]
- Kernc, D.; Strojnik, V.; Vengust, R. Early Initiation of a Strength Training Based Rehabilitation after Lumbar Spine Fusion Improves Core Muscle Strength: A Randomized Controlled Trial. J. Orthop. Surg. Res. 2018, 13, 151. [Google Scholar] [CrossRef] [PubMed]
- Kjellby-Wendt, G.; Styf, J.; Carlsson, S.G. Early Active Rehabilitation after Surgery for Lumbar Disc Herniation: A Prospective, Randomized Study of Psychometric Assessment in 50 Patients. Acta Orthop. Scand. 2001, 72, 518–524. [Google Scholar] [CrossRef]
- Erdogmus, C.B.; Resch, K.L.; Sabitzer, R.; Müller, H.; Nuhr, M.; Schöggl, A.; Posch, M.; Osterode, W.; Ungersböck, K.; Ebenbichler, G.R. Physiotherapy-Based Rehabilitation Following Disc Herniation Operation: Results of a Randomized Clinical Trial. Spine 2007, 32, 2041–2049. [Google Scholar] [CrossRef]
- Ju, S.; Park, G.; Kim, E. Effects of an Exercise Treatment Program on Lumbar Extensor Muscle Strength and Pain of Rehabilitation Patients Recovering from Lumbar Disc Herniation Surgery. J. Phys. Ther. Sci. 2012, 24, 515–518. [Google Scholar] [CrossRef]
- Newsome, R.J.; May, S.; Chiverton, N.; Cole, A.A. A Prospective, Randomised Trial of Immediate Exercise Following Lumbar Microdiscectomy: A Preliminary Study. Physiotherapy 2009, 95, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Abbott, A.D.; Tyni-Lenné, R.; Hedlund, R. Early Rehabilitation Targeting Cognition, Behavior, and Motor Function after Lumbar Fusion: A Randomized Controlled Trial. Spine 2010, 35, 848–857. [Google Scholar] [CrossRef] [PubMed]
- Ogutluler Ozkara, G.; Ozgen, M.; Ozkara, E.; Armagan, O.; Arslantas, A.; Atasoy, M.A. Effectiveness of Physical Therapy and Rehabilitation Programs Starting Immediately after Lumbar Disc Surgery. Turk. Neurosurg. 2015, 25, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Oosterhuis, T.; Ostelo, R.W.; van Dongen, J.M.; Peul, W.C.; de Boer, M.R.; Bosmans, J.E.; Vleggeert-Lankamp, C.L.; Arts, M.P.; van Tulder, M.W. Early Rehabilitation after Lumbar Disc Surgery Is Not Effective or Cost-Effective Compared to No Referral: A Randomised Trial and Economic Evaluation. J. Physiother. 2017, 63, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Christensen, F.B.; Laurberg, I.; Bünger, C.E. Importance of the Back-Café Concept to Rehabilitation after Lumbar Spinal Fusion: A Randomized Clinical Study with a 2-Year Follow-Up. Spine 2003, 28, 2561–2569. [Google Scholar] [CrossRef]
- Kahanovitz, N.; Viola, K.; Muculloch, J. Limited Surgical Discectomy and Microdiscectomy: A Clinical Comparison. Spine 1989, 14, 79–81. [Google Scholar] [CrossRef]
- Salame, K.; Lidar, Z. Minimally Invasive Approach to Far Lateral Lumbar Disc Herniation: Technique and Clinical Results. Acta Neurochir. 2010, 152, 663–668. [Google Scholar] [CrossRef]
- Pourtaheri, S.; Issa, K.; Lord, E.; Ajiboye, R.; Drysch, A.; Hwang, K.; Faloon, M.; Sinha, K.; Emami, A. Paraspinal Muscle Atrophy After Lumbar Spine Surgery. Orthopedics 2016, 39, e209–e214. [Google Scholar] [CrossRef]
- Arja, H.; Tiina, K.; Ulla, T.; Jari, Y. Trunk Muscle Strength in Flexion, Extension, and Axial Rotation in Patients Managed with Lumbar Disc Herniation Surgery and in Healthy Control Subjects. Spine 2003, 28, 1068–1073. [Google Scholar] [CrossRef]
- Choi, J.H.; Jang, J.S.; Yoo, K.S.; Shin, J.M.; Jang, I.T. Functional Limitations Due to Stiffness after Long-Level Spinal Instrumented Fusion Surgery to Correct Lumbar Degenerative Flat Back. Spine 2018, 43, 1044–1051. [Google Scholar] [CrossRef] [PubMed]
- Rushton, A.; Heneghan, N.R.; Calvert, M.; Heap, A.; White, L.; Goodwin, P.C. Physiotherapy Post Lumbar Discectomy: Prospective Feasibility and Pilot Randomised Controlled Trial. PLoS ONE 2015, 10, e0142013. [Google Scholar] [CrossRef] [PubMed]
- Oosterhuis, T.; Costa, L.O.P.; Maher, C.G.; de Vet, H.C.W.; van Tulder, M.W.; Ostelo, R.W.J.G. Rehabilitation after Lumbar Disc Surgery. Cochrane Database Syst. Rev. 2014, 2014, CD003007. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).