Feasibility Testing of the Automatic Design of Three-Unit Implant Fixed Dental Prostheses with Different Dental CAD Software: A Pre-Clinical Pilot Trial
Abstract
1. Introduction
2. Material & Methods
2.1. Study Setup
2.2. Study Setting
- A. Full-arch scan of the upper and lower jaws including bilateral bite registration with tooth 17;
- B. Full-arch scan of the upper and lower jaws including bilateral bite registration without tooth 17;
- C. Quadrant scan of the upper and lower jaws including unilateral bite registration with tooth 17;
- D. Quadrant scan of the upper and lower jaws including unilateral bite registration without tooth 17.
2.3. Manual Adjustments, Time Evaluation, and Visual Examination
2.4. Statistical Analyses
3. Results
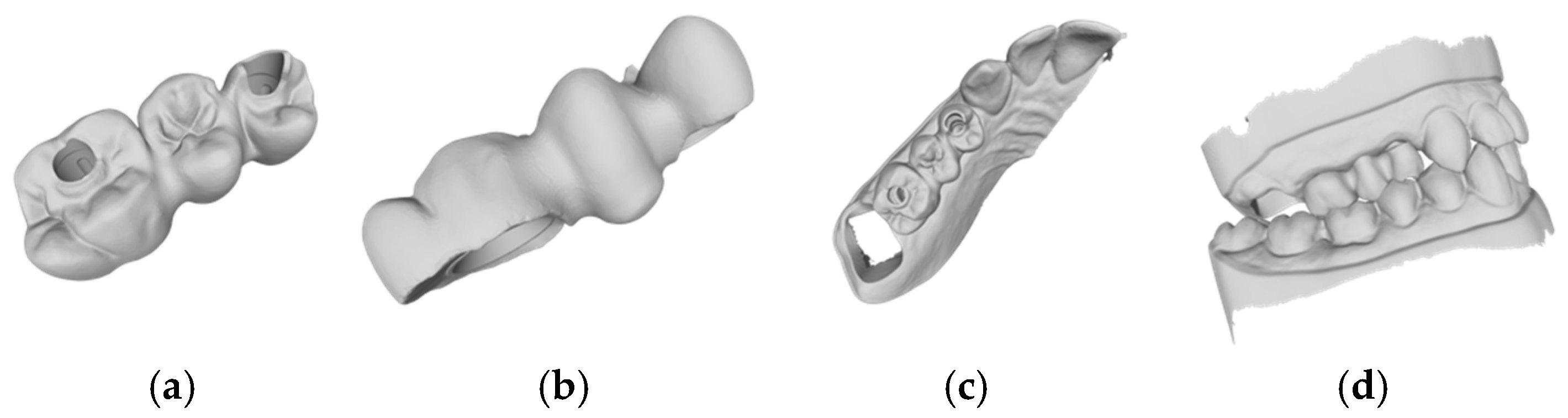
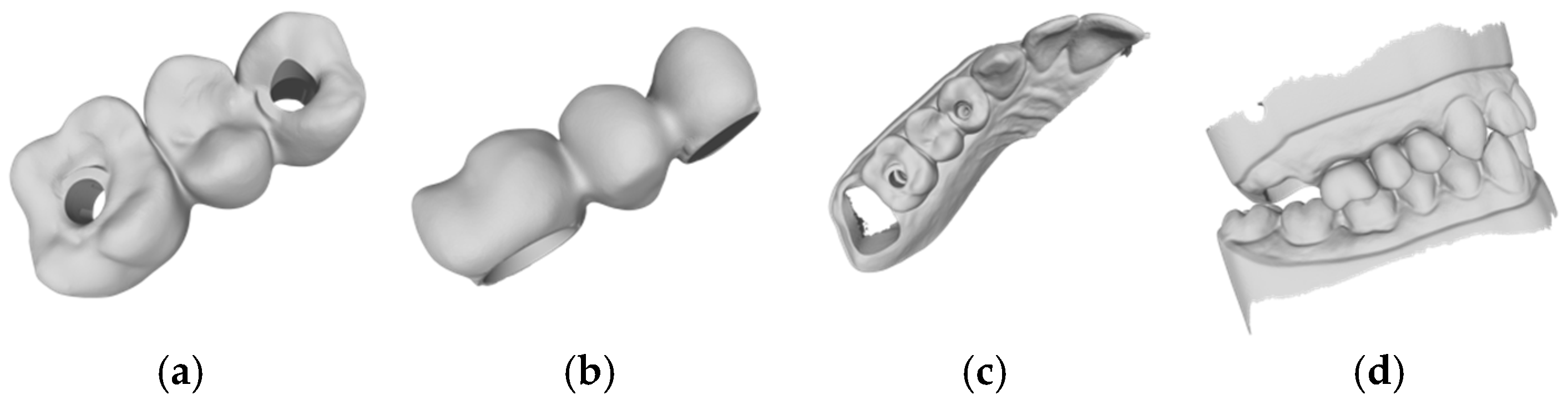
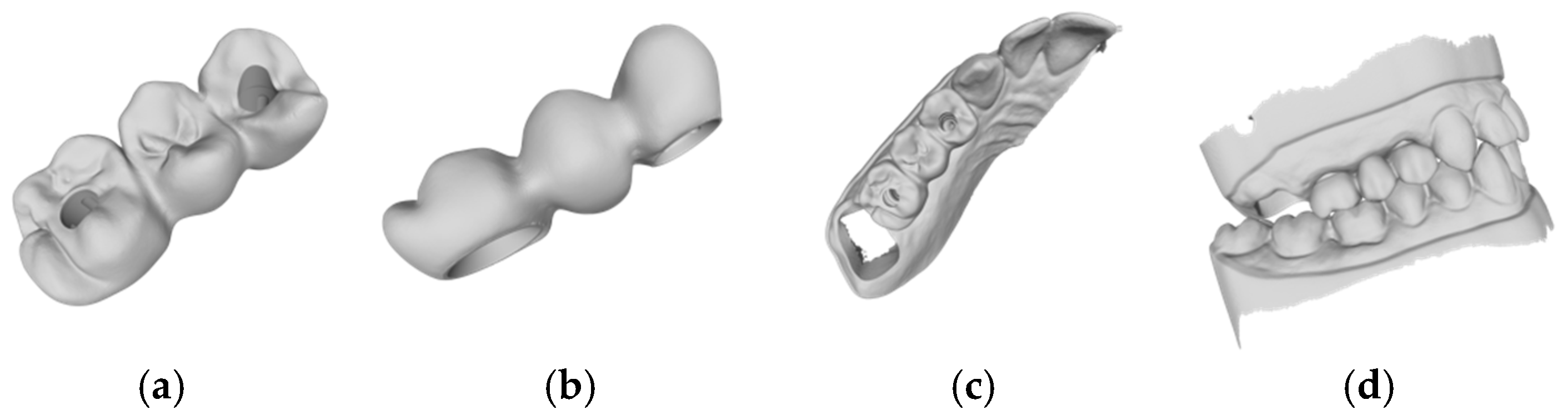
3.1. Results of the Automatic CAD Process
3.2. Time Efficiency
4. Discussion
4.1. Objective Assessment
4.2. Automatic Design
4.3. Time Efficiency
4.4. Artificial Intelligence
4.5. Limitations
4.6. Future
5. Conclusions
- The tested software systems were unable to automatically generate iFDP designs with clinically acceptable parameters.
- The manual adjustment of the automatically generated iFDP designs did not result in any significant difference in time efficiency compared to a fully manual design.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nicole, R. Wie tickt die Generation Z? Firmen Tappen im Dunkeln und Holen sich Generationen-Berater ins Haus. 2022. Available online: https://www.nzz.ch/wirtschaft/generation-z-firmen-holen-sich-generationen-berater-ins-haus-ld.1686557?reduced=true (accessed on 30 July 2023).
- Alauddin, M.S.; Baharuddin, A.S.; Ghazali, M.I.M. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare 2021, 9, 118. [Google Scholar] [CrossRef]
- Joda, T.; Yeung, A.W.K.; Hung, K.; Zitzmann, N.U.; Bornstein, M.M. Disruptive innovation in dentistry: What it is and what could be next. J. Dent. Res. 2021, 100, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: A comparative in vitro study. BMC Oral Health 2019, 19, 101. [Google Scholar] [CrossRef]
- Wang, F.; Tang, Q.; Xi, S.; Liu, R.; Niu, L. Comparison and evaluation of the morphology of crowns generated by biogeneric design technique with CEREC chairside system. PLoS ONE 2020, 15, e0227050. [Google Scholar] [CrossRef]
- Bohner, L.O.L.; Neto, P.T.; Ahmed, A.S.; Mori, M.; Lagana, D.C.; Sesma, N. CEREC Chairside System to Register and Design the Occlusion in Restorative Dentistry: A Systematic Literature Review. J. Esthet. Restor. Dent. 2016, 28, 208–220. [Google Scholar] [CrossRef]
- Erozan, Ç.; Ozan, O. Evaluation of the Precision of Different Intraoral Scanner-Computer Aided Design (CAD) Software Combinations in Digital Dentistry. Med. Sci. Monit. 2020, 26, e918529. [Google Scholar] [CrossRef]
- Joda, T.; Brägger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral Implant. Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef]
- Bernauer, S.A.; Zitzmann, N.U.; Joda, T. The Complete Digital Workflow in Fixed Prosthodontics Updated: A Systematic Review. Healthcare 2023, 11, 679. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, R.; Galli, M.; Chen, Z.; Mendonça, G.; Meirelles, L.; Wang, H.L.; Chan, H.L. Intraoral scanning reduces procedure time and improves patient comfort in fixed prosthodontics and implant dentistry: A systematic review. Clin. Oral Investig. 2021, 25, 6517–6531. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Zarone, F.; Ferrari, M. The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Oh, T.J.; Misch, C.E.; Wang, H.L. Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale. Clin. Oral Implant. Res. 2005, 16, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.L. The Role of Occlusion in Implant Therapy: A Comprehensive Updated Review. Implant. Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Saber, A.; Chakar, C.; Mokbel, N.; Nohra, J. Prevalence of Interproximal Contact Loss Between Implant-Supported Fixed Prostheses and Adjacent Teeth and Its impact on Marginal Bone Loss: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2020, 35, 625–630. [Google Scholar] [CrossRef]
- Yen, J.Y.; Kang, L.; Chou, I.C.; Lai, Y.L.; Lee, S.Y. Risk assessment of interproximal contact loss between implant-supported fixed prostheses and adjacent teeth: A retrospective radiographic study. J. Prosthet. Dent. 2022, 127, 86–92. [Google Scholar] [CrossRef]
- Johnson, G.K.; Leary, J.M. Pontic design and localized ridge augmentation in fixed partial denture design. Dent. Clin. N. Am. 1992, 36, 591–605. [Google Scholar] [CrossRef] [PubMed]
- Kazmi, S.M.R.; Iqbal, Z.; Muneer, M.U.; Riaz, S.; Zafar, M.S. Different pontic design for porcelain fused to metal fixed dental prosthesis: Contemporary guidelines and practice by general dental practitioners. Eur. J. Dent. 2018, 12, 375–379. [Google Scholar] [CrossRef]
- Arslan, Y.; Nemli, S.K.; Güngör, M.B.; Tamam, E.; Yılmaz, H. Evaluation of biogeneric design techniques with CEREC CAD/CAM system. J. Adv. Prosthodont. 2015, 7, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Litzenburger, A.P.; Hickel, R.; Richter, M.J.; Mehl, A.C.; Probst, F.A. Fully automatic CAD design of the occlusal morphology of partial crowns compared to dental technicians’ design. Clin. Oral Investig. 2013, 17, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, X.; Chen, M. Accurate extraction of outermost biological characteristic curves in tooth preparations with fuzzy regions. Comput. Biol. Med. 2018, 103, 208–219. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, T.; Zhou, Q.; Lu, Y. Comparison of the morphological accuracy of automatic crowns designed by multiple computer-aided design software programs with different levels of dentition information acquisition. J. Prosthet. Dent. 2023, 132, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Zhang, C.; Wang, Y.; Jiang, X.; Ren, S. Impact of scanning strategies on the accuracy of virtual interocclusal records in partially edentulous arch using intraoral scanner: An in vitro study. BMC Oral Health 2024, 24, 1184. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Çakmak, G.; Choi, J.; Lee, D.; Yoon, H.I.; Yilmaz, B.; Schimmel, M. Deep learning-designed implant-supported posterior crowns: Assessing time efficiency, tooth morphology, emergence profile, occlusion, and proximal contacts. J. Dent. 2024, 147, 105142. [Google Scholar] [CrossRef]
- Cho, J.H.; Çakmak, G.; Yi, Y.; Yoon, H.I.; Yilmaz, B.; Schimmel, M. Tooth morphology, internal fit, occlusion and proximal contacts of dental crowns designed by deep learning-based dental software: A comparative study. J. Dent. 2024, 141, 104830. [Google Scholar] [CrossRef]
- Chau, R.C.W.; Hsung, R.T.C.; McGrath, C.; Pow, E.H.N.; Lam, W.Y.H. Accuracy of artificial intelligence-designed single-molar dental prostheses: A feasibility study. J. Prosthet. Dent. 2024, 131, 1111–1117. [Google Scholar] [CrossRef] [PubMed]




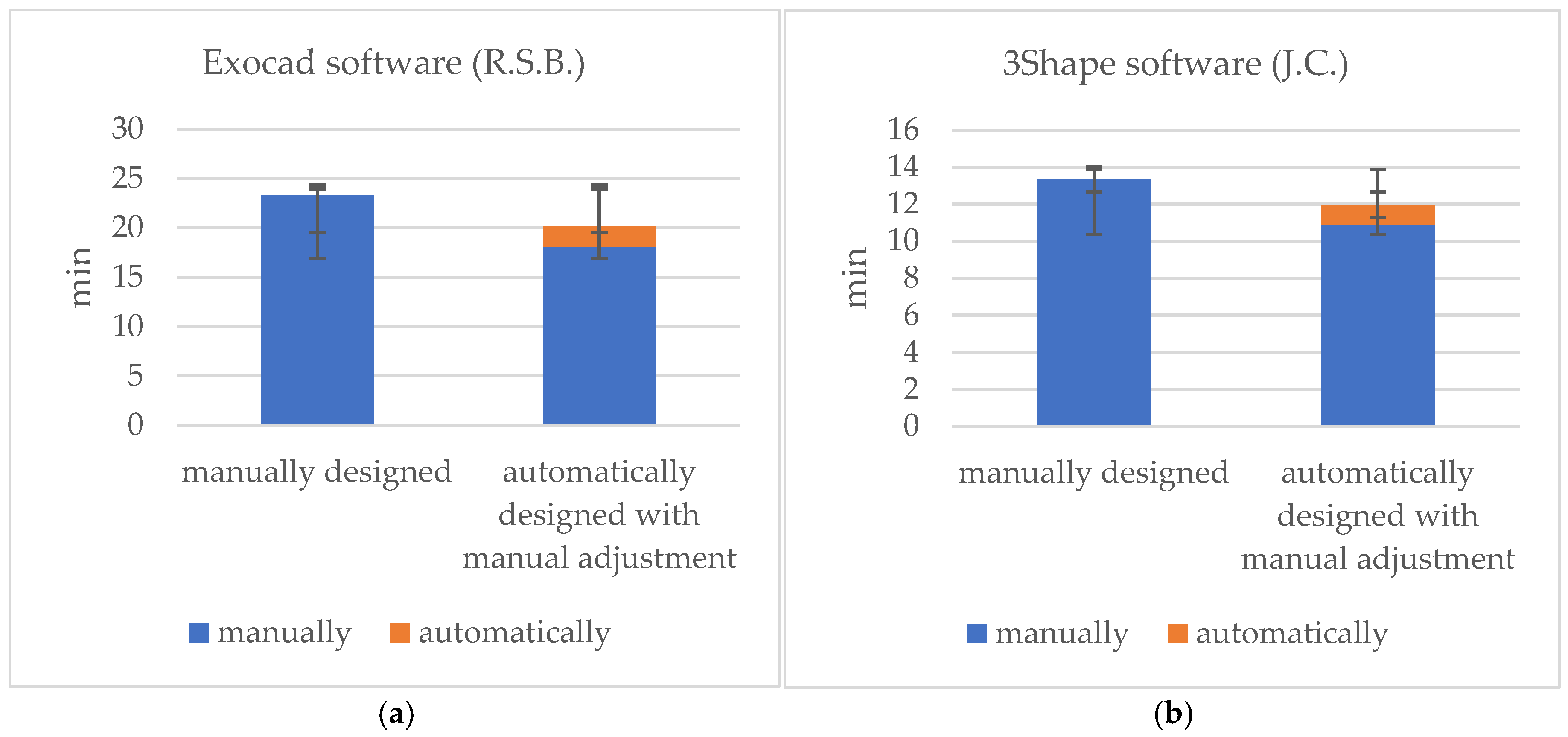
| Exocad (R.S.B.) | Manually | Automatically | Adjustment Time | 3Shape (J.C.) | Manually | Automatically | Adjustment Time |
|---|---|---|---|---|---|---|---|
| Group A | 22 min 51 s | 2 min 59 s | 13 min 21 s | Group A | 18 min 58 s | 1 min 10 s | 9 min 44 s |
| Group B | 19 min 56 s | 1 min 37 s | 19 min 47 s | Group B | 12 min 32 s | 1 min 12 s | 9 min 09 s |
| Group C | 23 min 58 s | 1 min 20 s | 21 min 41 s | Group C | 10 min 37 s | 1 min 05 s | 12 min 28 s |
| Group D | 26 min 23 s | 2 min 33 s | 17 min 21 s | Group D | 11 min 16 s | 54 s | 12 min 08 s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernauer, S.A.; Wieland, P.; Zitzmann, N.U.; Joda, T. Feasibility Testing of the Automatic Design of Three-Unit Implant Fixed Dental Prostheses with Different Dental CAD Software: A Pre-Clinical Pilot Trial. J. Clin. Med. 2025, 14, 233. https://doi.org/10.3390/jcm14010233
Bernauer SA, Wieland P, Zitzmann NU, Joda T. Feasibility Testing of the Automatic Design of Three-Unit Implant Fixed Dental Prostheses with Different Dental CAD Software: A Pre-Clinical Pilot Trial. Journal of Clinical Medicine. 2025; 14(1):233. https://doi.org/10.3390/jcm14010233
Chicago/Turabian StyleBernauer, Selina A., Philipp Wieland, Nicola U. Zitzmann, and Tim Joda. 2025. "Feasibility Testing of the Automatic Design of Three-Unit Implant Fixed Dental Prostheses with Different Dental CAD Software: A Pre-Clinical Pilot Trial" Journal of Clinical Medicine 14, no. 1: 233. https://doi.org/10.3390/jcm14010233
APA StyleBernauer, S. A., Wieland, P., Zitzmann, N. U., & Joda, T. (2025). Feasibility Testing of the Automatic Design of Three-Unit Implant Fixed Dental Prostheses with Different Dental CAD Software: A Pre-Clinical Pilot Trial. Journal of Clinical Medicine, 14(1), 233. https://doi.org/10.3390/jcm14010233









