Transsacral Bar Fixation for Osteoporotic H-Type Sacral Fractures: A Viable Alternative to Spinopelvic Fixation
Abstract
1. Introduction
- Iliosacral screws (IS): Minimally invasive and widely used, but biomechanical studies show that screw purchase is often insufficient in severely osteoporotic bone, leading to loosening or failure [10,21]. Cement augmentation may improve fixation strength but carries risks such as cement leakage and thermal injury [6].
- Trans-sacral bar (TSB) fixation: A bar spanning both sacroiliac joints achieves bicortical anchorage and distributes axial and torsional loads across the sacrum. This configuration is particularly attractive in osteoporotic bone, where the purchase of iliosacral screws alone is compromised [9,22]. Variants include single-bar, dual-bar, or hybrid constructs combining a TSB with bilateral iliosacral screws.
- Spinopelvic fixation (SPF): Lumbopelvic constructs provide maximal stability and are considered the traditional reference treatment in young patients with high-energy traumatic spinopelvic dissociations [23,24]. However, in elderly, frail patients, SPF carries considerable drawbacks—including longer operative times, increased blood loss, higher wound complication rates, and difficulties with postoperative mobilization [25,26].
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Patient Selection
- High-energy trauma mechanism;
- Pathological fractures due to metastatic disease, infection, or prior radiation therapy;
- Prior pelvic fixation;
- Incomplete imaging data or insufficient follow-up.
- FFP Type I—Isolated anterior pelvic ring fracture;
- FFP Type II—Non-displaced posterior ring fracture;
- FFP Type III—Unilateral displaced posterior ring fracture;
- FFP Type IV—Bilateral posterior ring involvement.
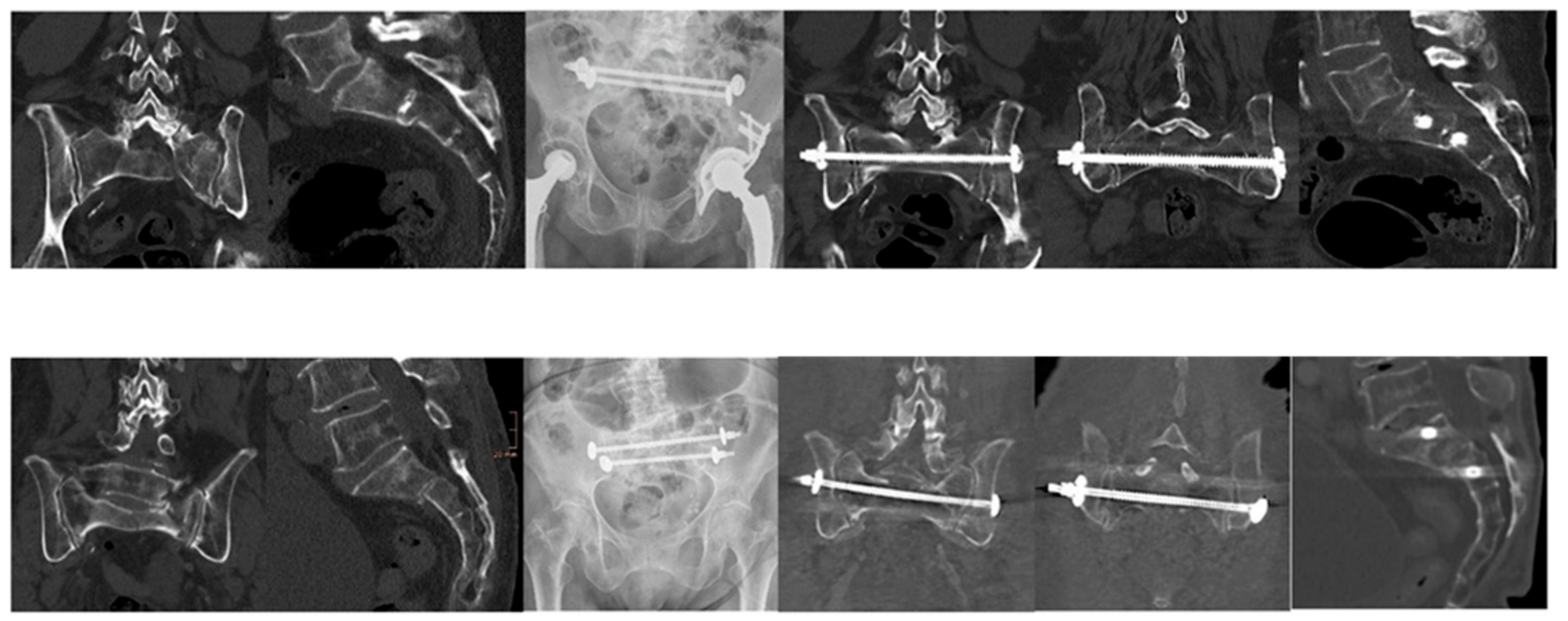
2.3. Surgical Technique
- Hybrid construct (TSB + bilateral iliosacral screws): A cannulated TSB (7.5 mm) was inserted percutaneously across the sacral body (typically S1) under navigated control. Two partially threaded iliosacral screws were then inserted bilaterally, usually at S1 but occasionally at S2 if anatomy dictated.
- Dual-bar construct (two parallel TSBs): In cases with adequate screw corridors or poor bone purchase, two parallel bars were introduced (S1 and S2). This configuration increased torsional resistance while maintaining a minimally invasive profile.
2.4. Data Collection and Variables
2.5. Bone Quality Assessment
- Circular regions of interest (ROIs) were placed in the L5 vertebral body trabecular bone, avoiding cortical margins and venous channels.
- If L5 was fractured or unsuitable, the nearest intact lumbar vertebra was chosen.
2.6. Postoperative Care and Rehabilitation
2.7. Follow-Up Protocol and Radiological Assessment
2.8. Outcome Measures
- Pain assessed on a numeric rating scale (NRS 0–10).
- Mobility, compared with pre-injury baseline (independent ambulation, walking aid, wheelchair, bedridden). Return to baseline was defined as functional recovery.
- Radiographic healing (union, absence of displacement, absence of implant failure).
- Complications, recorded according to Clavien–Dindo classification:
- o
- Intraoperative: bleeding, malposition, neurovascular injury.
- o
- Early postoperative (≤30 days): wound infection, hematoma, thromboembolism, pneumonia, urinary tract infection, delirium, new neurologic deficit.
- o
- Late postoperative (>30 days): implant loosening, migration, breakage, reoperation, new fractures, mortality.
- Length of stay (LOS).
- Survival: all-cause mortality at 30 days and 12 months.
2.9. Statistical Analysis
3. Results
3.1. Patient Demographics and Baseline Characteristics
3.2. Fracture Classification and Radiographic Findings
3.3. Surgical Management and Hospital Course
3.4. Intraoperative and Postoperative Complications
3.5. Opportunistic CT Bone Density (HU)
3.6. Postoperative Mobility and Rehabilitation
3.7. Follow-Up Pain and Implant Integrity
4. Discussion
4.1. Study Aim and Key Findings
4.2. Comparison with Literature
4.3. Fixation Strategies: Hybrid Versus Dual-Bar Constructs
4.4. Bone Quality and Osteoporosis Considerations
4.5. Safety Profile and Complications
4.6. Clinical and Economic Implications
4.7. Limitations
4.8. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SPF | Spinopelvic Fixation |
| TSB | Transsacral Bar |
| SIFs | Osteoporotic Sacral Insufficiency Fractures |
| FFP | Fragility Fractures of Pelvis |
| OF | Osteoporotic Fractures |
References
- Hemmann, P.; Friederich, M.; Bahrs, C.; Jacoby, J.; Körner, D. Substantial changes in fracture rates in German hospitals in 2018 compared with 2002: An epidemiological study. Arch. Orthop. Trauma Surg. 2022, 142, 1847–1857. [Google Scholar] [CrossRef]
- Rinne, P.P.; Laitinen, M.K.; Kannus, P.; Mattila, V.M. The incidence of pelvic fractures and related surgery in the Finnish adult population: A nationwide study of 33,469 patients between 1997 and 2014. Acta Orthop. 2020, 91, 587–592. [Google Scholar] [CrossRef]
- Lundin, N.; Huttunen, T.T.; Enocson, A.; Marcano, A.I.; Felländer-Tsai, L.; Berg, H.E. Epidemiology and mortality of pelvic and femur fractures—A nationwide register study of 417,840 fractures in Sweden across 16 years: Diverging trends for potentially lethal fractures. Acta Orthop. 2021, 92, 323–328. [Google Scholar] [CrossRef]
- Andrich, S.; Haastert, B.; Neuhaus, E.; Neidert, K.; Arend, W.; Ohmann, C.; Grebe, J.; Vogt, A.; Jungbluth, P.; Rösler, G.; et al. Epidemiology of pelvic fractures in Germany: Considerably high incidence rates among older people. PLoS ONE 2015, 10, e0139078. [Google Scholar] [CrossRef]
- Yamamoto, N.; Someko, H.; Nakashima, Y.; Nakao, S.; Kaneko, T.; Tsuge, T. Mortality following fragility fractures of the pelvis: Systematic review and meta-analysis. Injury 2025, 56, 112618. [Google Scholar] [CrossRef]
- Gewiess, J.; Albers, C.E.; Keel, M.J.B.; Frihagen, F.; Rommens, P.M.; Bastian, J.D. Chronic pelvic insufficiency fractures and their treatment. Arch. Orthop. Trauma Surg. 2024, 145, 76. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, L.; de Jongh, M.A.; De Munter, L.; Edwards, M.; Lansink, K.W.W. Prognostic factors and quality of life after pelvic fractures. The Brabant Injury Outcome Surveillance (BIOS) study. PLoS ONE 2020, 15, e0233690. [Google Scholar] [CrossRef]
- Rommens, P.M.; Hofmann, A. Fragility fractures of the pelvis: An update. J. Musculoskelet. Surg. Res. 2023, 7, 1–10. [Google Scholar] [CrossRef]
- Wagner, D.; Kisilak, M.; Porcheron, G.; Krämer, S.; Mehling, I.; Hofmann, A.; Rommens, P.M. Trans-sacral bar osteosynthesis provides low mortality and high mobility in patients with fragility fractures of the pelvis. Sci. Rep. 2021, 11, 14201. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Gomez, S.; Wahl, L.; Blecher, R.; Olewnik, Ł.; Iwanaga, J.; Maulucci, C.M.; Dumont, A.S.; Tubbs, R.S. Sacral fractures: An updated and comprehensive review. Injury 2021, 52, 366–375. [Google Scholar] [CrossRef]
- Yamauchi, T.; Sharma, S.; Chandra, S.; Tanaka, M.; Fujiwara, Y.; Arataki, S.; Sharma, A.; Yokoyama, Y.; Oomori, T.; Kanamaru, A.; et al. Superiority of MRI for evaluation of sacral insufficiency fracture. J. Clin. Med. 2022, 11, 4968. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Arand, C.; Hopf, J.C.; Mehling, I.; Dietz, S.O.; Wagner, D. Progress of instability in fragility fractures of the pelvis: An observational study. Injury 2019, 50, 1966–1973. [Google Scholar] [CrossRef] [PubMed]
- Andresen, J.R.; Radmer, S.; Andresen, R.; Prokop, A.; Schröder, G.; Nissen, U.; Schober, H.C. Comparative outcome of different treatment options for fragility fractures of the sacrum. BMC Musculoskelet. Disord. 2022, 23, 1106. [Google Scholar] [CrossRef]
- Ebeling, P.R.; Nguyen, H.H.; Aleksova, J.; Vincent, A.J.; Wong, P.; Milat, F. Secondary osteoporosis. Endocr. Rev. 2022, 43, 240–313. [Google Scholar] [CrossRef]
- Seeman, E. Pathogenesis of bone fragility in women and men. Lancet 2002, 359, 1841–1850. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, Y.; Liu, Q.; Jiang, Z.; Zhou, H.; Wang, Q. Global burden of low bone mineral density related fractures in pre-and post-menopausal women from 1990 to 2021, with projections to 2050. Osteoporos. Int. 2025, 1–13. [Google Scholar] [CrossRef]
- Xiao, P.-L.; Cui, A.-Y.; Hsu, C.-J.; Peng, R.; Jiang, N.; Xu, X.-H.; Ma, Y.-G.; Liu, D.; Lu, H.-D. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: A systematic review and meta-analysis. Osteoporos. Int. 2022, 33, 2137–2153. [Google Scholar] [CrossRef]
- Wagner, D.; Kamer, L.; Sawaguchi, T.; Richards, R.G.; Noser, H.; Rommens, P.M. Sacral bone mass distribution assessed by averaged three-dimensional CT models: Implications for pathogenesis and treatment of fragility fractures of the sacrum. JBJS 2016, 98, 584–590. [Google Scholar] [CrossRef]
- Linstrom, N.J.; Heiserman, J.E.; Kortman, K.E.; Crawford, N.R.; Baek, S.; Anderson, R.L.; Pitt, A.M.; Karis, J.P.; Ross, J.S.; Lekovic, G.P.; et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine 2009, 34, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Naisan, M.; Kramer, A.; Noufal, Y.; Afghanyar, Y.; Richter, M.; Drees, P.; Hartung, P. CT-Derived Bone Density as an Adjunct Predictor of Sacral Fracture Complexity in Older Adults. Injury 2025, 56, 112576. [Google Scholar] [CrossRef]
- Naisan, M.; Kramer, A.; Kindel, S.; Richter, M.; Ringel, F.; Hartung, P. Comparing different minimally invasive screw osteosyntheses methods for the stabilization of the sacral fractures. Injury 2025, 56, 112317. [Google Scholar] [CrossRef]
- Mehling, I.; Hessmann, M.H.; Rommens, P.M. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury 2012, 43, 446–451. [Google Scholar] [CrossRef]
- Brodell, J.D., Jr.; Lawlor, M.C.; Santangelo, G.; Kulp, A.; Haddas, R.; Mbagwu, C.; Benn, L.; Mesfin, A. Percutaneous lumbopelvic fixation is effective in the management of unstable transverse sacral fractures. Injury 2024, 55, 111825. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.K.; Quinnan, S.M. Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns. J. Orthop. Trauma 2016, 30, e318–e324. [Google Scholar] [CrossRef]
- Arshad, R.; Moglo, K.; El-Rich, M.; Schmidt, H. Spinal loads during dynamic full flexion and return to standing posture in different age and sex groups: A musculoskeletal model study. J. Biomech. 2024, 172, 112223. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Hassanzadeh, H.; Strike, S.A.; Menga, E.N.; Sponseller, P.D.; Kebaish, K.M. Pelvic fixation in adult and pediatric spine surgery: Historical perspective, indications, and techniques: AAOS exhibit selection. JBJS 2015, 97, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A. The FFP-classification: From eminence to evidence. Injury 2023, 54, S10–S19. [Google Scholar] [CrossRef]
- Ullrich, B.W.; Schnake, K.J.; Spiegl, U.J.A.; Mendel, T.; Behr, L.; Bula, P.; Flücht, L.B.; Franck, A.; Gercek, E.; Grüninger, S.; et al. OF-Pelvis classification of osteoporotic sacral and pelvic ring fractures. BMC Musculoskelet. Disord. 2021, 22, 992. [Google Scholar] [CrossRef]
- Godolias, P.; Plümer, J.; Cibura, C.; Dudda, M.; Schildhauer, T.A.; Chapman, J.R. Posterior pelvic ring injuries, lumbosacral junction instabilities and stabilization techniques for spinopelvic dissociation: A narrative review. Arch. Orthop. Trauma Surg. 2024, 144, 1627–1635. [Google Scholar] [CrossRef]
- Mendel, T.; Schenk, P.; Ullrich, B.W.; Hofmann, G.O.; Goehre, F.; Schwan, S.; Klauke, F. Mid-term outcome of bilateral fragility fractures of the sacrum after bisegmental transsacral stabilization versus spinopelvic fixation: A prospective study of two minimally invasive fixation constructs. Bone Jt. J. 2021, 103, 462–468. [Google Scholar] [CrossRef]
- Min, K.S.; Zamorano, D.P.; Wahba, G.M.; Garcia, I.; Bhatia, N.; Lee, T.Q. Comparison of two-transsacral-screw fixation versus triangular osteosynthesis for transforaminal sacral fractures. Orthopedics 2014, 37, e754–e760. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Value |
|---|---|
| Age, median (range) | 77.9 (66–89) years |
| Female, % | 87.1 |
| Male, % | 12.9 |
| Trauma mechanism | Fall 54.8%; Atraumatic 45.2% |
| Hounsfield Units (HU), mean | 75.8 ± 30.1 |
| FFP classification | FFP Type 4B (100%) |
| OF classification | OF Type 4 (100%) |
| Comminuted zone, % | 41.9 |
| Anterior ring involvement, % | 48.4 |
| Parameter | Value |
|---|---|
| Operative time, mean (range) | 71 min (41–110) |
| Hospital stay, mean (range) | 9.1 days (5–14) |
| Loosening rate, % | 0 |
| Walker at discharge, % | 61.3 |
| High walker at discharge, % | 12.9 |
| Crutches at discharge, % | 19.4 |
| Bedridden, % | 3.2 |
| Pain level at 3 months, mean | 1.9 |
| Pain level at 12 months, mean | 1.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naisan, M.; Schmitz, F.; Noufal, Y.; Afghanyar, Y.; Fröhlich, M.; Richter, M.; Drees, P.; Hartung, P. Transsacral Bar Fixation for Osteoporotic H-Type Sacral Fractures: A Viable Alternative to Spinopelvic Fixation. J. Clin. Med. 2025, 14, 6503. https://doi.org/10.3390/jcm14186503
Naisan M, Schmitz F, Noufal Y, Afghanyar Y, Fröhlich M, Richter M, Drees P, Hartung P. Transsacral Bar Fixation for Osteoporotic H-Type Sacral Fractures: A Viable Alternative to Spinopelvic Fixation. Journal of Clinical Medicine. 2025; 14(18):6503. https://doi.org/10.3390/jcm14186503
Chicago/Turabian StyleNaisan, Martin, Felix Schmitz, Yazan Noufal, Yama Afghanyar, Matthias Fröhlich, Marcus Richter, Philipp Drees, and Philipp Hartung. 2025. "Transsacral Bar Fixation for Osteoporotic H-Type Sacral Fractures: A Viable Alternative to Spinopelvic Fixation" Journal of Clinical Medicine 14, no. 18: 6503. https://doi.org/10.3390/jcm14186503
APA StyleNaisan, M., Schmitz, F., Noufal, Y., Afghanyar, Y., Fröhlich, M., Richter, M., Drees, P., & Hartung, P. (2025). Transsacral Bar Fixation for Osteoporotic H-Type Sacral Fractures: A Viable Alternative to Spinopelvic Fixation. Journal of Clinical Medicine, 14(18), 6503. https://doi.org/10.3390/jcm14186503





