Guided Personalized Surgery (GPS) in Posterostabilized Total Knee Replacement: A Radiological Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Characteristics
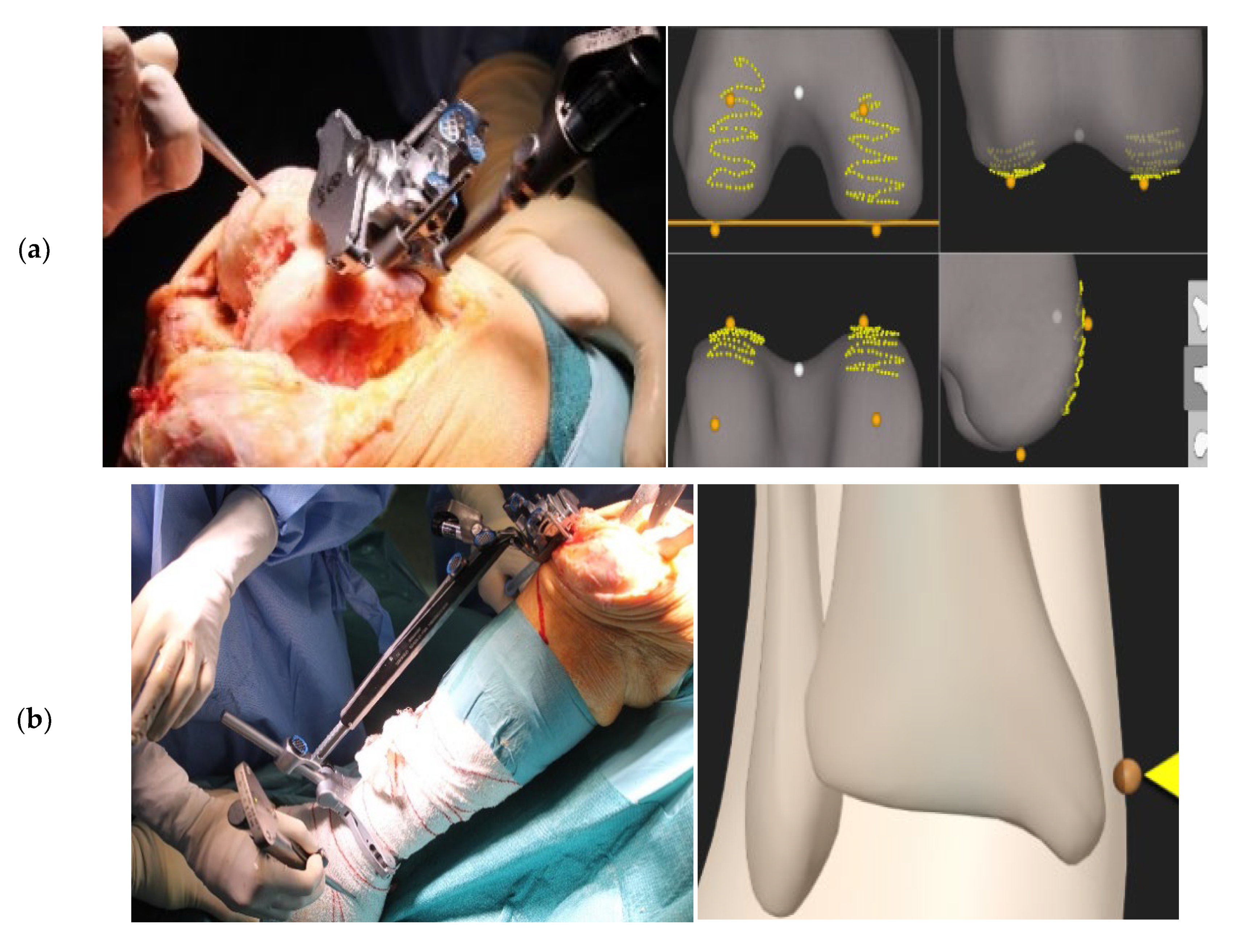
2.2. Surgical Technique
2.3. Study Variables
- The hip-knee-ankle (HKA), the mechanical lateral distal femoral angle (mLDFA), the mechanical medial proximal tibial angle (mMPTA), and the mechanical femorotibial angle (MFTA). The mLFDA and mMPTA angles were categorized as “Neutral” (mLFDA ≥ 87° and mMPTA ≥ 87°), “Varus of the tibia and femur” (mLFDA ≥ 90° and mMPTA < 87°) and “Valgus” (mLFDA < 87° and mMPTA ≥ 87°) [17,18].
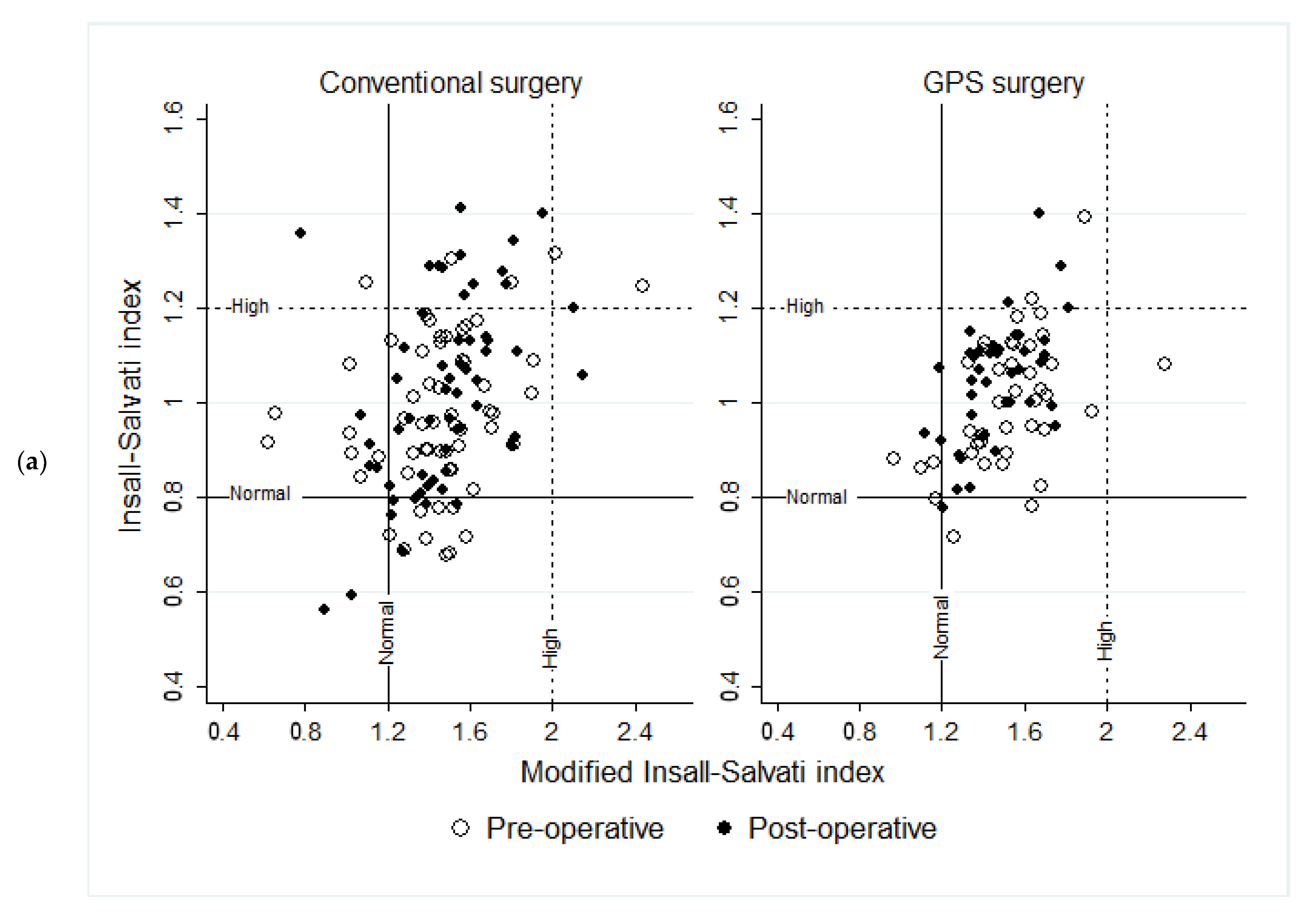
- The patellar height was evaluated with the Insall–Salvati index—IS (<0.8 low, 0.8–1.2 normal, >1.2 high), Insall–Salvati modified index—ISm (>2 high, 1.2–2.1 normal), the Caton–Deschamps index—CD (<0.6 low, 0.6–1.2 normal, >1.2 high), and the Blackburne–Peel index—BP (<0.5 low, 0.5–1 normal, >1 high) [15].
2.4. Statistical Analysis
3. Results
3.1. Participants Characteristics and Radiographic Assessment
3.1.1. General Characteristics
3.1.2. Radiographs Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, J.A.; Lewallen, D.G. Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet. Disord. 2014, 15, 127. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Ong, K.L.; Lau, E.; Widmer, M.; Maravic, M.; Gomez-Barrena, E.; de Pina Mde, F.; Manno, V.; Torre, M.; Walter, W.L.; et al. International survey of primary and revision total knee replacement. Int. Orthop. 2011, 35, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Matharu, G.S.; Culliford, D.J.; Blom, A.W.; Judge, A. Projections for primary hip and knee replacement surgery up to the year 2060: An analysis based on data from The National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Ind. Mark. Manag. 2022, 104, 443–448. [Google Scholar] [CrossRef]
- Skou, S.T.; Roos, E.M.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Simonsen, O.; Rasmussen, S. A Randomized, Controlled Trial of Total Knee Replacement. N. Engl. J. Med. 2015, 373, 1597–1606. [Google Scholar] [CrossRef]
- Nam, D.; Nunley, R.M.; Barrack, R.L. Patient dissatisfaction following total knee replacement: A growing concern? Bone Jt. J. 2014, 96-B, 96–100. [Google Scholar] [CrossRef]
- Cheng, T.; Zhao, S.; Peng, X.; Zhang, X. Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1307–1322. [Google Scholar] [CrossRef]
- Longstaff, L.M.; Sloan, K.; Stamp, N.; Scaddan, M.; Beaver, R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J. Arthroplast. 2009, 24, 570–578. [Google Scholar] [CrossRef]
- Hernández-Vaquero, D. The alignment of the knee replacement. Old myths and new controversies. Rev. Esp. Cir. Ortop. Traumatol. 2021, 65, 386–397. [Google Scholar] [CrossRef]
- Parratte, S.; Pagnano, M.W.; Trousdale, R.T.; Berry, D.J. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J. Bone Jt. Surg. Am. 2010, 92, 2143–2149. [Google Scholar] [CrossRef]
- Oussedik, S.; Abdel, M.P.; Victor, J.; Pagnano, M.W.; Haddad, F.S. Alignment in total knee arthroplasty. Bone Jt. J. 2020, 102-B, 276–279. [Google Scholar] [CrossRef]
- Carli, A.; Aoude, A.; Reuven, A.; Matache, B.; Antoniou, J.; Zukor, D.J. Inconsistencies between navigation data and radiographs in total knee arthroplasty are system-dependent and affect coronal alignment. Can. J. Surg. 2014, 57, 305–313. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Seo, S.S.; Seo, J.H.; Sohn, M.W.; Kim, Y.J. Differences in measurement of lower limb alignment among different registration methods of navigation and radiographs in TKA using the OrthoPilot system. Orthopedics 2012, 35, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Tigani, D.; Busacca, M.; Moio, A.; Rimondi, E.; Del Piccolo, N.; Sabbioni, G. Preliminary experience with electromagnetic navigation system in TKA. Knee 2009, 16, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Exatech. Logic Implants with Truliant Instruments Operative Technique. 2023. Available online: https://www.exac.com/wp-content/uploads/2024/09/712-35-30-RevB-Truliant-implants-with-LogicLPI-instruments-MDR_Web.pdf (accessed on 31 December 2024).
- Leon-Muñoz, V. Measurements Guide for Knee Prosthetic Surgery (Spanish) Sociedad Española de Rodilla (SEROD): Basic Formation Course 2.1.2 (Primary Knee Arthroplasty). 2021. Available online: https://serod.org/pdf/2.1.2_guia_mediciones.pdf (accessed on 31 December 2024).
- Ewald, F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin. Orthop. Relat. Res. 1989, 248, 9–12. [Google Scholar] [CrossRef]
- Almaawi, A.M.; Hutt, J.R.B.; Masse, V.; Lavigne, M.; Vendittoli, P.A. The Impact of Mechanical and Restricted Kinematic Alignment on Knee Anatomy in Total Knee Arthroplasty. J. Arthroplast. 2017, 32, 2133–2140. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chang, F.S.; Chen, K.H.; Huang, K.C.; Su, K.C. Mismatch between femur and tibia coronal alignment in the knee joint: Classification of five lower limb types according to femoral and tibial mechanical alignment. BMC Musculoskelet. Disord. 2018, 19, 411. [Google Scholar] [CrossRef]
- Tantavisut, S.; Amarase, C.; Ngarmukos, S.; Tanavalee, C.; Tanavalee, A. Knee joint line related to bony landmarks of the knee: A radiologic study in a Thai population. Knee Surg. Relat. Res. 2022, 34, 5. [Google Scholar] [CrossRef]
- Keshmiri, A.; Maderbacher, G.; Baier, C.; Sendtner, E.; Schaumburger, J.; Zeman, F.; Grifka, J.; Springorum, H.R. The influence of component alignment on patellar kinematics in total knee arthroplasty. Acta Orthop. 2015, 86, 444–450. [Google Scholar] [CrossRef]
- Fu, Y.; Wang, M.; Liu, Y.; Fu, Q. Alignment outcomes in navigated total knee arthroplasty: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1075–1082. [Google Scholar] [CrossRef]
- Kim, Y.H.; Park, J.W.; Kim, J.S. 2017 Chitranjan S. Ranawat Award: Does Computer Navigation in Knee Arthroplasty Improve Functional Outcomes in Young Patients? A Randomized Study. Clin. Orthop. Relat. Res. 2018, 476, 6–15. [Google Scholar] [CrossRef]
- Brin, Y.S.; Nikolaou, V.S.; Joseph, L.; Zukor, D.J.; Antoniou, J. Imageless computer assisted versus conventional total knee replacement. A Bayesian meta-analysis of 23 comparative studies. Int. Orthop. 2011, 35, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Hetaimish, B.M.; Khan, M.M.; Simunovic, N.; Al-Harbi, H.H.; Bhandari, M.; Zalzal, P.K. Meta-analysis of navigation vs conventional total knee arthroplasty. J. Arthroplast. 2012, 27, 1177–1182. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Bolch, C.; Jung, A.; Hamad, C.; Angibaud, L.; Stulberg, B.N.; Huddleston, J.I., 3rd. Accuracy and precision in resection alignment: Insights from 10,144 clinical cases using a contemporary computer-assisted total knee arthroplasty system. Knee 2020, 27, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Iacono, F.; Raspugli, G.F.; Filardo, G.; Bruni, D.; Zaffagnini, S.; Bignozzi, S.; Lo Presti, M.; Akkawi, I.; Neri, M.P.; Marcacci, M. The adductor tubercle: An important landmark to determine the joint line level in revision total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3212–3217. [Google Scholar] [CrossRef]
- van Lieshout, W.A.M.; Valkering, K.P.; Koenraadt, K.L.M.; van Etten-Jamaludin, F.S.; Kerkhoffs, G.; van Geenen, R.C.I. The negative effect of joint line elevation after total knee arthroplasty on outcome. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1477–1486. [Google Scholar] [CrossRef]
- Hannan, R.; Free, M.; Arora, V.; Harle, R.; Harvie, P. Accuracy of computer navigation in total knee arthroplasty: A prospective computed tomography-based study. Med. Eng. Phys. 2020, 79, 52–59. [Google Scholar] [CrossRef]
- Angibaud, L.D.; Dai, Y.; Liebelt, R.A.; Gao, B.; Gulbransen, S.W.; Silver, X.S. Evaluation of the Accuracy and Precision of a Next Generation Computer-Assisted Surgical System. Clin. Orthop. Surg. 2015, 7, 225–233. [Google Scholar] [CrossRef][Green Version]


| Conventional Surgery (n = 59) Mean ± SD n (%) | GPS (n = 41) Mean ± SD n (%) | p Value | |
|---|---|---|---|
| Age | 72.8 ± 8.1 | 71.9 ± 8.9 | 0.588 t |
| Female sex | 36 (61.0%) | 24 (58.5%) | 0.803 j |
| BMI | 31.6 ± 5.1 | 30.4 ± 5.2 | 0.455 u |
| Surgery characteristics | |||
| Primary TKR (yes) | 58 (98.3%) | 41 (100%) | 0.402 j |
Laterality:
| 39 (66.1%) 20 (33.9%) | 28 (68.3%) 13 (31.7%) | 0.819 j |
| Alignment Angle | Measure Time | Conventional Surgery n = 59 (Mean ± SD) | GPS Surgery n = 41 (Mean ± SD) | Mean Comparison, by Surgery Type | Variance Comparison, by Surgery Type |
|---|---|---|---|---|---|
| mLDFA (°) | Pre-Operative | 97.2 ± 2.8 | 97.9 ± 2.9 | p = 0.293 t | p = 0.819 t |
| Post-Operative | 95.1 ± 2.6 | 96.7 ± 2.3 | p = 0.003 t | p = 0.373 f | |
| Pre-Post mean comparison | p = 0.000 pt | p = 0.053 pt | |||
| Pre-Post variance comparison | p = 0.614 f | p = 0.150 f | |||
| mMPTA (°) | Pre-Operative | 86.6 ± 2.6 | 86.6 ± 3.1 | p = 0.921 t | p = 0.233 f |
| Post-Operative | 88.9 ± 2.5 | 88.3 ± 1.3 | p = 0.132 t | p = 0.000 f | |
| Pre-Post mean comparison | p = 0.000 pt | p = 0.002 pt | |||
| Pre-Post variance comparison | p = 0.611 f | p = 0.000 f | |||
| FTA (°) | Pre-Operative | 175.6 ± 4.0 | 174.4 ± 4.1 | p = 0.128 z | p = 0.807 w |
| Post-Operative | 175.5 ± 3.3 | 175.3 ± 2.4 | p = 0.340 z | p = 0.049 w | |
| Pre-Post mean comparison | p = 0.899 pt | p = 0.295 pt | |||
| Pre-Post variance comparison | p = 0.179 w | p = 0.016 w | |||
| HKA (°) | Pre-Operative | 183.9 ± 4.1 | 184.4 ± 4.5 | p = 0.520 t | p = 0.490 f |
| Post-Operative | 184 ± 3.4 | 185 ± 2.5 | p = 0.098 t | p = 0.039 f | |
| Pre-Post mean comparison | p = 0.834 pt | p = 0.616 pt | |||
| Pre-Post variance comparison | p = 0.157 f | p = 0.001 f |
| Index | Measure Time | Conventional Surgery n = 59 (Mean ± SD) | GPS Surgery n = 41 (Mean ± SD) | Mean Comparison, by Surgery | Variance Comparison, by Surgery |
|---|---|---|---|---|---|
| IS | Pre-Operative | 0.98 ± 0.2 | 0.99 ± 0.1 | p = 0.501 t | p = 0.237 f |
| Post-Operative | 1.02 ± 0.2 | 1.04 ± 0.1 | p = 0.431 t | p = 0.002 f | |
| Pre-Post mean comparison | p = 0.031 pt | p = 0.008 pt | |||
| Pre-Post variance comparison | p = 0.119 f | p = 0.596 f | |||
| ISm | Pre-Operative | 1.45 ± 0.3 | 1.52 ± 0.2 | p = 0.157 z | p = 0.561 w |
| Post-Operative | 1.48 ± 0.3 | 1.47 ± 0.2 | p = 0.842 t | p = 0.008 f | |
| Pre-Post mean comparison | p = 0.632 pt | p = 0.199 pt | |||
| Pre-Post variance comparison | p = 0.977 w | p = 0.067 f | |||
| CD | Pre-Operative | 0.83 ± 0.2 | 0.84 ± 0.2 | p = 0.472 z | p = 0.685 w |
| Post-Operative | 0.72 ± 0.2 | 0.77 ± 0.1 | p = 0.183 t | p = 0.011 f | |
| Pre-Post mean comparison | p = 0.000 pt | p = 0.011 pt | |||
| Pre-Post variance comparison | p = 0.023 w | p = 0.333 f | |||
| BP | Pre-Operative | 0.75 ± 0.2 | 0.77 ± 0.2 | p = 0.314 z | p = 0.575 w |
| Post-Operative | 0.69 ± 0.2 | 0.75 ± 0.1 | p = 0.099 t | p = 0.011 f | |
| Pre-Post mean comparison | p = 0.043 pt | p = 0.295 pt | |||
| Pre-Post variance comparison | p = 0.074 w | p = 0.584 f |
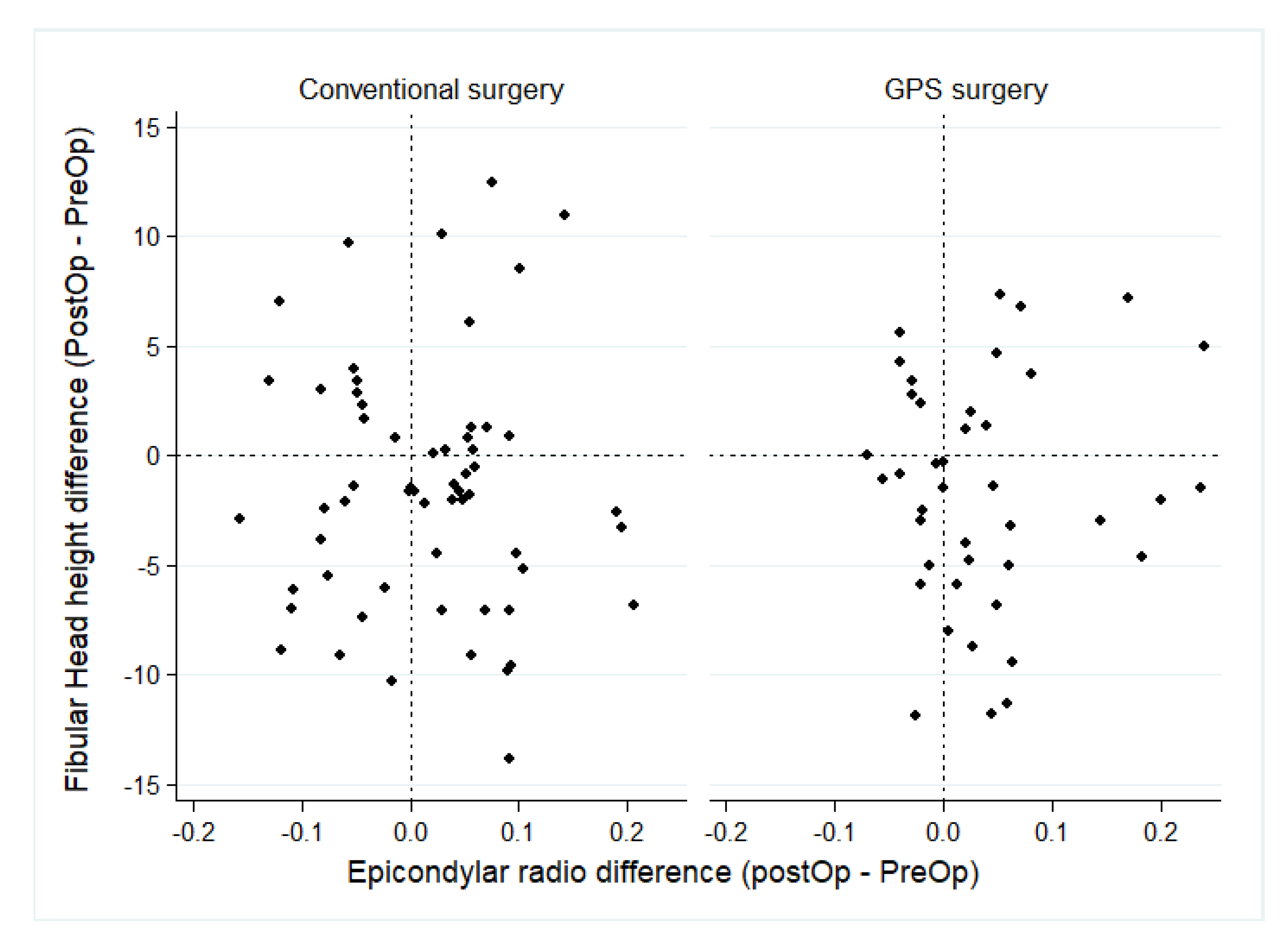
| Articular Joint Line | Measure Time | Conventional Surgery n = 59 (Mean ± SD) | GPS Surgery n = 41 (Mean ± SD) | Mean Comparison, by Surgery | Variance Comparison, by Surgery |
|---|---|---|---|---|---|
| ER | Pre-Operative | 0.62 ± 0.1 | 0.63 ± 0.1 | p = 0.378 z | p = 0.450 w |
| Post-Operative | 0.63 ± 0.1 | 0.66 ± 0.1 | p = 0.004 z | p = 0.004 w | |
| Pre-Post mean comparison | p = 0.179 pt | p = 0.004 pt | |||
| Pre-Post variance comparison | p = 0.289 f | p = 0.317 w | |||
| FH | Pre-Operative | 17.6 ± 5.1 | 17.3 ± 5.3 | p = 0.795 t | p = 0.791 f |
| Post-Operative | 16.1 ± 4.3 | 15.7 ± 3.8 | p = 0.634 t | p = 0.451 f | |
| Pre-Post mean comparison | p = 0.045 pt | p = 0.028 pt | |||
| Pre-Post variance comparison | p = 0.186 f | p = 0.044 f |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Andrés-Torán, A.; Padilla-Eguiluz, N.G.; Hernández-Esteban, P.; Gómez-Barrena, E. Guided Personalized Surgery (GPS) in Posterostabilized Total Knee Replacement: A Radiological Study. J. Clin. Med. 2025, 14, 429. https://doi.org/10.3390/jcm14020429
de Andrés-Torán A, Padilla-Eguiluz NG, Hernández-Esteban P, Gómez-Barrena E. Guided Personalized Surgery (GPS) in Posterostabilized Total Knee Replacement: A Radiological Study. Journal of Clinical Medicine. 2025; 14(2):429. https://doi.org/10.3390/jcm14020429
Chicago/Turabian Stylede Andrés-Torán, Ana, Norma G. Padilla-Eguiluz, Pablo Hernández-Esteban, and Enrique Gómez-Barrena. 2025. "Guided Personalized Surgery (GPS) in Posterostabilized Total Knee Replacement: A Radiological Study" Journal of Clinical Medicine 14, no. 2: 429. https://doi.org/10.3390/jcm14020429
APA Stylede Andrés-Torán, A., Padilla-Eguiluz, N. G., Hernández-Esteban, P., & Gómez-Barrena, E. (2025). Guided Personalized Surgery (GPS) in Posterostabilized Total Knee Replacement: A Radiological Study. Journal of Clinical Medicine, 14(2), 429. https://doi.org/10.3390/jcm14020429






