Three-Dimensional Posture Analysis-Based Modifications After Manual Therapy: A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
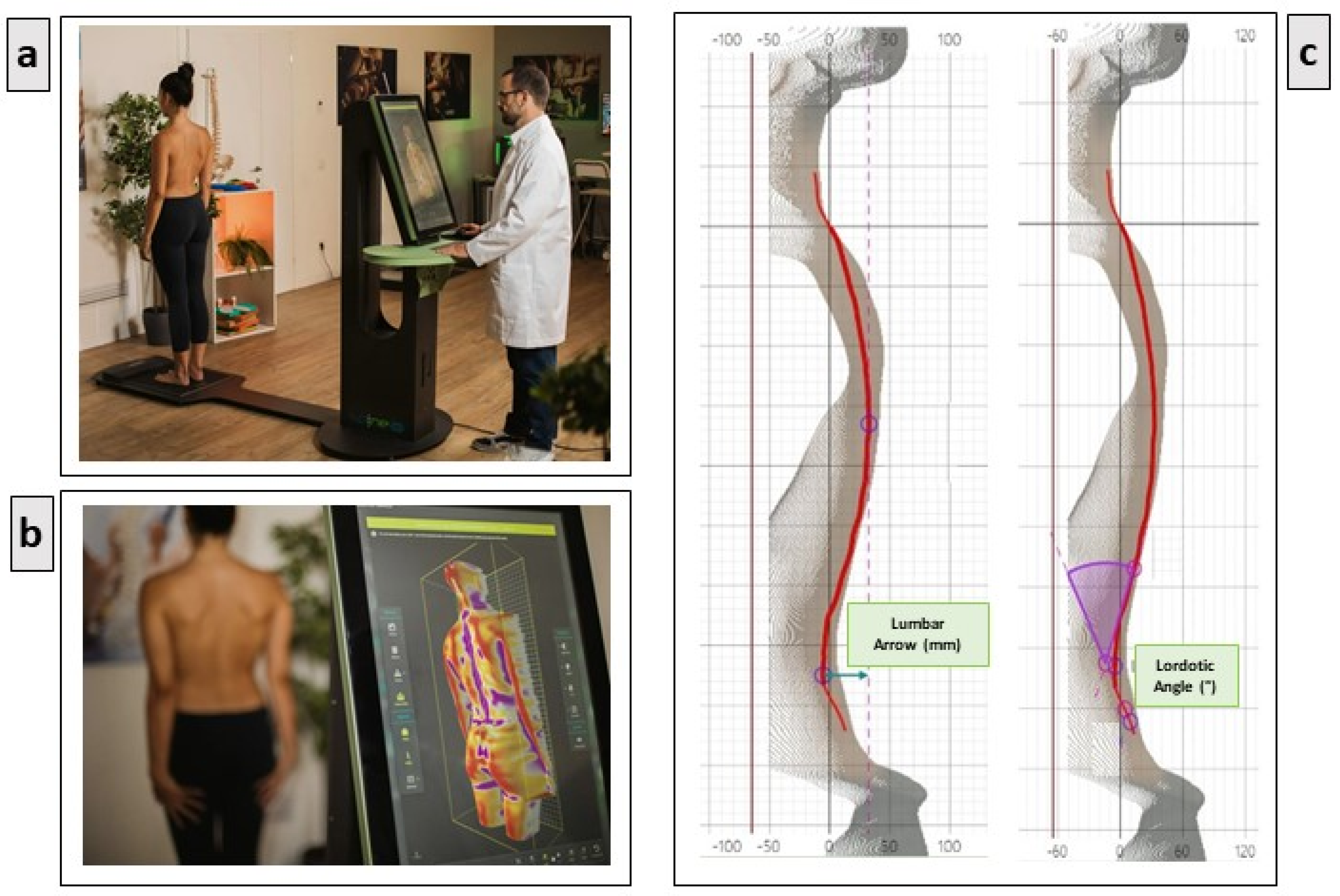
2.2. The Experimental Setup
2.3. Data Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Michalik, R.; Hamm, J.; Quack, V.; Eschweiler, J.; Gatz, M.; Betsch, M. Dynamic spinal posture and pelvic position analysis using a rasterstereographic device. J. Orthop. Surg. Res. 2020, 15, 389. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Ravalli, S.; Maugeri, G.; Bianco, A.; Palma, A.; Di Rosa, M.; Musumeci, G. Technological advancements in the analysis of human motion and posture management through digital devices. World J. Orthop. 2021, 12, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Drerup, B.; Hierholzer, E. Evaluation of frontal radiographs of scoliotic spines--Part I. Measurement of position and orientation of vertebrae and assessment of clinical shape parameters. J. Biomech. 1992, 25, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Bassani, T.; Stucovitz, E.; Galbusera, F.; Brayda-Bruno, M. Is rasterstereography a valid noninvasive method for the screening of juvenile and adolescent idiopathic scoliosis? Eur. Spine J. 2019, 28, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Molinaro, L.; Russo, L.; Cubelli, F.; Taborri, J.; Rossi, S. Reliability analysis of an innovative technology for the assessment of spinal abnormalities. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Messina, Italy, 22–24 June 2022; pp. 1–6. [Google Scholar]
- D’Amico, M.; Kinel, E.; Roncoletta, P. Normative 3D opto-electronic stereo-photogrammetric posture and spine morphology data in young healthy adult population. PLoS ONE 2017, 12, e0179619. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- with the Support of the Working Group; Carpinelli Mazzi, M.; Iavarone, A.; Russo, G.; Musella, C.; Milan, G.; D’Anna, F.; Garofalo, E.; Chieffi, S.; Sannino, M.; et al. Mini-Mental State Examination: New normative values on subjects in Southern Italy. Aging Clin. Exp. Res. 2020, 32, 699–702. [Google Scholar] [CrossRef]
- Tramontano, M.; Tamburella, F.; Dal Farra, F.; Bergna, A.; Lunghi, C.; Innocenti, M.; Cavera, F.; Savini, F.; Manzo, V.; D’Alessandro, G. International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare 2021, 10, 28. [Google Scholar] [CrossRef]
- Consorti, G.; Castagna, C.; Tramontano, M.; Longobardi, M.; Castagna, P.; Di Lernia, D.; Lunghi, C. Reconceptualizing Somatic Dysfunction in the Light of a Neuroaesthetic Enactive Paradigm. Healthcare 2023, 11, 479. [Google Scholar] [CrossRef]
- Arcuri, L.; Consorti, G.; Tramontano, M.; Petracca, M.; Esteves, J.E.; Lunghi, C. “What you feel under your hands”: Exploring professionals’ perspective of somatic dysfunction in osteopathic clinical practice—A qualitative study. Chiropr. Man. Ther. 2022, 30, 32. [Google Scholar] [CrossRef]
- Castagna, C.; Consorti, G.; Turinetto, M.; Lunghi, C. Osteopathic Models Integration Radar Plot: A Proposed Framework for Osteopathic Diagnostic Clinical Reasoning. J. Chiropr. Humanit. 2021, 28, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Dal Farra, F.; Bergna, A.; Lunghi, C.; Bruini, I.; Galli, M.; Vismara, L.; Tramontano, M. Reported biological effects following Osteopathic Manipulative Treatment: A comprehensive mapping review. Complement. Ther. Med. 2024, 82, 103043. [Google Scholar] [CrossRef] [PubMed]
- Löken, L.S.; Wessberg, J.; Morrison, I.; McGlone, F.; Olausson, H. Coding of pleasant touch by unmyelinated afferents in humans. Nat. Neurosci. 2009, 12, 547–548. [Google Scholar] [CrossRef] [PubMed]
- Ledwoń, D.; Danch-Wierzchowska, M.; Bugdol, M.; Bibrowicz, K.; Szurmik, T.; Myśliwiec, A.; Mitas, A.W. Real-Time Back Surface Landmark Determination Using a Time-of-Flight Camera. Sensors 2021, 21, 6425. [Google Scholar] [CrossRef]
- Joshi, S.; Balthillaya, G.; Neelapala, Y.V.R. Immediate effects of cervicothoracic junction mobilization versus thoracic manipulation on the range of motion and pain in mechanical neck pain with cervicothoracic junction dysfunction: A pilot randomized controlled trial. Chiropr. Man. Ther. 2020, 28, 38. [Google Scholar] [CrossRef]
- Croy, I.; Sehlstedt, I.; Wasling, H.B.; Ackerley, R.; Olausson, H. Gentle touch perception: From early childhood to adolescence. Dev. Cogn. Neurosci. 2019, 35, 81–86. [Google Scholar] [CrossRef]
- Baroni, F.; Ruffini, N.; D’Alessandro, G.; Consorti, G.; Lunghi, C. The role of touch in osteopathic practice: A narrative review and integrative hypothesis. Complement. Ther. Clin. Pract. 2021, 42, 101277. [Google Scholar] [CrossRef]
- McGlone, F.; Cerritelli, F.; Walker, S.; Esteves, J. The role of gentle touch in perinatal osteopathic manual therapy. Neurosci. Biobehav. Rev. 2017, 72, 1–9. [Google Scholar] [CrossRef]
- Eckstein, M.; Mamaev, I.; Ditzen, B.; Sailer, U. Calming Effects of Touch in Human, Animal, and Robotic Interaction—Scientific State-of-the-Art and Technical Advances. Front. Psychiatry 2020, 11, 555058. [Google Scholar] [CrossRef]
- Castral, T.C.; Warnock, F.; Leite, A.M.; Haas, V.J.; Scochi, C.G.S. The effects of skin-to-skin contact during acute pain in preterm newborns. Eur. J. Pain. 2008, 12, 464–471. [Google Scholar] [CrossRef]
- Widström, A.; Brimdyr, K.; Svensson, K.; Cadwell, K.; Nissen, E. Skin-to-skin contact the first hour after birth, underlying implications and clinical practice. Acta Paediatr. 2019, 108, 1192–1204. [Google Scholar] [CrossRef] [PubMed]
- Bergman, N.J. New policies on skin-to-skin contact warrant an oxytocin-based perspective on perinatal health care. Front. Psychol. 2024, 15, 1385320. [Google Scholar] [CrossRef] [PubMed]
- Manzotti, A.; Cerritelli, F.; Monzani, E.; Savioli, L.; Esteves, J.E.; Lista, G.; Lombardi, E.; Rocca, S.; Biasi, P.; Galli, M.; et al. Dynamic touch induces autonomic changes in preterm infants as measured by changes in heart rate variability. Brain Res. 2023, 1799, 148169. [Google Scholar] [CrossRef] [PubMed]
- Manzotti, A.; Cerritelli, F.; Esteves, J.E.; Lista, G.; Lombardi, E.; La Rocca, S.; Gallace, A.; McGlone, F.P.; Walker, S.C. Dynamic touch reduces physiological arousal in preterm infants: A role for c-tactile afferents? Dev. Cogn. Neurosci. 2019, 39, 100703. [Google Scholar] [CrossRef]
- Bonanno, M.; Papa, G.A.; Calabrò, R.S. The Neurophysiological Impact of Touch-Based Therapy: Insights and Clinical Benefits. J. Integr. Neurosci. 2024, 23, 214. [Google Scholar] [CrossRef]
- Björnsdotter, M.; Morrison, I.; Olausson, H. Feeling good: On the role of C fiber mediated touch in interoception. Exp. Brain Res. 2010, 207, 149–155. [Google Scholar] [CrossRef]
- Williams, J.M.; Haq, I.; Lee, R.Y. The effect of pain relief on dynamic changes in lumbar curvature. Man. Ther. 2013, 18, 149–154. [Google Scholar] [CrossRef]
- Ruffini, N.; D’Alessandro, G.; Mariani, N.; Pollastrelli, A.; Cardinali, L.; Cerritelli, F. Variations of high frequency parameter of heart rate variability following osteopathic manipulative treatment in healthy subjects compared to control group and sham therapy: Randomized controlled trial. Front. Neurosci. 2015, 9, 272. [Google Scholar] [CrossRef]
- Stępnik, J.; Czaprowski, D.; Kędra, A. Effect of manual osteopathic techniques on the autonomic nervous system, respiratory system function and head-cervical-shoulder complex-a systematic review. Front. Med. 2024, 11, 1358529. [Google Scholar] [CrossRef]
- Henley, C.E.; Ivins, D.; Mills, M.; Wen, F.K.; Benjamin, B.A. Osteopathic manipulative treatment and its relationship to autonomic nervous system activity as demonstrated by heart rate variability: A repeated measures study. Osteopath. Med. Prim. Care 2008, 2, 7. [Google Scholar] [CrossRef]
- Cerritelli, F.; Cardone, D.; Pirino, A.; Merla, A.; Scoppa, F. Does Osteopathic Manipulative Treatment Induce Autonomic Changes in Healthy Participants? A Thermal Imaging Study. Front. Neurosci. 2020, 14, 887. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, S.; Morris, P.; Mercer, H.; Baker, M.; Gallese, V.; Reddy, V. Proximity and gaze influences facial temperature: A thermal infrared imaging study. Front. Psychol. 2014, 5, 845. [Google Scholar] [CrossRef] [PubMed]
- Lunghi, C.; Tozzi, P.; Fusco, G. The biomechanical model in manual therapy: Is there an ongoing crisis or just the need to revise the underlying concept and application? J. Bodyw. Mov. Ther. 2016, 20, 784–799. [Google Scholar] [CrossRef] [PubMed]

| Age (Mean ± SD) | Gender (M/F) | Weight (Mean ± SD) | Height (Mean ± SD) | |
|---|---|---|---|---|
| CTRL | 28.75 ± 5.3 | 35/20 | 68.18 ± 12.12 | 172.98 ± 9.44 |
| GTI | 27.55 ± 5.58 | 32/23 | 69.45 ± 14.72 | 173.53 ± 9.8 |
| OMT | 27.85 ± 4.17 | 32/23 | 69.77 ± 12.06 | 173.93 ± 8.49 |
| Cervical Arrow | Lumbar Arrow | |||||||
|---|---|---|---|---|---|---|---|---|
| S1 | S2 | S1 | S2 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CTRL | 42.65 | 17.44 | 42.25 | 17.80 | 42.76 | 14.20 | 41.31 | 13.94 |
| GTI | 43.62 * | 17.52 | 41.62 * | 17.53 | 40.25 | 13.62 | 39.89 | 14.30 |
| OMT | 43.05 * | 13.89 | 40.51 * | 14.88 | 44.42 | 11.50 | 43.33 | 11.99 |
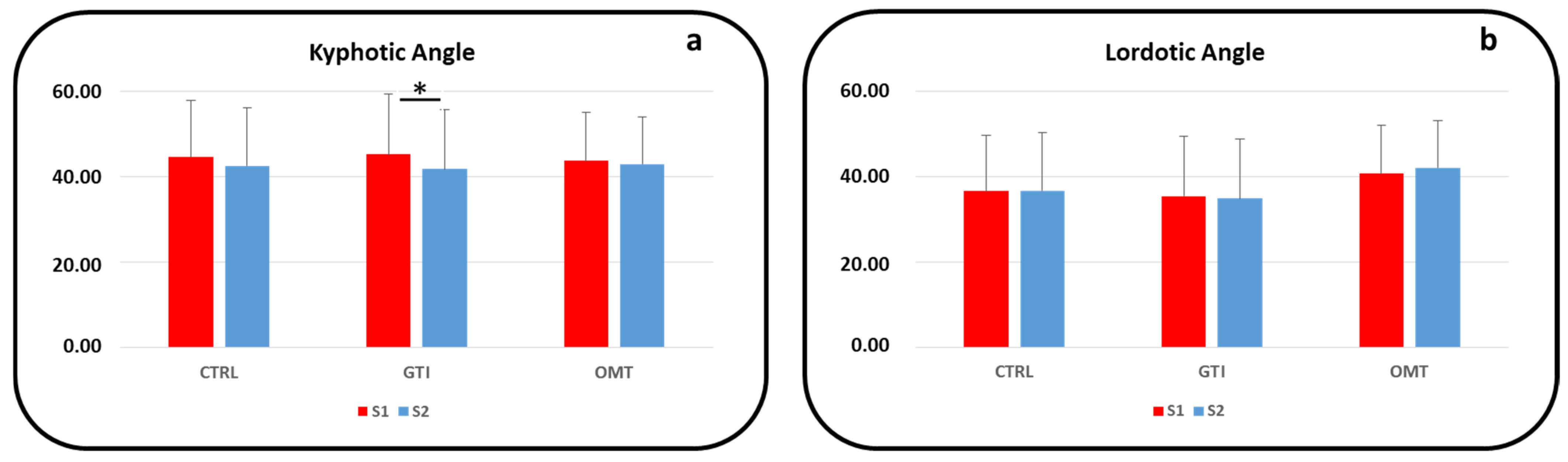
| Kyphotic Angle | Lordotic Angle | |||||||
|---|---|---|---|---|---|---|---|---|
| S1 | S2 | S1 | S2 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CTRL | 44.60 | 12.56 | 42.47 | 12.25 | 36.61 | 13.39 | 36.62 | 14.64 |
| GTI | 45.23 * | 13.32 | 41.71 * | 12.44 | 35.40 | 12.08 | 34.80 | 11.81 |
| OMT | 43.73 | 11.95 | 42.89 | 11.14 | 40.69 | 10.58 | 42.06 | 12.26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scoppa, F.; Graffitti, A.; Pirino, A.; Piermaria, J.; Tamburella, F.; Tramontano, M. Three-Dimensional Posture Analysis-Based Modifications After Manual Therapy: A Preliminary Study. J. Clin. Med. 2025, 14, 634. https://doi.org/10.3390/jcm14020634
Scoppa F, Graffitti A, Pirino A, Piermaria J, Tamburella F, Tramontano M. Three-Dimensional Posture Analysis-Based Modifications After Manual Therapy: A Preliminary Study. Journal of Clinical Medicine. 2025; 14(2):634. https://doi.org/10.3390/jcm14020634
Chicago/Turabian StyleScoppa, Fabio, Andrea Graffitti, Alessio Pirino, Jacopo Piermaria, Federica Tamburella, and Marco Tramontano. 2025. "Three-Dimensional Posture Analysis-Based Modifications After Manual Therapy: A Preliminary Study" Journal of Clinical Medicine 14, no. 2: 634. https://doi.org/10.3390/jcm14020634
APA StyleScoppa, F., Graffitti, A., Pirino, A., Piermaria, J., Tamburella, F., & Tramontano, M. (2025). Three-Dimensional Posture Analysis-Based Modifications After Manual Therapy: A Preliminary Study. Journal of Clinical Medicine, 14(2), 634. https://doi.org/10.3390/jcm14020634








