Impact of Obesity on Pubertal Timing and Male Fertility
Abstract
1. Introduction
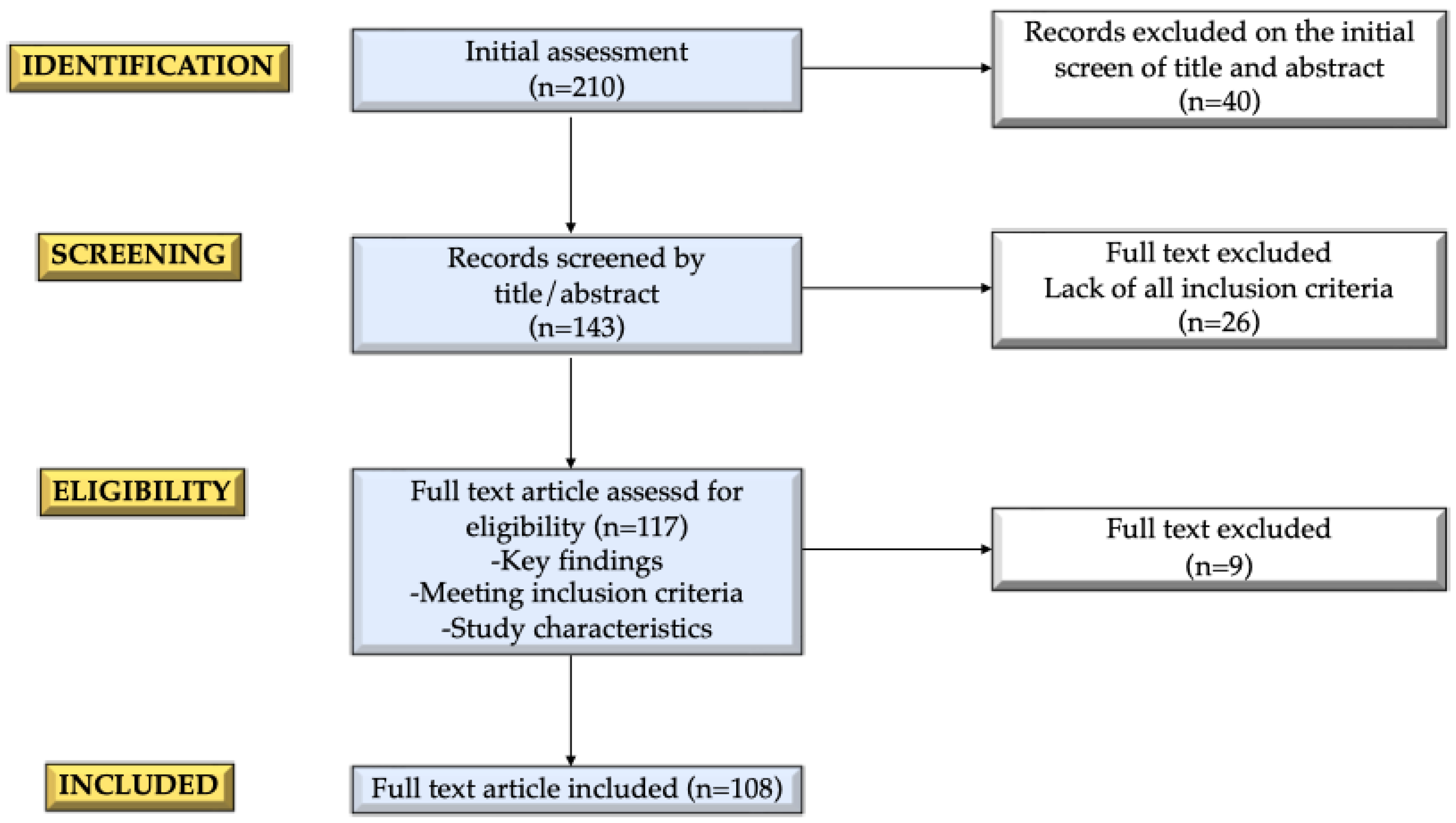
2. Methods
3. Pubertal Development and Reproductive Function in Males
4. Impact of Obesity on Pubertal Timing in Males
4.1. Obesity and Pubertal Timing
4.2. Mechanisms Linking Obesity and Puberty
5. Obesity and Male Fertility
5.1. Functional Hypogonadism
5.2. Insulin Resistance and Hyperglycemia
5.3. Chronic Inflammation
5.4. Adipokines
5.5. Sirtuins
5.6. Irisin
5.7. Gut Hormones
5.8. Gut Microbiome
5.9. Sperm Transcriptome and Epigenetic Modifications
5.10. Role of Weight Loss in Improving Fertility Outcomes
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Regional Office for Europe WHO European Childhood Obesity Surveillance Initiative (COSI) Report on the Fourth Round of Data Collection, 2015–2017; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 January 2025).
- Wood, C.L.; Lane, L.C.; Cheetham, T. Puberty: Normal Physiology (Brief Overview). Best Pract. Res. Clin. Endocrinol. Metab. 2019, 33, 101265. [Google Scholar] [CrossRef] [PubMed]
- Rohayem, J.; Alexander, E.C.; Heger, S.; Nordenström, A.; Howard, S.R. Mini-Puberty, Physiological and Disordered: Consequences, and Potential for Therapeutic Replacement. Endocr. Rev. 2024, 45, 460–492. [Google Scholar] [CrossRef] [PubMed]
- Busch, A.S.; Højgaard, B.; Hagen, C.P.; Teilmann, G. Obesity Is Associated with Earlier Pubertal Onset in Boys. J. Clin. Endocrinol. Metab. 2020, 105, e1667–e1672. [Google Scholar] [CrossRef] [PubMed]
- Brix, N.; Ernst, A.; Lauridsen, L.L.B.; Parner, E.; Støvring, H.; Olsen, J.; Henriksen, T.B.; Ramlau-Hansen, C.H. Timing of Puberty in Boys and Girls: A Population-Based Study. Paediatr. Perinat. Epidemiol. 2019, 33, 70–78. [Google Scholar] [CrossRef]
- Calcaterra, V.; Magenes, V.C.; Hruby, C.; Siccardo, F.; Mari, A.; Cordaro, E.; Fabiano, V.; Zuccotti, G. Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty. Children 2023, 10, 241. [Google Scholar] [CrossRef]
- Lee, J.M.; Wasserman, R.; Kaciroti, N.; Gebremariam, A.; Steffes, J.; Dowshen, S.; Harris, D.; Serwint, J.; Abney, D.; Smitherman, L.; et al. Timing of Puberty in Overweight Versus Obese Boys. Pediatrics 2016, 137, e20150164. [Google Scholar] [CrossRef]
- Lee, J.M.; Kaciroti, N.; Appugliese, D.; Corwyn, R.F.; Bradley, R.H.; Lumeng, J.C. Body Mass Index and Timing of Pubertal Initiation in Boys. Arch. Pediatr. Adolesc. Med. 2010, 164, 139–144. [Google Scholar] [CrossRef]
- Salas-Huetos, A.; Maghsoumi-Norouzabad, L.; James, E.R.; Carrell, D.T.; Aston, K.I.; Jenkins, T.G.; Becerra-Tomás, N.; Javid, A.Z.; Abed, R.; Torres, P.J.; et al. Male Adiposity, Sperm Parameters and Reproductive Hormones: An Updated Systematic Review and Collaborative Meta-analysis. Obes. Rev. 2021, 22, e13082. [Google Scholar] [CrossRef]
- AbbasiHormozi, S.; Kouhkan, A.; Shahverdi, A.; Parikar, A.; Shirin, A.; Vesali, S. How Much Obesity and Diabetes Do Impair Male Fertility? Reprod. Biol. Endocrinol. 2023, 21, 48. [Google Scholar] [CrossRef] [PubMed]
- La Vignera, S.; Condorelli, R.A.; Duca, Y.; Cannarella, R.; Giacone, F.; Calogero, A.E. FSH Treatment for Normogonadotropic Male Infertility: A Synergistic Role for Metformin? Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 5994–5998. [Google Scholar] [CrossRef]
- Raee, P.; Shams Mofarahe, Z.; Nazarian, H.; Abdollahifar, M.-A.; Ghaffari Novin, M.; Aghamiri, S.; Ghaffari Novin, M. Male Obesity Is Associated with Sperm Telomere Shortening and Aberrant mRNA Expression of Autophagy-Related Genes. Basic Clin. Androl. 2023, 33, 13. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A Scale for the Quality Assessment of Narrative Review Articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.T.; Denniss, A.R. An Introduction to Writing Narrative and Systematic Reviews—Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018, 27, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Herbison, A.E. The Gonadotropin-Releasing Hormone Pulse Generator. Endocrinology 2018, 159, 3723–3736. [Google Scholar] [CrossRef] [PubMed]
- Zirkin, B.R.; Papadopoulos, V. Leydig Cells: Formation, Function, and Regulation. Biol. Reprod. 2018, 99, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Griswold, M.D. The Central Role of Sertoli Cells in Spermatogenesis. Semin. Cell Dev. Biol. 1998, 9, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.-M.; Yang, W.-X. Molecular Regulation of Hypothalamus-Pituitary-Gonads Axis in Males. Gene 2014, 551, 15–25. [Google Scholar] [CrossRef]
- Hiort, O. The Differential Role of Androgens in Early Human Sex Development. BMC Med. 2013, 11, 152. [Google Scholar] [CrossRef]
- Bay, K.; Virtanen, H.E.; Hartung, S.; Ivell, R.; Main, K.M.; Skakkebaek, N.E.; Andersson, A.-M.; Nordic Cryptorchidism Study Group; Toppari, J. Insulin-like Factor 3 Levels in Cord Blood and Serum from Children: Effects of Age, Postnatal Hypothalamic-Pituitary-Gonadal Axis Activation, and Cryptorchidism. J. Clin. Endocrinol. Metab. 2007, 92, 4020–4027. [Google Scholar] [CrossRef]
- Abbara, A.; Koysombat, K.; Phylactou, M.; Eng, P.C.; Clarke, S.; Comninos, A.N.; Yang, L.; Izzi-Engbeaya, C.; Hanassab, S.; Smith, N.; et al. Insulin-like Peptide 3 (INSL3) in Congenital Hypogonadotrophic Hypogonadism (CHH) in Boys with Delayed Puberty and Adult Men. Front. Endocrinol. 2022, 13, 1076984. [Google Scholar] [CrossRef] [PubMed]
- Gowkielewicz, M.; Lipka, A.; Zdanowski, W.; Waśniewski, T.; Majewska, M.; Carlberg, C. Anti-Müllerian Hormone: Biology and Role in Endocrinology and Cancers. Front. Endocrinol. 2024, 15, 1468364. [Google Scholar] [CrossRef]
- Forest, M.G.; Cathiard, A.M.; Bertrand, J.A. Evidence of Testicular Activity in Early Infancy. J. Clin. Endocrinol. Metab. 1973, 37, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Johannsen, T.H.; Main, K.M.; Ljubicic, M.L.; Jensen, T.K.; Andersen, H.R.; Andersen, M.S.; Petersen, J.H.; Andersson, A.-M.; Juul, A. Sex Differences in Reproductive Hormones During Mini-Puberty in Infants With Normal and Disordered Sex Development. J. Clin. Endocrinol. Metab. 2018, 103, 3028–3037. [Google Scholar] [CrossRef] [PubMed]
- Busch, A.S.; Ljubicic, M.L.; Upners, E.N.; Fischer, M.B.; Raket, L.L.; Frederiksen, H.; Albrethsen, J.; Johannsen, T.H.; Hagen, C.P.; Juul, A. Dynamic Changes of Reproductive Hormones in Male Minipuberty: Temporal Dissociation of Leydig and Sertoli Cell Activity. J. Clin. Endocrinol. Metab. 2022, 107, 1560–1568. [Google Scholar] [CrossRef]
- Howard, S.R. Interpretation of Reproductive Hormones before, during and after the Pubertal Transition-Identifying Health and Disordered Puberty. Clin. Endocrinol. 2021, 95, 702–715. [Google Scholar] [CrossRef]
- Gerhardt, C.M.; Travers, S.H.; Slover, R.H. Chapter 43—Disorders of Puberty. In Endocrine Secrets, 5th ed.; McDermott, M.T., Ed.; Mosby: Philadelphia, PA, USA, 2009; pp. 362–375. ISBN 978-0-323-05885-8. [Google Scholar]
- Witchel, S.F.; Pinto, B.; Burghard, A.C.; Oberfield, S.E. Update on Adrenarche. Curr. Opin. Pediatr. 2020, 32, 574–581. [Google Scholar] [CrossRef]
- Mäntyselkä, A.; Jääskeläinen, J.; Lindi, V.; Viitasalo, A.; Tompuri, T.; Voutilainen, R.; Lakka, T.A. The Presentation of Adrenarche Is Sexually Dimorphic and Modified by Body Adiposity. J. Clin. Endocrinol. Metab. 2014, 99, 3889–3894. [Google Scholar] [CrossRef]
- Rosenfield, R.L. Normal and Premature Adrenarche. Endocr. Rev. 2021, 42, 783–814. [Google Scholar] [CrossRef]
- Aghaee, S.; Deardorff, J.; Quesenberry, C.P.; Greenspan, L.C.; Kushi, L.H.; Kubo, A. Associations Between Childhood Obesity and Pubertal Timing Stratified by Sex and Race/Ethnicity. Am. J. Epidemiol. 2022, 191, 2026–2036. [Google Scholar] [CrossRef]
- Augsburger, P.; Liimatta, J.; Flück, C.E. Update on Adrenarche—Still a Mystery. J. Clin. Endocrinol. Metab. 2024, 109, 1403–1422. [Google Scholar] [CrossRef]
- Kim, S.-H.; Moon, J.-Y.; Sasano, H.; Choi, M.H.; Park, M.-J. Body Fat Mass Is Associated With Ratio of Steroid Metabolites Reflecting 17,20-Lyase Activity in Prepubertal Girls. J. Clin. Endocrinol. Metab. 2016, 101, 4653–4660. [Google Scholar] [CrossRef][Green Version]
- Busch, A.S.; Hollis, B.; Day, F.R.; Sørensen, K.; Aksglaede, L.; Perry, J.R.B.; Ong, K.K.; Juul, A.; Hagen, C.P. Voice Break in Boys-Temporal Relations with Other Pubertal Milestones and Likely Causal Effects of BMI. Hum. Reprod. Oxf. Engl. 2019, 34, 1514–1522. [Google Scholar] [CrossRef]
- Marshall, W.A.; Tanner, J.M. Variations in the Pattern of Pubertal Changes in Boys. Arch. Dis. Child. 1970, 45, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.M.; Seierøe, K.; Pakkenberg, B. The Total Number of Leydig and Sertoli Cells in the Testes of Men across Various Age Groups—A Stereological Study. J. Anat. 2015, 226, 175–179. [Google Scholar] [CrossRef]
- Ruwanpura, S.M.; McLachlan, R.I.; Meachem, S.J. Hormonal Regulation of Male Germ Cell Development. J. Endocrinol. 2010, 205, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Pierik, F.H.; Vreeburg, J.T.; Stijnen, T.; De Jong, F.H.; Weber, R.F. Serum Inhibin B as a Marker of Spermatogenesis. J. Clin. Endocrinol. Metab. 1998, 83, 3110–3114. [Google Scholar] [CrossRef]
- Rockett, J.C.; Lynch, C.D.; Buck, G.M. Biomarkers for Assessing Reproductive Development and Health: Part 1--Pubertal Development. Environ. Health Perspect. 2004, 112, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.; Ahmed, M.L.; Dunger, D.B. Lessons from Large Population Studies on Timing and Tempo of Puberty (Secular Trends and Relation to Body Size): The European Trend. Mol. Cell. Endocrinol. 2006, 254–255, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Euling, S.Y.; Herman-Giddens, M.E.; Lee, P.A.; Selevan, S.G.; Juul, A.; Sørensen, T.I.A.; Dunkel, L.; Himes, J.H.; Teilmann, G.; Swan, S.H. Examination of US Puberty-Timing Data from 1940 to 1994 for Secular Trends: Panel Findings. Pediatrics 2008, 121 (Suppl. S3), S172–S191. [Google Scholar] [CrossRef]
- Brix, N.; Ramlau-Hansen, C.H. Obesity in Both Boys and Girls Associated with Earlier Pubertal Timing. J. Pediatr. 2021, 234, 286–288. [Google Scholar] [CrossRef]
- Ahmed, M.L.; Ong, K.K.; Dunger, D.B. Childhood Obesity and the Timing of Puberty. Trends Endocrinol. Metab. 2009, 20, 237–242. [Google Scholar] [CrossRef]
- Kaplowitz, P.B. Link Between Body Fat and the Timing of Puberty. Pediatrics 2008, 121, S208–S217. [Google Scholar] [CrossRef] [PubMed]
- Herman-Giddens, M.E.; Steffes, J.; Harris, D.; Slora, E.; Hussey, M.; Dowshen, S.A.; Wasserman, R.; Serwint, J.R.; Smitherman, L.; Reiter, E.O. Secondary Sexual Characteristics in Boys: Data From the Pediatric Research in Office Settings Network. Pediatrics 2012, 130, e1058–e1068. [Google Scholar] [CrossRef] [PubMed]
- Brix, N.; Ernst, A.; Lauridsen, L.L.B.; Parner, E.T.; Arah, O.A.; Olsen, J.; Henriksen, T.B.; Ramlau-Hansen, C.H. Childhood Overweight and Obesity and Timing of Puberty in Boys and Girls: Cohort and Sibling-Matched Analyses. Int. J. Epidemiol. 2020, 49, 834–844. [Google Scholar] [CrossRef]
- Deardorff, J.; Reeves, J.W.; Hyland, C.; Tilles, S.; Rauch, S.; Kogut, K.; Greenspan, L.C.; Shirtcliff, E.; Lustig, R.H.; Eskenazi, B.; et al. Childhood Overweight and Obesity and Pubertal Onset Among Mexican-American Boys and Girls in the CHAMACOS Longitudinal Study. Am. J. Epidemiol. 2022, 191, 7–16. [Google Scholar] [CrossRef]
- Bygdell, M.; Kindblom, J.M.; Celind, J.; Nethander, M.; Ohlsson, C. Childhood BMI Is Inversely Associated with Pubertal Timing in Normal-Weight but Not Overweight Boys. Am. J. Clin. Nutr. 2018, 108, 1259–1263. [Google Scholar] [CrossRef]
- Chung, S. Growth and Puberty in Obese Children and Implications of Body Composition. J. Obes. Metab. Syndr. 2017, 26, 243–250. [Google Scholar] [CrossRef]
- Mohsenipour, R.; Abbasi, F.; Setoodeh, A.; Sayarifard, F.; Rostami, P.; Moinfar, Z.; Amoli, M.M.; Tajdini, P.; Rabbani, A. Early and Delayed Puberty among Iranian Children with Obesity. Minerva Endocrinol. 2022, 47, 167–171. [Google Scholar] [CrossRef]
- Bell, J.A.; Carslake, D.; Wade, K.H.; Richmond, R.C.; Langdon, R.J.; Vincent, E.E.; Holmes, M.V.; Timpson, N.J.; Davey Smith, G. Influence of Puberty Timing on Adiposity and Cardiometabolic Traits: A Mendelian Randomisation Study. PLoS Med. 2018, 15, e1002641. [Google Scholar] [CrossRef] [PubMed]
- Cousminer, D.L.; Berry, D.J.; Timpson, N.J.; Ang, W.; Thiering, E.; Byrne, E.M.; Taal, H.R.; Huikari, V.; Bradfield, J.P.; Kerkhof, M.; et al. Genome-Wide Association and Longitudinal Analyses Reveal Genetic Loci Linking Pubertal Height Growth, Pubertal Timing and Childhood Adiposity. Hum. Mol. Genet. 2013, 22, 2735–2747. [Google Scholar] [CrossRef]
- Reinehr, T.; Roth, C.L. Is There a Causal Relationship between Obesity and Puberty? Lancet Child Adolesc. Health 2019, 3, 44–54. [Google Scholar] [CrossRef]
- Moriarty-Kelsey, M.; Harwood, J.E.F.; Travers, S.H.; Zeitler, P.S.; Nadeau, K.J. Testosterone, Obesity and Insulin Resistance in Young Males: Evidence for an Association between Gonadal Dysfunction and Insulin Resistance during Puberty. J. Pediatr. Endocrinol. Metab. JPEM 2010, 23, 1281–1287. [Google Scholar] [CrossRef]
- Haymond, M.W.; Chung, S.T. Commentary on the Impact of Obesity and Puberty on Insulin Sensitivity. J. Clin. Endocrinol. Metab. 2020, 105, e2082–e2083. [Google Scholar] [CrossRef] [PubMed]
- Pospisilova, H.; Stárka, L.; Hill, M.; Dušková, M. The Relationship between Estradiol and Obesity in Men. Endocr. Abstr. 2020, 70, AEP468. [Google Scholar] [CrossRef]
- Sánchez-Garrido, M.A.; García-Galiano, D.; Tena-Sempere, M. Early Programming of Reproductive Health and Fertility: Novel Neuroendocrine Mechanisms and Implications in Reproductive Medicine. Hum. Reprod. Update 2022, 28, 346–375. [Google Scholar] [CrossRef] [PubMed]
- Kalem, Z.; Namli Kalem, M.; Anadol, E.; Bakirarar, B.; Yilmaz, C.; Elmas, C.; Yalcinkaya, P.; Ruso, H.; Gurgan, T. Maternal Nutrition and Reproductive Functions of Female and Male Offspring. Reproduction 2018, 156, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Franzago, M.; Rovere, M.L.; Franchi, P.G.; Vitacolonna, E.; Stuppia, L. Epigenetics and Human Reproduction: The Primary Prevention of the Noncommunicable Diseases. Epigenomics 2019, 11, 1441–1460. [Google Scholar] [CrossRef] [PubMed]
- Ponce, D.; Rodríguez, F.; Miranda, J.P.; Binder, A.M.; Santos, J.L.; Michels, K.B.; Cutler, G.B.; Pereira, A.; Iñiguez, G.; Mericq, V. Differential Methylation Pattern in Pubertal Girls Associated with Biochemical Premature Adrenarche. Epigenetics 2023, 18, 2200366. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Cena, H.; Loperfido, F.; Rossi, V.; Grazi, R.; Quatrale, A.; De Giuseppe, R.; Manuelli, M.; Zuccotti, G. Evaluating Phthalates and Bisphenol in Foods: Risks for Precocious Puberty and Early-Onset Obesity. Nutrients 2024, 16, 2732. [Google Scholar] [CrossRef] [PubMed]
- Wagner, I.V.; Oliver, E.; Dötsch, J.; Söder, O. Adverse Effects of Metabolic Disorders in Childhood on Adult Reproductive Function and Fertility in the Male. J. Pediatr. Endocrinol. Metab. 2021, 34, 13–23. [Google Scholar] [CrossRef]
- Cannarella, R.; Crafa, A.; Curto, R.; Condorelli, R.A.; La Vignera, S.; Calogero, A.E. Obesity and Male Fertility Disorders. Mol. Asp. Med. 2024, 97, 101273. [Google Scholar] [CrossRef]
- George, B.T.; Jhancy, M.; Dube, R.; Kar, S.S.; Annamma, L.M. The Molecular Basis of Male Infertility in Obesity: A Literature Review. Int. J. Mol. Sci. 2023, 25, 179. [Google Scholar] [CrossRef] [PubMed]
- Service, C.A.; Puri, D.; Al Azzawi, S.; Hsieh, T.-C.; Patel, D.P. The Impact of Obesity and Metabolic Health on Male Fertility: A Systematic Review. Fertil. Steril. 2023, 120, 1098–1111. [Google Scholar] [CrossRef]
- Cannarella, R.; Caruso, M.; Condorelli, R.A.; Timpanaro, T.A.; Caruso, M.A.; La Vignera, S.; Calogero, A.E. Testicular Volume in 268 Children and Adolescents Followed-up for Childhood Obesity-a Retrospective Cross-Sectional Study. Eur. J. Endocrinol. 2023, 188, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Leisegang, K.; Sengupta, P.; Agarwal, A.; Henkel, R. Obesity and Male Infertility: Mechanisms and Management. Andrologia 2021, 53, e13617. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Sun, M.; Ye, J.; Luo, D.; Su, X.; Zheng, D.; Feng, L.; Gao, L.; Yu, C.; Guan, Q. The Effect of Aromatase on the Reproductive Function of Obese Males. Horm. Metab. Res. 2017, 49, 572–579. [Google Scholar] [CrossRef]
- Hazra, R.; Corcoran, L.; Robson, M.; McTavish, K.J.; Upton, D.; Handelsman, D.J.; Allan, C.M. Temporal Role of Sertoli Cell Androgen Receptor Expression in Spermatogenic Development. Mol. Endocrinol. 2013, 27, 12–24. [Google Scholar] [CrossRef]
- Abel, M.H.; Baker, P.J.; Charlton, H.M.; Monteiro, A.; Verhoeven, G.; De Gendt, K.; Guillou, F.; O’Shaughnessy, P.J. Spermatogenesis and Sertoli Cell Activity in Mice Lacking Sertoli Cell Receptors for Follicle-Stimulating Hormone and Androgen. Endocrinology 2008, 149, 3279–3285. [Google Scholar] [CrossRef]
- Kelly, D.M.; Jones, T.H. Testosterone and Obesity. Obes. Rev. 2015, 16, 581–606. [Google Scholar] [CrossRef] [PubMed]
- Genchi, V.A.; Rossi, E.; Lauriola, C.; D’Oria, R.; Palma, G.; Borrelli, A.; Caccioppoli, C.; Giorgino, F.; Cignarelli, A. Adipose Tissue Dysfunction and Obesity-Related Male Hypogonadism. Int. J. Mol. Sci. 2022, 23, 8194. [Google Scholar] [CrossRef]
- Ghafouri-Fard, S.; Shoorei, H.; Mohaqiq, M.; Haidar Abbas Raza, S.; Taheri, M. The Role of Different Compounds on the Integrity of Blood-Testis Barrier: A Concise Review Based on in Vitro and in Vivo Studies. Gene 2021, 780, 145531. [Google Scholar] [CrossRef] [PubMed]
- Kley, H.K.; Edelmann, P.; Krüskemper, H.L. Relationship of Plasma Sex Hormones to Different Parameters of Obesity in Male Subjects. Metabolism 1980, 29, 1041–1045. [Google Scholar] [CrossRef]
- Stárka, L.; Hill, M.; Pospíšilová, H.; Dušková, M. Estradiol, Obesity and Hypogonadism. Physiol. Res. 2020, 69, S273–S278. [Google Scholar] [CrossRef] [PubMed]
- Šarac, I. The influence of metabolic syndrome on reproductive health—The impact of low vitamin D. In Reference Module in Food Science; Elsevier: Amsterdam, The Netherlands, 2019; p. B9780081005965225249. ISBN 978-0-08-100596-5. [Google Scholar]
- Engin, A.B. Mechanism of Obesity-Related Lipotoxicity and Clinical Perspective. Adv. Exp. Med. Biol. 2024, 1460, 131–166. [Google Scholar] [CrossRef]
- Wu, L.L.-Y.; Dunning, K.R.; Yang, X.; Russell, D.L.; Lane, M.; Norman, R.J.; Robker, R.L. High-Fat Diet Causes Lipotoxicity Responses in Cumulus–Oocyte Complexes and Decreased Fertilization Rates. Endocrinology 2010, 151, 5438–5445. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Tian, Z.; Qi, X.; Chen, P.; Yang, Q.; Guan, Q.; Ye, J.; Yu, C. Switching from High-Fat Diet to Normal Diet Ameliorate BTB Integrity and Improve Fertility Potential in Obese Male Mice. Sci. Rep. 2023, 13, 14152. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Zhang, M.; Su, X.; Liu, L.; Zhou, X.; Zhang, X.; Zheng, D.; Yu, C.; Guan, Q. High Fat Diet Impairs Spermatogenesis by Regulating Glucose and Lipid Metabolism in Sertoli Cells. Life Sci. 2020, 257, 118028. [Google Scholar] [CrossRef]
- Ameratunga, D.; Gebeh, A.; Amoako, A. Obesity and Male Infertility. Best Pract. Res. Clin. Obstet. Gynaecol. 2023, 90, 102393. [Google Scholar] [CrossRef]
- Davidson, L.M.; Millar, K.; Jones, C.; Fatum, M.; Coward, K. Deleterious Effects of Obesity upon the Hormonal and Molecular Mechanisms Controlling Spermatogenesis and Male Fertility. Hum. Fertil. 2015, 18, 184–193. [Google Scholar] [CrossRef]
- Aquila, S.; Gentile, M.; Middea, E.; Catalano, S.; Andò, S. Autocrine Regulation of Insulin Secretion in Human Ejaculated Spermatozoa. Endocrinology 2005, 146, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.D.; Majzoub, A.; Agawal, A. Metabolic Syndrome and Male Fertility. World J. Mens Health 2019, 37, 113–127. [Google Scholar] [CrossRef]
- Law, N.C.; Hunzicker-Dunn, M.E. Insulin Receptor Substrate 1, the Hub Linking Follicle-Stimulating Hormone to Phosphatidylinositol 3-Kinase Activation. J. Biol. Chem. 2016, 291, 4547–4560. [Google Scholar] [CrossRef]
- Maresch, C.C.; Stute, D.C.; Fleming, T.; Lin, J.; Hammes, H.-P.; Linn, T. Hyperglycemia Induces Spermatogenic Disruption via Major Pathways of Diabetes Pathogenesis. Sci. Rep. 2019, 9, 13074. [Google Scholar] [CrossRef]
- Facondo, P.; Di Lodovico, E.; Delbarba, A.; Anelli, V.; Pezzaioli, L.C.; Filippini, E.; Cappelli, C.; Corona, G.; Ferlin, A. The Impact of Diabetes Mellitus Type 1 on Male Fertility: Systematic Review and Meta-analysis. Andrology 2022, 10, 426–440. [Google Scholar] [CrossRef]
- Ding, G.-L.; Liu, Y.; Liu, M.-E.; Pan, J.-X.; Guo, M.-X.; Sheng, J.-Z.; Huang, H.-F. The Effects of Diabetes on Male Fertility and Epigenetic Regulation during Spermatogenesis. Asian J. Androl. 2015, 17, 948–953. [Google Scholar] [CrossRef]
- Tsilidis, K.K.; Rohrmann, S.; McGlynn, K.A.; Nyante, S.J.; Lopez, D.S.; Bradwin, G.; Feinleib, M.; Joshu, C.E.; Kanarek, N.; Nelson, W.G.; et al. Association between Endogenous Sex Steroid Hormones and Inflammatory Biomarkers in US Men. Andrology 2013, 1, 919–928. [Google Scholar] [CrossRef]
- Yeap, B.B.; Knuiman, M.W.; Divitini, M.L.; Handelsman, D.J.; Beilby, J.P.; Beilin, J.; McQuillan, B.; Hung, J. Differential Associations of Testosterone, Dihydrotestosterone and Oestradiol with Physical, Metabolic and Health-related Factors in Community-dwelling Men Aged 17–97 Years from the Busselton Health Survey. Clin. Endocrinol. 2014, 81, 100–108. [Google Scholar] [CrossRef]
- Hong, C.Y.; Park, J.H.; Ahn, R.S.; Im, S.Y.; Choi, H.-S.; Soh, J.; Mellon, S.H.; Lee, K. Molecular Mechanism of Suppression of Testicular Steroidogenesis by Proinflammatory Cytokine Tumor Necrosis Factor Alpha. Mol. Cell. Biol. 2004, 24, 2593–2604. [Google Scholar] [CrossRef]
- Pini, T.; Parks, J.; Russ, J.; Dzieciatkowska, M.; Hansen, K.C.; Schoolcraft, W.B.; Katz-Jaffe, M. Obesity Significantly Alters the Human Sperm Proteome, with Potential Implications for Fertility. J. Assist. Reprod. Genet. 2020, 37, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Watanobe, H.; Hayakawa, Y. Hypothalamic Interleukin-1β and Tumor Necrosis Factor-α, But Not Interleukin-6, Mediate the Endotoxin-Induced Suppression of the Reproductive Axis in Rats. Endocrinology 2003, 144, 4868–4875. [Google Scholar] [CrossRef]
- Tremellen, K. Oxidative Stress and Male Infertility—A Clinical Perspective. Hum. Reprod. Update 2008, 14, 243–258. [Google Scholar] [CrossRef] [PubMed]
- Kaltsas, A.; Zikopoulos, A.; Dimitriadis, F.; Sheshi, D.; Politis, M.; Moustakli, E.; Symeonidis, E.N.; Chrisofos, M.; Sofikitis, N.; Zachariou, A. Oxidative Stress and Erectile Dysfunction: Pathophysiology, Impacts, and Potential Treatments. Curr. Issues Mol. Biol. 2024, 46, 8807–8834. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, J.; Zaman, S. Associations Between C-Reactive Protein, Obesity, Sex, and PCI Outcomes. JACC Cardiovasc. Interv. 2020, 13, 2893–2895. [Google Scholar] [CrossRef] [PubMed]
- Osmancevic, A.; Daka, B.; Michos, E.D.; Trimpou, P.; Allison, M. The Association between Inflammation, Testosterone and SHBG in Men: A Cross-Sectional Multi-Ethnic Study of Atherosclerosis. Clin. Endocrinol. 2023, 99, 190–197. [Google Scholar] [CrossRef]
- Madah, A.T.; Hadi, S.; Abouhamzeh, B.; Hadi, V.; Abdollahi, M.; Omidi, K. The Association between Dietary Inflammatory Index and C-Reactive Protein in Plasma and Semen with Semen Quality: A Cross-Sectional Study. Int. J. Reprod. Biomed. IJRM 2023, 21, 835–844. [Google Scholar] [CrossRef]
- Roumaud, P.; Martin, L.J. Roles of Leptin, Adiponectin and Resistin in the Transcriptional Regulation of Steroidogenic Genes Contributing to Decreased Leydig Cells Function in Obesity. Horm. Mol. Biol. Clin. Investig. 2015, 24, 25–45. [Google Scholar] [CrossRef]
- Tsatsanis, C.; Dermitzaki, E.; Avgoustinaki, P.; Malliaraki, N.; Mytaras, V.; Margioris, A. The Impact of Adipose Tissue-Derived Factors on the Hypothalamic-Pituitary-Gonadal (HPG) Axis. Hormones 2015, 14, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, F.; Condorelli, R.A.; Mongioì, L.M.; Cannarella, R.; Cimino, L.; Magagnini, M.C.; Crafa, A.; La Vignera, S.; Calogero, A.E. Molecular Mechanisms Underlying the Relationship between Obesity and Male Infertility. Metabolites 2021, 11, 840. [Google Scholar] [CrossRef] [PubMed]
- Fruhwürth, S.; Vogel, H.; Schürmann, A.; Williams, K.J. Novel Insights into How Overnutrition Disrupts the Hypothalamic Actions of Leptin. Front. Endocrinol. 2018, 9, 89. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.T.; Acohido, B.V.; Clifton, D.K.; Steiner, R.A. KiSS-1 Neurones Are Direct Targets for Leptin in the Ob/Ob Mouse. J. Neuroendocrinol. 2006, 18, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Clément, K.; Vaisse, C.; Lahlou, N.; Cabrol, S.; Pelloux, V.; Cassuto, D.; Gourmelen, M.; Dina, C.; Chambaz, J.; Lacorte, J.-M.; et al. A Mutation in the Human Leptin Receptor Gene Causes Obesity and Pituitary Dysfunction. Nature 1998, 392, 398–401. [Google Scholar] [CrossRef]
- Considine, R.V. Increased Serum Leptin Indicates Leptin Resistance in Obesity. Clin. Chem. 2011, 57, 1461–1462. [Google Scholar] [CrossRef]
- Ghaderpour, S.; Ghiasi, R.; Heydari, H.; Keyhanmanesh, R. The Relation between Obesity, Kisspeptin, Leptin, and Male Fertility. Horm. Mol. Biol. Clin. Investig. 2022, 43, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.D.; Moreira, A.C.; Sá, R.; Monteiro, M.P.; Sousa, M.; Carvalho, R.A.; Silva, B.M.; Oliveira, P.F.; Alves, M.G. Leptin Modulates Human Sertoli Cells Acetate Production and Glycolytic Profile: A Novel Mechanism of Obesity-Induced Male Infertility? Biochim. Biophys. Acta BBA—Mol. Basis Dis. 2015, 1852, 1824–1832. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Judd, R.L. Adiponectin regulation and function. In Comprehensive Physiology; Prakash, Y.S., Ed.; Wiley: Hoboken, NJ, USA, 2018; pp. 1031–1063. ISBN 978-0-470-65071-4. [Google Scholar]
- Zorena, K.; Jachimowicz-Duda, O.; Ślęzak, D.; Robakowska, M.; Mrugacz, M. Adipokines and Obesity. Potential Link to Metabolic Disorders and Chronic Complications. Int. J. Mol. Sci. 2020, 21, 3570. [Google Scholar] [CrossRef] [PubMed]
- Han, S.J.; Boyko, E.J.; Fujimoto, W.Y.; Kahn, S.E.; Leonetti, D.L. Low Plasma Adiponectin Concentrations Predict Increases in Visceral Adiposity and Insulin Resistance. J. Clin. Endocrinol. Metab. 2017, 102, 4626–4633. [Google Scholar] [CrossRef]
- Thomas, S.; Kratzsch, D.; Schaab, M.; Scholz, M.; Grunewald, S.; Thiery, J.; Paasch, U.; Kratzsch, J. Seminal Plasma Adipokine Levels Are Correlated with Functional Characteristics of Spermatozoa. Fertil. Steril. 2013, 99, 1256–1263.e3. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Huang, C.; Zhang, X.; Wang, J.; Ma, P.; Liu, Y.; Xiao, T.; Zabel, B.A.; Zhang, J.V. Chemerin-Derived Peptide C -20 Suppressed Gonadal Steroidogenesis. Am. J. Reprod. Immunol. 2014, 71, 265–277. [Google Scholar] [CrossRef]
- Yu, M.; Yang, Y.; Huang, C.; Ge, L.; Xue, L.; Xiao, Z.; Xiao, T.; Zhao, H.; Ren, P.; Zhang, J.V. Chemerin: A Functional Adipokine in Reproductive Health and Diseases. Biomedicines 2022, 10, 1910. [Google Scholar] [CrossRef]
- Moretti, E.; Collodel, G.; Mazzi, L.; Campagna, M.; Iacoponi, F.; Figura, N. Resistin, Interleukin-6, Tumor Necrosis Factor-Alpha, and Human Semen Parameters in the Presence of Leukocytospermia, Smoking Habit, and Varicocele. Fertil. Steril. 2014, 102, 354–360. [Google Scholar] [CrossRef]
- Costa, C.D.S.; Hammes, T.O.; Rohden, F.; Margis, R.; Bortolotto, J.W.; Padoin, A.V.; Mottin, C.C.; Guaragna, R.M. SIRT1 Transcription Is Decreased in Visceral Adipose Tissue of Morbidly Obese Patients with Severe Hepatic Steatosis. Obes. Surg. 2010, 20, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Petrangeli, E.; Coroniti, G.; Brini, A.T.; De Girolamo, L.; Stanco, D.; Niada, S.; Silecchia, G.; Morgante, E.; Lubrano, C.; Russo, M.A.; et al. Hypoxia Promotes the Inflammatory Response and Stemness Features in Visceral Fat Stem Cells From Obese Subjects. J. Cell. Physiol. 2016, 231, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Hirschey, M.D.; Shimazu, T.; Jing, E.; Grueter, C.A.; Collins, A.M.; Aouizerat, B.; Stančáková, A.; Goetzman, E.; Lam, M.M.; Schwer, B.; et al. SIRT3 Deficiency and Mitochondrial Protein Hyperacetylation Accelerate the Development of the Metabolic Syndrome. Mol. Cell 2011, 44, 177–190. [Google Scholar] [CrossRef]
- Kolthur-Seetharam, U.; Teerds, K.; De Rooij, D.G.; Wendling, O.; McBurney, M.; Sassone-Corsi, P.; Davidson, I. The Histone Deacetylase SIRT1 Controls Male Fertility in Mice Through Regulation of Hypothalamic-Pituitary Gonadotropin Signaling1. Biol. Reprod. 2009, 80, 384–391. [Google Scholar] [CrossRef]
- Rato, L.G.; Alves, M.M.; Silva, B.; Sousa, M.F.; Oliveira, P. Sirtuins: Novel Players in Male Reproductive Health. Curr. Med. Chem. 2016, 23, 1084–1099. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, F.; Cannarella, R.; Garofalo, V.; Marino, M.; La Vignera, S.; Condorelli, R.; Tiranini, L.; Nappi, R.; Calogero, A. The Role of Irisin throughout Women’s Life Span. Biomedicines 2023, 11, 3260. [Google Scholar] [CrossRef] [PubMed]
- Kamenov, Z.; Assyov, Y.; Angelova, P.; Gateva, A.; Tsakova, A. Irisin and Testosterone in Men with Metabolic Syndrome. Horm. Metab. Res. 2017, 49, 755–759. [Google Scholar] [CrossRef] [PubMed]
- Rosická, M.; Krsek, M.; Matoulek, M.; Jarkovská, Z.; Marek, J.; Justová, V.; Lacinová, Z. Serum Ghrelin Levels in Obese Patients: The Relationship to Serum Leptin Levels and Soluble Leptin Receptors Levels. Physiol. Res. 2003, 52, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Kheradmand, A.; Dezfoulian, O.; Tarrahi, M.J. Ghrelin Attenuates Heat-Induced Degenerative Effects in the Rat Testis. Regul. Pept. 2011, 167, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.D.; Sá, R.; Monteiro, M.P.; Barros, A.; Sousa, M.; Carvalho, R.A.; Silva, B.M.; Oliveira, P.F.; Alves, M.G. Ghrelin Acts as Energy Status Sensor of Male Reproduction by Modulating Sertoli Cells Glycolytic Metabolism and Mitochondrial Bioenergetics. Mol. Cell. Endocrinol. 2016, 434, 199–209. [Google Scholar] [CrossRef]
- Martins, A.D.; Monteiro, M.P.; Silva, B.M.; Barros, A.; Sousa, M.; Carvalho, R.A.; Oliveira, P.F.; Alves, M.G. Metabolic Dynamics of Human Sertoli Cells Are Differentially Modulated by Physiological and Pharmacological Concentrations of GLP-1. Toxicol. Appl. Pharmacol. 2019, 362, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rago, V.; De Rose, D.; Santoro, M.; Panza, S.; Malivindi, R.; Andò, S.; D’Agata, R.; Aquila, S. Human Sperm Express the Receptor for Glucagon-like Peptide-1 (GLP-1), Which Affects Sperm Function and Metabolism. Endocrinology 2020, 161, bqaa031. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.; Juhl, C.R.; Kjøller, E.T.; Lundgren, J.R.; Janus, C.; Dehestani, Y.; Saupstad, M.; Ingerslev, L.R.; Duun, O.M.; Jensen, S.B.K.; et al. Sperm Count Is Increased by Diet-Induced Weight Loss and Maintained by Exercise or GLP-1 Analogue Treatment: A Randomized Controlled Trial. Hum. Reprod. 2022, 37, 1414–1422. [Google Scholar] [CrossRef] [PubMed]
- Ding, N.; Zhang, X.; Zhang, X.D.; Jing, J.; Liu, S.S.; Mu, Y.P.; Peng, L.L.; Yan, Y.J.; Xiao, G.M.; Bi, X.Y.; et al. Impairment of Spermatogenesis and Sperm Motility by the High-Fat Diet-Induced Dysbiosis of Gut Microbes. Gut 2020, 69, 1608–1619. [Google Scholar] [CrossRef] [PubMed]
- Santiago, J.; Silva, J.V.; Howl, J.; Santos, M.A.S.; Fardilha, M. All You Need to Know about Sperm RNAs. Hum. Reprod. Update 2021, 28, 67–91. [Google Scholar] [CrossRef] [PubMed]
- Donkin, I.; Versteyhe, S.; Ingerslev, L.R.; Qian, K.; Mechta, M.; Nordkap, L.; Mortensen, B.; Appel, E.V.R.; Jørgensen, N.; Kristiansen, V.B.; et al. Obesity and Bariatric Surgery Drive Epigenetic Variation of Spermatozoa in Humans. Cell Metab. 2016, 23, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ding, Z. Obesity, a Serious Etiologic Factor for Male Subfertility in Modern Society. Reproduction 2017, 154, R123–R131. [Google Scholar] [CrossRef]
- López, P.; Castro, A.; Flórez, M.; Miranda, K.; Aranda, P.; Sánchez-González, C.; Llopis, J.; Arredondo, M. miR-155 and miR-122 Expression of Spermatozoa in Obese Subjects. Front. Genet. 2018, 9, 175. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, R.M.; Taganov, K.D.; Boldin, M.P.; Cheng, G.; Baltimore, D. MicroRNA-155 Is Induced during the Macrophage Inflammatory Response. Proc. Natl. Acad. Sci. USA 2007, 104, 1604–1609. [Google Scholar] [CrossRef]
- Chen, X.; Ba, Y.; Ma, L.; Cai, X.; Yin, Y.; Wang, K.; Guo, J.; Zhang, Y.; Chen, J.; Guo, X.; et al. Characterization of microRNAs in Serum: A Novel Class of Biomarkers for Diagnosis of Cancer and Other Diseases. Cell Res. 2008, 18, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Law, C.; Lo Conte, R.; Power, C. Intergenerational Influences on Childhood Body Mass Index: The Effect of Parental Body Mass Index Trajectories. Am. J. Clin. Nutr. 2009, 89, 551–557. [Google Scholar] [CrossRef] [PubMed]
- McPherson, N.O.; Fullston, T.; Bakos, H.W.; Setchell, B.P.; Lane, M. Obese Father’s Metabolic State, Adiposity, and Reproductive Capacity Indicate Son’s Reproductive Health. Fertil. Steril. 2014, 101, 865–873.e1. [Google Scholar] [CrossRef] [PubMed]
- Faienza, M.F.; Urbano, F.; Moscogiuri, L.A.; Chiarito, M.; De Santis, S.; Giordano, P. Genetic, Epigenetic and Enviromental Influencing Factors on the Regulation of Precocious and Delayed Puberty. Front. Endocrinol. 2022, 13, 1019468. [Google Scholar] [CrossRef]
- On Behalf of Obesity Programs of nutrition, Education, Research and Assessment (OPERA) Group; Bellastella, G.; Menafra, D.; Puliani, G.; Colao, A.; Savastano, S. How Much Does Obesity Affect the Male Reproductive Function? Int. J. Obes. Suppl. 2019, 9, 50–64. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Jensen, M.E.; Young, M.D.; Callister, R.; Plotnikoff, R.C.; Morgan, P.J. Improvement in Erectile Function Following Weight Loss in Obese Men: The SHED-IT Randomized Controlled Trial. Obes. Res. Clin. Pract. 2013, 7, e450–e454. [Google Scholar] [CrossRef]
- Håkonsen, L.B.; Thulstrup, A.M.; Aggerholm, A.S.; Olsen, J.; Bonde, J.P.; Andersen, C.Y.; Bungum, M.; Ernst, E.H.; Hansen, M.L.; Ernst, E.H.; et al. Does Weight Loss Improve Semen Quality and Reproductive Hormones? Results from a Cohort of Severely Obese Men. Reprod. Health 2011, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Svart, M.; Rittig, N.; Luong, T.V.; Gopalasingam, N.; Vestergaard, E.T.; Gormsen, L.; Søndergaard, E.; Thomsen, H.H.; Gravholt, C.H. Three Weeks on a Ketogenic Diet Reduces Free Testosterone and Free Estradiol in Middle-Aged Obese Men and Women. J. Nutr. Metab. 2024, 2024, 9301369. [Google Scholar] [CrossRef] [PubMed]

| Reference | Type of Study | Study Population | Main Results | Conclusion |
|---|---|---|---|---|
| Aghaee et al. (2022) [32] | Observational cohort study | 8500 boys and girls aged 6–18 (mean age: 12.5 years) | Childhood obesity was linked to earlier pubertal onset, particularly in specific ethnic groups (p < 0.01). | Obesity advances pubertal timing with differences by race/ethnicity |
| Ahmed et al. (2009) [44] | Review | Various studies on childhood obesity and puberty (no specific population size) | Obesity was linked to both earlier and more variable pubertal timing (p < 0.05 in selected studies). | Obesity may lead to earlier puberty, but the progression can vary |
| Bell et al. (2018) [52] | Mendelian randomization | 264,000 boys and girls from UK Biobank cohort (mean age: 8 years) | Higher childhood BMI causally linked to earlier pubertal onset in both boys and girls (p < 0.001) | Childhood obesity may directly cause earlier pubertal onset |
| Brix et al. (2019) [6] | Population-based cohort | 11,046 Danish boys and girls aged 6–18 years | Higher BMI was associated with earlier puberty onset in both sexes (p < 0.01) | BMI is a key predictor of pubertal onset timing |
| Brix et al. (2020) [47] | Cohort and sibling-matched study | 11,046 boys and girls from a birth cohort (aged 5–15 years) | Childhood overweight and obesity were associated with earlier puberty in both boys and girls (p < 0.001) | Sibling-matched analyses confirm the association between obesity and earlier puberty |
| Brix et al. (2021) [43] | Review | Review of studies on childhood obesity and pubertal timing (no specific population size) | Both boys and girls with obesity experienced earlier pubertal timing, with significant associations found across different studies (p < 0.05) | Obesity in both boys and girls is associated with earlier pubertal timing, highlighting the impact of childhood BMI on development |
| Bygdell et al. (2018) [49] | Cohort study | Swedish cohort of boys aged 6–18 years | Higher BMI was associated with later pubertal onset in normal weight boys but not in overweight boys (p < 0.05) | BMI influences pubertal timing in boys with a stronger effect in normal weight individuals |
| Busch et al. (2020) [5] | Longitudinal cohort study | 218 boys with obesity (mean age: 10.8 years) and 660 controls in Denmark | Boys with obesity experienced earlier testicular enlargement compared to controls (p = 0.01) | Obesity is associated with earlier pubertal onset in boys |
| Calcaterra et al. (2023) [7] | Review | Review of various studies on childhood obesity, high-fat diets, and central precocious puberty (no specific sample size) | Consistent associations between childhood obesity, high-fat diet, and earlier onset of central precocious puberty with obesity being a key risk factor for earlier pubertal timing (p < 0.01 across multiple studies) | Childhood obesity and high-fat diet are significant risk factors for central precocious puberty with implications for early pubertal development in children |
| Calcaterra et al. (2024) [7] | Review | Various studies on food contaminants and their impact on childhood development (no specific population size) | Phthalates and bisphenol exposure in foods were linked to precocious puberty and early-onset obesity (p < 0.05 across multiple studies) | Phthalates and bisphenol exposure through food may contribute to earlier pubertal onset and obesity in children, emphasizing the need for dietary interventions |
| Chung et al. (2017) [50] | Review | Various studies on childhood obesity (no specific sample size) | Obesity in boys often delayed puberty due to insulin resistance and hyperinsulinemia, which disrupt normal HPG axis function (p < 0.05) | Obesity may delay puberty in boys due to metabolic and hormonal changes, emphasizing the need to manage weight to prevent developmental delays |
| Cousminer et al. (2014) [53] | Genome-wide association study | 6000 children and adolescents (aged 8–18 years) | Identified genetic loci associated with both higher BMI and earlier puberty (p < 0.05) | Shared genetic pathways may underlie both childhood obesity and early puberty |
| Deardorff et al. (2021) [48] | Longitudinal cohort study | 700 Mexican–American boys and girls (aged 5–13 years) from the CHAMACOS cohort | Childhood overweight conditions and obesity were significantly associated with an earlier onset of pubertal markers (thelarche in girls, gonadarche in boys), with a stronger effect observed in girls (p < 0.01) | Childhood overweight conditions and obesity lead to earlier pubertal onset in Mexican–American children, with gender differences in the strength of associations |
| Euling et al. (2008) [42] | Review | Data from 17077 U.S. children and adolescents (aged 6–18) from 1940 to 1994 | Pubertal timing shifted earlier over the decades especially in girls. Increased childhood obesity and environmental factors may play a role (p < 0.01) | Secular trends show earlier puberty onset over time likely due to a combination of genetic, nutritional, and environmental influences |
| Herman-Giddens et al. (2012) [46] | Cross-sectional study | 4131 U.S. boys aged 6–16 years (mean age: 12 years) | Boys with higher BMI showed earlier pubertal onset (pubic hair and genital development) (p < 0.05) | Childhood obesity accelerates pubertal timing in boys |
| Kaplowitz (2008) [45] | Review | Various studies (no specific population size) | Increased adiposity impacted pubertal onset by influencing leptin and sex hormones (p < 0.01 in related studies) | Body fat influences pubertal timing through multiple mechanisms |
| Lee et al. (2010) [9] | Longitudinal cohort study | 401 boys aged 5–12 years (U.S.) | Higher BMI was associated with earlier pubertal initiation, particularly in pubic hair and genital development (p < 0.01) | Childhood obesity is linked to earlier pubertal initiation in boys with stronger associations for higher BMI |
| Lee et al. (2016) [8] | Cross-sectional | 1601 overweight and boys with obesity aged 6-16 years (U.S.) | Boys with obesity experienced delayed puberty, while overweight boys showed earlier onset compared to normal weight peers (p = 0.03) | Obesity may delay puberty onset, while overweight boys tend to have earlier puberty |
| Mohsenipour et al. (2022) [51] | Cross-sectional | 168 children with obesity from Tehran, Iran, ages 7–14 | Delayed puberty was significantly more common in boys with obesity than girls with obesity (p = 0.029) | Obesity may delay puberty in boys more frequently than in girls |
| Ong et al. (2006) [41] | Review | Various European population-based studies on timing and tempo of puberty (no specific population size) | Secular trends in Europe showed links between body size and earlier pubertal onset (p < 0.05) | Body size influences secular trends in pubertal timing in Europe |
| Reinehr and Roth (2019) [54] | Review | Various studies on obesity and puberty (no specific population size) | Leptin and other metabolic factors were involved in the relationship between obesity and puberty (p < 0.05 in several studies) | Obesity may influence puberty onset through metabolic and hormonal pathways |
| Reference | Type of Study | Study Population | Main Results | Conclusion |
|---|---|---|---|---|
| Salas-Huetos et al. (2021) [10] | Systematic review and meta-analysis | Various studies (60 for qualitative analysis, 28 for quantitative analysis) on association between adiposity, sperm quality, and reproductive hormones | Overweight and/or obesity were associated with low semen quality and altered reproductive hormones (p < 0.05) | Healthy body weight is important for sperm quality parameters and male fertility |
| AbbasiHormozi et al. (2023) [11] | Cross-sectional | 40 healthy men, 40 men with obesity, 35 lean males with DM, 35 males with obesity and DM | Sperm parameters were significantly lower and leptin levels were significantly increased in cases compared to controls. Total testosterone and SHBG were significantly lower in men with obesity and DM. Insulin positively correlated to metabolic-associated indices and hsCRP, whereas it negatively correlated with sperm parameters | Obesity and diabetes are associated with metabolic changes, hormonal dysfunction, and inflammatory disturbance that may explain subfertility |
| La Vignera et al. (2019) [12] | Interventional study | Males with insulin-resistance and normogonadotropic idiopathic infertility receiving 150 units of FSH 3 times a week alone (n = 35, group A) or in association with slow-release metformin 500 mg/day (n = 35, group B) | Group B obtained higher sperm DNA fragmentation normalization rate (p = 0.03), sperm concentration, progressive motility, and morphology (p < 0.0001) | The addition of metformin in insulin-resistant infertile males improves the efficacy of FSH therapy |
| Tsilidis et al. (2013) [90] | Observational retrospective study | 809 adult men | Higher testosterone was associated with lower CRP (p < 0.05), while higher estradiol correlated with higher CRP and WBC (p < 0.05). SHBG was inversely correlated to WBC (p = 0.04) | Higher androgen and lower estrogen correlate to anti-inflammatory markers in men |
| Yeap et al. (2014) [91] | Cross-sectional observational study | 2143 men aged 17–97 years | Testosterone was inversely associated with metabolic syndrome score. In multivariable models, higher testosterone was associated with lower age, BMI, and CRP | Circulating androgens are more related to age and metabolic factors than cardiovascular or chronic disease |
| Pini et al. (2020) [93] | Observational study | 5 men with no overt andrological diagnosis, analysis of sperm proteome (2034 proteins) | 24 sperm proteins involved in inflammation, oxidative stress, DNA damage repair and sperm function were significantly (p < 0.05) less abundant in men with obesity compared with healthy weight controls | In men with obesity, oxidative stress and inflammation have negative impact on proteins involved in spermatogenesis, leading to subfertility |
| Thomas et al. (2013) [112] | Cross-sectional study | 96 adult males stratified in normal weight, overweight, and obese groups | Adipokine levels were different in serum and seminal plasma. Higher BMI was associated with decreased seminal progranulin. Adiponectin and progranulin levels in seminal plasma correlated positively with sperm parameters (p < 0.05) | Adipokines influence sperm functionality |
| Moretti et al. (2014) [115] | Cross-sectional study | 110 adult males, 47 with infertility and 63 without a history of infertility | Resistin concentration was higher in semen than in serum, had negative correlations with sperm motility, and positive correlations with apoptotic sperm and TNF-α and IL-6 levels. Cytokine levels were significantly higher in infertile patients compared with controls | Semen resistin may play a regulatory role in inflammation of the male reproductive system |
| Andersen et al. (2022) [128] | Randomized controlled trial | 56 adult males (18–65 years) with obesity assigned to 8-week low-calorie diet followed by randomization to 52 weeks of either placebo, exercise training, liraglutide, or liraglutide combined with exercise training | Men lost on average 16.5 kg, which increased sperm concentration (p < 0.01) and sperm count (p < 0.01). These improvements were maintained for 52 weeks in men who maintained the weight loss | Sperm parameters improved after weight loss (both through exercise or liraglutide) in men with obesity |
| Raee et al. (2023) [13] | Cross-sectional cohort study | Semen analysis of 32 males with obesity and 32 normal-weight controls | Short telomere length was negatively correlated to BMI, sperm DNA fragmentation index, immature chromatin, and intracellular ROS levels in patients with obesity (p < 0.05). Obesity was associated with worse semen parameters and higher percentages of DNA fragmentation index, immature chromatin, apoptosis, and elevated ROS levels | Obesity is associated with sperm telomere shortening |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calcaterra, V.; Tiranini, L.; Magenes, V.C.; Rossi, V.; Cucinella, L.; Nappi, R.E.; Zuccotti, G. Impact of Obesity on Pubertal Timing and Male Fertility. J. Clin. Med. 2025, 14, 783. https://doi.org/10.3390/jcm14030783
Calcaterra V, Tiranini L, Magenes VC, Rossi V, Cucinella L, Nappi RE, Zuccotti G. Impact of Obesity on Pubertal Timing and Male Fertility. Journal of Clinical Medicine. 2025; 14(3):783. https://doi.org/10.3390/jcm14030783
Chicago/Turabian StyleCalcaterra, Valeria, Lara Tiranini, Vittoria Carlotta Magenes, Virginia Rossi, Laura Cucinella, Rossella Elena Nappi, and Gianvincenzo Zuccotti. 2025. "Impact of Obesity on Pubertal Timing and Male Fertility" Journal of Clinical Medicine 14, no. 3: 783. https://doi.org/10.3390/jcm14030783
APA StyleCalcaterra, V., Tiranini, L., Magenes, V. C., Rossi, V., Cucinella, L., Nappi, R. E., & Zuccotti, G. (2025). Impact of Obesity on Pubertal Timing and Male Fertility. Journal of Clinical Medicine, 14(3), 783. https://doi.org/10.3390/jcm14030783








