Dimensions Define Stability: Insertion Torque of Orthodontic Mini-Implants: A Comparative In Vitro Study
Abstract
:1. Introduction
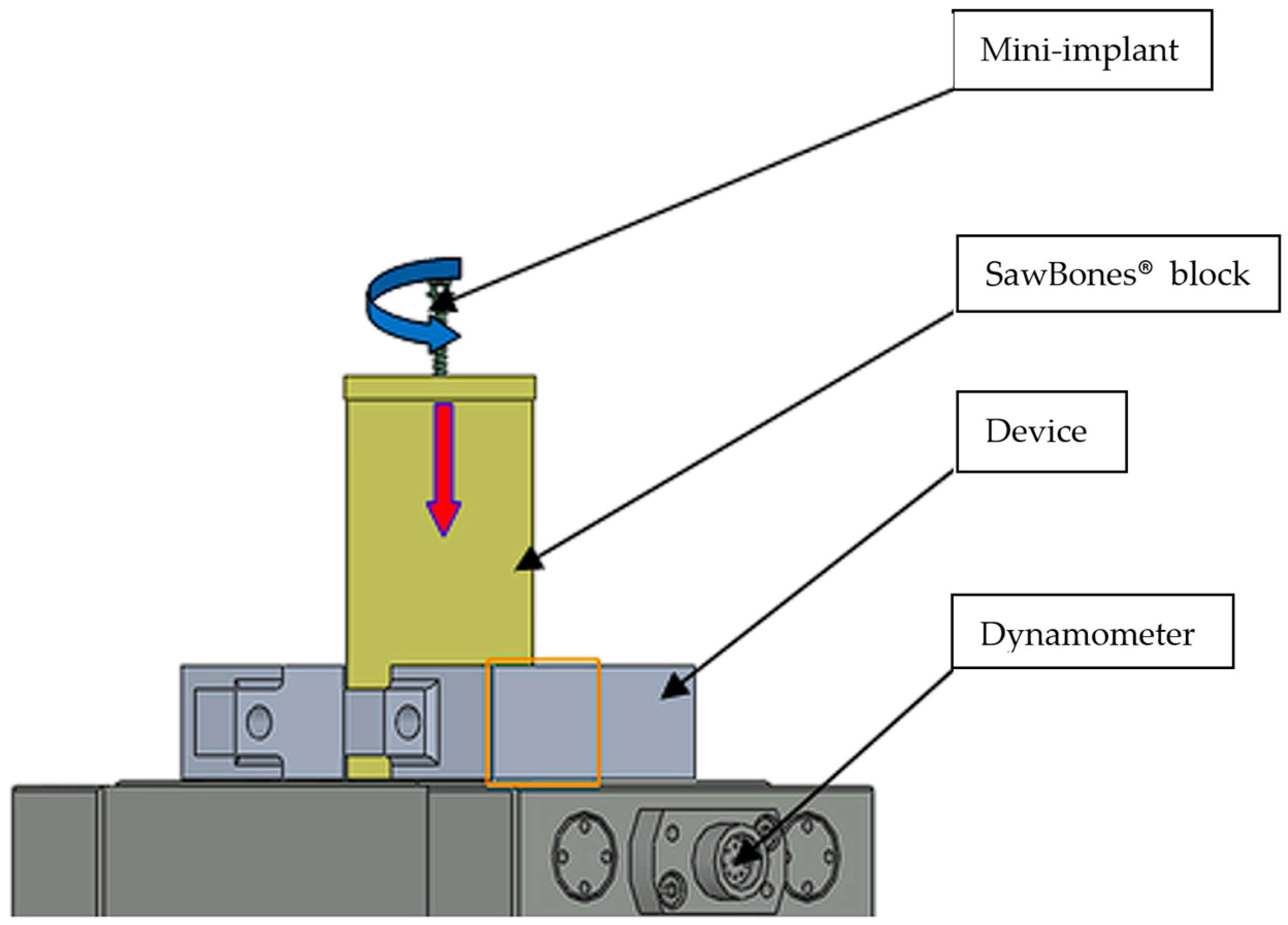
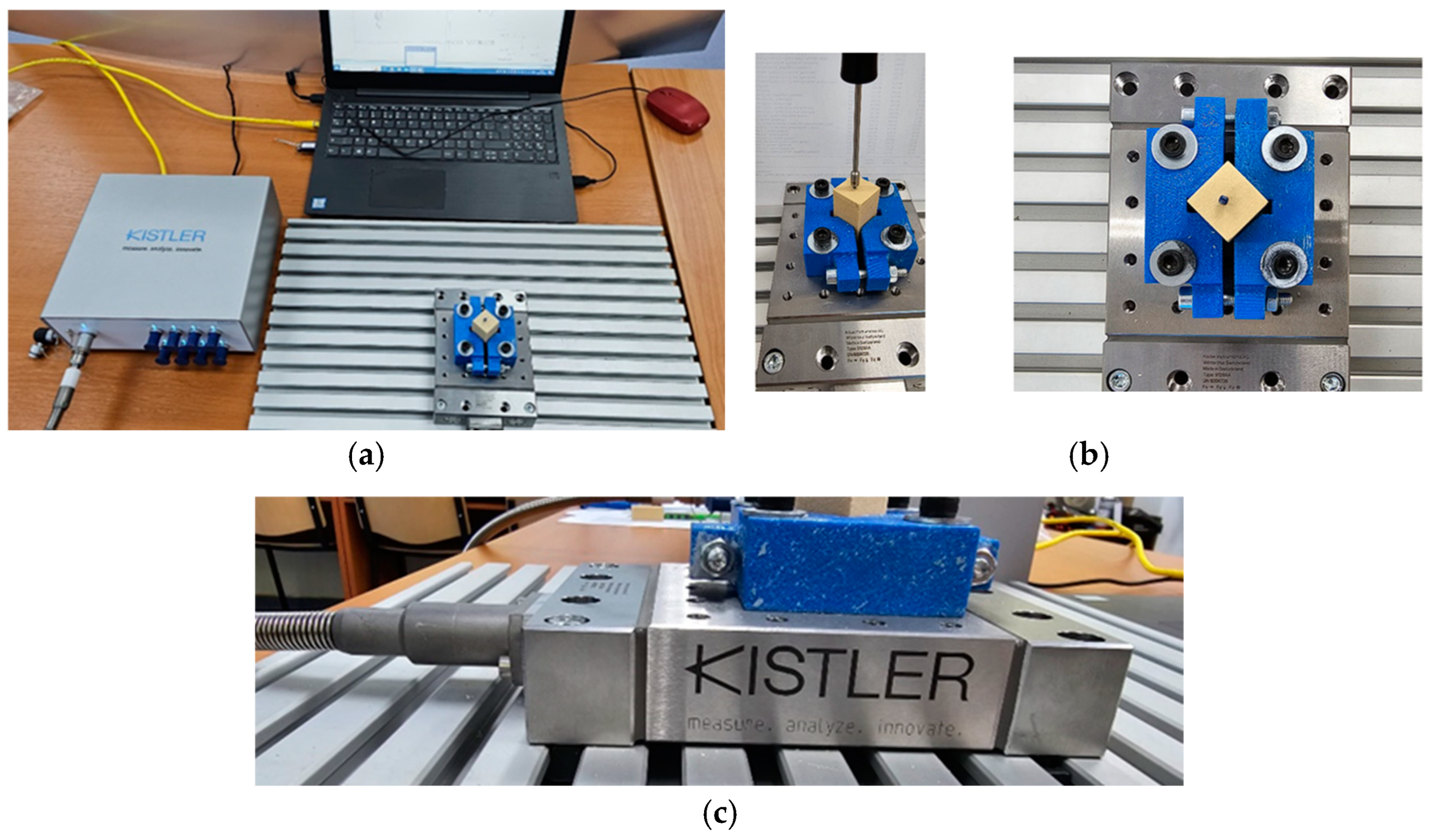
2. Materials and Methods
2.1. Ethical Clearance
2.2. Pilot Study Design
- Group 1: Lengths of 6.0 mm with varying diameters (1.4, 1.6, and 2.0 mm);
- Group 2: Lengths of 8.0 mm with varying diameters (1.4, 1.6, and 2.0 mm);
- Group 3: Lengths of 10.0 mm with varying diameters (1.4, 1.6, and 2.0 mm);
- Group 4: Lengths of 12.0 mm with varying diameters (1.4, 1.6, and 2.0 mm).
2.3. Artificial Bone Model and Mechanical Testing Standards
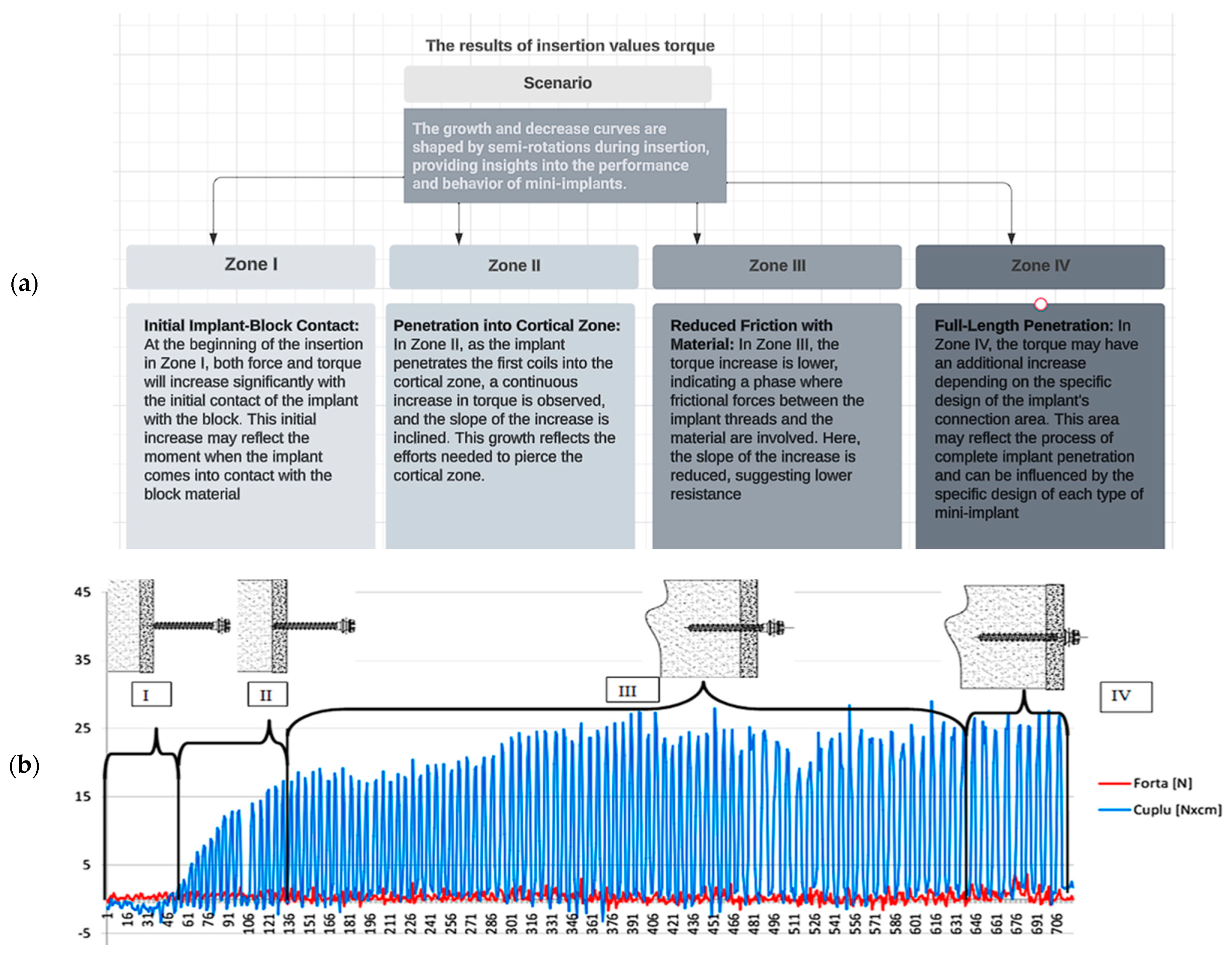
2.4. Data Acquisition and Biomechanical Analysis of Insertion Force (IF) and Torque
- Zone I—Where the contact between the implant and the block occurs;
- Zone II—After penetrating the first coils of the implant into the cortical zone, an increase in torque can be observed until piercing this zone, and the slope of the increase inclines;
- Zone III—An area where the increase in driving torque due to friction between the implant’s flanks and the material has a very low slope of increase;
- Zone IV—The zone where the implant has penetrated the entire length and, depending on the shape of the implant’s connection area (between the cylindrical zone and the head of the implant), there may be an additional torque increase. The shape of the curves with a growth–decrease pattern is caused by each semi-rotation of the implant/screwdriver used.
2.5. Data Analysis
3. Results
3.1. Comparative Analysis of IF and Torque Across Mini-Implant Types and Sizes
3.2. Statistical Analysis: Analysis of Insertion Differences Among Types of Mini-Implants
3.3. Analysis of Insertion Differences Among Types of Mini-Implants
4. Discussion
4.1. Limitations of the Study
- Limited sample size: This study examines a total of 12 mini-implants from three different manufacturers, categorized into four groups based on diameter and length. While this provided valuable insights into the mechanical properties of these specific mini-implants, a larger sample size and inclusion of additional brands could offer a more comprehensive understanding of IT variability.
- Lack of pre-drilling: Mini-implants were inserted at a 90° angle into the artificial bone without pre-drilling. While this simulated clinical conditions where pre-drilling may not always be feasible, it could have influenced the IT values observed. Pre-drilling is a common clinical practice that can impact the stability and torque values of mini-implants.
- Single torque measurement: This study focused solely on maximum IT values and did not assess removal torques or mechanical stability over time. Evaluating both insertion and removal torques, as well as assessing mechanical stability under loading conditions, would provide a more comprehensive understanding of mini-implant performance.
- Manufacturer-specific differences: Variability in mini-implant design and manufacturing processes among different brands may have influenced the observed torque values. While this study compares mini-implants from three manufacturers, additional factors such as surface treatment and material composition could also contribute to torque variability, but were not addressed in this analysis.
4.2. Future Directions
- Randomized controlled trials (RCTs): Conducting RCTs will help validate these findings in real clinical scenarios, ensuring a higher level of evidence.
- Comparative studies: Future research should compare mini-implants with alternative anchorage devices to determine the most effective approach in different orthodontic cases.
- Long-term clinical validation: Future studies should investigate the long-term stability and success rates of different mini-implant designs in in vivo conditions.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jacobson, A. Mini-implants in orthodontics: Innovative anchorage concepts. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 471–472. [Google Scholar] [CrossRef]
- Anbarasu, P.; Ramesh, B.; Annamalai, I.; Subramanian, S. Mini implant ‘safe zones’ in orthodontics: A comprehensive review. Arch. Oral Biol. 2022, 12, 9–18. [Google Scholar] [CrossRef]
- Seifi, M.; Matini, N.S. Evaluation of primary stability of innovated orthodontic miniscrew system (STS). An ex-vivo study. J. Clin. Exp. Dent. 2016, 8, 255–259. [Google Scholar] [CrossRef]
- Lim, S.A.; Cha, J.Y.; Hwang, C.J. Insertion torque of orthodontic miniscrews according to changes in shape, diameter and length. Angle Orthod. 2008, 78, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Fuh, L.; Tsai, M.; Hsu, J. The effects of insertion approach on the stability of dental implants. Appl. Bionics Biomech. 2022, 2022, 7188240. [Google Scholar] [CrossRef]
- Trisi, P.; Perfetti, G.; Baldoni, E.; Berardi, D.; Colagiovanni, M.; Scogna, G. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Implant. Res. 2009, 20, 46771. [Google Scholar] [CrossRef]
- Torres, P.; Deglow, E.; Zubizarreta-Macho, Á.; Tzironi, G.; Menéndez, H.; Castro, J.; Montero, S. Effect of the computer-aided static navigation technique on the accuracy of bicortical mini-implants placement site for maxillary skeletal expansion appliances: An in vitro study. BMC Oral Health 2023, 23, 86. [Google Scholar] [CrossRef]
- Gapski, R.; Wang, H.L.; Mascarenhas, P.; Lang, N.P. Critical review of immediate implant loading. Clin. Oral Implant. Res. 2003, 14, 515–527. [Google Scholar] [CrossRef]
- Cleek, T.M.; Reynolds, K.J.; Hearn, T.C. Effect of screw torque level on cortical bone pull out strength. J. Orthop. Trauma 2007, 21, 117–123. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Hirabayashi, M.; Uemura, M.; Shimizu, N. Recommended placement torque when tightening an orthodontic mini-implant. Clin. Oral Implant. Res. 2005, 17, 109–114. [Google Scholar] [CrossRef]
- Leles, C.; Leles, J.; Curado, T.; Silva, J.; Nascimento, L.; Paula, M.; McKenna, G. Mandibular bone characteristics, drilling protocols, and final insertion torque for titanium-zirconium mini-implants for overdentures: A cross-sectional analysis. Clin. Implant. Dent. Relat. Res. 2023, 25, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.; Nojima, L.; Nojim, M.; Ruellas, A. Comparative study of fracture torque for orthodontic mini-implants of different trademarks. Oral Surg. 2008, 1, 84–87. [Google Scholar] [CrossRef]
- Meira, T.M.; Tanaka, O.M.; Ronsani, M.M.; Maruo, I.T.; Guariza-Filho, O.; Camargo, E.S.; Maruo, H. Insertion torque, pull-out strength and cortical bone thickness in contact with orthodontic mini-implants at different insertion angles. Eur. J. Orthod. 2013, 35, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Cho, J.H.; Chung, K.R.; Kook, Y.A.; Nelson, G. Removal torque values of surface-treated mini-implants after loading. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 36–43. [Google Scholar] [CrossRef]
- Chang, J.Z.; Chen, Y.J.; Tung, Y.Y.; Chiang, Y.Y.; Lai, E.H.; Chen, W.P.; Lin, C.P. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef]
- Florvaag, B.; Kneuertz, P.; Lazar, F.; Koebke, J.; Zoller, J.E.; Braumann, B.; Mischkowski, R.A. Biomechanical properties of orthodontic miniscrews. An in vitro study. J. Orofac. Orthop. 2010, 71, 5367. [Google Scholar] [CrossRef]
- Montasser, M.A.; Scribante, A. Root injury during interradicular insertion is the most common complication associated with orthodontic miniscrews. J. Evid. Based Dent. Pract. 2022, 22, 101688. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Wu, Y.; Chen, C.; Wang, C.; Zhao, L. Miniscrews for orthodontic anchorage: Analysis of risk factors correlated with the progressive susceptibility to failure. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e192–e202. [Google Scholar] [CrossRef]
- Vinodh, S.; Sangamesh, B.; Patil, V.; Ahmed, S.; Naidu, V. Fracture resistance of commonly used self-drilling mini-implants of various diameters. J. Indian Orthod. Soc. 2020, 54, 31–38. [Google Scholar] [CrossRef]
- Malik, F.; Khan, F.; Ali, S.; Rana, F.; Haq, H.; Hussain, M. Factors affecting success and failure of orthodontic mini-implants: A retrospective review. Prof. Med. J. 2023, 30, 285–291. [Google Scholar] [CrossRef]
- Giudice, A.; Rustico, L.; Longo, M.; Oteri, G.; Papadopoulos, M.; Nucera, R. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J. Orthod. 2021, 51, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.; Hajeer, M.; Sultan, K.; Almahdi, W.H.; Alhaffar, J.B.; Almahdi, W.H. Evaluation of the patient-reported outcome measures (proms) with temporary skeletal anchorage devices in fixed orthodontic treatment: A systematic review. Cureus 2023, 3, 150–170. [Google Scholar] [CrossRef]
- Ravi, J.; Duraisamy, S.; Rajaram, K.; Kannan, R.; Arumugam, E. Survival rate and stability of surface-treated and non-surface-treated orthodontic mini-implants: A randomized clinical trial. Dent. Press J. Orthod. 2023, 28, e2321345. [Google Scholar] [CrossRef]
- Najjar, H.; Ghander, F.; Almuaysh, A.; Alzaid, S.; Almasaud, L.; Alsobhi, F.; Alsaif, M. Indications and success rates of skeletal anchorage systems in orthodontics. JOHS 2023, 3, 561–567. [Google Scholar] [CrossRef]
- Fayed, M.M.S.; Pazera, P.; Katsaros, C. Optimal sites for orthodontic mini-implant placement assessed by cone beam computed tomography. Angle Orthod. 2010, 80, 939–951. [Google Scholar] [CrossRef] [PubMed]
- ASTMF1839-08; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. ASTM International: West Conshohocken, PA, USA, 2008.
- Pan, C.; Liu, P.; Tseng, Y.; Chou, S.; Wu, C.; Chang, H. Effects of cortical bone thickness and trabecular bone density on primary stability of orthodontic mini-implants. J. Dent. Sci. 2019, 14, 383–388. [Google Scholar] [CrossRef]
- Sawbone. Available online: https://www.sawbones.com/endpoint-virtual-orthopedic-mechanical-implant-tests-fea (accessed on 1 March 2025).
- ASTM F543-A2; Standard Specification and Test Methods for Metallic Medical Bone Screws. ASTM International: West Conshohocken, PA, USA, 2017. Available online: https://www.astm.org/f0543-02.html (accessed on 1 November 2022).
- Nucera, R.; Costa, S.; Bellocchio, A.; Barbera, S.; Drago, S.; Silvestrini, A.; Migliorati, M. Evaluation of palatal bone depth, cortical bone, and mucosa thickness for optimal orthodontic miniscrew placement performed according to the third palatal ruga clinical reference. Eur. J. Orthod. 2022, 44, 530–536. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Amorfini, L.; Nucera, R.; Silvestrini-Biavati, A. Maximum insertion torque loss after miniscrew placement in orthodontic patients: A randomized controlled trial. Orthod. Craniofac. Res. 2020, 24, 386–395. [Google Scholar] [CrossRef]
- Wilmes, B.; Ottenstreuer, S.; Su, Y.; Drescher, D. Impact of implant design on primary stability of orthodontic mini-implants. J. Orofac. Orthop. 2008, 69, 42–50. [Google Scholar] [CrossRef]
- Wilmes, B.; Su, Y.; Drescher, D. Insertion angle impact on primary stability of orthodontic mini-implants. Angle Orthod. 2008, 78, 1065–1070. [Google Scholar] [CrossRef]
- Chen, Y.; Kyung, H.; Gao, L.; Yu, W.; Bae, E.; Kim, S. Mechanical properties of self-drilling orthodontic micro-implants with different diameters. Angle Orthod. 2010, 80, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Miglani, A.; Cyan, C. Effects of a mini implant’s size and site on its stability using resonance frequency analysis. J. Indian Orthod. Soc. 2020, 55, 138–145. [Google Scholar] [CrossRef]
- Dutta, S.; Bhat, J. Orthodontic mini implant and their primary stability: A comparative study. Int. J. Appl. Dent. Sci. 2021, 8, 642–644. [Google Scholar] [CrossRef]
- Drescher, D. Impact of bone quality, implant type, and implantation site preparation on insertion torques of mini-implants used for orthodontic anchorage. Int. J. Oral Maxillofac. Surg. 2011, 40, 697703. [Google Scholar] [CrossRef]
- Asok, N. Retention of mini screws in orthodontics—A comparative in vitro study on the variables. South Eur. J. Orthod. Dentofac. Res. 2021, 7, 38–42. [Google Scholar] [CrossRef]
- Kim, S.; Lee, S.; Cho, I.; Kim, S.; Kim, T. Rotational resistance of surface-treated mini-implants. Angle Orthod. 2009, 79, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Oh, N.; Kim, E.; Paek, J.; Kook, Y.; Jeong, D.; Cho, I.; Nelson, G. Evaluation of stability of surface-treated mini-implants in diabetic rabbits. Int. J. Dent. 2014, 2014, 838356. [Google Scholar] [CrossRef]
- Nova, M.; Carvalho, F.; Elias, C.; Artese, F. Avaliação do torque para inserção, remoção e fratura de diferentes mini-implantes ortodônticos. Dent. Press J. Orthod. 2008, 13, 76–87. [Google Scholar] [CrossRef]
- Atieh, M.; Baqain, Z.; Tawse-Smith, A.; Ma, S.; Almoselli, M.; Lin, L.; Alsabeeha, N. The influence of insertion torque values on the failure and complication rates of dental implants: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2021, 23, 341–360. [Google Scholar] [CrossRef]
- Singh, J.; Singh, S.; Gupta, A.; Nayak, S.; Vatsa, R.; Priyadarshni, P. Comparative evaluation of primary stability of two different types of orthodontic mini-implants. J. Pharm. Bioallied Sci. 2021, 13, 128. [Google Scholar] [CrossRef]
- Park, K.; Kwon, J.; Kim, S.; Heo, S.; Koak, J.; Lee, J.; Kim, M. The relationship between implant stability quotient values and implant insertion variables: A clinical study. J. Oral Rehabil. 2011, 39, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Assad-Loss, T.; Kitahara-Céia, F.; Silveira, G.; Elias, C.; Mucha, J. Fracture strength of orthodontic mini-implants. Dent. Press J. Orthod. 2017, 22, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.; Jensen, E.; Sampson, W.; Dreyer, C. Torque requirements and the influence of pilot holes on orthodontic miniscrew microdamage. Appl. Sci. 2021, 11, 3564. [Google Scholar] [CrossRef]
- Redžepagić-Vražalica, L.; Mesic, E.; Pervan, N.; Hadžiabdić, V.; Delić, M.; Glušac, M. Impact of implant design and bone properties on the primary stability of orthodontic mini-implants. Appl. Sci. 2021, 11, 1183. [Google Scholar] [CrossRef]

| Density | Compression | Tension | Shear | |||||
|---|---|---|---|---|---|---|---|---|
| PCF | g/cc | Fractional Volume | Strength MPa | Modulus MPa | Strength MPa | Modulus MPa | Strength MPa | Modulus MPa |
| 20 | 0.32 | 0.27 | 8.4 | 210 | 5.6 | 284 | 4.3 | 49 |
| 40 | 0.64 | 0.54 | 31 | 759 | 19 | 1000 | 11 | 130 |
| Group | Diameter (mm) | Type | Manufacturer | IF (N) | IT (N/cm) |
|---|---|---|---|---|---|
| 1: Length 6 mm | 1.4 | Self-drilling | Jeil | 1.2–1.5 | 12–14 |
| 1.6 | Self-drilling | Jeil | 1.8–2 | 16–17 | |
| 2.0 | Self-drilling | Jeil | 2.3–2.4 | 25 | |
| 2: Length 8 mm | 1.4 | Self-drilling | Leone | 2.26–2.8 | 18–19 |
| 1.6 | Self-drilling | Jeil | 2.7 | 28–30 | |
| 2.0 | Self-drilling | Lomas | 3.6–3.8 | 34–35 | |
| 3: Length 10 mm | 1.4 | Self-drilling | Jeil | 3.5 | 20–22 |
| 1.6 | Self-drilling | Leone | 3.5 | 18 | |
| 2.0 | Self-drilling | Lomas | 3.0 | 27–28 | |
| 4: Length 12 mm | 1.4 | Self-drilling | Lomas | 4.3–5.0 | 20–23 |
| 1.6 | Self-drilling | Leone | 4.7 | 13–15 | |
| 2.0 | Self-drilling | Jeil | 4.5 | 20–23 |
| Manufacturer | Indicator | Mean | Median | Standard Deviation |
|---|---|---|---|---|
| Jeil | Average IF | 2.850 | 2.550 | 1.2502 |
| Average IT | 21.83 | 22.50 | 5.707 | |
| Leone | Average IF | 3.633 | 3.500 | 1.0066 |
| Average IT | 17.00 | 18.00 | 1.732 | |
| Lomas | Average IF | 3.400 | 3.400 | 0.5657 |
| Average IT | 31.50 | 31.50 | 4.950 |
| Sum of Squares | df | Mean Square | F | Sig. | ||
|---|---|---|---|---|---|---|
| IF | Between Groups | 1.364 | 2 | 0.682 | 0.537 | 0.604 |
| Within Groups | 10.162 | 8 | 1.270 | |||
| Total | 11.525 | 10 | ||||
| IT | Between Groups | 254.848 | 2 | 127.424 | 5.273 | 0.035 |
| Within Groups | 193.333 | 8 | 24.167 | |||
| Total | 448.182 | 10 | ||||
| Variabila | JEL | LEONE | LOMAS |
|---|---|---|---|
| Jeil | 0.390 | 0.097 | |
| Leone | 0.390 | 0.029 * | |
| Lomas | 0.097 | 0.029 * | - |
| Variable | IF—Correlation Coefficient | IF—Sig. (2-Tailed) | IT—Correlation Coefficient | IT—Sig. (2-Tailed) | Diameter—Correlation Coefficient | Diameter—Sig. (2-Tailed) |
|---|---|---|---|---|---|---|
| IF | 1.000 | - | 0.265 | 0.430 | 0.586 | 0.058 |
| IT | 0.265 | 0.430 | 1.000 | - | 0.609 * | 0.047 * |
| Diameter | 0.586 | 0.058 | 0.609 * | 0.047 * | 1.000 | - |
| Variable | IF—Correlation Coefficient | IF—Sig. (2-Tailed) | IT—Correlation Coefficient | IT—Sig. (2-Tailed) | Length—Correlation Coefficient | Length—Sig. (2-Tailed) |
|---|---|---|---|---|---|---|
| IF | 1.000 | - | 0.265 | 0.430 | 0.890 * | 0.000 * |
| IT | 0.265 | 0.430 | 1.000 | - | 0.056 | 0.869 |
| Length | 0.890 * | 0.000 * | 0.056 | 0.869 | 1.000 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romanec, C.L.; Panaite, T.; Zetu, I.N. Dimensions Define Stability: Insertion Torque of Orthodontic Mini-Implants: A Comparative In Vitro Study. J. Clin. Med. 2025, 14, 1752. https://doi.org/10.3390/jcm14051752
Romanec CL, Panaite T, Zetu IN. Dimensions Define Stability: Insertion Torque of Orthodontic Mini-Implants: A Comparative In Vitro Study. Journal of Clinical Medicine. 2025; 14(5):1752. https://doi.org/10.3390/jcm14051752
Chicago/Turabian StyleRomanec, Cristian Liviu, Tinela Panaite, and Irina Nicoleta Zetu. 2025. "Dimensions Define Stability: Insertion Torque of Orthodontic Mini-Implants: A Comparative In Vitro Study" Journal of Clinical Medicine 14, no. 5: 1752. https://doi.org/10.3390/jcm14051752
APA StyleRomanec, C. L., Panaite, T., & Zetu, I. N. (2025). Dimensions Define Stability: Insertion Torque of Orthodontic Mini-Implants: A Comparative In Vitro Study. Journal of Clinical Medicine, 14(5), 1752. https://doi.org/10.3390/jcm14051752








