Digital Cognitive Behavioral Therapy for Panic Disorder and Agoraphobia: A Meta-Analytic Review of Clinical Components to Maximize Efficacy
Abstract
:1. Introduction
2. Methods
2.1. Protocol
2.2. Research Questions
2.3. Eligibility Criteria and Group Definition
2.4. Database and Search Strategy
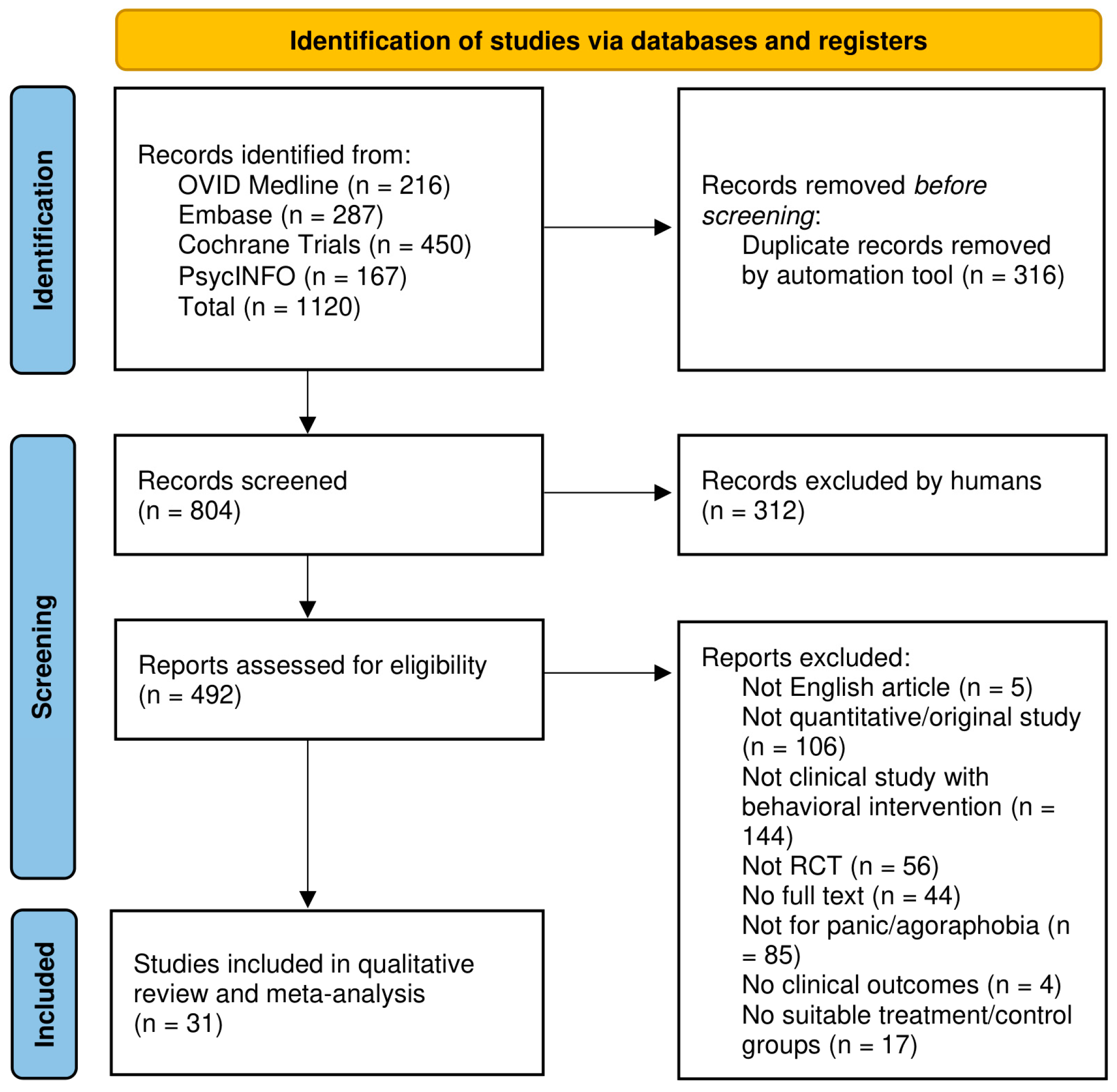
2.5. Study Selection
2.6. Risk of Bias (RoB)
2.7. Intervention Components
2.8. Data Extraction
2.9. Effect Size Estimation
2.10. Statistical Analyses
3. Results
3.1. Selected Studies
3.2. Risk of Bias Assessment
3.3. Assessment of Intervention Components
3.4. Study Characteristics
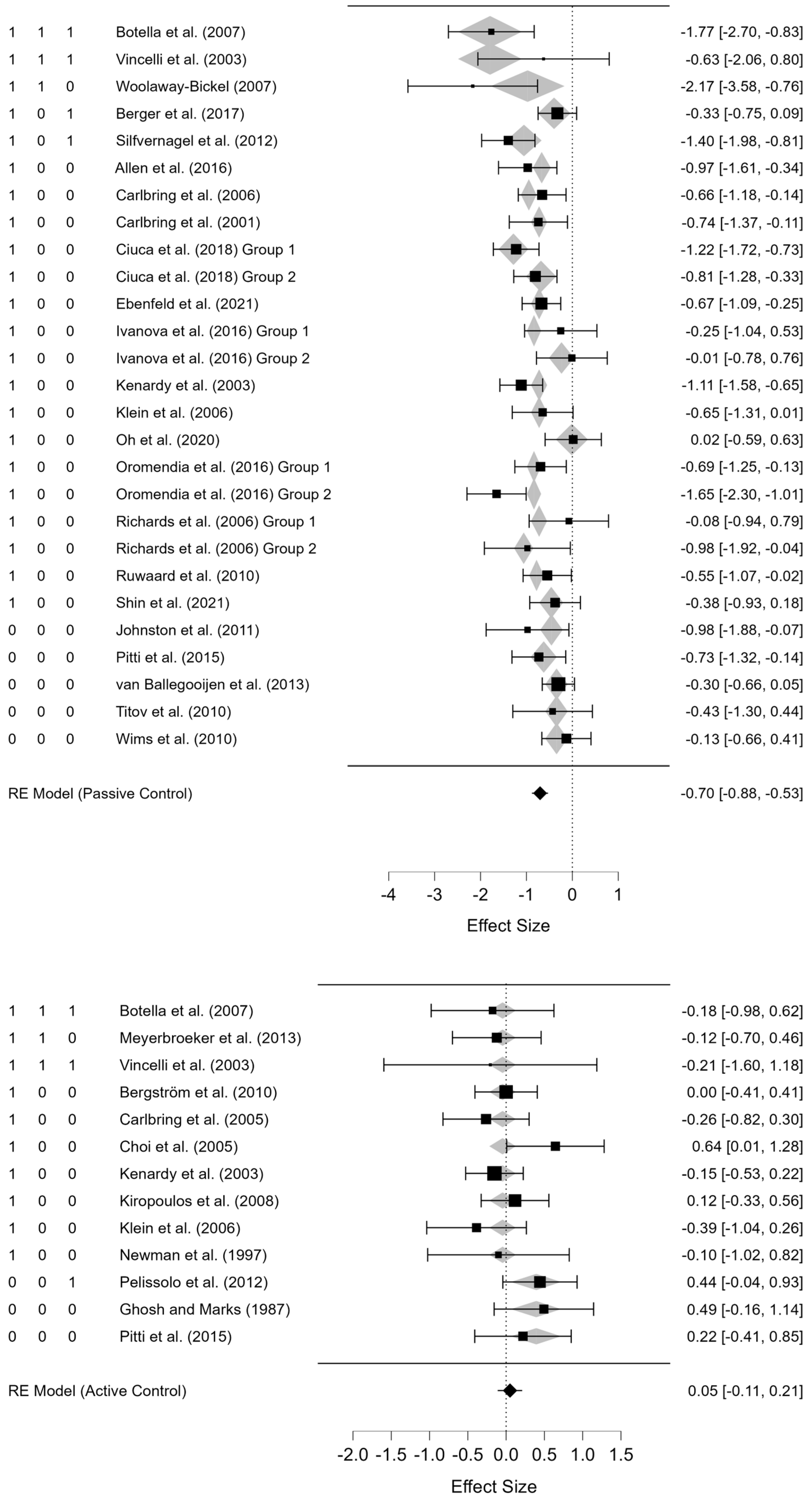
3.5. Overall and Subgroup Effects
3.6. Meta-Regression
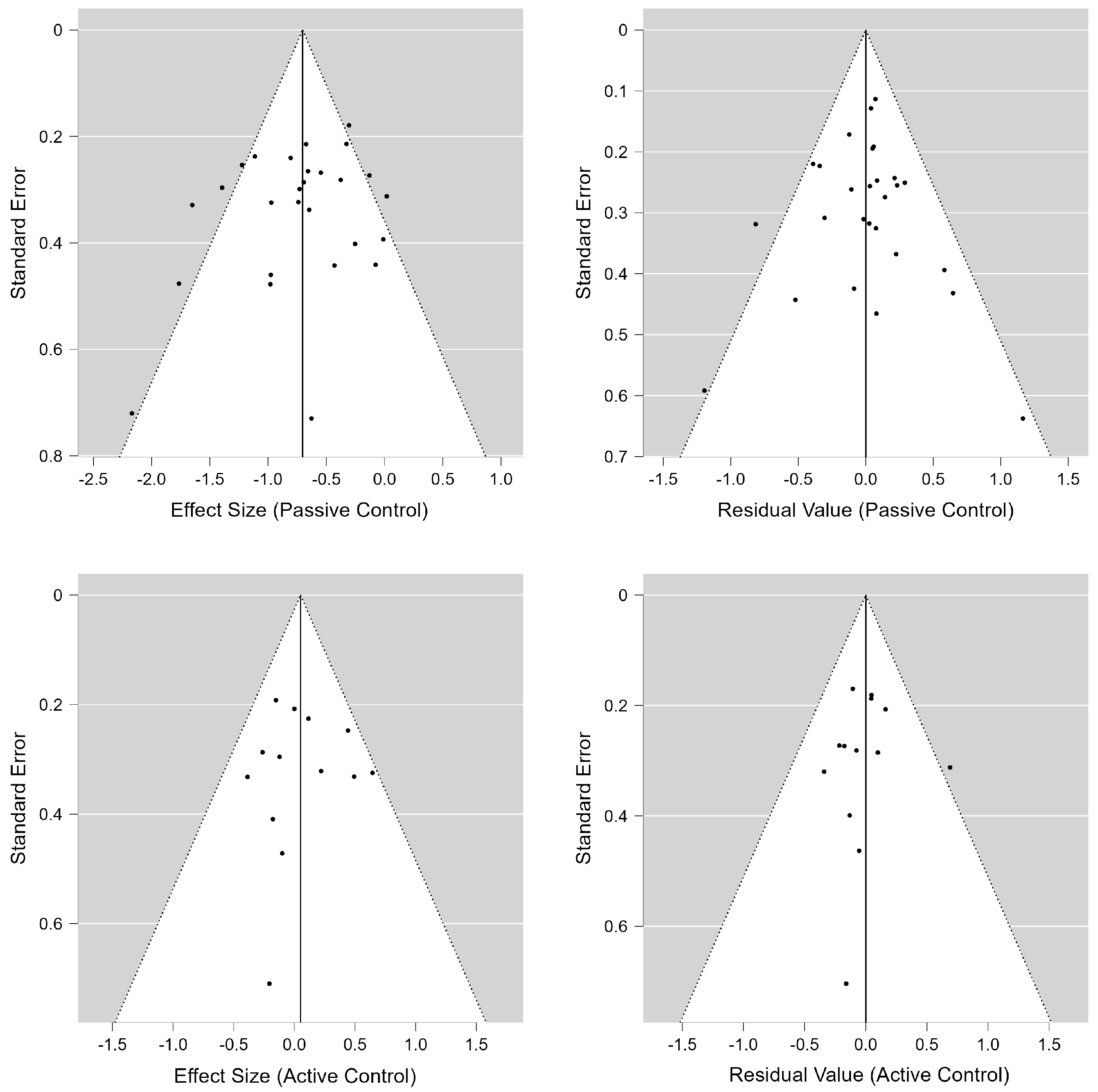
3.7. Publication Bias
4. Discussion
4.1. Limitations
4.2. Conclusions and Implications
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Panic Disorder, 2nd ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2009. [Google Scholar]
- Gunter, R.W.; Whittal, M.L. Dissemination of cognitive-behavioral treatments for anxiety disorders: Overcoming barriers and improving patient access. Clin. Psychol. Rev. 2010, 30, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Carl, J.R.; Miller, C.B.; Henry, A.L.; Stott, R.; Björgvinsson, T. Efficacy of digital cognitive behavioral therapy for moderate-to-severe symptoms of generalized anxiety disorder: A randomized controlled trial. Depress. Anxiety 2020, 37, 1129–1139. [Google Scholar] [CrossRef]
- Hedman, E.; Ljótsson, B.; Lindefors, N. Cognitive behavior therapy via the Internet: A systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev. Pharmacoecon. Outcomes Res. 2012, 12, 745–764. [Google Scholar] [CrossRef] [PubMed]
- Wind, T.R.; Rijkeboer, M.; Andersson, G.; Riper, H. The COVID-19 pandemic: The “black swan” for mental health care and a turning point for e-health. Internet Interv. 2020, 20, 100317. [Google Scholar] [CrossRef]
- Getachew, E.; Adebeta, T.; Muzazu, S.G.Y.; Charlie, L.; Said, B.; Tesfahunei, H.A.; Wanjiru, C.L.; Acam, J.; Kajogoo, V.D.; Solomon, S.; et al. Digital health in the era of COVID-19: Reshaping the next generation of healthcare. Front. Public Health 2023, 11, 942703. [Google Scholar] [CrossRef] [PubMed]
- Ndayishimiye, C.; Lopes, H.; Middleton, J. A systematic scoping review of digital health technologies during COVID-19: A new normal in primary health care delivery. Health Technol. 2023, 13, 273–284. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar]
- Fodor, L.A.; Coteț, C.D.; Cuijpers, P.; Szamoskozi, Ș.; David, D.; Cristea, I.A. The effectiveness of virtual reality-based interventions for symptoms of anxiety and depression: A meta-analysis. Sci. Rep. 2018, 8, 10323. [Google Scholar] [CrossRef]
- Stech, E.P.; Lim, J.; Upton, E.L.; Newby, J.M. Internet-delivered cognitive behavioral therapy for panic disorder with or without agoraphobia: A systematic review and meta-analysis. Cogn. Behav. Ther. 2020, 49, 270–293. [Google Scholar] [CrossRef]
- Firth, J.; Torous, J.; Carney, R.; Newby, J.; Cosco, T.D.; Christensen, H.; Sarris, J. Digital Technologies in the Treatment of Anxiety: Recent Innovations and Future Directions. Curr. Psychiatry Rep. 2018, 20, 56. [Google Scholar] [CrossRef]
- Pompoli, A.; Furukawa, T.A.; Efthimiou, O.; Imai, H.; Tajika, A.; Salanti, G. Dismantling cognitive-behavior therapy for panic disorder: A systematic review and component network meta-analysis. Psychol. Med. 2018, 48, 1945–1953. [Google Scholar] [CrossRef]
- Boettcher, H.; Brake, C.A.; Barlow, D.H. Origins and outlook of interoceptive exposure. J. Behav. Ther. Exp. Psychiatry 2016, 53, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Deacon, B.; Kemp, J.J.; Dixon, L.J.; Sy, J.T.; Farrell, N.R.; Zhang, A.R. Maximizing the efficacy of interoceptive exposure by optimizing inhibitory learning: A randomized controlled trial. Behav. Res. Ther. 2013, 51, 588–596. [Google Scholar] [CrossRef]
- Craske, M.G.; Kircanski, K.; Zelikowsky, M.; Mystkowski, J.; Chowdhury, N.; Baker, A. Optimizing inhibitory learning during exposure therapy. Behav. Res. Ther. 2008, 46, 5–27. [Google Scholar] [CrossRef] [PubMed]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing exposure therapy: An inhibitory learning approach. Behav. Res. Ther. 2014, 58, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Böhnlein, J.; Altegoer, L.; Muck, N.K.; Roesmann, K.; Redlich, R.; Dannlowski, U.; Leehr, E.J. Factors influencing the success of exposure therapy for specific phobia: A systematic review. Neurosci. Biobehav. Rev. 2020, 108, 796–820. [Google Scholar] [CrossRef]
- Smits, J.A.J.; Powers, M.B.; Otto, M.W. Personalized Exposure Therapy: A Person-Centered Transdiagnostic Approach; Oxford University Press: New York, NY, USA, 2019. [Google Scholar]
- Ashley, E.A. The Precision Medicine Initiative. JAMA 2015, 313, 2119. [Google Scholar] [CrossRef]
- Čēšková, E.; Šilhán, P. From Personalized Medicine to Precision Psychiatry? Neuropsychiatr. Dis. Treat. 2021, 17, 3663–3668. [Google Scholar] [CrossRef]
- Harvey, A.; Watkins, E.; Mansell, W.; Shafran, R. Cognitive Behavioural Processes Across Psychological Disorders: A Transdiagnostic Approach to Research and Treatment; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Nordgren, L.B.; Hedman, E.; Etienne, J.; Bodin, J.; Kadowaki, Å.; Eriksson, S.; Lindkvist, E.; Andersson, G.; Carlbring, P. Effectiveness and cost-effectiveness of individually tailored Internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: A randomized controlled trial. Behav. Res. Ther. 2014, 59, 1–11. [Google Scholar] [CrossRef]
- Silfvernagel, K.; Westlinder, A.; Andersson, S.; Bergman, K.; Hernandez, R.D.; Fallhagen, L.; Lundqvist, I.; Masri, N.; Viberg, L.; Forsberg, M.-L.; et al. Individually tailored internet-based cognitive behaviour therapy for older adults with anxiety and depression: A randomised controlled trial. Cogn. Behav. Ther. 2017, 47, 286–300. [Google Scholar] [CrossRef]
- Păsărelu, C.R.; Andersson, G.; Bergman Nordgren, L.; Dobrean, A. Internet-delivered transdiagnostic and tailored cognitive behavioral therapy for anxiety and depression: A systematic review and meta-analysis of randomized controlled trials. Cogn. Behav. Ther. 2016, 46, 1–28. [Google Scholar] [CrossRef]
- National Evidence-based Healthcare Collaborating Agency. NECA’s Guidance for Undertaking Systematic Reviews and Meta-Analyses for Intervention; National Evidence-based Healthcare Collaborating Agency: Seoul, Republic of Korea, 2011. [Google Scholar]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Mehling, W.E.; DiBlasi, Z.; Hecht, F. Bias Control in Trials of Bodywork: A Review of Methodological Issues. J. Altern. Complement. Med. 2005, 11, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Shear, M.K.; Brown, T.A.; Barlow, D.H.; Money, R.; Sholomskas, D.E.; Woods, S.W.; Gorman, J.M.; Papp, L.A. Multicenter Collaborative Panic Disorder Severity Scale. Am. J. Psychiatry 1997, 154, 1571–1575. [Google Scholar] [CrossRef] [PubMed]
- Chambless, D.L.; Caputo, G.C.; Jasin, S.E.; Gracely, E.J.; Williams, C. The Mobility Inventory for Agoraphobia. Behav. Res. Ther. 1985, 23, 35–44. [Google Scholar] [CrossRef]
- Chambless, D.L.; Caputo, G.C.; Bright, P.; Gallagher, R. Assessment of fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. J. Consult. Clin. Psychol. 1984, 52, 1090–1098. [Google Scholar] [CrossRef]
- Marks, I.M.; Mathews, A.M. Brief standard self-rating for phobic patients. Behav. Res. Ther. 1979, 17, 263–277. [Google Scholar] [CrossRef]
- Bandelow, B. Assessing the efficacy of treatments for panic disorder and agoraphobia. II. The Panic and Agoraphobia Scale. Int. Clin. Psychopharmacol. 1995, 10, 73–82. [Google Scholar] [CrossRef]
- Odriozola, E.E.; de Corral Gargallo, P.; Bajos, E.G.; Rovira, D.P.; Mas, M.B. Un nuevo inventario de agorafobia (IA). Análisis Modif. Conducta 1992, 18, 101–123. [Google Scholar]
- McNeish, D. On Using Bayesian Methods to Address Small Sample Problems. Struct. Equ. Model. Multidiscip. J. 2016, 23, 750–773. [Google Scholar] [CrossRef]
- Nomura, S.; Ogata, Y.; Komaki, F.; Toda, S. Bayesian forecasting of recurrent earthquakes and predictive performance for a small sample size. J. Geophys. Res. 2011, 116, B04307. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Gwet, K. Handbook of Inter-Rater Reliability; Stataxis Publishing Company: Gaithersburg, MD, USA, 2001. [Google Scholar]
- Allen, A.R.; Newby, J.M.; Mackenzie, A.; Smith, J.; Boulton, M.; Loughnan, S.A.; Andrews, G. Internet cognitive-behavioural treatment for panic disorder: Randomised controlled trial and evidence of effectiveness in primary care. BJPsych Open 2016, 2, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Berger, T.; Urech, A.; Krieger, T.; Stolz, T.; Schulz, A.; Vincent, A.; Moser, C.T.; Moritz, S.; Meyer, B. Effects of a transdiagnostic unguided Internet intervention (“velibra”) for anxiety disorders in primary care: Results of a randomized controlled trial. Psychol. Med. 2016, 47, 67–80. [Google Scholar] [CrossRef]
- Bergström, J.; Andersson, G.; Ljótsson, B.; Rück, C.; Andréewitch, S.; Karlsson, A.; Carlbring, P.; Andersson, E.; Lindefors, N. Internet-versus group-administered cognitive behaviour therapy for panic disorder in a psychiatric setting: A randomised trial. BMC Psychiatry 2010, 10, 54. [Google Scholar] [CrossRef]
- Botella, C.; García-Palacios, A.; Villa, H.; Baños, R.M.; Quero, S.; Alcañiz, M.; Riva, G. Virtual reality exposure in the treatment of panic disorder and agoraphobia: A controlled study. Clin. Psychol. Psychother. 2007, 14, 164–175. [Google Scholar] [CrossRef]
- Carlbring, P.; Bohman, S.; Brunt, S.; Buhrman, M.; Westling, B.E.; Ekselius, L.; Andersson, G. Remote Treatment of Panic Disorder: A Randomized Trial of Internet-Based Cognitive Behavior Therapy Supplemented With Telephone Calls. Am. J. Psychiatry 2006, 163, 2119–2125. [Google Scholar] [CrossRef]
- Carlbring, P.; Nilsson-Ihrfelt, E.; Waara, J.; Kollenstam, C.; Buhrman, M.; Kaldo, V.; Söderberg, M.; Ekselius, L.; Andersson, G. Treatment of panic disorder: Live therapy vs. self-help via the Internet. Behav. Res. Ther. 2005, 43, 1321–1333. [Google Scholar] [CrossRef] [PubMed]
- Carlbring, P.; Westling, B.E.; Ljungstrand, P.; Ekselius, L.; Andersson, G. Treatment of panic disorder via the internet: A randomized trial of a self-help program. Behav. Ther. 2001, 32, 751–764. [Google Scholar] [CrossRef]
- Choi, Y.H.; Vincelli, F.; Riva, G.; Wiederhold, B.K.; Lee, J.H.; Park, K.H. Effects of Group Experiential Cognitive Therapy for the Treatment of Panic Disorder with Agoraphobia. Cyberpsychol. Behav. 2005, 8, 387–393. [Google Scholar] [CrossRef]
- Ciuca, A.M.; Berger, T.; Crișan, L.G.; Miclea, M. Internet-based treatment for panic disorder: A three-arm randomized controlled trial comparing guided (via real-time video sessions) with unguided self-help treatment and a waitlist control. J. Anxiety Disord. 2018, 56, 43–55. [Google Scholar] [CrossRef]
- Ebenfeld, L.; Lehr, D.; Ebert, D.D.; Stegemann, S.K.; Riper, H.; Funk, B.; Berking, M. Evaluating a Hybrid Web-Based Training Program for Panic Disorder and Agoraphobia: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e20829. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Marks, I.M. Self-treatment of agoraphobia by exposure. Behav. Ther. 1987, 18, 3–16. [Google Scholar] [CrossRef]
- Ivanova, E.; Lindner, P.; Ly, K.H.; Dahlin, M.; Vernmark, K.; Andersson, G.; Carlbring, P. Guided and unguided Acceptance and Commitment Therapy for social anxiety disorder and/or panic disorder provided via the Internet and a smartphone application: A randomized controlled trial. J. Anxiety Disord. 2016, 44, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Johnston, L.; Titov, N.; Andrews, G.; Spence, J.; Dear, B.F. A RCT of a Transdiagnostic Internet-Delivered Treatment for Three Anxiety Disorders: Examination of Support Roles and Disorder-Specific Outcomes. PLoS ONE 2011, 6, e28079. [Google Scholar] [CrossRef]
- Kenardy, J.A.; Dow, M.G.T.; Johnston, D.W.; Newman, M.G.; Thomson, A.; Taylor, C.B. A Comparison of Delivery Methods of Cognitive-Behavioral Therapy for Panic Disorder: An International Multicenter Trial. J. Consult. Clin. Psychol. 2003, 71, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- Kiropoulos, L.A.; Klein, B.; Austin, D.W.; Gilson, K.; Pier, C.; Mitchell, J.; Ciechomski, L. Is internet-based CBT for panic disorder and agoraphobia as effective as face-to-face CBT? J. Anxiety Disord. 2008, 22, 1273–1284. [Google Scholar] [CrossRef]
- Klein, B.; Richards, J.C.; Austin, D.W. Efficacy of internet therapy for panic disorder. J. Behav. Ther. Exp. Psychiatry 2006, 37, 213–238. [Google Scholar] [CrossRef] [PubMed]
- Meyerbroeker, K.; Morina, N.; Kerkhof, G.A.; Emmelkamp, P.M.G. Virtual Reality Exposure Therapy Does Not Provide Any Additional Value in Agoraphobic Patients: A Randomized Controlled Trial. Psychother. Psychosom. 2013, 82, 170–176. [Google Scholar] [CrossRef]
- Newman, M.G.; Kenardy, J.; Herman, S.; Taylor, C.B. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. J. Consult. Clin. Psychol. 1997, 65, 178–183. [Google Scholar] [CrossRef]
- Oh, J.; Jang, S.; Kim, H.; Kim, J.J. Efficacy of mobile app-based interactive cognitive behavioral therapy using a chatbot for panic disorder. Int. J. Med. Inform. 2020, 140, 104171. [Google Scholar] [CrossRef]
- Oromendia, P.; Orrego, J.; Bonillo, A.; Molinuevo, B. Internet-based self-help treatment for panic disorder: A randomized controlled trial comparing mandatory versus optional complementary psychological support. Cogn. Behav. Ther. 2016, 45, 270–286. [Google Scholar] [CrossRef] [PubMed]
- Pelissolo, A.; Zaoui, M.; Aguayo, G.; Yao, S.N.; Roche, S.; Ecochard, R.; Gueyffier, F.; Pull, C.; Berthoz, A.; Jouvent, R.; et al. Virtual reality exposure therapy versus cognitive behavior therapy for panic disorder with agoraphobia: A randomized comparison study. Cyberpsychol. Behav. Soc. Netw. 2012, 5, 35–43. [Google Scholar]
- Pitti, C.T.; Peñate, W.; de la Fuente, J.; Bethencourt, J.M.; Roca-Sánchez, M.J.; Acosta, L.; Villaverde, M.L.; Gracia, R. The combined use of virtual reality exposure in the treatment of agoraphobia. Actas Esp. Psiquiatr. 2015, 43, 133–145. [Google Scholar] [PubMed]
- Richards, J.C.; Klein, B.; Austin, D.W. Internet cognitive behavioural therapy for panic disorder: Does the inclusion of stress management information improve end-state functioning? Clin. Psychol. 2006, 10, 2–15. [Google Scholar] [CrossRef]
- Ruwaard, J.; Broeksteeg, J.; Schrieken, B.; Emmelkamp, P.; Lange, A. Web-based therapist-assisted cognitive behavioral treatment of panic symptoms: A randomized controlled trial with a three-year follow-up. J. Anxiety Disord. 2010, 24, 387–396. [Google Scholar] [CrossRef]
- Shin, B.; Oh, J.; Kim, B.H.; Kim, H.E.; Kim, H.; Kim, S.; Kim, J.-J. Effectiveness of Self-Guided Virtual Reality-based Cognitive Behavioral Therapy for Panic Disorder. JMIR Ment. Health 2021, 8, e30590. [Google Scholar] [CrossRef]
- Silfvernagel, K.; Carlbring, P.; Kabo, J.; Edström, S.; Eriksson, J.; Månson, L.; Andersson, G. Individually Tailored Internet-Based Treatment for Young Adults and Adults With Panic Attacks: Randomized Controlled Trial. J. Med. Internet Res. 2012, 14, e65. [Google Scholar] [CrossRef] [PubMed]
- Titov, N.; Andrews, G.; Johnston, L.; Robinson, E.; Spence, J. Transdiagnostic Internet treatment for anxiety disorders: A randomized controlled trial. Behav. Res. Ther. 2010, 48, 890–899. [Google Scholar] [CrossRef]
- van Ballegooijen, W.; Riper, H.; Klein, B.; Ebert, D.D.; Kramer, J.; Meulenbeek, P.; Cuijpers, P. An Internet-Based Guided Self-Help Intervention for Panic Symptoms: Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e154. [Google Scholar] [CrossRef]
- Vincelli, F.; Anolli, L.; Bouchard, S.; Wiederhold, B.K.; Zurloni, V.; Riva, G. Experiential Cognitive Therapy in the Treatment of Panic Disorders with Agoraphobia: A Controlled Study. Cyberpsychol. Behav. 2003, 6, 321–328. [Google Scholar] [CrossRef]
- Wims, E.; Titov, N.; Andrews, G.; Choi, I. Clinician-Assisted Internet-Based Treatment is Effective for Panic: A Randomized Controlled Trial. Aust. N. Z. J. Psychiatry 2010, 44, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Woolaway-Bickel, K. An Empirical Test of Calm for PD: A Computer-Administered Learning Module for Panic Disorder. Ph.D. Thesis, The Ohio State University, Columbus, OH, USA, 2007. [Google Scholar]
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef]
- Abramowitz, J.S.; Deacon, B.J.; Whiteside, S.P.H. Exposure Therapy for Anxiety, 2nd ed.; Guilford Publications: New York, NY, USA, 2019. [Google Scholar]
- Lindner, P.; Miloff, A.; Hamilton, W.; Reuterskiöld, L.; Andersson, G.; Powers, M.B.; Carlbring, P. Creating state of the art, next-generation Virtual Reality exposure therapies for anxiety disorders using consumer hardware platforms: Design considerations and future directions. Cogn. Behav. Ther. 2017, 46, 404–420. [Google Scholar] [CrossRef]
- Jung, H.W.; Jang, K.W.; Nam, S.; Ahn, M.E.; Lee, S.-K.; Kim, Y.J.; Shin, J.-K.; Park, J.H.; Roh, D. Personalized virtual reality exposure for panic disorder and agoraphobia: A preliminary neurophysiological study. Compr. Psychiatry 2024, 129, 152447. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Cuijpers, P. Internet-Based and Other Computerized Psychological Treatments for Adult Depression: A Meta-Analysis. Cogn. Behav. Ther. 2009, 38, 196–205. [Google Scholar] [CrossRef]
- Bandelow, B.; Wedekind, D. Internet psychotherapeutic interventions for anxiety disorders—A critical evaluation. BMC Psychiatry 2022, 22, 40. [Google Scholar] [CrossRef]
- González-Robles, A.; Miguel, C.; Richards, D.; Duffy, D.; Enrique, Á. A scoping review of therapist behaviors in guided digital mental health interventions. Internet Interv. 2024, 37, 100751. [Google Scholar] [CrossRef] [PubMed]
- Papola, D.; Ostuzzi, G.; Tedeschi, F.; Gastaldon, C.; Purgato, M.; Del Giovane, C.; Pompoli, A.; Pauley, D.; Karyotaki, E.; Sijbrandij, M.; et al. CBT treatment delivery formats for panic disorder: A systematic review and network meta-analysis of randomised controlled trials. Psychol. Med. 2022, 53, 614–624. [Google Scholar] [CrossRef]
- Shaban-Nejad, A.; Michalowski, M.; Buckeridge, D.L. Health intelligence: How artificial intelligence transforms population and personalized health. NPJ Digit. Med. 2018, 1, 53. [Google Scholar] [CrossRef]
- Triantafyllidis, A.K.; Tsanas, A. Applications of Machine Learning in Real-Life Digital Health Interventions: Review of the Literature. J. Med. Internet Res. 2019, 21, e12286. [Google Scholar] [CrossRef]
- Farrokhyar, F.; Skorzewski, P.; Phillips, M.R.; Garg, S.J.; Sarraf, D.; Thabane, L.; Bhandari, M.; Chaudhary, V.; Wykoff, C.C.; Sivaprasad, S.; et al. When to believe a subgroup analysis: Revisiting the 11 criteria. Eye 2022, 36, 2075–2077. [Google Scholar] [CrossRef] [PubMed]
- Inglis, G.; Archibald, D.; Doi, L.; Laird, Y.; Malden, S.; Marryat, L.; McAteer, J.; Pringle, J.; Frank, J. Credibility of subgroup analyses by socioeconomic status in public health intervention evaluations: An underappreciated problem? SSM-Popul. Health 2018, 6, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Briel, M.; Walter, S.D.; Guyatt, G.H. Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ 2010, 340, c117. [Google Scholar] [CrossRef] [PubMed]

| Article | Format | Guide | Symptom | Recruitment | Sample | Diagnosis i | Country | Period | #Sessions | COI | Control | Control Type | n Treat. | n Cont. | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen et al. (2016) [38] | App | Guided | Panic | Online | Public | MINI | AU | 8 weeks | 5 | No | Passive | Waitlist | 16 | 31 ii | PDSS-SR |
| Berger et al. (2017) [39] | App | Unguided | PD/A | Clinic | Patient | SCID | CH/DE | 9 weeks | 6 | Yes | Passive | Waitlist | 48 | 41 | MI-Alone |
| Bergström et al. (2010) [40] | App | Guided | PD/A | Clinic | Patient | MINI | SE | 10 weeks | 10 | No | Active | CBT | 44 | 49 ii | PDSS |
| Botella et al. (2007) [41] | VR | Guided | PD/A | Clinic | Patient | ADIS | ES | 9 weeks | 9 | Yes | Active | IVE | 12 | 12 | PDSS |
| Passive | Waitlist | 12 | 13 | ||||||||||||
| Carlbring et al. (2006) [42] | App | Guided | Panic | Community/Online | Public | SCID | SE | 10 weeks | 10 | No | Passive | Waitlist | 30 | 30 | MI-Alone |
| Carlbring et al. (2005) [43] | App | Guided | Panic | Community/Online | Public | SCID | SE | 10 weeks | 10 | No | Active | CBT | 25 | 24 | MI-Alone |
| Carlbring et al. (2001) [44] | App | Guided | Panic | Community/Online | Public | CIDI | SE | 7–12 weeks | 6 | No | Passive | Waitlist | 21 | 20 | MI-Alone |
| Choi et al. (2005) [45] | FtF + VR | Guided | PDA | Clinic | Patient | DSM-IV | KR | 4 weeks | 4 | No | Active | CBT | 20 | 20 | ACQ |
| Ciuca et al. (2018) [46] Group 1 | App | Guided | Panic | Community/Online | Public | PDSS-SR | RO | 12 weeks | 16 | Yes | Passive | Waitlist | 36 | 38 | PDSS-SR |
| Ciuca et al. (2018) [46] Group 2 | App | Unguided | Panic | Community/Online | Public | PDSS-SR | RO | 12 weeks | 16 | Yes | Passive | Waitlist | 37 | 38 | PDSS-SR |
| Ebenfeld et al. (2021) [47] | App | Guided | PD/A | Community/Online | Public | PAS | DE | 6 weeks | 6 | Yes | Passive | Waitlist | 45 | 47 | PAS |
| Ghosh and Marks (1987) [48] | App | Unguided | Agoraph-obia | Clinic | Patient | DSM-III | UK | 8 weeks | 8 | No | Active | CBT | 15 | 25 ii,iii | FQ-Agoraphobia |
| Ivanova et al. (2016) [49] Group 1 | App | Guided | Panic | Community/Online | Public | SCID | SE | 10 weeks | 8 | Yes | Passive | Waitlist | 13 | 12 | PDSS-SR |
| Ivanova et al. (2016) [49] Group 2 | App | Unguided | Panic | Community/Online | Public | SCID | SE | 10 weeks | 8 | Yes | Passive | Waitlist | 14 | 12 | PDSS-SR |
| Johnston et al. (2011) [50] | App | Guided | PD/A | Online | Public | MINI | AU | 10 weeks | 8 | No | Passive | Waitlist | 20 iv | 7 | PDSS-SR |
| Kenardy et al. (2003) [51] | App | Guided | Panic | Clinic/ Community | Patient + Public | SCID | UK/AU | 6 weeks | 6 | No | Active | CBT | 41 | 81 v | MI-Alone |
| Passive | Waitlist | 41 | 41 | ||||||||||||
| Kiropoulos et al. (2008) [52] | App | Guided | PD/A | Community/Online | Public | ADIS | AU | 6–8 weeks | 6 | No | Active | CBT | 45 | 35 ii | PDSS |
| Klein et al. (2006) [53] | App | Guided | Panic | Community/Online | Public | ADIS | AU | 6–8 weeks | 6 | No | Active | CBT | 19 | 18 | ACQ |
| Passive | Waitlist | 19 | 18 | ||||||||||||
| Meyerbroeker et al. (2013) [54] | VR | Guided | PDA | Clinic | Patient | SCID | NL | 8–10 weeks | 10 | No | Active | IVE | 24 | 22 ii | MI-Alone |
| Newman et al. (1997) [55] | App | Guided | Panic | Community | Public | SCID (DSM-III) | US | 12 weeks | 4 | No | Active | CBT | 9 | 9 ii | MI-Alone |
| Oh et al. (2020) [56] | App | Unguided | Panic | Clinic | Patient | MINI | KR | 4 weeks | N/A vi | No | Passive | Self-help | 21 | 20 ii | PDSS |
| Oromendia et al. (2016) [57] Group 1 | App | Guided | Panic | Online | Public | MINI | ES | 8 weeks | 8 | Yes | Passive | Waitlist | 27 | 25 | PDSS-SR |
| Oromendia et al. (2016) [57] Group 2 | App | Guided | Panic | Online | Public | MINI | ES | 8 weeks | 8 | Yes | Passive | Waitlist | 25 | 25 | PDSS-SR |
| Pelissolo et al. (2012) [58] | VR | Guided | PDA | Clinic | Patient | MINI | FR/LU | 12 weeks | 12 | No | Active | CBT | 33 | 34 ii | PDSS |
| Pitti et al. (2015) [59] | FtF + VR vii | Guided | Agoraph-obia | Clinic | Patient | CIDI | ES | 11 weeks | 11 | No | Active | CBT | 19 | 20 ii | IA |
| Passive | Waitlist | 19 | 32 ii | ||||||||||||
| Richards et al. (2006) [60] Group 1 | App | Guided | Panic | Community/Online | Public | ADIS | AU | 6–8 weeks | 6 | No | Passive | Waitlist | 12 | 9 | ACQ |
| Richards et al. (2006) [60] Group 2 | App | Guided | Panic | Community/Online | Public | ADIS | AU | 6–8 weeks | 6 + 6 | No | Passive | Waitlist | 11 | 9 | ACQ |
| Ruwaard et al. (2010) [61] | App | Guided | Panic | Community | Public | DSM-IV | NL | 11 weeks | 7 | Yes | Passive | Waitlist | 27 | 31 | PDSS-SR |
| Shin et al. (2021) [62] | VR | Unguided | Panic | Clinic | Patient | MINI (DSM-V) | KR | 4 weeks | 12 | No | Passive | Waitlist | 33 | 21 | PDSS |
| Silfvernagel et al. (2012) [63] | App | Guided | Panic | Online | Public | SCID | SE | 8 weeks | 6–8 | No | Passive | Waitlist | 29 | 28 viii | PDSS |
| Titov et al. (2010) [64] | App | Guided | PD/A | Online | Public | MINI | AU | 6–8 weeks | 6 | No | Passive | Waitlist | 10 | 11 | PDSS-SR |
| van Ballegooijen et al. (2013) [65] | App | Guided | Panic | Community/Online | Public | PDSS-SR | NL | 6–12 weeks | 6 | No | Passive | Waitlist | 63 | 63 | PDSS-SR |
| Vincelli et al. (2003) [66] | FtF + VR | Guided | PDA ix | Clinic | Patient | DSM-IV | IT | 8 weeks | 8 + 1 | No | Active | CBT | 4 | 4 | FQ |
| Passive | Waitlist | 4 | 4 | ||||||||||||
| Wims et al. (2010) [67] | App | Guided | PD/A | Online | Public | MINI | AU | 6–8 weeks | 6 | No | Passive | Waitlist | 29 | 25 | MI-Alone |
| Woolaway-Bickel (2007) [68] | App | Unguided | Panic | Community | Public | ADIS | US | 10 weeks | 10 | No | Passive | Waitlist | 7 | 6 ii,x | Agoraphobic Symptom Composite (FQ + MI) |
| Passive Control | Active Control | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| k | m | n | g [95% CI] | I2 | k | m | n | g [95% CI] | I2 | ||
| Overall | 23 | 27 | 1326 | −0.70 [−0.88, −0.53] | 53 | 13 | 13 | 663 | 0.05 [−0.11, 0.21] | 1 | |
| ite | 1 | 18 | 22 | 1047 | −0.76 [−0.96, −0.57] | 53 | 10 | 10 | 517 | −0.05 [−0.22, 0.13] | 0 |
| 0 | 5 | 5 | 279 | −0.40 [−0.64, −0.16] | 0 | 3 | 3 | 146 | 0.39 [0.06, 0.72] | 0 | |
| ile | 1 | 3 | 3 | 46 | −1.60 [−2.28, −0.92] | 0 | 3 | 3 | 78 | −0.15 [−0.59, 0.30] | 0 |
| 0 | 20 | 24 | 1280 | −0.66 [−0.83, −0.49] | 50 | 10 | 10 | 585 | 0.08 [−0.10, 0.26] | 12 | |
| pe | 1 | 4 | 4 | 179 | −1.00 [−1.62, −0.38] | 65 | 3 | 3 | 99 | 0.24 [−0.16, 0.63] | 0 |
| 0 | 19 | 23 | 1147 | −0.66 [−0.83, −0.49] | 45 | 10 | 10 | 564 | 0.02 [−0.15, 0.19] | 0 | |
| Meta-Regression Model for Passive Control [R2 = 0.551, I2 = 0%] | ||||
| Predictor | B | SE | 95% CI | BFinclusion |
| Intercept | 0.59 | 0.26 | [0.08, 1.10] | |
| ite (1) | −0.38 | 0.15 | [−0.67, −0.09] | 22.92 ** |
| ile (1) | −0.63 | 0.38 | [−1.37, 0.12] | 6.44 * |
| pe (1) | −0.27 | 0.20 | [−0.66, 0.12] | 4.27 * |
| Guide (guided) | −0.60 | 0.15 | [−0.90, −0.30] | >100 *** |
| #Sessions | −0.06 | 0.02 | [−0.09, −0.02] | 36.07 ** |
| Meta-Regression Model for Active Control [R2 = 0.409, I2 = 0%] | ||||
| Predictor | B | SE | 95% CI | BFinclusion |
| Intercept | 0.39 | 0.17 | [0.06, 0.72] | |
| ite (1) | −0.44 | 0.19 | [−0.81, −0.07] | 11.26 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, H.W.; Jang, K.W.; Nam, S.; Kim, A.; Lee, J.; Ahn, M.E.; Lee, S.-K.; Kim, Y.J.; Shin, J.-K.; Roh, D. Digital Cognitive Behavioral Therapy for Panic Disorder and Agoraphobia: A Meta-Analytic Review of Clinical Components to Maximize Efficacy. J. Clin. Med. 2025, 14, 1771. https://doi.org/10.3390/jcm14051771
Jung HW, Jang KW, Nam S, Kim A, Lee J, Ahn ME, Lee S-K, Kim YJ, Shin J-K, Roh D. Digital Cognitive Behavioral Therapy for Panic Disorder and Agoraphobia: A Meta-Analytic Review of Clinical Components to Maximize Efficacy. Journal of Clinical Medicine. 2025; 14(5):1771. https://doi.org/10.3390/jcm14051771
Chicago/Turabian StyleJung, Han Wool, Ki Won Jang, Sangkyu Nam, Areum Kim, Junghoon Lee, Moo Eob Ahn, Sang-Kyu Lee, Yeo Jin Kim, Jae-Kyoung Shin, and Daeyoung Roh. 2025. "Digital Cognitive Behavioral Therapy for Panic Disorder and Agoraphobia: A Meta-Analytic Review of Clinical Components to Maximize Efficacy" Journal of Clinical Medicine 14, no. 5: 1771. https://doi.org/10.3390/jcm14051771
APA StyleJung, H. W., Jang, K. W., Nam, S., Kim, A., Lee, J., Ahn, M. E., Lee, S.-K., Kim, Y. J., Shin, J.-K., & Roh, D. (2025). Digital Cognitive Behavioral Therapy for Panic Disorder and Agoraphobia: A Meta-Analytic Review of Clinical Components to Maximize Efficacy. Journal of Clinical Medicine, 14(5), 1771. https://doi.org/10.3390/jcm14051771







