Improving Image Quality of Chest Radiography with Artificial Intelligence-Supported Dual-Energy X-Ray Imaging System: An Observer Preference Study in Healthy Volunteers
Abstract
1. Introduction
2. Materials and Methods
2.1. Support and Funding
2.2. Participant Data
2.3. Image Acquisition
2.4. DE-AI Imaging Algorithm
2.5. Radiation Dose Estimations
2.6. Image Evaluation
2.7. Statistical Analysis
3. Results
3.1. Image Acquisition and Radiation Dose Estimations
3.2. Image Evaluation
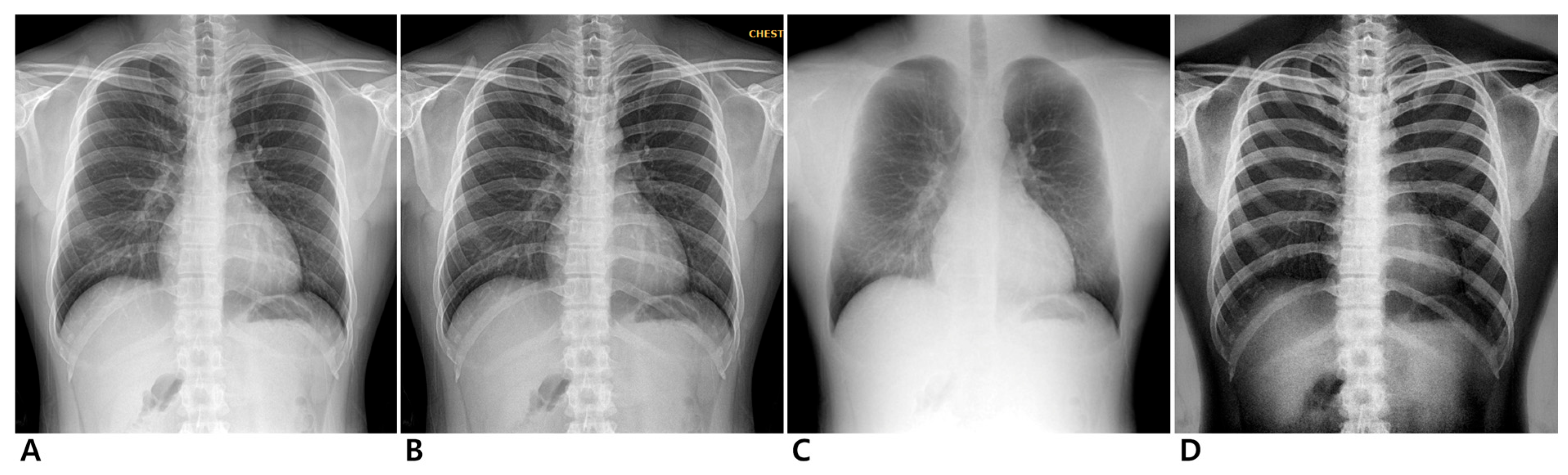
3.2.1. Conventional Standard vs. Enhanced Standard Images
3.2.2. Conventional Standard vs. Soft-Tissue-Selective Images
3.2.3. Conventional Standard vs. Bone-Selective Images
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Hoop, B.; Schaefer-Prokop, C.; Gietema, H.A.; de Jong, P.A.; van Ginneken, B.; van Klaveren, R.J.; Prokop, M. Screening for lung cancer with digital chest radiography: Sensitivity and number of secondary work-up CT examinations. Radiology 2010, 255, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, P.; Bosemani, V.; Cox, J. Do radiologists still need to report chest x rays? Postgrad. Med. J. 2009, 85, 339–341. [Google Scholar] [CrossRef]
- Gavelli, G.; Giampalma, E. Sensitivity and specificity of chest X-ray screening for lung cancer: Review article. Cancer 2000, 89, 2453–2456. [Google Scholar] [CrossRef] [PubMed]
- National Lung Screening Trial Research, T.; Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef]
- Pinsky, P.F.; Church, T.R.; Izmirlian, G.; Kramer, B.S. The National Lung Screening Trial: Results stratified by demographics, smoking history, and lung cancer histology. Cancer 2013, 119, 3976–3983. [Google Scholar] [CrossRef]
- Wender, R.; Fontham, E.T.; Barrera, E., Jr.; Colditz, G.A.; Church, T.R.; Ettinger, D.S.; Etzioni, R.; Flowers, C.R.; Gazelle, G.S.; Kelsey, D.K.; et al. American Cancer Society lung cancer screening guidelines. CA Cancer J. Clin. 2013, 63, 107–117. [Google Scholar] [CrossRef]
- Wolf, A.M.D.; Oeffinger, K.C.; Shih, T.Y.; Walter, L.C.; Church, T.R.; Fontham, E.T.H.; Elkin, E.B.; Etzioni, R.D.; Guerra, C.E.; Perkins, R.B.; et al. Screening for lung cancer: 2023 guideline update from the American Cancer Society. CA Cancer J. Clin. 2024, 74, 50–81. [Google Scholar] [CrossRef]
- Song, L.; Sun, H.; Xiao, H.; Lam, S.K.; Zhan, Y.; Ren, G.; Cai, J. Artificial intelligence for chest X-ray image enhancement. Radiat. Med. Prot. 2025, 6, 61–68. [Google Scholar] [CrossRef]
- Gupta, A.; Kikano, E.G.; Bera, K.; Baruah, D.; Saboo, S.S.; Lennartz, S.; Hokamp, N.G.; Gholamrezanezhad, A.; Gilkeson, R.C.; Laukamp, K.R. Dual energy imaging in cardiothoracic pathologies: A primer for radiologists and clinicians. Eur. J. Radiol. Open 2021, 8, 100324. [Google Scholar] [CrossRef]
- Li, X.; Luo, S.; Hu, Q.; Li, J.; Wang, D. Rib suppression in chest radiographs for lung nodule enhancement. In Proceedings of the 2015 IEEE International Conference on Information and Automation, Lijiang, China, 8–10 August 2015; pp. 50–55. [Google Scholar]
- Ogul, H.; Ogul, B.B.; Agildere, A.M.; Bayrak, T.; Sumer, E. Eliminating rib shadows in chest radiographic images providing diagnostic assistance. Comput. Methods Programs Biomed. 2016, 127, 174–184. [Google Scholar] [CrossRef]
- Zhou, B.; Lin, X.; Eck, B.; Hou, J.; Wilson, D. Generation of Virtual Dual Energy Images from Standard Single-Shot Radiographs Using Multi-scale and Conditional Adversarial Network. In Proceedings of the Computer Vision—ACCV 2018, Perth, Australia, 2–6 December 2018; Springer: Cham, Switzerland, 2019; pp. 298–313. [Google Scholar]
- Li, H.; Han, H.; Li, Z.; Wang, L.; Wu, Z.; Lu, J.; Zhou, S.K. High-Resolution Chest X-Ray Bone Suppression Using Unpaired CT Structural Priors. IEEE Trans. Med. Imaging 2020, 39, 3053–3063. [Google Scholar] [CrossRef] [PubMed]
- Lahmiri, S.; Boukadoum, M. Combined partial differential equation filtering and particle swarm optimization for noisy biomedical image segmentation. In Proceedings of the 2016 IEEE 7th Latin American Symposium on Circuits & Systems (LASCAS), Florianopolis, Brazil, 28 February–2 March 2016; pp. 363–366. [Google Scholar]
- Li, X.; Li, T.; Zhao, H.; Dou, Y.; Pang, C. Medical image enhancement in F-shift transformation domain. Health Inf. Sci. Syst. 2019, 7, 13. [Google Scholar] [CrossRef]
- Jifara, W.; Jiang, F.; Rho, S.; Cheng, M.; Liu, S. Medical image denoising using convolutional neural network: A residual learning approach. J. Supercomput. 2017, 75, 704–718. [Google Scholar] [CrossRef]
- Xu, L.; Zeng, X.; Huang, Z.; Li, W.; Zhang, H. Low-dose chest X-ray image super-resolution using generative adversarial nets with spectral normalization. Biomed. Signal Process. Control 2020, 55, 101600. [Google Scholar] [CrossRef]
- Zhao, C.-Y.; Jia, R.-S.; Liu, Q.-M.; Liu, X.-Y.; Sun, H.-M.; Zhang, X.-L. Chest X-ray images super-resolution reconstruction via recursive neural network. Multimed. Tools Appl. 2020, 80, 263–277. [Google Scholar] [CrossRef]
- Roy, S.; Tyagi, M.; Bansal, V.; Jain, V. SVD-CLAHE boosting and balanced loss function for Covid-19 detection from an imbalanced Chest X-Ray dataset. Comput. Biol. Med. 2022, 150, 106092. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.K.; Ghosh, A. ENResNet: A novel residual neural network for chest X-ray enhancement based COVID-19 detection. Biomed. Signal Process Control 2022, 72, 103286. [Google Scholar] [CrossRef]
- Lind Plesner, L.; Muller, F.C.; Brejnebol, M.W.; Laustrup, L.C.; Rasmussen, F.; Nielsen, O.W.; Boesen, M.; Brun Andersen, M. Commercially Available Chest Radiograph AI Tools for Detecting Airspace Disease, Pneumothorax, and Pleural Effusion. Radiology 2023, 308, e231236. [Google Scholar] [CrossRef]
- Ahn, J.S.; Ebrahimian, S.; McDermott, S.; Lee, S.; Naccarato, L.; Di Capua, J.F.; Wu, M.Y.; Zhang, E.W.; Muse, V.; Miller, B.; et al. Association of Artificial Intelligence-Aided Chest Radiograph Interpretation With Reader Performance and Efficiency. JAMA Netw. Open 2022, 5, e2229289. [Google Scholar] [CrossRef]
- Qin, Z.Z.; Ahmed, S.; Sarker, M.S.; Paul, K.; Adel, A.S.S.; Naheyan, T.; Barrett, R.; Banu, S.; Creswell, J. Tuberculosis detection from chest x-rays for triaging in a high tuberculosis-burden setting: An evaluation of five artificial intelligence algorithms. Lancet Digit. Health 2021, 3, e543–e554. [Google Scholar] [CrossRef]
- Ueda, D.; Matsumoto, T.; Yamamoto, A.; Walston, S.L.; Mitsuyama, Y.; Takita, H.; Asai, K.; Watanabe, T.; Abo, K.; Kimura, T.; et al. A deep learning-based model to estimate pulmonary function from chest x-rays: Multi-institutional model development and validation study in Japan. Lancet Digit. Health 2024, 6, e580–e588. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.; Atadjanov, I.; Seo, W.; Jo, M.; Park, J.; Ahn, J.; Kim, T.; Kim, H.; Shin, C.W. A Robust Method of Identifying the Optimal Cancellation Parameters for Dual-Energy Chest X-Ray Imaging. Phys. Med. Imaging 2022, 12031, 258–265. [Google Scholar] [CrossRef]
- Mok, T.C.W.; Chung, A.C.S. Large Deformation Diffeomorphic Image Registration with Laplacian Pyramid Networks. In Proceedings of the MICCAI 2020, Lima, Peru, 4–8 October 2020; Springer: Cham, Switzerland, 2020; pp. 211–221. [Google Scholar] [CrossRef]
- Song, J.; Jeong, J.-H.; Park, D.-S.; Kim, H.-H.; Seo, D.-C.; Ye, J.C. Unsupervised Denoising for Satellite Imagery Using Wavelet Directional CycleGAN. IEEE Trans. Geosci. Remote Sens. 2021, 59, 6823–6839. [Google Scholar] [CrossRef]
- Isola, P.; Zhu, J.Y.; Zhou, T.; Efros, A.A. Image-to-Image Translation with Conditional Adversarial Networks. In Proceedings of the 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July; pp. 5967–5976. [CrossRef]
- Eusemann, C.; Holmes, D.; Schmidt, B.; Flohr, T.; Robb, R.; McCollough, C.; Hough, D.; Huprich, J.; Wittmer, M.; Siddiki, H.; et al. Dual Energy CT: How to Best Blend both Energies in One Fused Image? In Proceedings of the SPIE 6918, Medical Imaging 2008: Visualization, Image-Guided Procedures, and Modeling, San Diego, CA, USA, 19–21 February 2008. [Google Scholar] [CrossRef]
- Ahn, S.Y.; Chae, K.J.; Goo, J.M. The Potential Role of Grid-Like Software in Bedside Chest Radiography in Improving Image Quality and Dose Reduction: An Observer Preference Study. Korean J. Radiol. 2018, 19, 526–533. [Google Scholar] [CrossRef]
- Chae, K.J.; Goo, J.M.; Ahn, S.Y.; Yoo, J.Y.; Yoon, S.H. Application of Deconvolution Algorithm of Point Spread Function in Improving Image Quality: An Observer Preference Study on Chest Radiography. Korean J. Radiol. 2018, 19, 147–152. [Google Scholar] [CrossRef]
- ICRP. Radiation and your patient: A guide for medical practitioners. In Proceedings of the Ann ICRP, The Hague, The Netherlands, 1 September 2001; Volume 31, pp. 5–31. [Google Scholar]
- European Commission; Directorate-General for Environment (European Commission). Guidance on Diagnostic Reference Levels (DRLs) for Medical Exposures; Publications Office: Luxembourg, 1999. [Google Scholar]
- Alomairy, N.; Hadi, D.; Al-Zaid, A.; Fasikh, R.; Arif, R.; Al-Hazmi, R.; Kharizy, A.; Alyami, A.; Hummdy, A.; Shubayr, N. Evaluation of the Entrance Surface Doses (ESD) for common diagnostic X-ray examinations. J. Radiat. Res. Appl. Sci. 2023, 16, 100754. [Google Scholar] [CrossRef]
- Urbaneja, A.; Dodin, G.; Hossu, G.; Bakour, O.; Kechidi, R.; Gondim Teixeira, P.; Blum, A. Added Value of Bone Subtraction in Dual-energy Digital Radiography in the Detection of Pneumothorax: Impact of Reader Expertise and Medical Specialty. Acad. Radiol. 2018, 25, 82–87. [Google Scholar] [CrossRef]
- Martini, K.; Baessler, M.; Baumueller, S.; Frauenfelder, T. Diagnostic accuracy and added value of dual-energy subtraction radiography compared to standard conventional radiography using computed tomography as standard of reference. PLoS ONE 2017, 12, e0174285. [Google Scholar] [CrossRef]
- Seah, J.C.Y.; Tang, C.H.M.; Buchlak, Q.D.; Holt, X.G.; Wardman, J.B.; Aimoldin, A.; Esmaili, N.; Ahmad, H.; Pham, H.; Lambert, J.F.; et al. Effect of a comprehensive deep-learning model on the accuracy of chest x-ray interpretation by radiologists: A retrospective, multireader multicase study. Lancet Digit. Health 2021, 3, e496–e506. [Google Scholar] [CrossRef]

| Anatomic Regions | 1 | 2 | 3 | 4 | 5 | Mean | 95% CI |
|---|---|---|---|---|---|---|---|
| Unobscured lung | 0 | 2 | 148 | 28 | 30 | 3.5 | [2.63; 4.47] |
| Hilum | 0 | 2 | 155 | 45 | 6 | 3.3 | [2.94; 3.58] |
| Minor fissure | 0 | 0 | 167 | 39 | 2 | 3.3 | [3.14; 3.40] * |
| Heart border | 0 | 3 | 124 | 65 | 16 | 3.4 | [2.91; 3.98] |
| Retrocardiac lung | 0 | 0 | 87 | 67 | 54 | 3.8 | [3.26; 4.42] * |
| Subdiaphragmatic lung | 0 | 0 | 111 | 44 | 53 | 3.7 | [2.96; 4.48] |
| Azygoesophageal recess | 0 | 7 | 79 | 73 | 49 | 3.8 | [3.11; 4.46] * |
| Proximal airway | 0 | 1 | 119 | 82 | 6 | 3.4 | [3.10; 3.78] * |
| Noise reduction (Soft-tissue) | 0 | 3 | 86 | 84 | 35 | 3.7 | [3.08; 4.37] * |
| Rib | 0 | 0 | 44 | 80 | 84 | 4.2 | [3.55; 4.84] * |
| Vertebral body and disc space | 0 | 0 | 30 | 95 | 83 | 4.3 | [3.70; 4.82] * |
| First costochondral joint | 0 | 0 | 106 | 79 | 23 | 3.6 | [3.07; 4.13] * |
| Clavicle | 0 | 0 | 65 | 71 | 72 | 4.4 | [4.09; 4.67] * |
| Scapula | 0 | 0 | 59 | 43 | 106 | 4.2 | [3.41; 5.04] * |
| Noise reduction (Bone) | 0 | 1 | 55 | 123 | 29 | 3.9 | [3.25; 4.48] * |
| Overall appearance | 0 | 3 | 76 | 83 | 46 | 3.8 | [3.20; 4.45] * |
| Anatomic Regions | 1 | 2 | 3 | 4 | 5 | Mean | 95% CI |
|---|---|---|---|---|---|---|---|
| Unobscured lung | 5 | 33 | 91 | 75 | 4 | 3.2 | [2.84; 3.56] |
| Hilum | 0 | 1 | 65 | 137 | 5 | 3.7 | [3.50; 3.91] * |
| Minor fissure | 0 | 14 | 181 | 13 | 0 | 3.0 | [2.86; 3.13] |
| Heart border | 0 | 18 | 76 | 99 | 15 | 3.5 | [3.03; 4.05] * |
| Retrocardiac lung | 7 | 76 | 99 | 26 | 0 | 2.7 | [2.21; 3.17] |
| Subdiaphragmatic lung | 9 | 69 | 111 | 19 | 0 | 2.7 | [2.25; 3.10] |
| Azygoesophageal recess | 10 | 78 | 102 | 18 | 0 | 2.6 | [2.32; 2.93] * |
| Proximal airway | 1 | 33 | 108 | 66 | 0 | 3.6 | [3.39; 3.88] * |
| Overall appearance | 7 | 51 | 77 | 73 | 0 | 3.3 | [3.00; 3.58] |
| Anatomic Regions | 1 | 2 | 3 | 4 | 5 | Mean | 95% CI |
|---|---|---|---|---|---|---|---|
| Rib | 0 | 2 | 22 | 97 | 87 | 4.3 | [3.87; 4.72] * |
| Vertebral body and disc space | 22 | 39 | 53 | 75 | 19 | 3.1 | [2.17; 4.12] |
| First costochondral joint | 0 | 2 | 56 | 98 | 52 | 4.0 | [3.40; 4.53] * |
| Clavicle | 0 | 0 | 23 | 105 | 80 | 4.3 | [3.77; 4.78] * |
| Scapula | 0 | 1 | 33 | 84 | 60 | 4.3 | [3.62; 4.92] * |
| Overall appearance | 0 | 4 | 38 | 116 | 50 | 4.0 | [3.47; 4.57] * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, S.-H.; Kim, J.; Kim, J.; Lee, J.-H.; Choi, I.; Shin, C.-W.; Park, C.-M. Improving Image Quality of Chest Radiography with Artificial Intelligence-Supported Dual-Energy X-Ray Imaging System: An Observer Preference Study in Healthy Volunteers. J. Clin. Med. 2025, 14, 2091. https://doi.org/10.3390/jcm14062091
Yoon S-H, Kim J, Kim J, Lee J-H, Choi I, Shin C-W, Park C-M. Improving Image Quality of Chest Radiography with Artificial Intelligence-Supported Dual-Energy X-Ray Imaging System: An Observer Preference Study in Healthy Volunteers. Journal of Clinical Medicine. 2025; 14(6):2091. https://doi.org/10.3390/jcm14062091
Chicago/Turabian StyleYoon, Sung-Hyun, Jihang Kim, Junghoon Kim, Jong-Hyuk Lee, Ilwoong Choi, Choul-Woo Shin, and Chang-Min Park. 2025. "Improving Image Quality of Chest Radiography with Artificial Intelligence-Supported Dual-Energy X-Ray Imaging System: An Observer Preference Study in Healthy Volunteers" Journal of Clinical Medicine 14, no. 6: 2091. https://doi.org/10.3390/jcm14062091
APA StyleYoon, S.-H., Kim, J., Kim, J., Lee, J.-H., Choi, I., Shin, C.-W., & Park, C.-M. (2025). Improving Image Quality of Chest Radiography with Artificial Intelligence-Supported Dual-Energy X-Ray Imaging System: An Observer Preference Study in Healthy Volunteers. Journal of Clinical Medicine, 14(6), 2091. https://doi.org/10.3390/jcm14062091






