The Distribution of Ocular Normative Parameters in a Spanish School Population
Abstract
1. Introduction
2. Materials and Methods
Measurement Procedure
- Axial length (AL);
- Corneal curvature (CR);
- Anterior chamber depth (ACD);
- Lens thickness (LT);
- Central corneal thickness (CCT);
- Posterior vitreous depth (PVD);
- Axial length/corneal curvature ratio (AL/CR).
3. Results
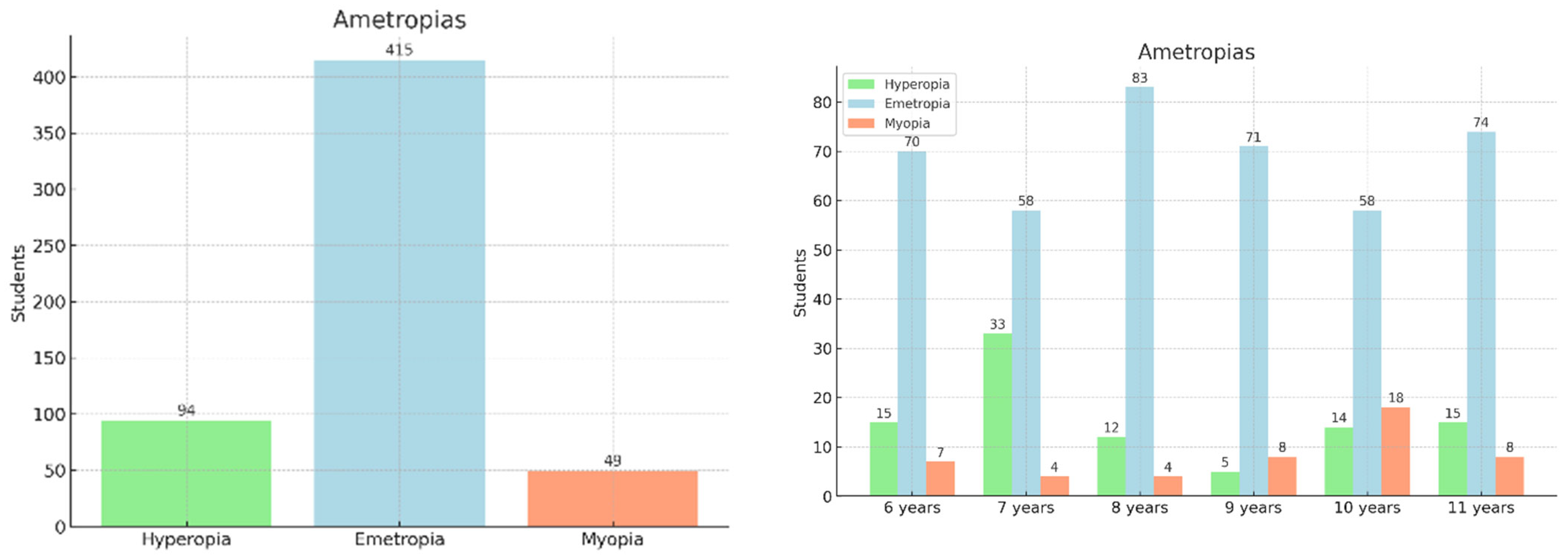
3.1. Demographic and Ocular Characteristics
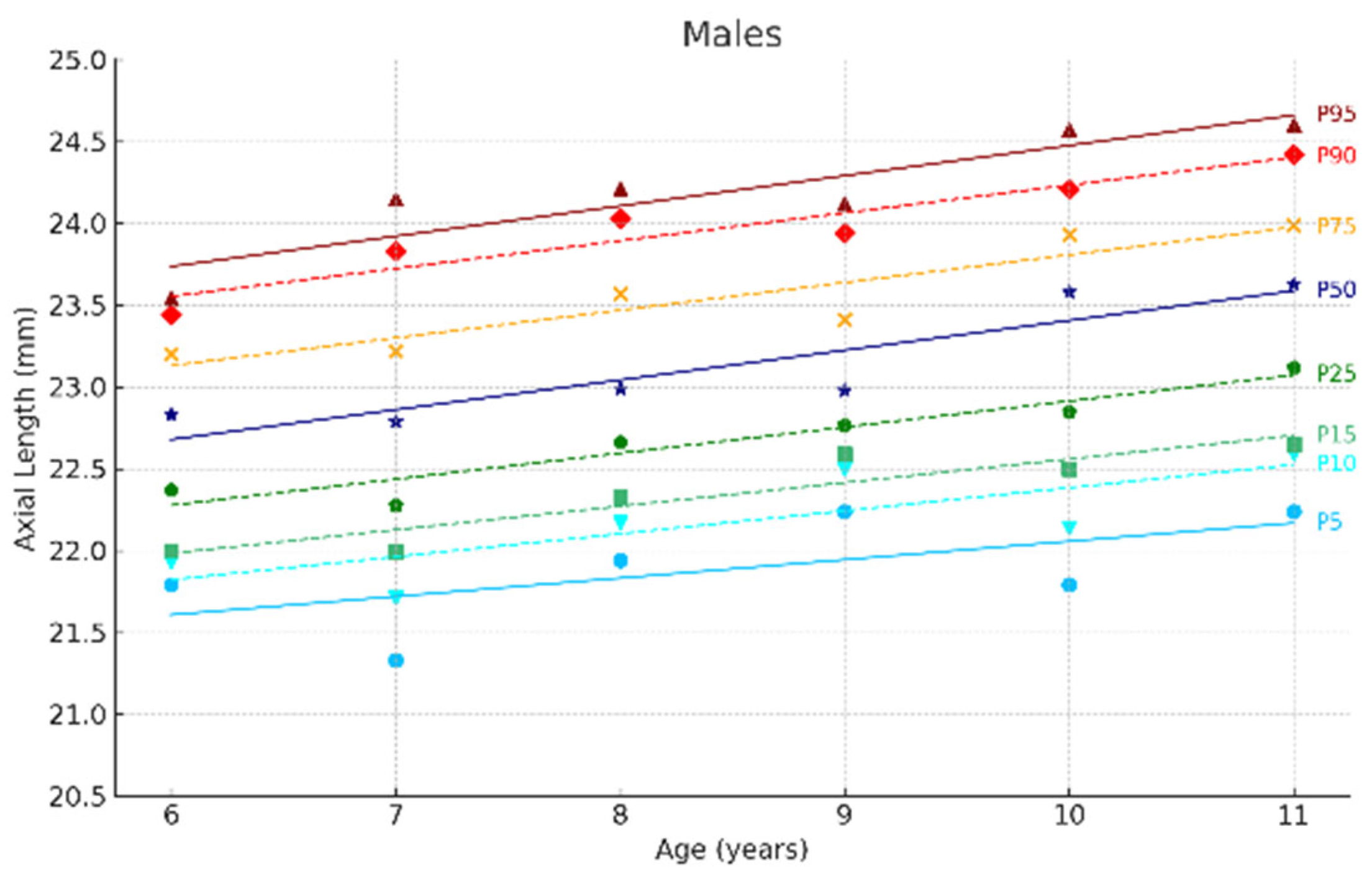
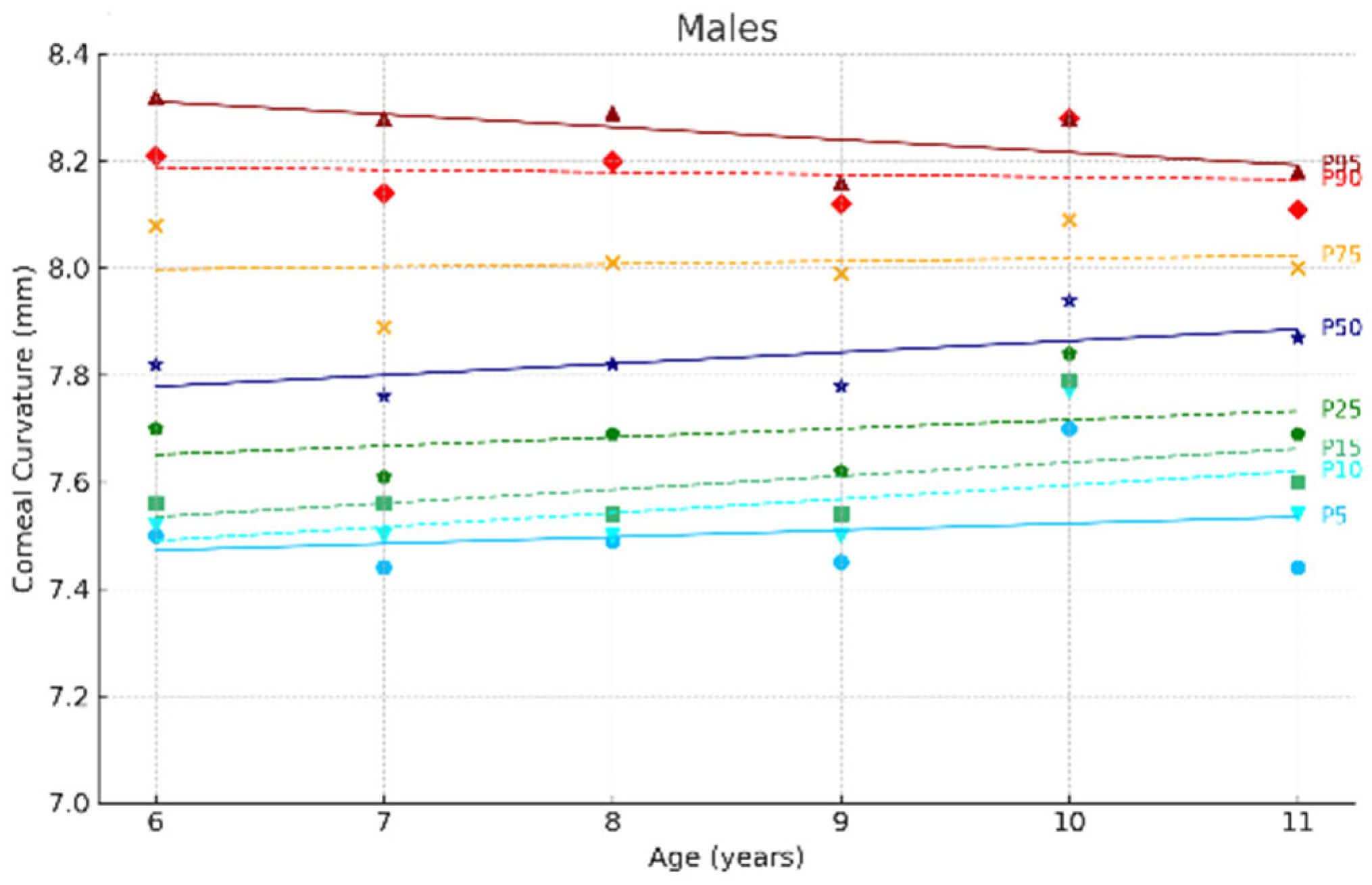
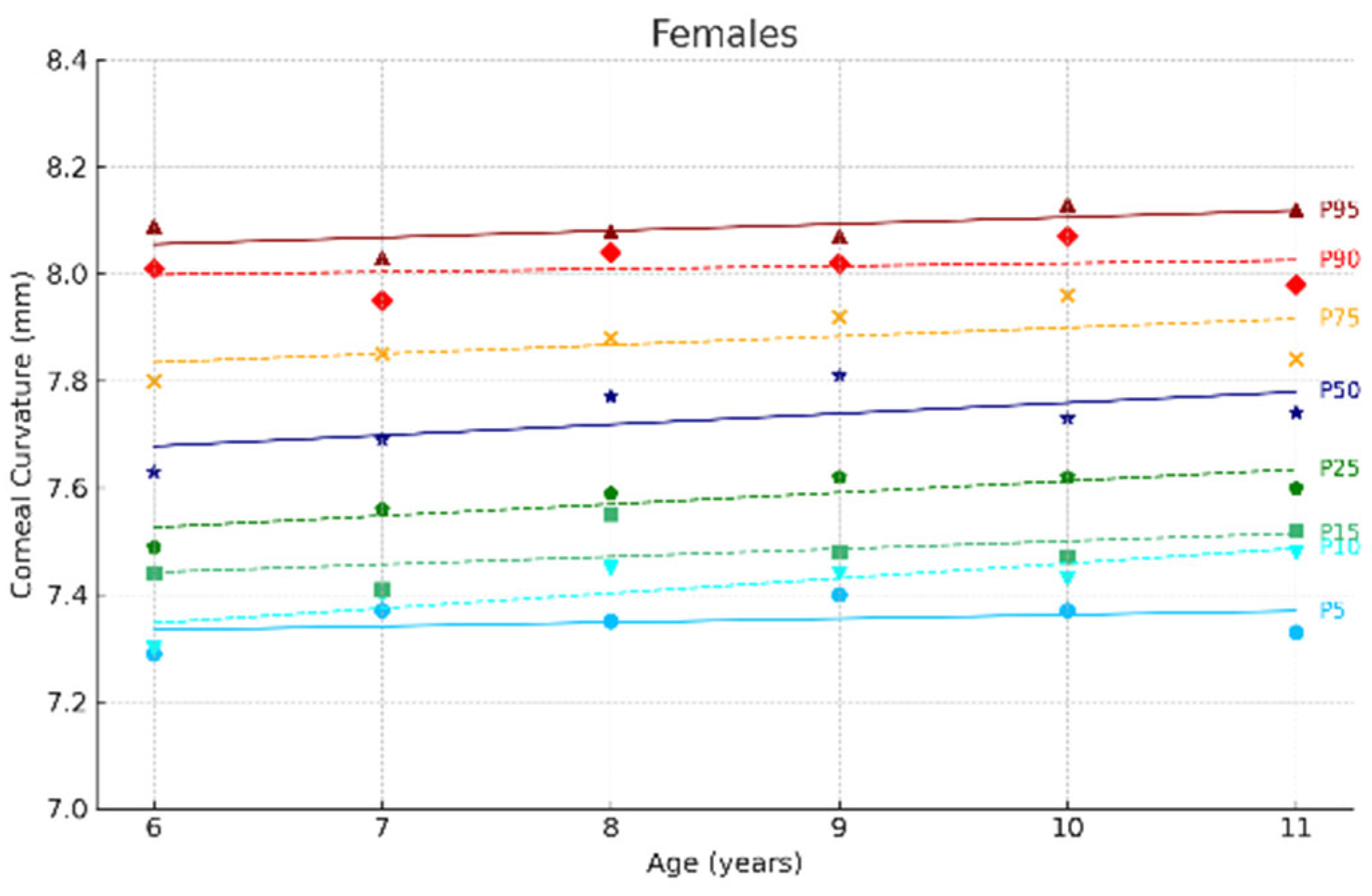
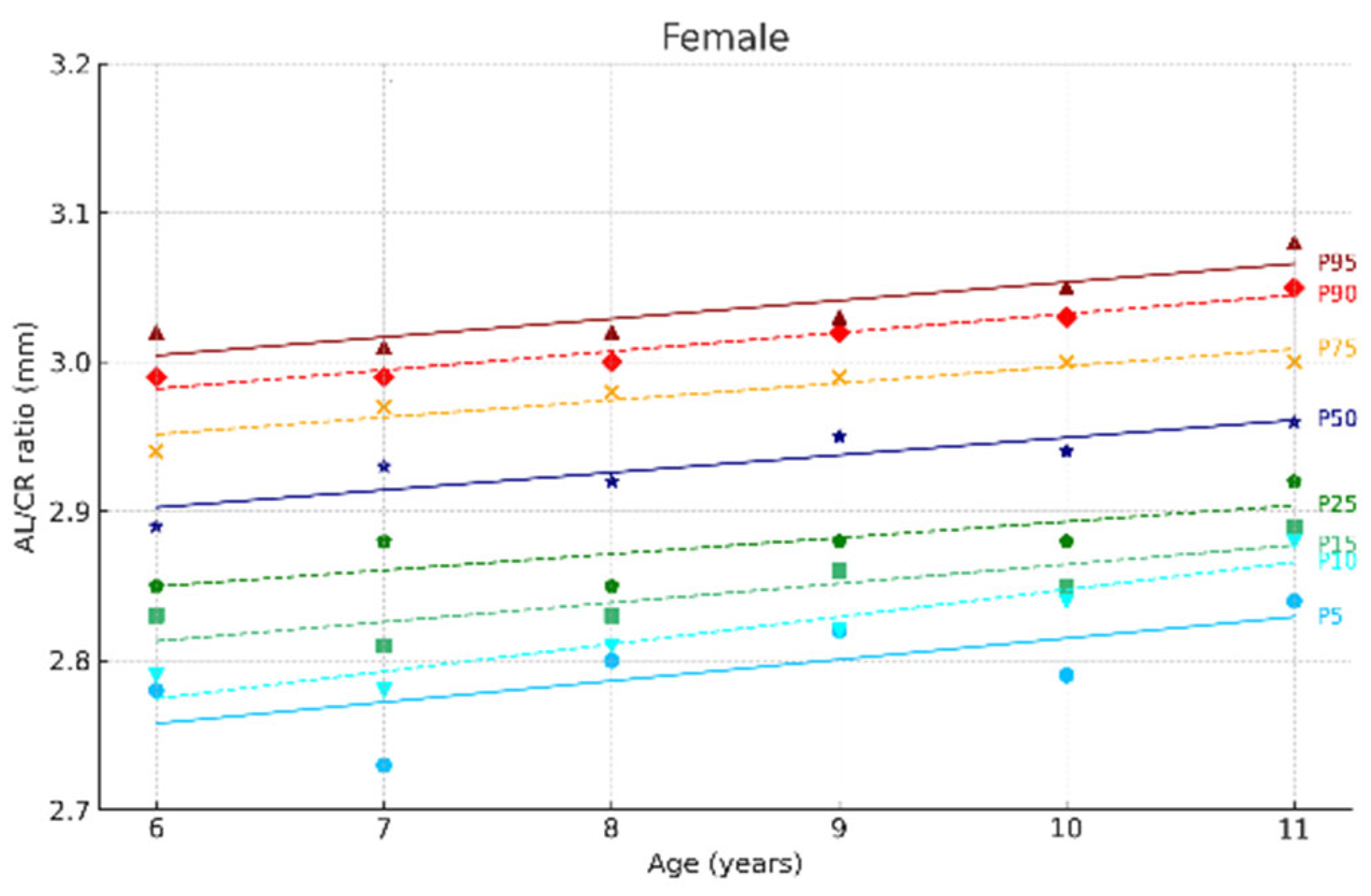
3.2. Growth Curves and Percentiles of Ocular Parameters
3.3. Correlations Between Ocular Parameters
3.4. Comparison of Spanish vs. European Parameters
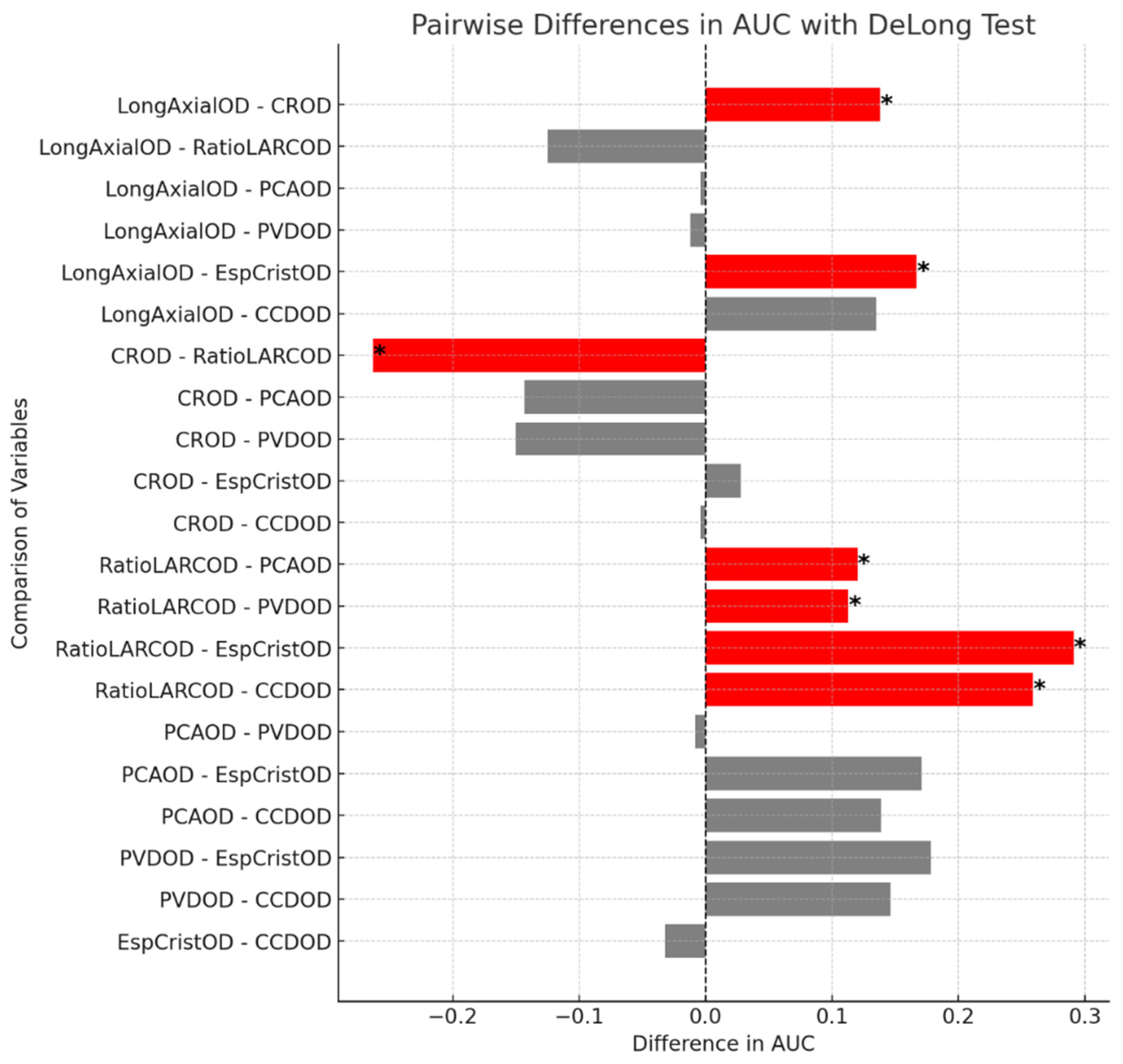
3.5. ROC Curve Analysis for Myopia Prediction Using Ocular Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AL | Axial length |
| CR | Corneal curvature |
| AL/CR | AL/CR ratio |
| ACD | Anterior chamber depth |
| PVD | Posterior vitreous depth |
| LT | Lens thickness |
| CCT | Central corneal thickness |
| SE | spherical equivalent |
References
- Alvarez-Peregrina, C.C.; Sanchez-Tena, M.A.M.A.; Martinez-Perez, C.C.; Villa-Collar, C.C. Prevalence and Risk Factors of Myopia in Spain. J. Ophthalmol. 2019, 2019, 3419576. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Peregrina, C.; Martinez-Perez, C.; Villa-Collar, C.; González-Pérez, M.; González-Abad, A.; Sánchez-Tena, M. The Prevalence of Myopia in Children in Spain: An Updated Study in 2020. Int. J. Environ. Res. Public Health 2021, 18, 12375. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Tena, M.; Martinez-Perez, C.; Villa-Collar, C.; González-Pérez, M.; González-Abad, A.; Afflelou, G.d.I.A.; Alvarez-Peregrina, C. Prevalence and Estimation of the Evolution of Myopia in Spanish Children. J. Clin. Med. 2024, 13, 1800. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Liang, J.; Pu, Y.; Chen, J.; Liu, M.; Ouyang, B.; Jin, Z.; Ge, W.; Wu, Z.; Yang, X.; Qin, C.; et al. Global prevalence, trend and projection of myopia in children and adolescents from 1990 to 2050: A comprehensive systematic review and meta-analysis. Br. J. Ophthalmol. 2024, 109, 362–371. [Google Scholar] [CrossRef]
- Fricke, T.R.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Naduvilath, T.J.; Ho, S.M.; Wong, T.Y.; Resnikoff, S. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: Systematic review, meta-analysis and modelling. Br. J. Ophthalmol. 2018, 102, 855–862. [Google Scholar] [CrossRef]
- Alvarez-Peregrina, C.; Martinez-Perez, C.; Sánchez-Tena, M. Myopia and Other Visual Disorders in Children. Int. J. Environ. Res. Public Health 2022, 19, 8912. [Google Scholar] [CrossRef]
- Yokoi, T.; Moriyama, M.; Hayashi, K.; Shimada, N.; Tomita, M.; Yamamoto, N.; Nishikawa, T.; Ohno-Matsui, K. Predictive factors for comorbid psychiatric disorders and their impact on vision-related quality of life in patients with high myopia. Int. Ophthalmol. 2014, 34, 171–183. [Google Scholar] [CrossRef]
- Rose, K.; Harper, R.; Tromans, C.; Waterman, C.; Goldberg, D.; Haggerty, C.; Tullo, A. Quality of life in myopia. Br. J. Ophthalmol. 2000, 84, 1031–1034. [Google Scholar] [CrossRef]
- Mutti, D.O.; Jordan, L.A.; Zadnik, K. Predicting the onset of myopia in children: Results from the CLEERE study. BMC Ophthalmol. 2021, 21, 279. [Google Scholar] [CrossRef]
- Mutti, D.O.; Sinnott, L.T.; Cotter, S.A.; Jones-Jordan, L.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.O.; Zadnik, K.O. Predicting the onset of myopia in children by age, sex, and ethnicity: Results from the CLEERE Study. Optom. Vis. Sci. 2024, 101, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Rozema, J.; Dankert, S.; Iribarren, R. Emmetropization and nonmyopic eye growth. Surv. Ophthalmol. 2023, 68, 759–783. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Jones, L.A.; Friedman, N.E.; Frane, S.L.; Lin, W.K.; Moeschberger, M.L.; Zadnik, K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Investig. Ophthalmol. Vis. Sci. 2005, 46, 3074–3080. [Google Scholar]
- Tideman, J.W.L.; Pärssinen, O.; Haarman, A.E.G.; Khawaja, A.P.; Wedenoja, J.; Williams, K.M.; Biino, G.; Ding, X.; Kähönen, M.; Lehtimäki, T.; et al. Evaluation of Shared Genetic Susceptibility to High and Low Myopia and Hyperopia. JAMA Ophthalmol. 2021, 139, 601–609. [Google Scholar]
- Morgan, I.G.; Wu, P.C.; Ostrin, L.A.; Tideman, J.W.L.; Yam, J.C.; Lan, W.; Baraas, R.C.; He, X.; Sankaridurg, P.; Saw, S.-M.; et al. IMI Risk Factors for Myopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 3. [Google Scholar]
- Mutti, D.O.; Hayes, J.R.; Mitchell, G.L.; Jones, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2510–2519. [Google Scholar]
- Tideman, J.W.L.; Polling, J.R.; Vingerling, J.R.; Jaddoe, V.W.V.; Williams, C.; Guggenheim, J.A.; Klaver, C.C.W. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018, 96, 301–309. [Google Scholar]
- Jones, L.A.; Mitchell, G.L.; Mutti, D.O.; Hayes, J.R.; Moeschberger, M.L.; Zadnik, K. Comparison of ocular component growth curves among refractive error groups in children. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2317–2327. [Google Scholar] [CrossRef] [PubMed]
- Jones-Jordan, L.A.; Sinnott, L.T.; Chu, R.H.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Twelker, J.D.; Zadnik, K. Myopia Progression as a Function of Sex, Age, and Ethnicity. Investig. Ophthalmol. Vis. Sci. 2021, 62, 36. [Google Scholar]
- Verkicharla, P.K.; Kammari, P.; Das, A.V. Myopia progression varies with age and severity of myopia. PLoS ONE 2020, 15, e0241759. [Google Scholar]
- Rozema, J.; Dankert, S.; Iribarren, R.; Lanca, C.; Saw, S.M. Axial Growth and Lens Power Loss at Myopia Onset in Singaporean Children. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3091–3099. [Google Scholar]
- Tapasztó, B.; Flitcroft, D.I.; Aclimandos, W.A.; Jonas, J.B.; De Faber, J.H.N.; Nagy, Z.Z.; Kestelyn, P.G.; Januleviciene, I.; Grzybowski, A.; Vidinova, C.N.; et al. Myopia management algorithm. Annexe to the article titled Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol. 2024, 34, 952–966. [Google Scholar] [PubMed]
- Vera-Diaz, F.A.; Jnawali, A.; Panorgias, A.; Bex, P.J.; Kerber, K.L. Baseline metrics that may predict future myopia in young children. Ophthalmic Physiol. Opt. 2023, 43, 466–481. [Google Scholar]
- Iribarren, R. Crystalline lens and refractive development. Prog. Retin. Eye Res. 2015, 47, 86–106. [Google Scholar] [PubMed]
- Rozema, J.J.; Sanchez, V.; Artal, N.; Gramajo, A.L.; Torres, E.; Luna, J.D.; Iribarren, R.; Tassignon, M.-J.; Juarez, C.P. Lens opacity based modelling of the age-related straylight increase. Vis. Res. 2015, 117, 25–33. [Google Scholar]
- Rozema, J.J.; Farzanfar, A. Refractive development II: Modelling normal and myopic eye growth. Ophthalmic Physiol. Opt. 2025, 45, 120–134. [Google Scholar]
- Zadnik, K.; Sinnott, L.T.; Cotter, S.A.; Jones-Jordan, L.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Mutti, D.O. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol. 2015, 133, 683–689. [Google Scholar]
- Jiang, X.M.; Lu, Y.Y.; Han, X.; Tan, Q.; Wu, J.S. Proportion and characteristic of emmetropia in schoolchildren aged 6–11y: The Shenzhen elementary school eye study. Int. J. Ophthalmol. 2020, 13, 1983–1989. [Google Scholar] [CrossRef]
- Grosvenor, T.; Goss, D.A. Role of the cornea in emmetropia and myopia. Optom. Vis. Sci. 1998, 75, 132–145. [Google Scholar]
- He, X.; Zou, H.; Lu, L.; Zhao, R.; Zhao, H.; Li, Q.; Zhu, J. Axial length/corneal radius ratio: Association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE 2015, 10, e0111766. [Google Scholar]
- Foo, V.H.; Verkicharla, P.K.; Ikram, M.K.; Chua, S.Y.; Cai, S.; Tan, C.S.; Chong, Y.S.; Kwek, K.; Gluckman, P.; Wong, T.Y.; et al. Axial Length/Corneal Radius of Curvature Ratio and Myopia in 3-Year-Old Children. Transl. Vis. Sci. Technol. 2016, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Scheiman, M.; Gwiazda, J.; Zhang, Q.; Deng, L.; Fern, K.; Manny, R.E.; Weissberg, E.; Hyman, L. Longitudinal changes in corneal curvature and its relationship to axial length in the Correction of Myopia Evaluation Trial (COMET) cohort. J. Optom. 2016, 9, 13–21. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Sankaridurg, P.; Xiong, S.; Li, W.; Naduvilath, T.; Lin, S.; Weng, R.; Lv, M.; Ma, Y.; Lu, L.; et al. Prevalence of myopia and high myopia, and the association with education: Shanghai Child and Adolescent Large-scale Eye Study (SCALE): A cross-sectional study. BMJ Open 2021, 11, e048450. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Deng, H.; Zhong, H.; Yu, Y.; Zhao, J.; Chen, S.; Li, S.; Zhu, M. A longitudinal study of the effect of ocular biometrics measures on myopia onset. Graefes Arch. Clin. Exp. Ophthalmol. 2021, 259, 999–1008. [Google Scholar] [CrossRef]



| Male | Female | p Value | |
|---|---|---|---|
| Median (IQR) Min–Max | Median (IQR) Min–Max | ||
| No. of eyes (n) | 259 | 299 | |
| Age (years) | 8.00 (7.00–10.00) (6.00, 12.00) | 9.00 (7.00–10.00) (6.00, 12.00) | |
| Axial length (mm) (AL) | 23.04 (22.60–23.64) (20.34, 25.59) | 22.59 (22.12–23.12) (19.64, 25.23) | p < 0.001 |
| Corneal curvature (mm) (CR) | 7.83 (7.68–8.02) (7.18, 8.79) | 7.74 (7.56–7.87) (7.00, 8.48) | p < 0.001 |
| AL/CR | 2.94 (2.90–3.00) (2.65, 3.25) | 2.93 (2.88–2.98) (2.63, 3.19) | p = 0.03 |
| Anterior chamber depth (mm) (ACD) | 3.59 (3.42–3.75) (2.90, 4.30) | 3.51 (3.31–3.65) (2.72, 4.07) | p < 0.001 |
| Posterior vitreous depth (mm) (PVD) | 3.04 (2.86–3.19) (2.31, 3.70) | 2.95 (2.77–3.10) (2.19, 3.57) | p < 0.001 |
| Crystalline lens thickness (mm) (LT) | 3.47 (3.33–3.60) (3.05, 4.05) | 3.52 (3.40–3.63) (3.01, 4.16) | p = 0.003 |
| Corneal thickness (mm) (CCT) | 0.56 (0.54–0.58) (0.47, 0.67) | 0.55 (0.53–0.57) (0.48, 0.64) | p < 0.001 |
| 6 Years | 7 Years | 8 Years | 9 Years | 10 Years | 11 Years | p Value | ||
|---|---|---|---|---|---|---|---|---|
| No. of eyes (n) | Male | 45 | 45 | 48 | 40 | 41 | 39 | |
| Female | 47 | 50 | 51 | 44 | 49 | 58 | ||
| Axial length (mm) (AL) | Male | 22.83 (22.36–23.22) (21.22, 24.19) | 22.79 (22.18–22.23) (20.34, 24.61) | 22.99 (22.66–23.58) (21.37, 25.34) | 22.98 (22.75–23.44) (20.77, 24.32) | 23.58 (22.83–23.94) (21.43, 25.41) | 23.63 (23.12–23.99) (21.76, 25.59) | p < 0.001 |
| Female | 22.05 (21.70–22.64) (20.32, 23.89) | 22.45 (22.06–22.97) (16.64, 23.60) | 22.45 (22.17–23.05) (20.70, 23.88) | 22.88 (22.27–23.35) (20.83, 24.73) | 22.78 (22.40–23.20) (21.26, 23.78) | 22.87 (22.46–23.28) (21.48, 25.23) | ||
| Corneal curvature (mm) (CR) | Male | 7.82 (7.69–8.09) (7.37, 8.63) | 7.76 (7.60–7.92) (7.18, 8.42) | 7.82 (7.68–8.01) (7.26, 8.48) | 7.78 (7.61–7.99) (7.41, 8.39) | 7.94 (7.83–8.09) (7.20, 8.79) | 7.87 (7.69–8.00) (7.33, 8.43) | p = 0.013 |
| Female | 7.63 (7.49–7.80) (7.00, 8.30) | 7.69 (7.54–7.85) (7.17, 8.13) | 7.77 (7.58–7.88 (7.09, 8.31) | 7.81 (7.30–7.92) (7.25, 8.48) | 7.73 (7.60–7.97) (7.17, 8.35) | 7.74 (7.59–7.84) (7.28, 8.33) | ||
| AL/CR | Male | 2.90 (2.85–2.94) (2.66, 3.06) | 2.93 (2.88–2.98) (2.68, 3.09) | 2.94 (2.90–2.99) (2.75, 3.16) | 2.97 (2.91–3.02) (2.69, 3.15) | 2.94 (2.89–3.00) (2.65, 3.11) | 3.00 (2.95–3.05) (2.87, 3.25) | p < 0.001 |
| Female | 2.89 (2.85–2.94) (2.73, 3.05) | 2.93 (2.88–2.97) (2.67, 3.08) | 2.92 (2.85–2.98) (2.64, 3.03) | 2.95 (2.88–2.99) (2.75, 3.06) | 2.94 (2.88–3.00) (2.70, 3.19) | 2.96 (2.92–3.00) (2.63, 3.14) | ||
| Anterior chamber depth (mm) (ACD) | Male | 3.51 (3.38–3.63) (3.01.3.95) | 3.55 (3.39–3.69) (2.94, 3.92) | 3.61 (3.42–3.74) (3.10, 4.23) | 3.56 (3.40–3.76) (3.11, 4.11) | 3.65 (3.40–3.85) (2.90, 4.11) | 3.78 (3.59–3.93) (3.18, 4.30) | p < 0.001 |
| Female | 3.38 (3.29–3.58) (2.94, 4.04) | 3.58 (3.28–3.73) (2.93, 4.06) | 3.48 (3.24–3.68) (2.72, 3.98) | 3.48 (3.38–3.67) (3.09, 4.07) | 3.53 (3.36–3.68) (2.92, 4.04) | 3.54 (3.37–3.65) (2.84, 4.02) | ||
| Posterior vitreous depth(mm) (PVD) | Male | 2.96 (2.81–3.06) (2.50, 3.38) | 3.01 (2.86–3.12) (2.38, 3.34) | 3.06 (2.86–3.19) (2.51, 3.65) | 2.98 (2.83–3.19) (2.60, 3.54) | 3.08 (2.84–3.26) (2.31, 3.53) | 3.20 (3.02–3.34) (2.57, 3.71) | p = 0.001 |
| Female | 2.83 (2.76–3.03) (2.36, 3.50) | 3.01 (2.72–3.17) (2.43, 3.55) | 2.90 (2.70–3.10) (2.19, 3.49) | 2.92 (2.81–3.07) (2.54, 3.57) | 2.97 (2.82–3.13) (2.37, 3.49) | 3.00 (2.84–3.11) (2.32, 3.47) | ||
| Crystalline lens thickness (mm) (LT) | Male | 3.60 (3.39–3.71) (3.15, 4.02) | 3.47 (3.35–3.59) (3.18, 4.05) | 3.47 (3.32–3.61) (3.12, 3.83) | 3.49 (3.37–3.59) (3.05, 3.86) | 3.46 (3.31–3.52) (3.15, 3.88) | 3.40 (3.29–3.51) (3.05, 3.96) | p < 0.001 |
| Female | 3.59 (3.49–3.67) (3.30, 4.04) | 3.55 (3.40–3.67) (3.15, 3.94) | 3.52 (3.39–3.68) (3.25, 4.16) | 3.47 (3.36–3.60) (3.14, 3.96) | 3.48 (3.40–3.55) (3.01, 3.96) | 3.50 (3.41–3.58) (3.06, 3.91) | ||
| Corneal thickness (mm) (CCT) | Male | 0.56 (0.54–0.58) (0.48, 0.63) | 0.55 (0.53–0.57) (0.47, 0.63) | 0.56 (0.54–0.58) (0.50, 0.67) | 0.56 (0.54–0.59) (0.49, 0.66) | 0.56 (0.52–0.58) (0.48, 0.63) | 0.56 (0.54–0.59) (0.48, 0.63) | p = 0.421 |
| Female | 0.55 (0.53–0.56) (0.50, 0.60) | 0.55 (0.52–0.57) (0.48, 0.59) | 0.55 (0.53–0.57) (0.48, 0.63) | 0.55 (0.52–0.57) (0.48, 00.64) | 0.55 (0.52–057) (0.48, 0.62) | 0.55 (0.53–0.56) (0.50, 0.62) |
| AL | CR | RAL/CR | ACD | PVD | LT | CCT | |
|---|---|---|---|---|---|---|---|
| AL | 1 | 0.642 ** | 0.443 ** | 0.483** | 0.471** | −0.373 ** | 0.150 ** |
| CR | 0.642 ** | 1 | −0.331 ** | 0.003 | −0.017 | 0.023 | 0.168 ** |
| AL/CR | 0.443 ** | −0.331 ** | 1 | 0.647 ** | 0.653 ** | −0.531 ** | −0.002 |
| ACD | 0.483 ** | 0.003 | 0.647 ** | 1 | 0.992 ** | −0.475 ** | 0.104 * |
| PVD | 0.471 ** | −0.017 | 0.653 ** | 0.992 ** | 1 | −0.480 ** | −0.008 |
| LT | −0.373 ** | 0.023 | −0.531 ** | −0.475 ** | −0.480 ** | 1 | 0.001 |
| CCT RE | 0.150 ** | 0.168 ** | −0.002 | 0.104 * | −0.008 | 0.001 | 1 |
| Valid N | Median | 95.0% Lower CI for Median | 95.0% Upper CI for Median | Tideman, 2018 [17] | Statistical Significance | ||||
|---|---|---|---|---|---|---|---|---|---|
| AL | Age | 6 | Female | 47 | 22.05 | 21.9 | 22.34 | 22.06 | NO |
| Male | 45 | 22.83 | 22.56 | 23.02 | 22.59 | NO | |||
| 9 | Female | 44 | 22.88 | 22.58 | 23.17 | 22.79 | NO | ||
| Male | 40 | 22.98 | 22.85 | 23.21 | 23.31 | SI | |||
| CR | Age | 6 | Female | 47 | 7.63 | 7.55 | 7.75 | 7.7 | NO |
| Male | 45 | 7.82 | 7.77 | 7.94 | 7.84 | NO | |||
| 9 | Female | 44 | 7.81 | 7.77 | 7.89 | 7.72 | SI | ||
| Male | 40 | 7.78 | 7.72 | 7.91 | 7.84 | NO | |||
| LA/RC | Age | 6 | Female | 47 | 2.89 | 2.87 | 2.92 | 2.87 | NO |
| Male | 45 | 2.9 | 2.87 | 2.92 | 2.89 | NO | |||
| 9 | Female | 44 | 2.95 | 2.9 | 2.97 | 2.95 | NO | ||
| Male | 40 | 2.97 | 2.94 | 3 | 2.97 | NO | |||
| Area Under the ROC Curve | |||||
|---|---|---|---|---|---|
| Test Result Variable(s) | Area | Std. Error a | Asymptotic Sig. b | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||
| AL | 0.555 | 0.052 | 0.294 | 0.453 | 0.656 |
| CR | 0.416 | 0.059 | 0.155 | 0.301 | 0.532 |
| LA/CR | 0.679 | 0.052 | 0.001 | 0.576 | 0.782 |
| ACD | 0.559 | 0.055 | 0.286 | 0.451 | 0.666 |
| PVD | 0.566 | 0.056 | 0.235 | 0.457 | 0.675 |
| LT | 0.388 | 0.053 | 0.035 | 0.284 | 0.492 |
| CCT | 0.42 | 0.059 | 0.178 | 0.304 | 0.536 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Jiménez, R.; Povedano-Montero, F.J.; Bernárdez-Vilaboa, R.; Gomez-de-Liano, R.; Guemes-Villahoz, N.; Cedrún-Sánchez, J.E. The Distribution of Ocular Normative Parameters in a Spanish School Population. J. Clin. Med. 2025, 14, 2507. https://doi.org/10.3390/jcm14072507
González-Jiménez R, Povedano-Montero FJ, Bernárdez-Vilaboa R, Gomez-de-Liano R, Guemes-Villahoz N, Cedrún-Sánchez JE. The Distribution of Ocular Normative Parameters in a Spanish School Population. Journal of Clinical Medicine. 2025; 14(7):2507. https://doi.org/10.3390/jcm14072507
Chicago/Turabian StyleGonzález-Jiménez, Rut, F. Javier Povedano-Montero, Ricardo Bernárdez-Vilaboa, Rosario Gomez-de-Liano, Noemí Guemes-Villahoz, and Juan E. Cedrún-Sánchez. 2025. "The Distribution of Ocular Normative Parameters in a Spanish School Population" Journal of Clinical Medicine 14, no. 7: 2507. https://doi.org/10.3390/jcm14072507
APA StyleGonzález-Jiménez, R., Povedano-Montero, F. J., Bernárdez-Vilaboa, R., Gomez-de-Liano, R., Guemes-Villahoz, N., & Cedrún-Sánchez, J. E. (2025). The Distribution of Ocular Normative Parameters in a Spanish School Population. Journal of Clinical Medicine, 14(7), 2507. https://doi.org/10.3390/jcm14072507









