A Western-Style Diet Influences Ingestive Behavior and Glycemic Control in a Rat Model of Roux-en-Y Gastric Bypass Surgery
Abstract
1. Introduction
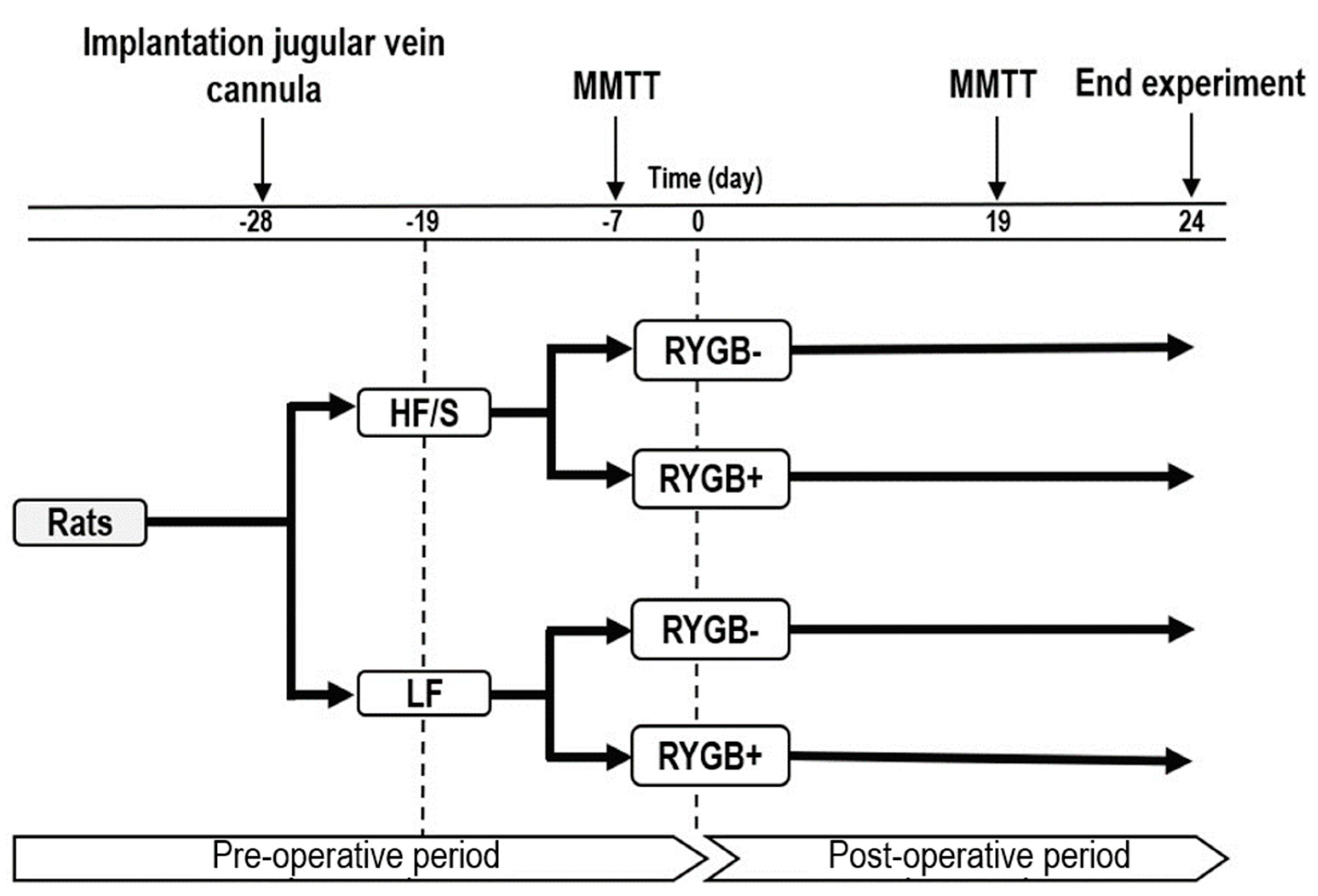
2. Materials and Methods
2.1. Animals
2.2. Jugular Vein Cannulation
2.3. Diet
2.4. Meal Pattern Analysis
2.5. Roux-en-Y Gastric Bypass Surgery
2.6. Mixed Meal Tolerance Test
2.7. Glucose Homeostasis Calculations
2.8. Termination
2.9. Data Analysis
3. Results
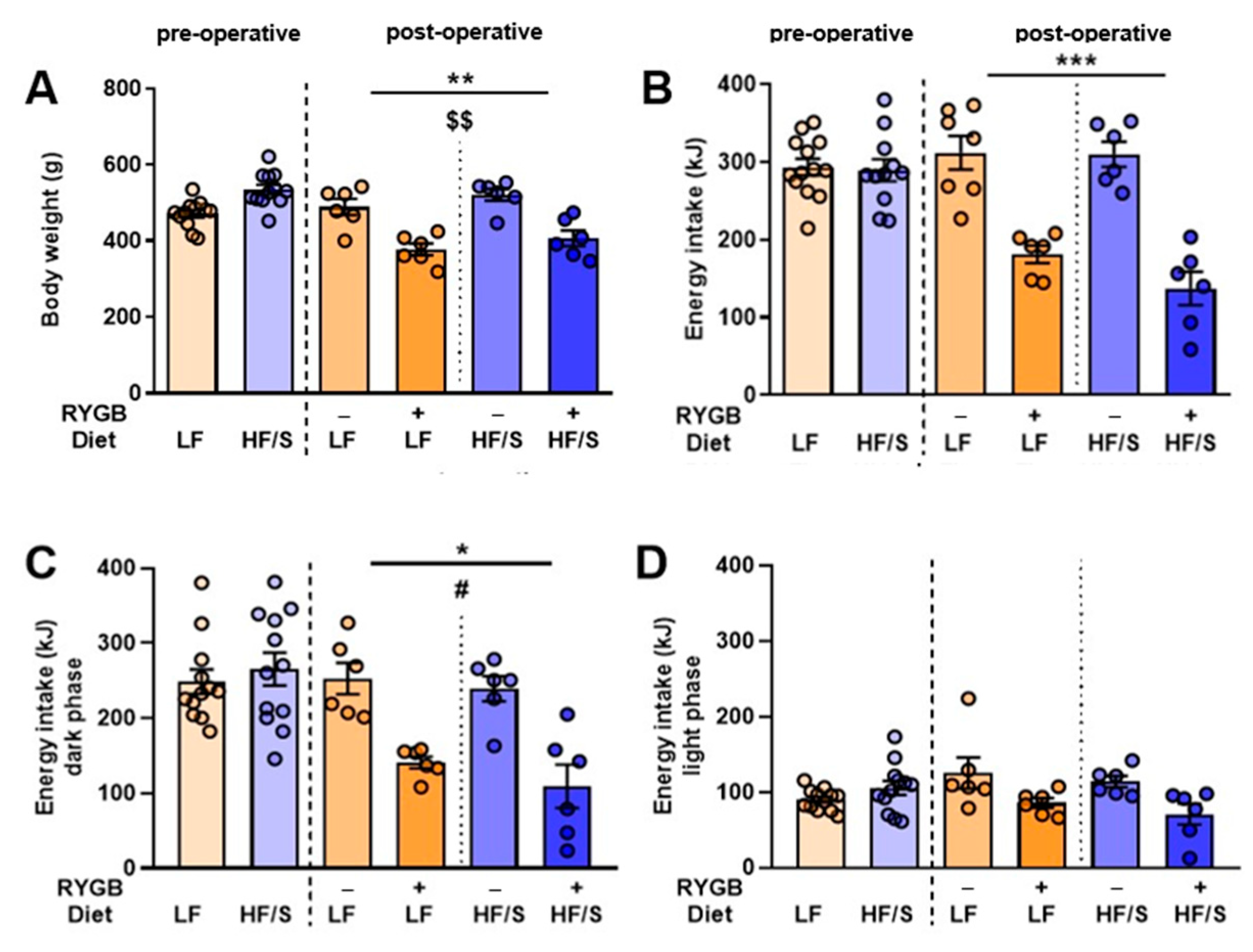
3.1. Body Weight and Energy Intake
3.1.1. Body Weight
3.1.2. Energy Intake
3.2. Meal Patterns
3.3. Glucose Homeostasis Parameters
3.3.1. Baseline Fasted State
3.3.2. Post-Prandial State
3.4. Influence of Meal Pattern Parameters on Glucose Homeostasis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUC | area under the curve |
| BMI | body mass index |
| GLP-1 | glucagon-like peptide-1 |
| HF/S | high fat with added sucrose |
| LF | low fat |
| MCA | meal cluster analysis |
| MMTT | mixed meal tolerance test |
| RYGB | Roux-en-Y gastric bypass |
| T2DM | type 2 diabetes mellitus |
References
- Salehi, M.; D’Alessio, D.A. Mechanisms of surgical control of type 2 diabetes: GLP-1 is the key factor—Maybe. Surg. Obes. Relat. Dis. 2016, 12, 1230–1235. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Promintzer-schifferl, M.; Prager, G.; Anderwald, C.; Mandl, M.; Esterbauer, H.; Shakeri-leidenmühler, S.; Pacini, G.; Stadler, M.; Bischof, M.G.; Ludvik, B.; et al. Effects of Gastric Bypass Surgery on Insulin Resistance and Insulin Secretion in Nondiabetic Obese Patients. Obesity 2011, 19, 1420–1426. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Chen, L.; Yu, C.; Piao, D.; Wang, Y.; Han, P. Roux-en-Y gastric bypass increases hepatic and peripheral insulin sensitivity in rats with type 2 diabetes mellitus. Surg. Obes. Relat. Dis. 2014, 10, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Sjöström, L.; Narbro, K.; Sjöström, C.D.; Karason, K.; Larsson, B.; Wedel, H.; Lystig, T.; Sullivan, M.; Bouchard, C.; Carlsson, B.; et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 2007, 357, 741–752. [Google Scholar] [CrossRef]
- DePaula, A.L.; Macedo, A.L.V.; Rassi, N.; Machado, C.A.; Schraibman, V.; Silva, L.Q.; Halpern, A. Laparoscopic treatment of type 2 diabetes mellitus for patients with a body mass index less than 35. Surg. Endosc. Other Interv. Tech. 2008, 22, 706–716. [Google Scholar] [CrossRef]
- Bojsen-Møller, K.N. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Dan. Med. J. 2015, 62, B5057. [Google Scholar]
- Madsbad, S.; Dirksen, C.; Holst, J.J. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol. 2014, 2, 152–164. [Google Scholar] [CrossRef]
- Murphy, K.G.; Bloom, S.R. Gut hormones and the regulation of energy homeostasis. Nature 2006, 444, 854–859. [Google Scholar] [CrossRef]
- Berthoud, H.; Shin, A.C.; Zheng, H. Obesity surgery and gut—Brain communication. Physiol. Behav. 2011, 105, 106–119. [Google Scholar] [CrossRef]
- Halmi, K.A.; Mason, E.; Falk, J.R.; Stunkard, A. Appetitive behavior after gastric bypass for obesity. Int. J. Obes. 1981, 5, 457–464. [Google Scholar]
- Zakeri, R.; Batterham, R.L. Potential mechanisms underlying the effect of bariatric surgery on eating behaviour. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 3–11. [Google Scholar] [CrossRef]
- Xu, Y.; Ohinata, K.; Meguid, M.; Marx, W.; Tada, T.; Chen, C.; Quinn, R.; Inui, A. Gastric Bypass Model in the Obese Rat to Study Metabolic Mechanisms of Weight Loss. J. Surg. Res. 2002, 107, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Furnes, M.W.; Stenström, B.; Tømmerås, K.; Skoglund, T.; Dickson, S.L.; Kulseng, B.; Zhao, C.-M.; Chen, D. Feeding Behavior in Rats Subjected to Gastrectomy or Gastric Bypass Surgery. Eur. Surg. Res. 2008, 40, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Evers, S.S.; Boersma, G.J.; Tamashiro, K.L.K.; Scheurink, A.J.W.; van Dijk, G. Roman high and low avoidance rats differ in their response to chronic olanzapine treatment at the level of body weight regulation, glucose homeostasis, and cortico-mesolimbic gene expression. J. Psychopharmacol. 2017, 31, 1437–1452. [Google Scholar] [CrossRef]
- Hoornenborg, C.W.; Somogyi, E.; Bruggink, J.E.; Boyle, C.N.; Lutz, T.A.; Emous, M.; van Beek, A.P.; Nyakas, C.; van Dijk, G. Weight loss in adult male Wistar rats by Roux-en-Y gastric bypass is primarily explained by caloric intake reduction and pre-surgery body weight. Am. J. Physiol. Integr. Comp. Physiol. 2024, 326, R507–R514. [Google Scholar] [CrossRef]
- Karapetsas, G. Effects of Laboratory Housing Conditions on NEUROBIOlogy of Energy Balance in Mice; University of Groningen: Groningen, The Netherlands, 2021. [Google Scholar]
- Vito R Muggeo, M.M. Segmented: An R package to fit regression models with broken-line relationships. R News 2022, 8, 20–25. [Google Scholar]
- Cortez, M.Y.; Torgan, C.E.; Brozinick, J.T., Jr.; Ivy, J.L. Insulin resistance of obese Zucker rats exercise trained at two different intensities. Am. J. Physiol. 1991, 261, 613–619. [Google Scholar] [CrossRef]
- Maki, K.C.; Kelley, K.M.; Lawless, A.L.; Hubacher, R.L.; Schild, A.L.; Dicklin, M.R.; Rains, T.M. Validation of Insulin Sensitivity and Secretion Indices Derived from the Liquid Meal Tolerance Test. Diabetes Technol. Ther. 2011, 13, 661–666. [Google Scholar] [CrossRef]
- Steinert, R.E.; Feinle-Bisset, C.; Asarian, L.; Horowitz, M.; Beglinger, C.; Geary, N. Ghrelin, CCK, GLP-1, and PYY(3–36): Secretory Controls and Physiological Roles in Eating and Glycemia in Health, Obesity, and After RYGB. Physiol. Rev. 2017, 97, 411–463. [Google Scholar] [CrossRef]
- Fosset, S.; Fromentin, G.; Rampin, O.; Lang, V.; Mathieu, F.; Tomé, D. Pharmacokinetics and feeding responses to muramyl dipeptide in rats. Physiol. Behav. 2003, 79, 173–182. [Google Scholar] [CrossRef]
- Zheng, H.; Shin, A.C.; Lenard, N.R.; Townsend, R.L.; Patterson, L.M.; Sigalet, D.L.; Berthoud, H. Meal patterns, satiety, and food choice in a rat model of Roux-en-Y gastric bypass surgery. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 297, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Gero, D.; Steinert, R.E.; Hosa, H.; Cummings, D.E.; Bueter, M. Appetite, glycemia, and entero-insular hormone responses differ between oral, gastric-remnant, and duodenal administration of a mixed-meal test after roux-en-y gastric bypass. Diabetes Care 2018, 41, 1295–1297. [Google Scholar] [CrossRef] [PubMed]
- Laurenius, A.; Larsson, I.; Bueter, M.; Melanson, K.J.; Bosaeus, I.; Forslund, H.B.; Lönroth, H.; Fändriks, L.; Olbers, T. Changes in eating behaviour and meal pattern following Roux-en-Y gastric bypass. Int. J. Obes. 2012, 36, 348–355. [Google Scholar] [CrossRef]
- Shin, H.S.; Ingram, J.R.; McGill, A.T.; Poppitt, S.D. Lipids, CHOs, proteins: Can all macronutrients put a ‘brake’ on eating? Physiol. Behav. 2013, 120, 114–123. [Google Scholar] [CrossRef]
- Grayson, B.E.; Hakala-Finch, A.P.; Kekulawala, M.; Laub, H.; Egan, A.E.; Ressler, I.B.; Woods, S.C.; Herman, J.P.; Seeley, R.J.; Benoit, S.C.; et al. Weight loss by calorie restriction versus bariatric surgery differentially regulates the HPA axis in male rats. Stress 2014, 17, 484–493. [Google Scholar] [CrossRef]
- Seyfried, F.; Miras, A.D.; Bueter, M.; Prechtl, C.G.; Spector, A.C.; Roux, C.W. Le Effects of preoperative exposure to a high-fat versus a low-fat diet on ingestive behavior after gastric bypass surgery in rats. Surg. Endosc. 2013, 27, 4192. [Google Scholar] [CrossRef]
- le Roux, C.W.; Bueter, M.; Theis, N.; Werling, M.; Ashrafian, H.; Löwenstein, C.; Athanasiou, T.; Bloom, S.R.; Spector, A.C.; Olbers, T.; et al. Gastric bypass reduces fat intake and preference. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011, 301, R1057–R1066. [Google Scholar] [CrossRef]
- Mathes, C.M.; Letourneau, C.; Blonde, G.D.; Roux, C.W.L.; Spector, A.C. Roux-en-y gastric bypass in rats progressively decreases the proportion of fat calories selected from a palatable cafeteria diet. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 310, R952–R959. [Google Scholar] [CrossRef]
- Mahawar, K.K.; Sharples, A.J. Contribution of Malabsorption to Weight Loss After Roux-en-Y Gastric Bypass: A Systematic Review. Obes. Surg. 2017, 27, 2194–2206. [Google Scholar] [CrossRef]
- Lutz, T.A.; Bueter, M. The physiology underlying Roux-en-Y gastric bypass: A status report. AJP Regul. Integr. Comp. Physiol. 2014, 307, R1275–R1291. [Google Scholar] [CrossRef]
- White, M.A.; Kalarchian, M.A.; Masheb, R.M.; Marcus, M.D.; Grilo, C.M. Loss of control over eating predicts outcomes in bariatric surgery patients: A prospective, 24-month follow-up study. J. Clin. Psychiatry 2010, 71, 175–184. [Google Scholar] [CrossRef] [PubMed]
- van Beek, A.P.; Emous, M.; Laville, M.; Tack, J. Dumping syndrome after esophageal, gastric or bariatric surgery: Pathophysiology, diagnosis, and management. Obes. Rev. 2017, 18, 68–85. [Google Scholar] [CrossRef] [PubMed]
- Benoit, B.; Plaisancié, P.; Awada, M.; Géloën, A.; Estienne, M.; Capel, F.; Malpuech-Brugère, C.; Debard, C.; Pesenti, S.; Morio, B.; et al. High-fat diet action on adiposity, inflammation, and insulin sensitivity depends on the control low-fat diet. Nutr. Res. 2013, 33, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, I.; Sundbom, M.; Abrahamsson, N.; Haenni, A. Comparison of Meal Pattern and Postprandial Glucose Response in Duodenal Switch and Gastric Bypass Patients. Obes. Surg. 2019, 29, 2210–2216. [Google Scholar] [CrossRef]
- Hao, Z.; Zhao, Z.; Berthoud, H.R.; Ye, J. Development and Verification of a Mouse Model for Roux-en-Y Gastric Bypass Surgery with a Small Gastric Pouch. PLoS ONE 2013, 8, e52922. [Google Scholar] [CrossRef]
- Jørgensen, N.B.; Jacobsen, S.H.; Dirksen, C.; Bojsen-Møller, K.N.; Naver, L.; Hvolris, L.; Clausen, T.R.; Wulff, B.S.; Worm, D.; Lindqvist Hansen, D.; et al. Acute and long-term effects of Roux-en-Y gastric bypass on glucose metabolism in subjects with Type 2 diabetes and normal glucose tolerance. Am. J. Physiol. Endocrinol. Metab. 2012, 303, 122–131. [Google Scholar] [CrossRef]
- Martinussen, C.; Bojsen-Møller, K.N.; Dirksen, C.; Jacobsen, S.H.; Jørgensen, N.B.; Kristiansen, V.B.; Holst, J.J.; Madsbad, S. Immediate enhancement of first-phase insulin secretion and unchanged glucose effectiveness in patients with type 2 diabetes after Roux-en-Y gastric bypass. Am. J. Physiol. Endocrinol. Metab. 2015, 308, E535–E544. [Google Scholar] [CrossRef]
- Pezeshki, A.; Chelikani, P.K. Effects of Roux-en-Y gastric bypass and ileal transposition surgeries on glucose and lipid metabolism in skeletal muscle and liver. Surg. Obes. Relat. Dis. 2014, 10, 217–228. [Google Scholar] [CrossRef]
- Svane, M.S.; Jørgensen, N.B.; Bojsen-Møller, K.N.; Dirksen, C.; Nielsen, S.; Kristiansen, V.B.; Toräng, S.; Wewer Albrechtsen, N.J.; Rehfeld, J.F.; Hartmann, B.; et al. Peptide YY and glucagon-like peptide-1 contribute to decreased food intake after Roux-en-Y gastric bypass surgery. Int. J. Obes. 2016, 40, 1699–1706. [Google Scholar] [CrossRef]
- Liou, A.P.; Paziuk, M.; Luevano, J.M.; Machineni, S.; Turnbaugh, P.J.; Kaplan, L.M. Conserved Shifts in the Gut Microbiota Due to Gastric Bypass Reduce Host Weight and Adiposity. Sci. Transl. Med. 2013, 5, 178ra41. [Google Scholar] [CrossRef]


| Fasting glucose homeostasis parameters | ||
| 1. | HOMA-IR | |
| 2. | HOMA-B | |
| Post-prandial glucose homeostasis parameters | ||
| 3. | AUCins, AUCgluc | |
| 4. | Beta-cell sensitivity | |
| 5. | Insulinogenic index | |
| LF RYGB− | LF RYGB+ | HF/S RYGB− | HF/S RYGB+ | Main Effect | |
|---|---|---|---|---|---|
| Fasting glucose homeostasis parameters | |||||
| Glucose mM | 5.80 ± 0.32 | 5.26 ± 0.20 | 6.70 ± 0.16 | 4.84 ± 0.18 | S, D |
| Insulin (ng/mL) | 2.06 ± 0.34 | 0.77 ± 0.14 | 1.76 ± 0.09 | 0.74 ± 0.19 | S |
| HOMA-IR | 0.543 ± 0.119 | 0.165 ± 0.028 | 0.527 ± 0.038 | 0.171 ± 0.050 | S |
| HOMA-B | 0.99 ± 0.05 | 0.69 ± 0.13 | 0.42 ± 0.13 | 0.60 ± 0.16 | D |
| Post-prandial glucose homeostasis parameters | |||||
| AUCgluc | 29.9 ± 7.5 | 70.2 ± 8.7 | 139.9 ± 19.2 | 108.7 ± 31.0 | D, S, D × S |
| AUCins | 94.6 ± 40.8 | 67.1 ± 23.9 | 189.8 ± 11.4 | 109.5 ± 26.5 | D, s = 0.058 |
| AUCins/AUCgluc | 2.9 ± 0.7 | 0.9 ± 0.3 | 1.5 ± 0.2 | 1.2 ± 0.2 | S, d × s |
| Insulinogenic index 0–5 min | 2.89 ± 2.82 | 1.22 ± 0.32 | 4.47 ± 1.44 | 0.52 ± 0.23 | |
| Insulinogenic index 0–10 min | 7.88 ± 0.86 | 1.43 ± 0.34 | 2.43 ± 0.66 | 1.79 ± 0.56 | D, S, D × S |
| Insulinogenic index 0–15 min | 4.00 ± 1.09 | 1.46 ± 0.27 | 1.79 ± 0.14 | 1.42 ± 0.40 | S |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoornenborg, C.W.; Somogyi, E.; Bruggink, J.E.; Boyle, C.N.; Lutz, T.A.; Emous, M.; van Beek, A.P.; van Dijk, G. A Western-Style Diet Influences Ingestive Behavior and Glycemic Control in a Rat Model of Roux-en-Y Gastric Bypass Surgery. J. Clin. Med. 2025, 14, 2642. https://doi.org/10.3390/jcm14082642
Hoornenborg CW, Somogyi E, Bruggink JE, Boyle CN, Lutz TA, Emous M, van Beek AP, van Dijk G. A Western-Style Diet Influences Ingestive Behavior and Glycemic Control in a Rat Model of Roux-en-Y Gastric Bypass Surgery. Journal of Clinical Medicine. 2025; 14(8):2642. https://doi.org/10.3390/jcm14082642
Chicago/Turabian StyleHoornenborg, C. Warner, Edit Somogyi, Jan E. Bruggink, Christina N. Boyle, Thomas A. Lutz, Marloes Emous, André P. van Beek, and Gertjan van Dijk. 2025. "A Western-Style Diet Influences Ingestive Behavior and Glycemic Control in a Rat Model of Roux-en-Y Gastric Bypass Surgery" Journal of Clinical Medicine 14, no. 8: 2642. https://doi.org/10.3390/jcm14082642
APA StyleHoornenborg, C. W., Somogyi, E., Bruggink, J. E., Boyle, C. N., Lutz, T. A., Emous, M., van Beek, A. P., & van Dijk, G. (2025). A Western-Style Diet Influences Ingestive Behavior and Glycemic Control in a Rat Model of Roux-en-Y Gastric Bypass Surgery. Journal of Clinical Medicine, 14(8), 2642. https://doi.org/10.3390/jcm14082642






