Impact of Rehabilitation on Outcomes after TAVI: A Preliminary Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Data Source and Study Population
2.2. Data Recorded
2.3. Follow-up
2.4. Rehabilitation
2.5. Geriatric Rehabilitation
2.6. Cardiac Rehabilitation
2.7. Statistical Analyses
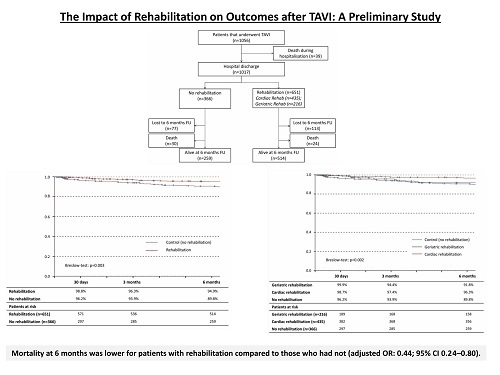
3. Results
3.1. Patient Characteristics
3.2. Procedural and In-Hospital Outcomes
3.3. Outcomes at Six Months
3.4. Cardiac vs. Geriatric Rehabilitation
4. Discussion
Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ribeiro, G.S.; Melo, R.D.; Deresz, L.F.; Dal Lago, P.; Pontes, M.R.; Karsten, M. Cardiac rehabilitation programme after transcatheter aortic valve implantation versus surgical aortic valve replacement: Systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 688–697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaede, L.; Blumenstein, J.; Kim, W.K.; Liebetrau, C.; Dörr, O.; Nef, H.; Hamm, C.; Elsässer, A.; Möllmann, H. Trends in aortic valve replacement in Germany in 2015: Transcatheter versus isolated surgical aortic valve repair. Clin. Res. Cardiol. 2017, 106, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Pressler, A.; Christle, J.W.; Lechner, B.; Grabs, V.; Haller, B.; Hettich, I.; Jochheim, D.; Mehilli, J.; Lange, R.; Bleiziffer, S.; et al. Exercise training improves exercise capacity and quality of life after transcatheter aortic valve implantation: A randomized pilot trial. Am. Heart J. 2016, 182, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Eichler, S.; Salzwedel, A.; Reibis, R.; Nothroff, J.; Harnath, A.; Schikora, M.; Butter, C.; Wegscheider, K.; Völler, H. Multicomponent cardiac rehabilitation in patients after transcatheter aortic valve implantation: Predictors of functional and psychocognitive recovery. Eur. J. Prev. Cardiol. 2017, 24, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Zanettini, R.; Gatto, G.; Mori, I.; Pozzoni, M.B.; Pelenghi, S.; Martinelli, L.; Klugmann, S. Cardiac rehabilitation and mid-term follow-up after transcatheter aortic valve implantation. J. Geriatr. Cardiol. 2014, 11, 279–285. [Google Scholar] [PubMed]
- Sola, M.; Ramm, C.J.; Kolarczyk, L.M.; Teeter, E.G.; Yeung, M.; Caranasos, T.G.; Vavalle, J.P. Application of a multidisciplinary enhanced recovery after surgery pathway to improve patient outcomes after transcatheter aortic valve implantation. Am. J. Cardiol. 2016, 118, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Völler, H.; Salzwedel, A.; Nitardy, A.; Buhlert, H.; Treszl, A.; Wegscheider, K. Effect of cardiac rehabilitation on functional and emotional status in patients after transcatheter aortic-valve implantation. Eur. J. Prev. Cardiol. 2015, 22, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Karoff, M.; Held, K.; Bjarnason-Wehrens, B. Cardiac rehabilitation in Germany. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V.; Littman, A.B. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J. Am. Coll. Cardiol. 1993, 22, 678–683. [Google Scholar] [CrossRef] [Green Version]
- Lavie, C.J.; Milani, R.V. Disparate effects of improving aerobic exercise capacity and quality of life after cardiac rehabilitation in young and elderly coronary patients. J. Cardiopulm. Rehabil. 2000, 20, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Brown, A.; Ebrahim, S.; Jolliffe, J.; Noorani, H.; Rees, K.; Skidmore, B.; Stone, J.A.; Thompson, D.R.; Oldridge, N. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am. J. Med. 2004, 116, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Goel, K.; Lennon, R.J.; Tilbury, R.T.; Squires, R.W.; Thomas, R.J. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation 2011, 123, 2344–2352. [Google Scholar] [CrossRef] [PubMed]
- Russo, N.; Compostella, L.; Tarantini, G.; Setzu, T.; Napodano, M.; Bottio, T.; D’Onofrio, A.; Isabella, G.; Gerosa, G.; Iliceto, S.; et al. Cardiac rehabilitation after transcatheter versus surgical prosthetic valve implantation for aortic stenosis in the elderly. Eur. J. Prev. Cardiol. 2014, 21, 1341–1348. [Google Scholar] [CrossRef] [PubMed]
- Fauchere, I.; Weber, D.; Maier, W.; Altwegg, L.; Lüscher, T.F.; Grünenfelder, J.; Nowak, A.; Tüller, D.; Genoni, M.; Falk, V.; et al. Rehabilitation after TAVI compared to surgical aortic valve replacement. Int. J. Cardiol. 2014, 173, 564–566. [Google Scholar] [CrossRef] [PubMed]
- Sumner, J.; Grace, S.L.; Doherty, P. Predictors of Cardiac Rehabilitation Utilization in England: Results from the National Audit. J. Am. Heart. Assoc. 2016, 5, e003903. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.H.; Dickens, C.; Anderson, R.; Richards, D.A.; Taylor, R.S.; Ukoumunne, O.C.; Turner, K.M.; Gandhi, M.; Kuyken, W.; Gibson, A.; et al. Assessing the effectiveness of Enhanced Psychological Care for patients with depressive symptoms attending cardiac rehabilitation compared with treatment as usual (CADENCE): A pilot cluster randomised controlled trial. Trials 2018, 19, 211. [Google Scholar] [CrossRef] [PubMed]
- Eichler, S.; Salzwedel, A.; Harnath, A.; Butter, C.; Wegscheider, K.; Chiorean, M.; Völler, H.; Reibis, R. Nutrition and mobility predict all-cause mortality in patients 12 months after transcatheter aortic valve implantation. Clin. Res. Cardiol. 2018, 107, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S. The importance of rehabilitation with cardiovascular diabetic patients after surgical interventions. Clin. Res. Cardiol. 2006, 95, i103–109. [Google Scholar] [CrossRef] [PubMed]
- Casanova, C.; Celli, B.R.; Barria, P.; Casas, A.; Cote, C.; de Torres, J.P.; Jardim, J.; Lopez, M.V.; Marin, J.M.; Montes de Oca, M.; et al. The 6-min walk distance in healthy subjects: Reference standards from seven countries. Eur. Respir. J. 2011, 37, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Wohlfart, B.; Farazdaghi, G.R. Reference values for the physical work capacity on a bicycle ergometer for men—a comparison with a previous study on women. Clin. Physiol. Funct. Imaging 2003, 23, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Green, P.; Woglom, A.E.; Genereux, P.; Daneault, B.; Paradis, J.M.; Schnell, S.; Hawkey, M.; Maurer, M.S.; Kirtane, A.J.; Kodali, S.; et al. The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: A single-center experience. JACC Cardiovasc. Interv. 2012, 5, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Dewey, T.M. Frailty scores and the writing on the wall. JACC Cardiovasc. Interv. 2012, 5, 497–498. [Google Scholar] [CrossRef] [PubMed]
- Strens, D.; Colle, A.; Vrijens, F.; Paulus, D.; Eyssen, M.; van Brabandt, H.; van Vlaenderen, I. Multidisciplinary outpatient rehabilitation following cardiac revascularization or valve surgery: Patient-related factors for uptake. Eur. J. Prev. Cardiol. 2013, 20, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Van Engen-Verheul, M.; de Vries, H.; Kemps, H.; Kraaijenhagen, R.; de Keizer, N.; Peek, N. Cardiac rehabilitation uptake and its determinants in the Netherlands. Eur. J. Prev. Cardiol. 2013, 20, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.B.; Berg, S.K.; Sibilitz, K.L.; Søgaard, R.; Thygesen, L.C.; Yazbeck, A.M.; Zwisler, A.D. Availability of, referral to and participation in exercise-based cardiac rehabilitation after heart valve surgery: Results from the national CopenHeart survey. Eur. J. Prev. Cardiol. 2015, 22, 710–718. [Google Scholar] [CrossRef] [PubMed]




| Rehabilitation (n = 651) Mean ± SD or Median (IQR) or proportion of patients (%) | No Rehabilitation (n = 366) Mean ± SD or Median (IQR) or proportion of patients (%) | p-Value | |
|---|---|---|---|
| Age (years) | 80.7 ± 6.0 | 80.1 ± 6.1 | 0.107 |
| Male sex | 290/651 (44.5) | 177/366 (48.4) | 0.241 |
| Body mass index (kg/m2) | 27.4 ± 5.3 | 28.3 ± 6.2 | 0.017 |
| Diabetes | 228/642 (35.5) | 166/359 (46.2) | 0.001 |
| Chronic kidney disease * | 300/651 (53.9) | 182/366 (49.7) | 0.199 |
| Prior pacemaker | 133/644 (20.7) | 73/363 (20.1) | 0.838 |
| CAD | 426/644 (66.1) | 235/366 (66.0) | 0.965 |
| Prior CABG | 96/644 (14.9) | 44/356 (12.4) | 0.266 |
| Prior PCI | 248/644 (38.5) | 134/356 (37.6) | 0.787 |
| Mitral valve insufficiency (>II°) | 22/633 (3.5) | 20/356 (5.6) | 0.109 |
| Prior valve replacement | 24/649 (3.7) | 16/364 (4.4) | 0.584 |
| LVEF (%) | 53.2 ± 12.9 | 51.7 ± 12.6 | 0.073 |
| NYHA | 0.498 | ||
| class III | 469/620 (75.6) | 256/347 (73.8) | |
| class IV | 53/620 (8.5) | 35/347 (10.1) | |
| NT-proBNP (pg/mL) | 2095 (871; 5573) | 2466 (1117; 6987) | 0.030 |
| Logistic EuroScore I (%) | 17.0 ± 11.8 | 17.9 ± 12.6 | 0.251 |
| Rehabilitation (n = 651) Mean ± SD or Median (IQR) or proportion of patients (%) | No Rehabilitation (n = 366) Mean ± SD or Median (IQR) or proportion of patients (%) | p-Value | |
|---|---|---|---|
| Conversion to surgery | 4/650 (0.6) | 4/362 (1.1) | 0.467 |
| Stroke | 13/649 (2.0) | 12/362 (3.3) | 0.198 |
| PPI | 56/646 (8.7) | 21/364 (5.8) | 0.095 |
| Valve-in-valve | 24/651 (3.7) | 15/366 (4.1) | 0.743 |
| Hospitalization post-TAVI (days) | 7.0 (6.0; 9.0) | 6.0 (5.0; 8.0) | <0.001 |
| NT-proBNP (pg/mL) | 1777 (775; 3,722) | 1838 (879; 4,232) | 0.334 |
| Cardiac function at discharge † | |||
| LVEF (%) | 54.2 ± 11.1 | 52.5 ± 11.7 | 0.031 |
| Peak valve gradient (mmHg) | 11.8 ± 5.9 | 11.7 ± 5.5 | 0.865 |
| Aortic insufficiency | 0.230 | ||
| mild | 25/581 (4.3) | 9/321 (2.8) | |
| moderate/severe | 1/581 (0.2) | 2/321 (0.6) |
| Rehabilitation Mean ± SD or Median (IQR) or proportion of patients (%) | No Rehabilitation Mean ± SD or Median (IQR) or proportion of patients (%) | p-Value | |
|---|---|---|---|
| All-cause mortality | 24/538 (4.5) | 30/289 (10.4) | 0.001 |
| CV death | 9/538 (1.7) | 8/289 (2.8) | 0.290 |
| Non-CV death | 7/538 (1.3) | 14/289 (4.8) | 0.002 |
| Unknown cause of death | 8/538 (1.5) | 8/289 (2.8) | 0.202 |
| Rehospitalization | 93/538 (17.3) | 61/289 (21.1) | 0.178 |
| Cardiac function | |||
| LVEF (%) | 55.0 ± 10.3 | 54.6 ± 10.6 | 0.636 |
| Peak valve gradient (mmHg) | 11.2 ± 5.7 | 11.3 ± 5.4 | 0.982 |
| Aortic insufficiency | 0.287 | ||
| mild | 17/414 (4.1) | 6/222 (2.7) | |
| moderate/severe | 1/414 (0.2) | 2/222 (0.9) | |
| NYHA | 0.105 | ||
| Class III | 158/392 (40.3) | 76/206 (36.9) | |
| Class IV | 4/392 (1.0) | 7/206 (3.4) | |
| NT-proBNP (pg/mL) | 849 (364, 1952) | 758 (381, 1951) | 0.778 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butter, C.; Groß, J.; Haase-Fielitz, A.; Sims, H.; Deutsch, C.; Bramlage, P.; Neuss, M. Impact of Rehabilitation on Outcomes after TAVI: A Preliminary Study. J. Clin. Med. 2018, 7, 326. https://doi.org/10.3390/jcm7100326
Butter C, Groß J, Haase-Fielitz A, Sims H, Deutsch C, Bramlage P, Neuss M. Impact of Rehabilitation on Outcomes after TAVI: A Preliminary Study. Journal of Clinical Medicine. 2018; 7(10):326. https://doi.org/10.3390/jcm7100326
Chicago/Turabian StyleButter, Christian, Jessica Groß, Anja Haase-Fielitz, Helen Sims, Cornelia Deutsch, Peter Bramlage, and Michael Neuss. 2018. "Impact of Rehabilitation on Outcomes after TAVI: A Preliminary Study" Journal of Clinical Medicine 7, no. 10: 326. https://doi.org/10.3390/jcm7100326