Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications
Abstract
:1. Introduction
2. The Medial Brachial Cutaneous Nerve (MBCN)
2.1. Anatomy
2.2. Scanning Technique
2.3. Clinical Implication
3. The Intercostobrachial Cutaneous Nerve (IBCN)
3.1. Anatomy
3.2. Scanning Technique
3.3. Clinical Implication
4. The Medial Antebrachial Cutaneous Nerve (MACN)
4.1. Anatomy
4.2. Scanning Technique
4.3. Clinical Implication
5. The Lateral Antebrachial Cutaneous Nerve (LACN)
5.1. Anatomy
5.2. Scanning Technique
5.3. Clinical Implication
6. The Posterior Antebrachial Cutaneous Nerve (PACN)
6.1. Anatomy
6.2. Scanning Technique
6.3. Clinical Implication
7. The Superficial Branch of the Radial Nerve (SBRN)
7.1. Anatomy
7.2. Scanning Technique
7.3. Clinical Implication
8. The Dorsal Cutaneous Branch of the Ulnar Nerve (DCBUN)
8.1. Anatomy
8.2. Scanning Technique
8.3. Clinical Implication
9. The Palmar Cutaneous Branch of the Median Nerve (PCMN)
9.1. Anatomy
9.2. Scanning Technique
9.3. Clinical Implication
10. The Anterior Femoral Cutaneous Nerve (AFCN)
10.1. Anatomy
10.2. Scanning Technique
10.3. Clinical Implication
11. The Posterior Femoral Cutaneous Nerve (PFCN)
11.1. Anatomy
11.2. Scanning Technique
11.3. Clinical Implication
12. The Lateral Femoral Cutaneous Nerve (LFCN)
12.1. Anatomy
12.2. Scanning Technique
12.3. Clinical Implication
13. The Medial Sural Cutaneous Nerve (MSCN), Lateral Sural Cutaneous Nerve (LSCN), and Sural Nerve
13.1. Anatomy
13.2. Scanning Technique
13.3. Clinical Implication
14. The Saphenous Nerve
14.1. Anatomy
14.2. Scanning Technique
14.3. Clinical Implication
15. Discussion
15.1. Critical Analyses for the Studies included in This Review
15.2. Application of Ultrasound in Diagnosing Cutaneous/Intra-Epidermal Nerve Pathology
15.3. Expert Opinion and Future Recommendation
16. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Statements
References
- Wu, C.H.; Chang, K.V.; Ozcakar, L.; Hsiao, M.Y.; Hung, C.Y.; Shyu, S.G.; Wang, T.G.; Chen, W.S. Sonographic tracking of the upper limb peripheral nerves: A pictorial essay and video demonstration. Am. J. Phys. Med. Rehabil. 2015, 94, 740–747. [Google Scholar]
- Hung, C.Y.; Hsiao, M.Y.; Ozcakar, L.; Chang, K.V.; Wu, C.H.; Wang, T.G.; Chen, W.S. Sonographic Tracking of the Lower Limb Peripheral Nerves: A Pictorial Essay and Video Demonstration. Am. J. Phys. Med. Rehabil. 2016, 95, 698–708. [Google Scholar]
- Chang, K.V.; Lin, C.P.; Hung, C.Y.; Ozcakar, L.; Wang, T.G.; Chen, W.S. Sonographic Nerve Tracking in the Cervical Region: A Pictorial Essay and Video Demonstration. Am. J. Phys. Med. Rehabil. 2016, 95, 862–870. [Google Scholar]
- Chang, K.V.; Lin, C.P.; Lin, C.S.; Wu, W.T.; Karmakar, M.K.; Ozcakar, L. Sonographic tracking of trunk nerves: Essential for ultrasound-guided pain management and research. J. Pain Res. 2017, 10, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Wu, W.T.; Han, D.S.; Ozcakar, L. Ulnar Nerve Cross-Sectional Area for the Diagnosis of Cubital Tunnel Syndrome: A Meta-Analysis of Ultrasonographic Measurements. Arch. Phys. Med. Rehabil. 2018, 99, 743–757. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.J.; Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasound Parameters other than the Direct Measurement of Ulnar Nerve Size for Diagnosing Cubital Tunnel Syndrome: A Systemic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2018. [Google Scholar] [CrossRef] [PubMed]
- Race, C.M.; Saldana, M.J. Anatomic course of the medial cutaneous nerves of the arm. J. Hand Surg. 1991, 16, 48–52. [Google Scholar] [CrossRef]
- Magazzeni, P.; Jochum, D.; Iohom, G.; Mekler, G.; Albuisson, E.; Bouaziz, H. Ultrasound-Guided Selective Versus Conventional Block of the Medial Brachial Cutaneous and the Intercostobrachial Nerves: A Randomized Clinical Trial. Reg. Anesthesia Pain Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Loukas, M.; Hullett, J.; Louis, R.G., Jr.; Holdman, S.; Holdman, D. The gross anatomy of the extrathoracic course of the intercostobrachial nerve. Clin. Anatomy 2006, 19, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Thallaj, A.K.; Al Harbi, M.K.; Alzahrani, T.A.; El-Tallawy, S.N.; Alsaif, A.A.; Alnajjar, M. Ultrasound imaging accurately identifies the intercostobrachial nerve. Saudi Med. J. 2015, 36, 1241–1244. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, J.E.; Januario, A.M.; Lins, O.G. Intercostobrachial neuropathy due to axillary compression. Muscle Nerve 2009, 39, 411–412. [Google Scholar]
- Benedikt, S.; Parvizi, D.; Feigl, G.; Koch, H. Anatomy of the medial antebrachial cutaneous nerve and its significance in ulnar nerve surgery: An anatomical study. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 1582–1588. [Google Scholar]
- Thallaj, A.; Marhofer, P.; Kettner, S.C.; Al-Majed, M.; Al-Ahaideb, A.; Moriggl, B. High-resolution ultrasound accurately identifies the medial antebrachial cutaneous nerve at the midarm level: A clinical anatomic study. Reg. Anesthesia Pain Med. 2011, 36, 499–501. [Google Scholar] [CrossRef] [PubMed]
- Seror, P. Forearm pain secondary to compression of the medial antebrachial cutaneous nerve at the elbow. Arch. Phys. Med. Rehabil. 1993, 74, 540–542. [Google Scholar] [CrossRef]
- Yildiz, N.; Ardic, F. A rare cause of forearm pain: Anterior branch of the medial antebrachial cutaneous nerve injury: A case report. J. Brachial Plex. Peripher. Nerve Inj. 2008, 3, 10. [Google Scholar] [CrossRef] [PubMed]
- Bourne, M.H.; Wood, M.B.; Carmichael, S.W. Locating the lateral antebrachial cutaneous nerve. J. hand Surg. 1987, 12, 697–699. [Google Scholar] [CrossRef]
- Chiavaras, M.M.; Jacobson, J.A.; Billone, L.; Lawton, J.M.; Lawton, J. Sonography of the lateral antebrachial cutaneous nerve with magnetic resonance imaging and anatomic correlation. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2014, 33, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Maida, E.; Chiavaras, M.M.; Jelsing, E.J.; O’Driscoll, S.W.; Pawlina, W.; Smith, J. Sonographic Visualization of the Posterior Cutaneous Nerve of the Forearm: Technique and Validation Using Perineural Injections in a Cadaveric Model. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2017, 36, 1627–1637. [Google Scholar] [CrossRef] [PubMed]
- Finneran, J.J.; Sandhu, N. Ultrasound-Guided Posterior Antebrachial Cutaneous Nerve Block: Technical Description and Block Distribution in Healthy Volunteers. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L.; Kim, J.; Ducic, I. Painful neuroma of the posterior cutaneous nerve of the forearm after surgery for lateral humeral epicondylitis. J. Hand Surg. 2004, 29, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; Tinhofer, I.; Weninger, W.J.; Grisold, W. Anatomical and ultrasound correlation of the superficial branch of the radial nerve. Muscle Nerve 2014, 50, 939–942. [Google Scholar]
- Chang, K.V.; Hung, C.Y.; Ozcakar, L. Snapping Thumb and Superficial Radial Nerve Entrapment in De Quervain Disease: Ultrasound Imaging/Guidance Revisited. Pain Med. 2015, 16, 2214–2215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goto, A.; Kunihiro, O.; Murase, T.; Moritomo, H. The dorsal cutaneous branch of the ulnar nerve: An anatomical study. Hand Surg. 2010, 15, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Le Corroller, T.; Bauones, S.; Acid, S.; Champsaur, P. Anatomical study of the dorsal cutaneous branch of the ulnar nerve using ultrasound. Eur. Radiol. 2013, 23, 2246–2251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasound Imaging for Dorsal Ulnar Cutaneous Neuropathy With Extensor Carpi Ulnaris Tendinopathy. Am. J. Phys. Med. Rehabil. 2017, 96, e191–e192. [Google Scholar]
- Hobbs, R.A.; Magnussen, P.A.; Tonkin, M.A. Palmar cutaneous branch of the median nerve. J. Hand Surg. 1990, 15, 38–43. [Google Scholar] [CrossRef]
- Tagliafico, A.; Pugliese, F.; Bianchi, S.; Bodner, G.; Padua, L.; Rubino, M.; Martinoli, C. High-resolution sonography of the palmar cutaneous branch of the median nerve. AJR. Am. J. Roentgenol. 2008, 191, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Pivec, C.; Bodner, G.; Mayer, J.A.; Brugger, P.C.; Paraszti, I.; Moser, V.; Traxler, H.; Riegler, G. Novel Demonstration of the Anterior Femoral Cutaneous Nerves using Ultrasound. Ultraschall in Med. 2018, 39, 318–327. [Google Scholar]
- Meng, S.; Lieba-Samal, D.; Reissig, L.F.; Gruber, G.M.; Brugger, P.C.; Platzgummer, H.; Bodner, G. High-resolution ultrasound of the posterior femoral cutaneous nerve: Visualization and initial experience with patients. Skelet. Radiol. 2015, 44, 1421–1426. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.S.; Johnson, R.L.; Niesen, A.D.; Stoike, D.E.; Pawlina, W. Ultrasound-Guided Posterior Femoral Cutaneous Nerve Block: A. Cadaveric Study. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2018, 37, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Onat, S.S.; Ata, A.M.; Ozcakar, L. Ultrasound-Guided Diagnosis and Treatment of Meralgia Paresthetica. Pain Physician 2016, 19, E667–E669. [Google Scholar] [PubMed]
- Damarey, B.; Demondion, X.; Boutry, N.; Kim, H.J.; Wavreille, G.; Cotten, A. Sonographic assessment of the lateral femoral cutaneous nerve. J. Clin. Ultrasound JCU 2009, 37, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Li, D.; Shao, J.; Hu, B. An ultrasound study of anatomic variants of the sural nerve. Muscle Nerve 2011, 43, 560–562. [Google Scholar]
- Kim, I.S.; Han, H.Y.; Hong, J.T.; Kim, J.S.; Lim, S.H. Sural Neuroma with Lumbosacral Radiculopathy-like Symptoms Diagnosed by Electrodiagnosis and Ultrasound. Am. J. Phys. Med. Rehabil. 2015, 94, e61–e62. [Google Scholar]
- Horn, J.L.; Pitsch, T.; Salinas, F.; Benninger, B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg. Anesthesia Pain Med. 2009, 34, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Trescot, A.M.; Brown, M.N.; Karl, H.W. Infrapatellar saphenous neuralgia-diagnosis and treatment. Pain Physician 2013, 16, E315–E324. [Google Scholar] [PubMed]
- Evers, S.; Thoreson, A.R.; Smith, J.; Zhao, C.; Geske, J.R.; Amadio, P.C. Ultrasound-guided hydrodissection decreases gliding resistance of the median nerve within the carpal tunnel. Muscle Nerve 2018, 57, 25–32. [Google Scholar]
- Lacomis, D. Small-fiber neuropathy. Muscle Nerve 2002, 26, 173–188. [Google Scholar]
- Ebadi, H.; Siddiqui, H.; Ebadi, S.; Ngo, M.; Breiner, A.; Bril, V. Peripheral Nerve Ultrasound in Small Fiber Polyneuropathy. Ultrasound Med. Biol. 2015, 41, 2820–2826. [Google Scholar]
- Brouwer, B.A.; Merkies, I.S.; Gerrits, M.M.; Waxman, S.G.; Hoeijmakers, J.G.; Faber, C.G. Painful neuropathies: The emerging role of sodium channelopathies. J. Peripher. Nerv. Syst. JPNS 2014, 19, 53–65. [Google Scholar] [CrossRef] [PubMed]










| Nerve | Anatomy | Scanning Technique | Clinical Implication |
|---|---|---|---|
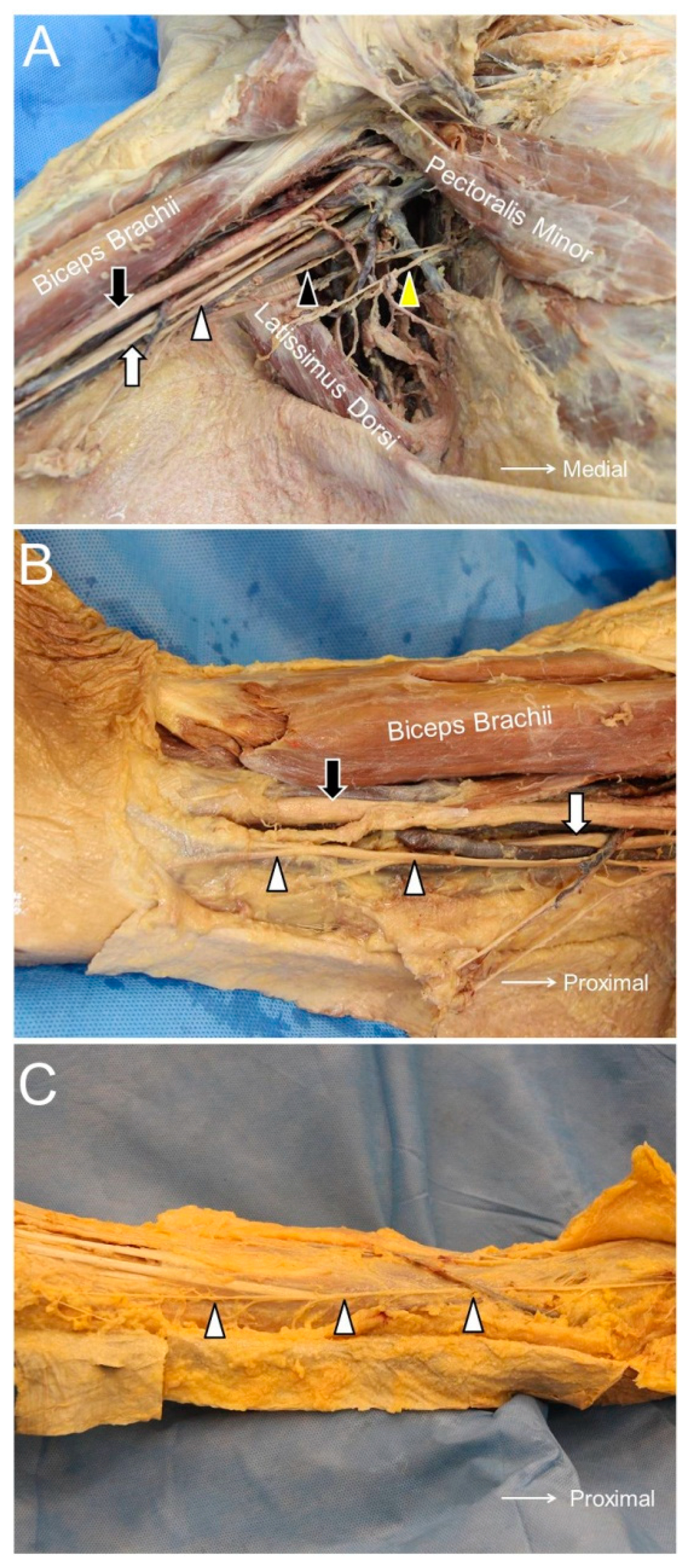
| Medial Brachial Cutaneous Nerve (MBCN) | The MBCN travels at the posterior aspect of the axilla in proximity to the axillary vein. | The transducer is placed on top of the teres major and latissimus dorsi muscles. The MBCN is located in the subcutaneous layer medial to the axillary neurovascular bundle. | The MBCN can be injured during surgeries near the axillary fossa, such as lymph node dissection and breast augmentation. |
| Intercostobrachial Cutaneous Nerve (IBCN) | The IBCN is the lateral cutaneous branch of the 2nd intercostal nerve. It pierces the intercostal and serratus anterior muscles, travels through the axilla, and reaches the middle aspect of the arm. | The transducer is placed on top of the teres major and latissimus dorsi muscles. The IBCN can be seen in the subcutaneous layer on top of the teres major and latissimus dorsi muscles. | The causes for injuries of the IBCN are similar to those of the MBCN. |
| Medial Antebrachial Cutaneous Nerve (MACN) | The MACN pierces the brachial fascia, which overlies the biceps brachii muscle and courses at the ulnar aspect of the brachial artery. At the elbow level, the MACN runs together with the basilic vein. | In the axillary fossa, the MACN can be seen on top of the axillary artery and vein, close to the median and ulnar nerves. The MACN can be identified distally following the basilic vein between the brachialis and the triceps brachii muscles. | The most common causes of MACN injury are iatrogenic, e.g., venous punctures, injections for medial epicondylitis, or cubital tunnel releases. |
| Lateral Antebrachial Cutaneous Nerve (LACN) | The LACN is the terminal sensory branch of the musculocutaneous nerve. | The transducer is placed on the elbow crease. The short axis of the LACN can be seen lateral to the biceps tendon. The cephalic vein is located beside the LACN. | Traumatic nerve injury during venipuncture is the main cause of LACN neuropathy. The second most common etiology is related to distal biceps tendon tears. |
| Posterior Antebrachial Cutaneous Nerve (PACN) | The PACN is a branch of the radial nerve and departs from its main trunk near the outlet of the spiral groove, then it emerges to the subcutaneous level. | The transducer is placed in the horizontal plane at the posterior mid-arm level. The radial nerve is seen underneath the lateral head of the triceps brachii muscle. Moving the transducer more distally, the PACN is seen leaving the radial nerve and then emerges at the subcutaneous level. | The PACN might be entrapped by scar tissue or a neuroma may develop after a lateral epicondylitis surgery. In patients with recalcitrant lateral epicondylitis, ultrasound (US)-guided injection and/or radiofrequency ablation can be considered as alternative approaches for better pain relief. |
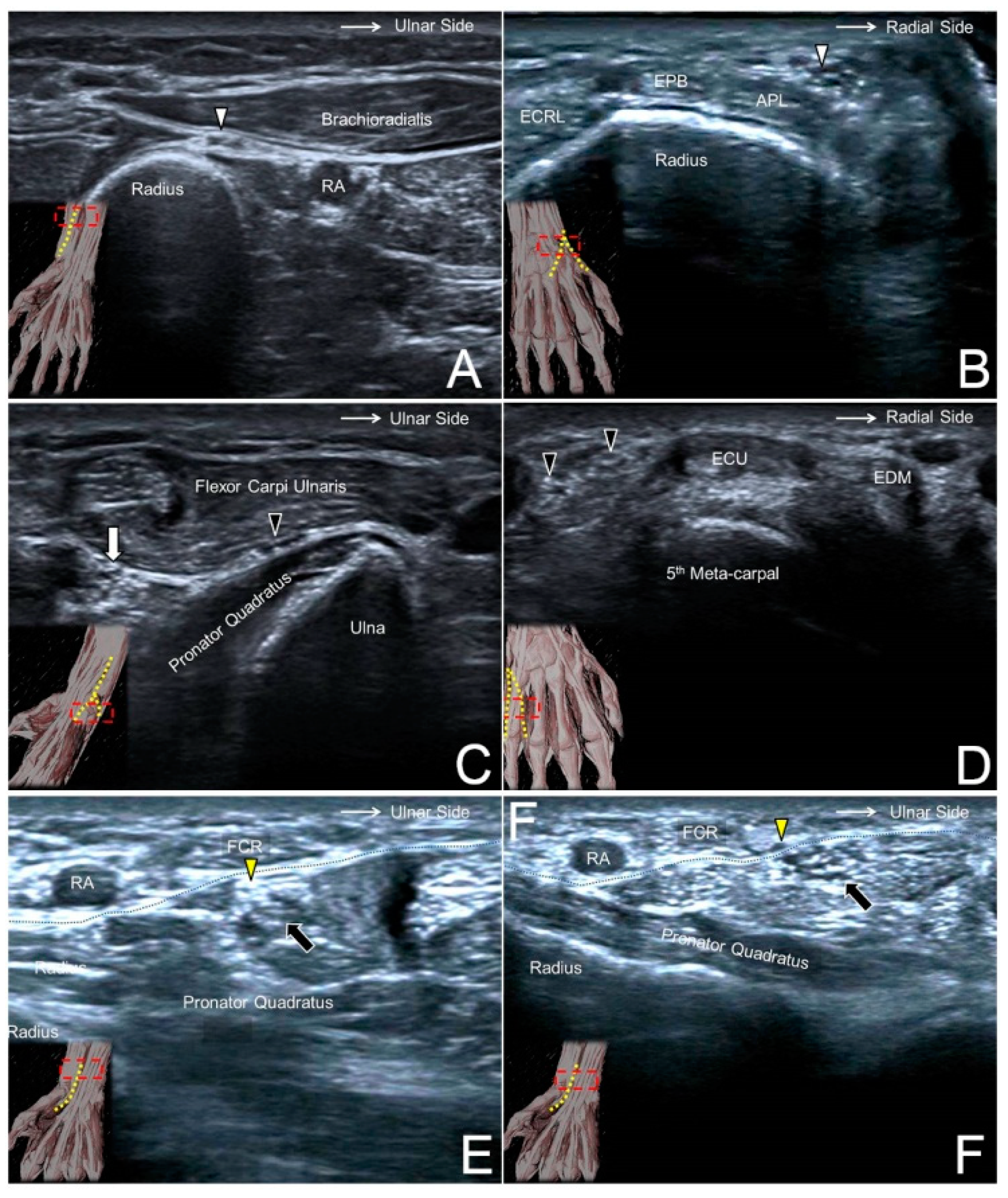
| Superficial Branch of the Radial Nerve (SBRN) | After branching from the main trunk of the radial nerve, the SBRN descends underneath the brachioradialis muscle and lateral to the radial artery. | The transducer is placed at the lateral side of the elbow crease to locate the radial nerve. Moving the transducer more distally, the SBRN is seen branching from the medial aspect of the radial nerve and descending underneath the brachioradialis muscle. | A compressive neuropathy of the SBRN is also named Wartenberg’s syndrome. The causes of nerve entrapment include compression by a bracelet, watch, or handcuff and irritation from an adjacent metal implant. An SBRN neuropathy is also associated with de Quervain’s tenosynovitis. |
| Dorsal Cutaneous Branch of the Ulnar Nerve (DCBUN) | The DCBUN branches from the ulnar nerve at the distal ulnar aspect of the forearm. It courses initially beneath the flexor carpi ulnaris tendon and pierces the deep fascia to reach the dorsal aspect of the wrist. | The transducer is placed on the distal third of the ventral forearm to locate the flexor carpi ulnaris muscle, underneath which lies the ulnar nerve. Moving the transducer more distally, the DCBUN is seen branching from the medial aspect of the ulnar nerve. | The risks of DCBUN neuropathy are similar to those of SBRN, e.g., compression by a bracelet or a metal plate fixed over the distal forearm. DCBUN neuropathy is associated with extensor carpi ulnaris tenosynovitis. |
| Palmar Cutaneous Branch of the Median Nerve (PCMN) | The PCMN arises from the radial aspect of the median nerve at the distal forearm. It pierces the antebrachial fascia between the flexor carpi radialis and palmaris longus tendons. | The transducer is placed on the distal forearm to visualize the median nerve. The PCMN emerges from the radial aspect of the median nerve. The PCMN later runs at the ulnar aspect of the flexor carpi radialis tendon. | Since the PCMN is superficial to the flexor retinaculum, it can easily be damaged during carpal tunnel release. When a US-guided short-axis injection for carpal tunnel syndrome is performed from the radial aspect, the PCMN should again/first be located to prevent an accidental injury. |
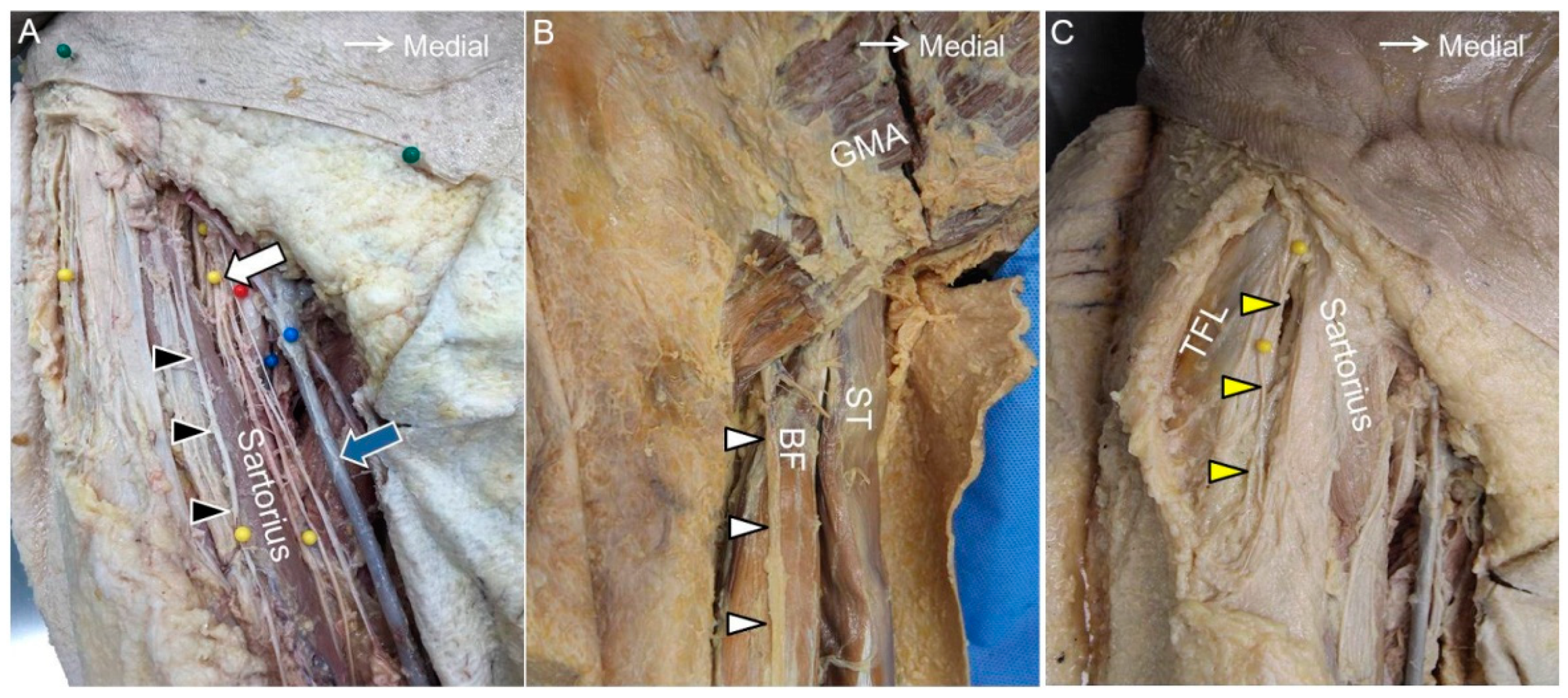
| Anterior Femoral Cutaneous Nerve (AFCN) | The AFCN is a branch of the femoral nerve. It divides into the intermediate and medial branches. | The transducer is placed horizontally at the proximal thigh to locate the femoral neurovascular bundle. The femoral nerve can be visualized lateral to the femoral artery and vein. Moving the transducer more distally, the AFCN is seen departing from the femoral nerve and coursing above the sartorius muscle. | An AFCN neuropathy commonly ensues due to iatrogenic injuries, e.g., a total knee replacement. Other causes comprise vein stripping, bypass grafting, lipoma excision, lymph node compression, and abscess removal. |
| Posterior Femoral Cutaneous Nerve (PFCN) | The PFCN courses parallel and medial to the sciatic nerve. At the level of the inferior gluteal fold, the PFCN starts to surface and departs from the sciatic nerve. | The transducer is placed on the proximal thigh, and the PFCN can be easily identified on the interval between the long head of the biceps femoris muscle and the semitendinosus muscle. | The PFCN is in proximity to the origin of the hamstring muscle. The most common cause of PFCN neuropathy is due to a hamstring injury. |
| Lateral Femoral Cutaneous Nerve (LFCN) | The LFCN usually passes underneath the inguinal ligament and runs in the fat compartment lateral to the sartorius muscle. | The transducer is placed proximal and medial to the anterior superior iliac spine to visualize the LFCN on the iliacus muscle. The transducer is then relocated distally to see the LFCN course underneath the inguinal ligament. | “Meralgia paresthetica” is a specific term used to describe symptoms regarding the entrapment of the LFCN. Common causes of nerve compression include tight clothing, increased belly fat, and pregnancy. |
| Sural Nerve | The medial sural cutaneous nerve originates from the tibial nerve in the popliteal fossa, and the lateral sural cutaneous nerve branches from the common peroneal nerve. The lateral sural cutaneous nerve gives off the sural communicating branch and merges with the medial sural cutaneous nerve to become the sural nerve at the middle calf. | Place the transducer at the mid-calf level to visualize the sural nerve on top of the gastrocnemius muscle. Moving the transducer distally, the sural nerve is visualized descending with the small saphenous vein and courses between the Achilles tendon and peroneus muscles at the distal leg. | The sural nerve is in proximity to the small saphenous vein and can be injured during surgeries for varicose veins. Another cause of nerve injury would be related to Achilles tendon ruptures whereby the nerve may be entrapped by an adjacent hematoma |
| Saphenous Nerve | The saphenous nerve is the terminal sensory branch of the femoral nerve and departs from the femoral nerve at the proximal thigh. It runs with the femoral artery inside the adductor tunnel and arises from the tunnel with the descending genicular artery. | The transducer is placed in the horizontal plane at the proximal medial thigh to locate the adductor canal. The saphenous nerve can be seen inside the canal. Moving the transducer more distally, the saphenous nerve will be seen exiting the adductor canal together with the descending genicular artery. | The saphenous nerve is vulnerable to injury during surgical interventions of the anterior medial knee. Common procedures that elicit a saphenous nerve injury include medial arthrotomy, meniscectomy, arthroscopic anterior cruciate ligament repair, and total knee replacement. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, K.-V.; Mezian, K.; Naňka, O.; Wu, W.-T.; Lou, Y.-M.; Wang, J.-C.; Martinoli, C.; Özçakar, L. Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. J. Clin. Med. 2018, 7, 457. https://doi.org/10.3390/jcm7110457
Chang K-V, Mezian K, Naňka O, Wu W-T, Lou Y-M, Wang J-C, Martinoli C, Özçakar L. Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. Journal of Clinical Medicine. 2018; 7(11):457. https://doi.org/10.3390/jcm7110457
Chicago/Turabian StyleChang, Ke-Vin, Kamal Mezian, Ondřej Naňka, Wei-Ting Wu, Yueh-Ming Lou, Jia-Chi Wang, Carlo Martinoli, and Levent Özçakar. 2018. "Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications" Journal of Clinical Medicine 7, no. 11: 457. https://doi.org/10.3390/jcm7110457
APA StyleChang, K.-V., Mezian, K., Naňka, O., Wu, W.-T., Lou, Y.-M., Wang, J.-C., Martinoli, C., & Özçakar, L. (2018). Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. Journal of Clinical Medicine, 7(11), 457. https://doi.org/10.3390/jcm7110457







