Small Airway Disease in Pulmonary Hypertension—Additional Diagnostic Value of Multiple Breath Washout and Impulse Oscillometry
Abstract
:1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Study Protocol
2.3. Statistical Analysis
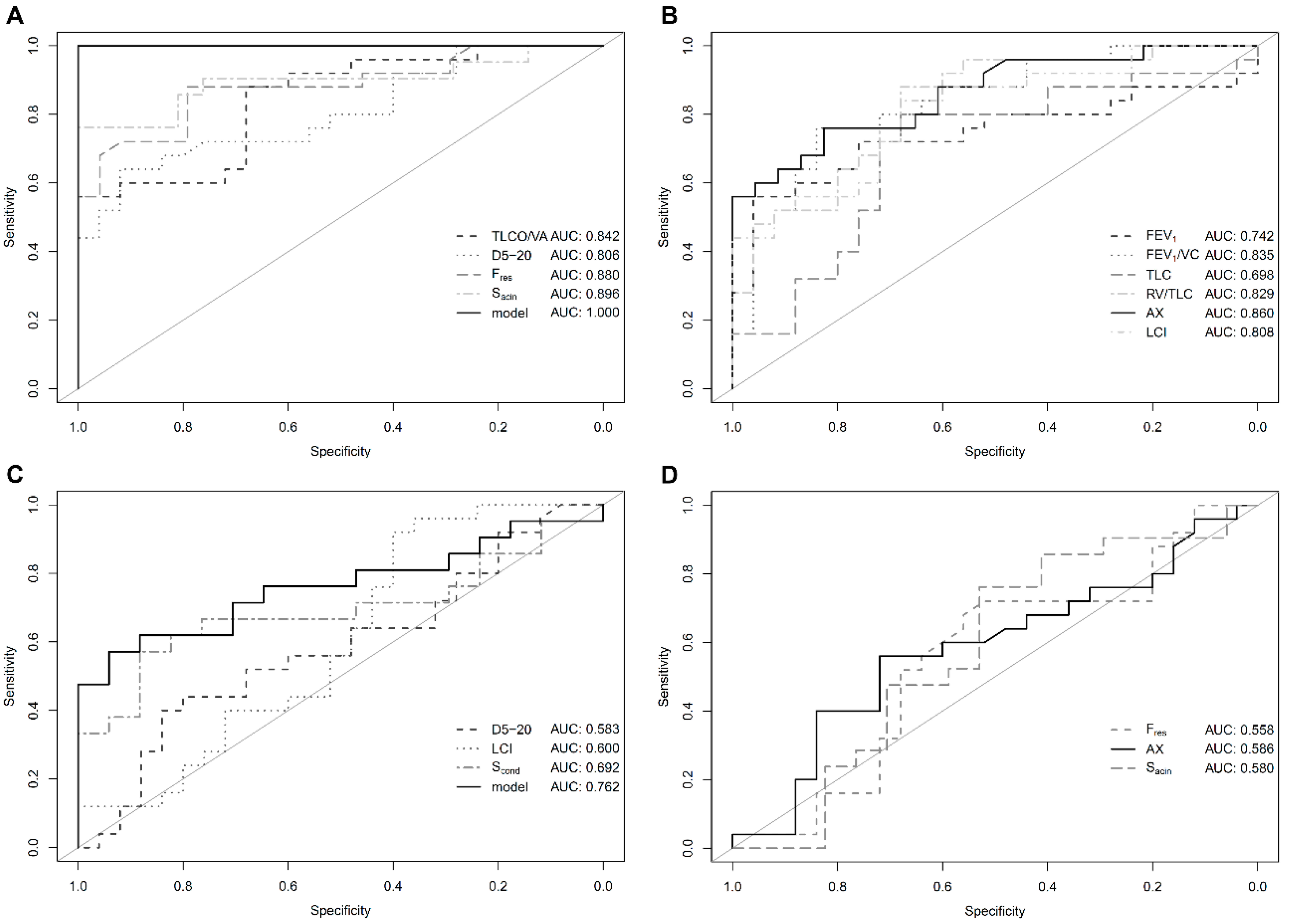
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Galie, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Respir. J. 2015, 46, 903–975. [Google Scholar] [CrossRef]
- Dyspnea. Mechanisms, assessment, and management: A consensus statement. American Thoracic Society. Am. J. Respir. Crit. Care Med. 1999, 159, 321–340. [Google Scholar] [CrossRef] [PubMed]
- Manning, H.L.; Schwartzstein, R.M. Pathophysiology of dyspnea. N. Engl. J. Med. 1995, 333, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, N.; McLoughlin, P. The structural basis of pulmonary hypertension in chronic lung disease: Remodelling, rarefaction or angiogenesis? J. Anat. 2002, 201, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Voelkel, N.F.; Quaife, R.A.; Leinwand, L.A.; Barst, R.J.; McGoon, M.D.; Meldrum, D.R.; Dupuis, J.; Long, C.S.; Rubin, L.J.; Smart, F.W.; et al. Right ventricular function and failure: Report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation 2006, 114, 1883–1891. [Google Scholar] [CrossRef]
- Burke, C.M.; Glanville, A.R.; Morris, A.J.; Rubin, D.; Harvey, J.A.; Theodore, J.; Robin, E.D. Pulmonary function in advanced pulmonary hypertension. Thorax 1987, 42, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.C.; Xu, X.Q.; Badesch, D.B.; Jiang, X.; Wu, Y.; Liu, J.M.; Wang, Y.; Pan, L.; Li, H.P.; Pu, J.L.; et al. Pulmonary function testing in patients with pulmonary arterial hypertension. Respir. Med. 2009, 103, 1136–1142. [Google Scholar] [CrossRef] [Green Version]
- Johnson, B.D.; Beck, K.C.; Olson, L.J.; O’Malley, K.A.; Allison, T.G.; Squires, R.W.; Gau, G.T. Pulmonary function in patients with reduced left ventricular function: Influence of smoking and cardiac surgery. Chest 2001, 120, 1869–1876. [Google Scholar] [CrossRef] [PubMed]
- Macchia, A.; Rodriguez Moncalvo, J.J.; Kleinert, M.; Comignani, P.D.; Gimeno, G.; Arakaki, D.; Laffaye, N.; Fuselli, J.J.; Massolin, H.P.; Gambarte, J.; et al. Unrecognised ventricular dysfunction in COPD. Eur. Respir. J. 2012, 39, 51–58. [Google Scholar] [CrossRef]
- Richter, M.J.; Voswinckel, R.; Tiede, H.; Schulz, R.; Tanislav, C.; Feustel, A.; Morty, R.E.; Ghofrani, H.A.; Seeger, W.; Reichenberger, F. Dynamic hyperinflation during exercise in patients with precapillary pulmonary hypertension. Respir. Med. 2012, 106, 308–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlsen, J.; Hasseriis Andersen, K.; Boesgaard, S.; Iversen, M.; Steinbruchel, D.; Bogelund Andersen, C. Pulmonary arterial lesions in explanted lungs after transplantation correlate with severity of pulmonary hypertension in chronic obstructive pulmonary disease. J. Heart Lung Transpl. 2013, 32, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Seeger, W.; Adir, Y.; Barbera, J.A.; Champion, H.; Coghlan, J.G.; Cottin, V.; de Marco, T.; Galie, N.; Ghio, S.; Gibbs, S.; et al. Pulmonary hypertension in chronic lung diseases. J. Am. Coll. Cardiol. 2013, 62, D109–D116. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.J.; Ewert, R.; Hoeper, M.M.; Olschewski, H.; Behr, J.; Winkler, J.; Wilkens, H.; Breuer, C.; Kubler, W.; Borst, M.M.; et al. Peripheral airway obstruction in primary pulmonary hypertension. Thorax 2002, 57, 473–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crisafulli, E.; Pisi, R.; Aiello, M.; Vigna, M.; Tzani, P.; Torres, A.; Bertorelli, G.; Chetta, A. Prevalence of Small-Airway Dysfunction among COPD Patients with Different GOLD Stages and Its Role in the Impact of Disease. Respiration 2017, 93, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Llontop, C.; Garcia-Quero, C.; Castro, A.; Dalmau, R.; Casitas, R.; Galera, R.; Iglesias, A.; Martinez-Ceron, E.; Soriano, J.B.; Garcia-Rio, F. Small airway dysfunction in smokers with stable ischemic heart disease. PLoS ONE 2017, 12, e0182858. [Google Scholar] [CrossRef] [Green Version]
- Trinkmann, F.; Saur, D.; Roth, K.; Borggrefe, M.; Kaden, J.; Michels, J.; Saur, J. Multiple breath washout (MBW) using sulfur hexafluoride – Proof of concept in COPD. Eur. Respir. J. 2016, 48, PA3440. [Google Scholar]
- Spiekerkoetter, E.; Fabel, H.; Hoeper, M.M. Effects of inhaled salbutamol in primary pulmonary hypertension. Eur. Respir. J. 2002, 20, 524–528. [Google Scholar] [CrossRef] [Green Version]
- Horsley, A.R.; O’Neill, K.; Downey, D.G.; Elborn, J.S.; Bell, N.J.; Smith, J.; Owers-Bradley, J. Closed circuit rebreathing to achieve inert gas wash-in for multiple breath wash-out. ERJ Open Res. 2016, 2. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Ho, D.; Imai, K.; King, G.; Stuart, E. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J. Stat. Softw. 2011, 42, 1–28. [Google Scholar] [CrossRef]
- Verbanck, S.; Thompson, B.R.; Schuermans, D.; Kalsi, H.; Biddiscombe, M.; Stuart-Andrews, C.; Hanon, S.; van Muylem, A.; Paiva, M.; Vincken, W.; et al. Ventilation heterogeneity in the acinar and conductive zones of the normal ageing lung. Thorax 2012, 67, 789–795. [Google Scholar] [CrossRef] [Green Version]
- Lum, S.; Stocks, J.; Stanojevic, S.; Wade, A.; Robinson, P.; Gustafsson, P.; Brown, M.; Aurora, P.; Subbarao, P.; Hoo, A.F.; et al. Age and height dependence of lung clearance index and functional residual capacity. Eur. Respir. J. 2013, 41, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Ciccone, M.M.; Aquilino, A.; Cortese, F.; Scicchitano, P.; Sassara, M.; Mola, E.; Rollo, R.; Caldarola, P.; Giorgino, F.; Pomo, V.; et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc. Heal. Risk Manag. 2010, 6, 297–305. [Google Scholar] [CrossRef]
- Trinkmann, F.; Gotzmann, J.; Saur, D.; Schroeter, M.; Roth, K.; Stach, K.; Borggrefe, M.; Saur, J.; Akin, I.; Michels, J.D. Multiple breath washout testing in adults with pulmonary disease and healthy controls—Can fewer measurements eventually be more? BMC Pulm. Med. 2017, 17, 185. [Google Scholar] [CrossRef] [PubMed]
- Fähndrich, S.; Lepper, P.; Trudzinski, F.; Seibert, M.; Wagenpfeil, S.; Bals, R. Lung Clearance Index is Increased in Patients with COPD—LCI Measurements in the Daily Routine. J. Pulm. Respir. Med. 2016, 6, 354. [Google Scholar] [CrossRef]
- Husemann, K.; Berg, N.; Engel, J.; Port, J.; Joppek, C.; Tao, Z.; Singer, F.; Schulz, H.; Kohlhaufl, M. Double tracer gas single-breath washout: Reproducibility in healthy subjects and COPD. Eur. Respir. J. 2014, 44, 1210–1222. [Google Scholar] [CrossRef] [PubMed]
- Bell, A.S.; Lawrence, P.J.; Singh, D.; Horsley, A. Feasibility and challenges of using multiple breath washout in COPD. Int. J. Chron. Obstruct. Pulm. Dis. 2018, 13, 2113–2119. [Google Scholar] [CrossRef] [PubMed]
- Yammine, S.; Lenherr, N.; Nyilas, S.; Singer, F.; Latzin, P. Using the same cut-off for sulfur hexafluoride and nitrogen multiple-breath washout may not be appropriate. J. Appl. Physiol. 2015, 119, 1510–1512. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, J.G. Lung clearance index: Should we really go back to nitrogen washout? Eur. Respir. J. 2014, 43, 655–656. [Google Scholar] [CrossRef]
- Sullivan, L.; Forno, E.; Pedersen, K.; Nielsen, J.G.; Weiner, D.J. Nitrogen back-diffusion during multiple-breath washout with 100% oxygen. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef]
- Kane, M.; Rayment, J.H.; Jensen, R.; McDonald, R.; Stanojevic, S.; Ratjen, F. Correcting for tissue nitrogen excretion in multiple breath washout measurements. PLoS ONE 2017, 12, e0185553. [Google Scholar] [CrossRef]
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.; Coates, A.; van der Grinten, C.P.; Gustafsson, P.; Hankinson, J.; et al. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCartney, C.T.; Weis, M.N.; Ruppel, G.L.; Nayak, R.P. Residual Volume and Total Lung Capacity to Assess Reversibility in Obstructive Lung Disease. Respir. Care 2016, 61, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.; Reinhold, P.; Goldman, M. Chapter 5: Forced oscillation technique and impulse oscillometry. In Lung Function testing: European Respiratory Society Monograph; Gosselink, R., Stam, H., Eds.; European Respiratory Society: Sheffield, UK, 2005; Volume 31, pp. 72–105. [Google Scholar]
| PH (n = 25) | Healthy Controls (n = 25) | Non-Healthy Controls (n = 25) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unit | Mean | Range | Mean | Range | p-Value # | Mean | Range | p-Value # | ||
| Age | years | 73 ± 10 | 46–86 | 55 ± 18 | 22–85 | <0.001 * | 72 ± 13 | 40–86 | 0.65 | |
| Male | 13 (52%) | 15 (60%) | 0.78 | 14 (56%) | >0.9 | |||||
| Weight | kg | 76 ± 16 | 53–110 | 81 ± 22 | 51–132 | 0.37 | 76 ± 16 | 53–110 | 0.98 | |
| Height | cm | 164 ± 9 | 149–178 | 171 ± 9 | 157–198 | 0.01 * | 165 ± 7 | 154–180 | 0.51 | |
| Obesity | ||||||||||
| yes/no | n | 8/17 | 8/17 | >0.9 | 9/16 | >0.9 | ||||
| % | 32/68 | 32/68 | 36/64 | |||||||
| Arterial hypertension | ||||||||||
| yes/no | n | 17/8 | 4/21 | <0.001 * | 16/9 | >0.9 | ||||
| % | 68/32 | 16/84 | 64/36 | |||||||
| Diabetes mellitus | ||||||||||
| yes/no | n | 7/18 | 2/23 | 0.14 | 4/21 | 0.49 | ||||
| % | 28/72 | 8/92 | 16/84 | |||||||
| Smoker | ||||||||||
| yes/ex/no | n | 2/10/13 | 3/6/16 | 0.47 | 3/11/11 | 0.81 | ||||
| % | 8/40/52 | 12/24/64 | 12/44/44 | |||||||
| PH (n = 25) | Healthy Controls (n = 25) | Non-Healthy Controls (n = 25) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unit | Mean | Range | Mean | Range | p-Value # | Mean | Range | p-Value # | |||
| Spirometry | |||||||||||
| FEV1/VC | % | 88 ± 13 | 44–109 | 98 ± 8 | 84–115 | <0.01 * | 86 ± 19 | 38–116 | 0.61 | ||
| FEV1 | %pred | 81 ± 32 | 27–152 | 101 ± 16 | 65–135 | 0.01 * | 74 ± 27 | 30–135 | 0.41 | ||
| VC | %pred | 91 ± 26 | 44–147 | 102 ± 16 | 64–124 | 0.06 | 88 ± 27 | 37–135 | 0.75 | ||
| Body Plethysmography | |||||||||||
| TLC | %pred | 97 ± 15 | 63–125 | 107 ± 10 | 87–124 | 0.01 * | 102 ± 31 | 51–166 | 0.47 | ||
| RV | %pred | 119 ± 25 | 80–188 | 120 ± 12 | 82–142 | 0.78 | 130 ± 57 | 56–324 | 0.38 | ||
| RV/TLC | % | 51 ± 9 | 33–71 | 39 ± 8 | 27–57 | <0.00001 * | 52 ± 11 | 30–83 | 0.88 | ||
| FRCpleth | L | 3.1 ± 0.7 | 1.8–4.5 | 3.1 ± 0.5 | 2.4–4.2 | 0.64 | 3.3 ± 1.2 | 1.8–6.2 | 0.30 | ||
| TLCO/VA | %pred | 69± 22 | 18–103 | 96 ± 10 | 80–115 | <0.00001 * | 70 ± 29 | 12–115 | 0.89 | ||
| Impulse Oscillometry | |||||||||||
| D5-20 | % | 49 ± 36 | 5–114 | 14 ± 12 | 0–47 | <0.0001 * | 40 ± 39 | 0–170 | 0.39 | ||
| Fres | Hz | 19 ± 6 | 9–37 | 11 ± 4 | 3–19 | <0.00001 * | 19 ± 7 | 8–35 | 0.74 | ||
| AX | - | 1.58 ± 1.62 | 0.11–7.8 | 0.29 ± 0.27 | 0.01–1.1 | <0.001 * | 1.30 ± 1.66 | 0.0–7.0 | 0.55 | ||
| Multiple Breath Washout | |||||||||||
| LCI | - | 8.7 ± 1.3 | 6.7–11.6 | 7.4 ± 0.8 | 6.2–8.9 | <0.001 * | 10.1 ± 2.9 | 7.2–17.6 | 0.04 * | ||
| FRCMBW | L | 2.6 ± 0.8 | 1.2–4.4 | 2.9 ± 0.8 | 1.2–4.4 | 0.14 | 2.5 ± 0.6 | 1.3–4.3 | 0.53 | ||
| Sacin | L−1 | 0.26 ± 0.12 | 0.03–0.46 | 0.1 ± 0.06 | −0.04–0.18 | <0.00001 * | 0.32 ± 0.35 | −0.14–1.12 | 0.50 | ||
| Scond | L−1 | 0.03 ± 0.07 | −0.14–0.15 | 0.05 ± 0.04 | −0.05–0.13 | 0.24 | 0.06 ± 0.03 | 0.0–0.13 | 0.04 * | ||
| PH (n = 25) | |||
|---|---|---|---|
| Unit | Mean | Range | |
| Right Heart Catheter | |||
| mPAP | mmHg | 34 ± 14 | 22–87 |
| PAWP | mmHg | 16 ± 6 | 2–25 |
| DPG | mmHg | 4 ± 8 | −6–24 |
| type | n | 10/11/4 | |
| pre/post/mixed | % | 40/44/16 | |
| Nizza class | n | 7/13/2/2/1 | |
| 1/2/3/4/5 | % | 28/52/8/8/4 | |
| Echocardiography | |||
| sPAP | mmHg | 57 ± 19 | 20–90 |
| TAPSE | mm | 19 ± 4 | 13–28 |
| heart failure | n | 2/13/4 | |
| sys/dia/both | % | 8/52/16 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trinkmann, F.; Gawlitza, J.; Künstler, M.; Schäfer, J.; Schroeter, M.; Michels, J.D.; Stach, K.; Dösch, C.; Saur, J.; Borggrefe, M.; et al. Small Airway Disease in Pulmonary Hypertension—Additional Diagnostic Value of Multiple Breath Washout and Impulse Oscillometry. J. Clin. Med. 2018, 7, 532. https://doi.org/10.3390/jcm7120532
Trinkmann F, Gawlitza J, Künstler M, Schäfer J, Schroeter M, Michels JD, Stach K, Dösch C, Saur J, Borggrefe M, et al. Small Airway Disease in Pulmonary Hypertension—Additional Diagnostic Value of Multiple Breath Washout and Impulse Oscillometry. Journal of Clinical Medicine. 2018; 7(12):532. https://doi.org/10.3390/jcm7120532
Chicago/Turabian StyleTrinkmann, Frederik, Joshua Gawlitza, Monique Künstler, Julia Schäfer, Michele Schroeter, Julia D. Michels, Ksenija Stach, Christina Dösch, Joachim Saur, Martin Borggrefe, and et al. 2018. "Small Airway Disease in Pulmonary Hypertension—Additional Diagnostic Value of Multiple Breath Washout and Impulse Oscillometry" Journal of Clinical Medicine 7, no. 12: 532. https://doi.org/10.3390/jcm7120532
APA StyleTrinkmann, F., Gawlitza, J., Künstler, M., Schäfer, J., Schroeter, M., Michels, J. D., Stach, K., Dösch, C., Saur, J., Borggrefe, M., & Akin, I. (2018). Small Airway Disease in Pulmonary Hypertension—Additional Diagnostic Value of Multiple Breath Washout and Impulse Oscillometry. Journal of Clinical Medicine, 7(12), 532. https://doi.org/10.3390/jcm7120532





