Sensitivity and Specificity of Ultrawide-Field Fundus Photography for the Staging of Sickle Cell Retinopathy in Real-Life Practice at Varying Expertise Level
Abstract
1. Introduction
2. Experimental Section
2.1. Population
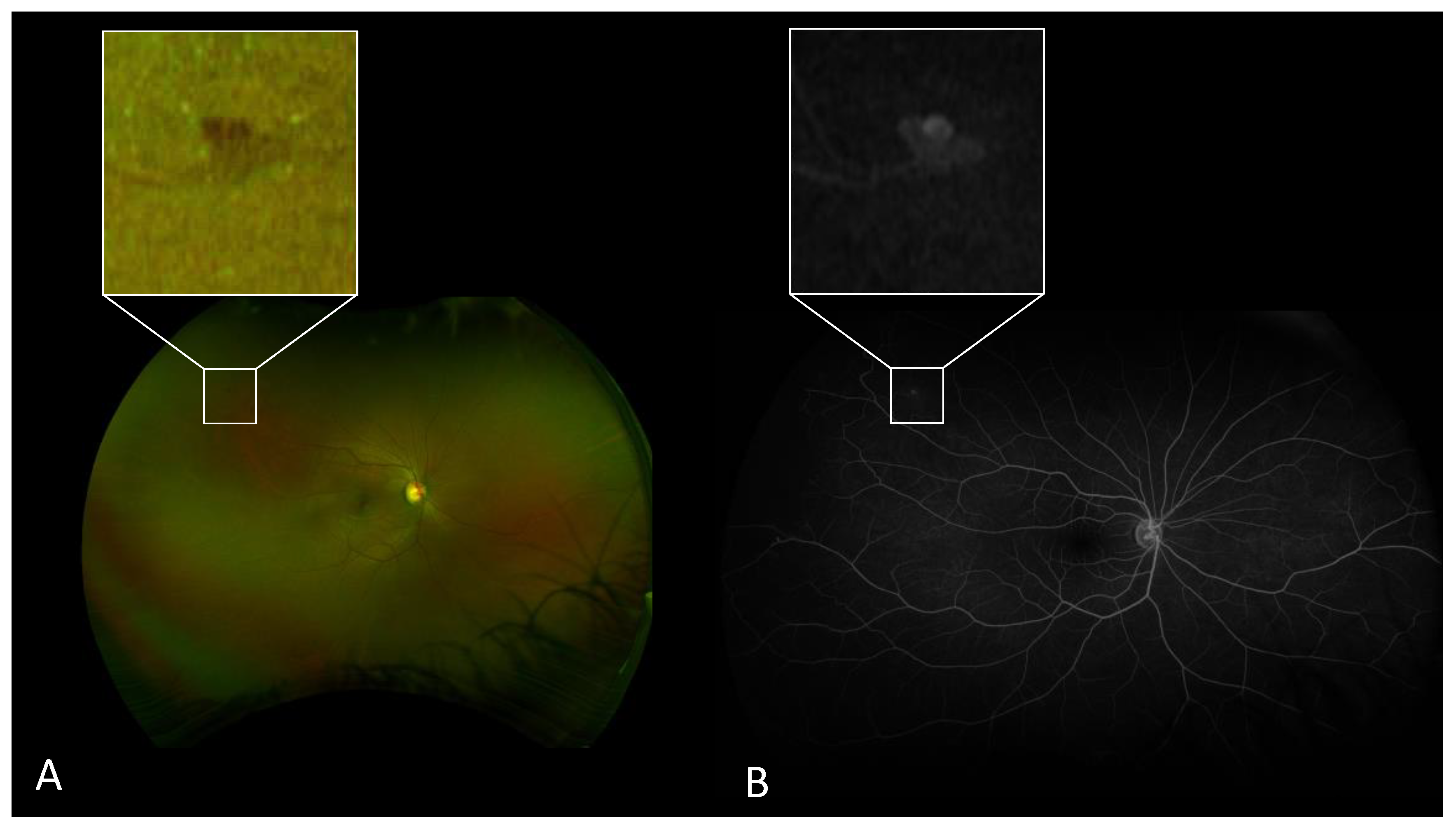
2.2. Image Acquisition and Image Analysis
2.3. Statistical Analysis
3. Results
3.1. Demographic Results
3.2. Sensitivity and Specificity of UW-FP
3.3. Inter-Method Agreement
3.4. Inter-Grader Agreement
3.5. SCR Stages and SCD Genotype
4. Discussion
Author Contributions
Conflicts of Interest
References
- Piel, F.B.; Hay, S.I.; Gupta, S.; Weatherall, D.J.; Williams, T.N. Global Burden of Sickle Cell Anaemia in Children under Five, 2010–2050: Modelling Based on Demographics, Excess Mortality, and Interventions. PLoS Med. 2013, 10, e1001484. [Google Scholar] [CrossRef] [PubMed]
- Piel, F.B.; Steinberg, M.H.; Rees, D.C. Sickle Cell Disease. N. Engl. J. Med. 2017, 376, 1561–1573. [Google Scholar] [CrossRef] [PubMed]
- Ware, R.E.; de Montalembert, M.; Tshilolo, L.; Abboud, M.R. Sickle cell disease. Lancet. 2017, 390, 311–323. [Google Scholar] [CrossRef]
- Yawn, B.P.; Buchanan, G.R.; Afenyi-Annan, A.N.; Ballas, S.K.; Hassell, K.L.; James, A.H.; Jordan, L.; Lanzkron, S.M.; Lottenberg, R.; Savage, W.J.; et al. Management of Sickle Cell Disease: Summary of the 2014 Evidence-Based Report by Expert Panel Members. Jama 2014, 312, 1033–1048. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, M.F. Natural history of untreated proliferative sickle retinopathy. Arch. Ophthalmol. 1971, 85, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Nagiel, A.; Lalane, R.A.; Sadda, S.R.; Schwartz, S.D. Ultra-widefield fundus imaging: A Review of Clinical Applications and Future Trends. Retina 2016, 36, 660–678. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.; Kiss, S. Detection and monitoring of sickle cell retinopathy using ultra wide-field color photography and fluorescein angiography. Retina 2011, 31, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Han, I.C.; Zhang, A.Y.; Liu, T.Y.A.; Linz, M.O.; Scott, A.W. Utility of ultra-widefield retinal imaging for the staging and management of sickle cell retinopathy. Retina 2019, 39, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, M.F. Classification and Pathogenesis of Proliferative Sickle Retinopathy. Am. J. Ophthalmol. 1971, 71, 649–665. [Google Scholar] [CrossRef]
- Downes, S.M.; Hambleton, I.R.; Chuang, E.L.; Lois, N.; Serjeant, G.R.; Bird, A.C. Incidence and Natural History of Proliferative Sickle Cell Retinopathy. Ophthalmology 2005, 112, 1869–1875. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S.C.N.; Schwartz, S.D. Peripheral Vessel Leakage (PVL): A New Angiographic Finding in Diabetic Retinopathy Identified with Ultra Wide-Field Fluorescein Angiography. Semin. Ophthalmol. 2010, 25, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Lee, M.Y.; Ham, D.-I. Ultrawide-Field Fluorescein Angiography for Evaluation of Diabetic Retinopathy. Korean J. Ophthalmol. 2012, 26, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Wessel, M.M.; Aaker, G.D.; Parlitsis, G.; Cho, M.; D’Amico, D.J.; Kiss, S. Ultra–wide-field angiography improves the detection and classification of diabetic retinopathy. Retina 2012, 32, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Friberg, T.R.; Gupta, A.; Yu, J.; Huang, L.; Suner, I.; Puliafito, C.A.; Schwartz, S.D. Ultrawide angle fluorescein angiographic imaging: A comparison to conventional digital acquisition systems. Ophthalmic Surg. Lasers Imaging 2008, 39, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Spaide, R.F. Peripheral areas of nonperfusion in treated central retinal vein occlusion as imaged by wide-field fluorescein angiography. Retina 2011, 31, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Pahl, D.A.; Green, N.S.; Bhatia, M.; Chen RWS. New Ways to Detect Pediatric Sickle Cell Retinopathy: A Comprehensive Review. J. Pediatr. Hematol./Oncol. 2017, 39, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Myint, K.T.; Sahoo, S.; Thein, A.W.; Moe, S.; Ni, H. Laser Therapy for Retinopathy in Sickle Cell Disease; Fibrosis, C.C., Group, G.D., Eds.; Cochrane Database of Systematic Reviews: New York, NY, USA, 2015. [Google Scholar] [CrossRef]
- Yannuzzi, L.A.; Rohrer, K.T.; Tindel, L.J.; Sobel, R.S.; Costanza, M.A.; Shields, W.; Zang, E. Fluorescein angiography complication survey. Ophthalmology 1986, 93, 611–617. [Google Scholar] [CrossRef]
- Xu, K.; Tzankova, V.; Li, C.; Sharma, S. Intravenous fluorescein angiography–associated adverse reactions. Can. J. Ophthalmol. 2016, 51, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Han, I.C.; Linz, M.O.; Liu, T.Y.A.; Zhang, A.Y.; Tian, J.; Scott, A.W. Correlation of Ultra-Widefield Fluorescein Angiography and OCT Angiography in Sickle Cell Retinopathy. Ophthalmol. Retina 2018, 2, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Falavarjani, K.G.; Scott, A.W.; Wang, K.; Han, I.C.; Chen, X.; Klufas, M.; Hubschman, J.-P.; Sadda, S.R.; Sarraf, D.; Tsui, I.; et al. Correlation of multimodal imaging in sickle cell retinopathy. Retina 2016, 36, S111–S117. [Google Scholar] [CrossRef] [PubMed]
| All Patients n = 63 Eyes, 33 Patients | HbSS Group n = 38 Eyes, 20 Patients | HbSC Group n = 21 Eyes, 11 Patients | -thal Group n = 4 Eyes, 2 Patients | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean or n | SD or Percent | Mean or n | SD or Percent | Mean or n | SD or Percent | Mean or n | SD or Percent | ||
| Age | 27.70 | 11.69 | 25.75 | 8.72 | 28.82 | 10.12 | 41 | 38.18 | 0.70 |
| Male sex | 15 | 45.45 | 8 | 40 | 6 | 54.54 | 1 | 50 | 0.73 |
| Goldberg stage | 1.68 | 0.93 | 1.55 | 0.80 | 2.14 | 0.96 | 0.5 | 0.58 | 0.004 |
| stage 0 | 4 | 6.35 | 1 | 2.63 | 1 | 4.76 | 2 | 50.00 | N/A |
| stage 1 | 27 | 42.86 | 21 | 55.26 | 4 | 19.05 | 2 | 50.00 | N/A |
| stage 2 | 18 | 28.57 | 10 | 26.32 | 8 | 38.10 | 0 | 0 | N/A |
| stage 3 | 13 | 20.63 | 6 | 15.79 | 7 | 33.33 | 0 | 0 | N/A |
| stage 4 | 1 | 1.59 | 0 | 0 | 1 | 4.76 | 0 | 0 | N/A |
| stage 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | N/A |
| Inter-Method | Retinal Specialist | Ophthalmology Resident | ||
| Agreement (%) | Kappa Coefficient | Agreement (%) | Kappa Coefficient | |
| Proliferative SCR | 100 | 1 | 98.41 | 0.9468 |
| SCR staging | 82.5 | 0.7561 | 63.49 | 0.5116 |
| Inter-Grader | UWF-FP | UWF-AF | ||
| Agreement (%) | Kappa Coefficient | Agreement (%) | Kappa Coefficient | |
| Proliferative SCR | 96.83 | 0.9032 | 95.24 | 0.8508 |
| SCR staging | 52.38 | 0.3647 | 53.97 | 0.3669 |
| Expertise Level | Stages Difference UWF-FP vs. UWF-FA | Eyes (%) | Stages (eyes) |
|---|---|---|---|
| Retinal specialist | + 1 stage difference | 1 (1.6) | 2-1 (1) |
| No stage difference | 52 (82.5) | - | |
| − 1 stage difference | 10 (15.9) | 0-1 (6) | |
| 1-2 (4) | |||
| Ophthalmology resident | + 2 stages difference | 2 (3.2) | 2-0 (2) |
| + 1 stage difference | 5 (7.9) | 1-0 (1) | |
| 2-1 (3) | |||
| 3-2 (1) | |||
| No stage difference | 40 (63.5) | ||
| − 1 stage difference | 14 (22.2) | 0-1 (7) | |
| 1-2 (7) | |||
| − 2 stages difference | 2 (3.2) | 0-2 (2) |
| Stages Difference | Eyes (%) | Stages (Eyes) |
|---|---|---|
| + 1 stage difference | 7 (11.11) | 2-1 (7) |
| No stage difference | 34 (53.97) | - |
| − 1 stage difference | 21 (33.33) | 0-1 (9) |
| 1-2 (10) | ||
| 2-3 (2) | ||
| − 2 stages difference | 1 (1.59) | 3-1 (1) |
| Goldberg Stage | Genotype | Total | ||
|---|---|---|---|---|
| SS (%) | SC (%) | thal (%) | ||
| 0 | 1 (25) | 1 (25) | 2 (50) | 4 |
| 1 | 21 (77,78) | 4 (14,81) | 2 (7,41) | 27 |
| 2 | 10 (55,56) | 8 (44,44) | 0 (0) | 18 |
| 3 | 6 (46,15) | 7 (53,85) | 0 (0) | 13 |
| 4 | 0 (0) | 1 (100) | 0 (0) | 1 |
| Total | 38 (60,32) | 21 (33,33) | 4 (6,35) | 63 (100) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bunod, R.; Mouallem-Beziere, A.; Amoroso, F.; Capuano, V.; Bitton, K.; Kamami-Levy, C.; Jung, C.; Souied, E.H.; Miere, A. Sensitivity and Specificity of Ultrawide-Field Fundus Photography for the Staging of Sickle Cell Retinopathy in Real-Life Practice at Varying Expertise Level. J. Clin. Med. 2019, 8, 1660. https://doi.org/10.3390/jcm8101660
Bunod R, Mouallem-Beziere A, Amoroso F, Capuano V, Bitton K, Kamami-Levy C, Jung C, Souied EH, Miere A. Sensitivity and Specificity of Ultrawide-Field Fundus Photography for the Staging of Sickle Cell Retinopathy in Real-Life Practice at Varying Expertise Level. Journal of Clinical Medicine. 2019; 8(10):1660. https://doi.org/10.3390/jcm8101660
Chicago/Turabian StyleBunod, Roxane, Alexandra Mouallem-Beziere, Francesca Amoroso, Vittorio Capuano, Karen Bitton, Cynthia Kamami-Levy, Camille Jung, Eric H. Souied, and Alexandra Miere. 2019. "Sensitivity and Specificity of Ultrawide-Field Fundus Photography for the Staging of Sickle Cell Retinopathy in Real-Life Practice at Varying Expertise Level" Journal of Clinical Medicine 8, no. 10: 1660. https://doi.org/10.3390/jcm8101660
APA StyleBunod, R., Mouallem-Beziere, A., Amoroso, F., Capuano, V., Bitton, K., Kamami-Levy, C., Jung, C., Souied, E. H., & Miere, A. (2019). Sensitivity and Specificity of Ultrawide-Field Fundus Photography for the Staging of Sickle Cell Retinopathy in Real-Life Practice at Varying Expertise Level. Journal of Clinical Medicine, 8(10), 1660. https://doi.org/10.3390/jcm8101660






