Minimally Invasive AC Joint Reconstruction System (MINAR®) in Modified Triple-Button Technique for the Treatment of Acute AC Joint Dislocation
Abstract
1. Introduction
2. Experimental Section
2.1. Patients
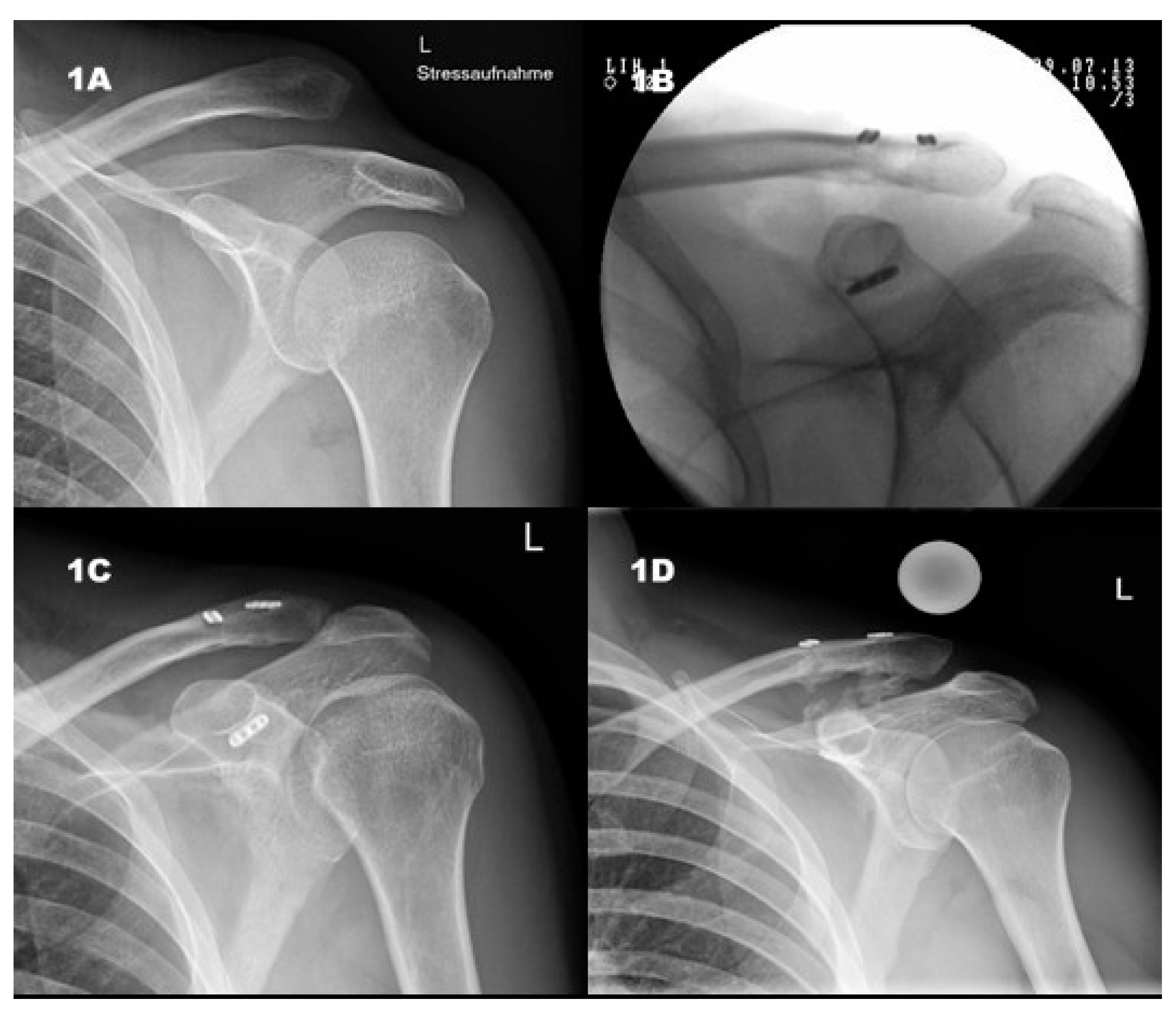
2.2. X-ray
2.3. Clinical Examination and Scores
2.4. Statistics
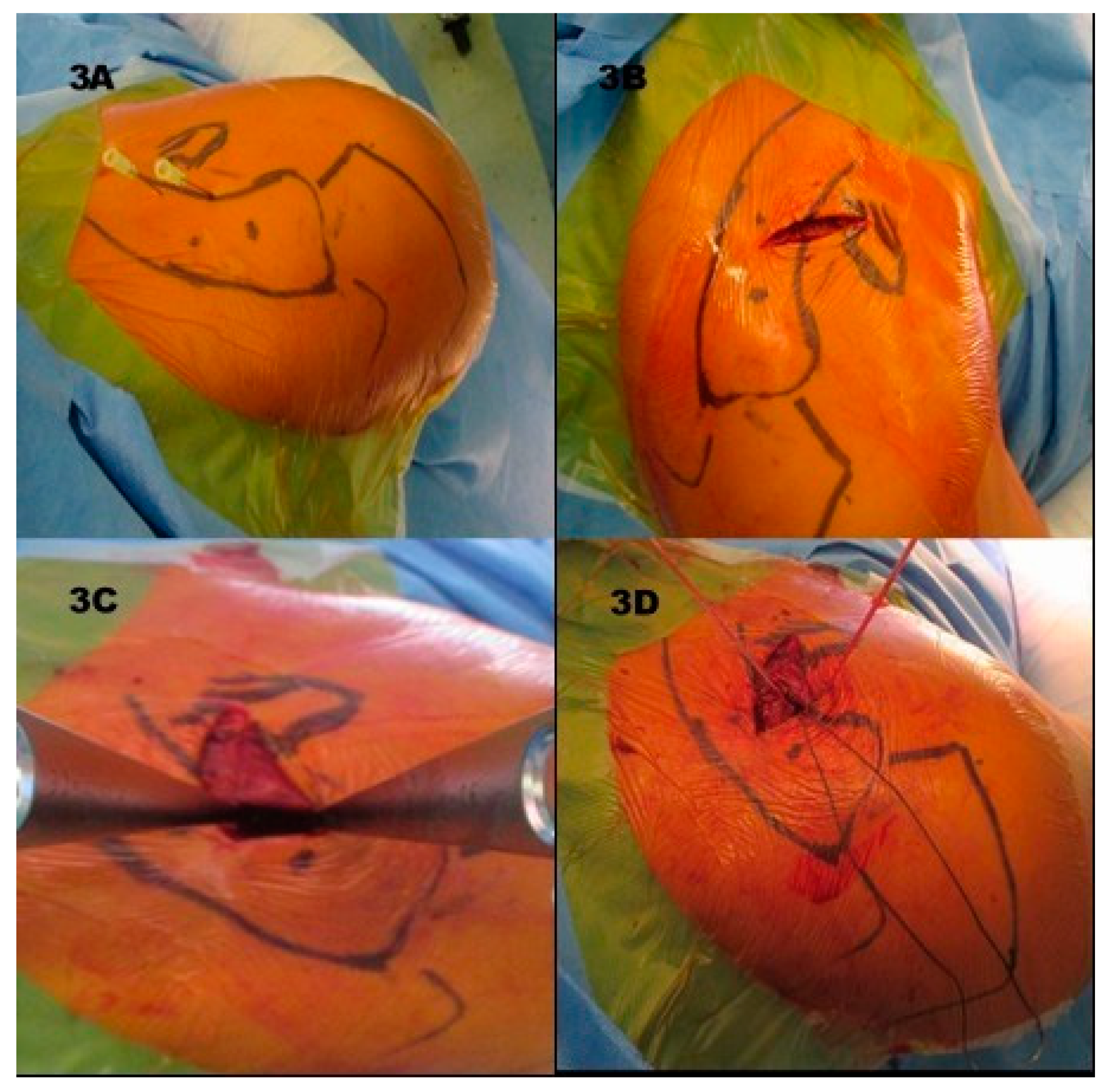
2.5. Surgical Technique and Follow-Up Treatment
3. Results
3.1. Functional Results and Horizontal Instability
3.2. Influencing Factors on Outcome
3.3. Radiological Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wang, G.; Xie, R.; Mao, T.; Xing, S. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J. Orthop. Surg. Res. 2018, 13, 1–7. [Google Scholar] [CrossRef]
- Wellmann, M.; Smith, T. Epidemiology, anatomy, biomechanics and imaging of acromioclavicular joint injuries. Unfallchirurg 2012, 115, 867–871. [Google Scholar] [CrossRef]
- Braun, S.; Imhoff, A.B.; Martenschläger, F. Arthroskopisch gestützte Techniken zur Versorgung der akuten und chronischen AC-Gelenk-Verletzung. Unfallchirurg 2015, 118, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Mikek, M. Long-Term Shoulder Function After Type I and II Acromioclavicular Joint Disruption. Am. J. Sports Med. 2008, 36, 2147–2150. [Google Scholar] [CrossRef] [PubMed]
- Abel, J.; Zumstein, M.A.; Bollinger, L.; Schär, M. Aktuelle Aspekte und neue Techniken bei Schultereckgelenksprengung. Orthopade 2018, 47, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Tamaoki, M.; Belloti, J.; Lenza, M.; Matsumoto, M.; Gomes dos Santos, J.; Faloppa, F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst. Rev. 2011, 8, CD007429. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; Rizzello, G. Surgical versus conservative management of Type III acromioclavicular dislocation: A systematic review. Br. Med. Bull. 2017, 122, 31–49. [Google Scholar] [CrossRef]
- Trainer, G.; Arciero, R.A.; Mazzocca, A.D. Practical Management of Grade III Acromioclavicular Separations. Clin. J. Sport. Med. 2008, 18, 162–166. [Google Scholar] [CrossRef]
- Gstettner, C.; Tauber, M.; Hitzl, W.; Resch, H. Rockwood type III acromioclavicular dislocation: Surgical versus conservative treatment. J. Shoulder Elb. Surg. 2008, 17, 220–225. [Google Scholar] [CrossRef]
- Beitze, K.; Mazzocca, A.D.; Bak, K.; Itoi, E.; Kibler, W.B.; Mirzayan, R.; Imhoff, A.B.; Calvo, E.; Arce, G.; Shea, K.; et al. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy 2014, 30, 271–278. [Google Scholar] [CrossRef]
- Tauber, M.; Koller, H.; Hitzl, W.; Resch, H. Dynamic Radiologic Evaluation of Horizontal Instability in Acute Acromioclavicular Joint Dislocations. Am. J. Sports Med. 2010, 38, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Zumstein, M.A.; Schiessl, P.; Ambuehl, B.; Bolliger, L.; Weihs, J.; Maurer, M.H.; Moor, B.K.; Schaer, M.; Raniga, S. New quantitative radiographic parameters for vertical and horizontal instability in acromioclavicular joint dislocations. Knee Surg. Sport Traumatol. Arthrosc. 2018, 26, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Helfen, T.; Siebenbürger, G.; Ockert, B.; Haasters, F. Therapy of acute acromioclavicular joint instability. Meta-analysis of arthroscopic/minimally invasive versus open procedures. Unfallchirurg 2015, 118, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Scheibel, M.; Dröschel, S.; Gerhardt, C.; Kraus, N. Arthroscopically Assisted Stabilization of Acute High-Grade Acromioclavicular Joint Separations. Am. J. Sports Med. 2011, 39, 1507–1516. [Google Scholar] [CrossRef]
- Saier, T.; Venjakob, A.J.; Minzlaff, P.; Fo, P. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: A biomechanical study. Knee Surg. Sport Traumatol. Arthrosc. 2015, 23, 1498–1505. [Google Scholar] [CrossRef]
- Debski, R.; Parsons, I., 4th; Woo, S.; Fu, F. Effect of Capsular Injury on Acromioclavicular Joint Mechanics. J. Bone Jt. Surg. 2001, 83, 1344–1351. [Google Scholar] [CrossRef]
- Hann, C.; Kraus, N.; Minkus, M.; Maziak, N.; Scheibel, M. Combined arthroscopically assisted coraco—And acromioclavicular stabilization of acute high—Grade acromioclavicular joint separations. Knee Surg. Sport Traumatol. Arthrosc. 2018, 26, 212–220. [Google Scholar] [CrossRef]
- Markel, J.; Schwarting, T.; Malcherczyk, D.; Peterlein, C.; Ruchholtz, S. Concomitant glenohumeral pathologies in high-grade acromioclavicular separation (type III–V). BMC Musculoskelet. Disord. 2017, 18, 1–5. [Google Scholar] [CrossRef]
- Pauly, S.; Gerhardt, C.; Haas, N.P.; Scheibel, M. Prevalence of concomitant intraarticular lesions in patients treated operatively for high-grade acromioclavicular joint separations. Knee Surg. Sport Traumatol. Arthrosc. 2009, 17, 513–517. [Google Scholar] [CrossRef]
- Tischer, T.; Salzmann, G.M.; El-azab, H.; Vogt, S.; Imhoff, A.B. Incidence of Associated Injuries with Acute Acromioclavicular Joint Dislocations Types III Through V. Am. J. Sports Med. 2009, 37, 136–139. [Google Scholar] [CrossRef]
- Flint, J.H.; Wade, A.M.; Giuliani, J.; Rue, J. Defining the Terms Acute and Chronic in Orthopaedic Sports Injuries: A Systematic Review. Am. J. Sports Med. 2013, 42, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Jobe, F.; Jobe, C. Painful athletic injuries of the shoulder. Clin. Orthop. Relat. Res. 1983, 173, 117–124. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Cvetanovich, G.L.; Kupfer, N.; Wimmer, M.A.; Verma, N.N.; Cole, B.J.; Romeo, A.A.; Nicholson, G.P. The champagne toast position isolates the supraspinatus better than the Jobe test: An electromyographic study of shoulder physical examination tests. J. Shoulder Elb. Surg. 2016, 25, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Hertel, R.; Ballmer, F.T.; Lambert, S.M.; Gerber, C. Lag signs in the diagnosis of rotator cuff rupture. J. Shoulder Elb. Surg. 1996, 5, 307–313. [Google Scholar] [CrossRef]
- Patte, D.; Goutallier, D. Extensive anterior release in the painful shoulder caused by anterior impingement. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1988, 74, 306–311. [Google Scholar] [PubMed]
- Gerber, C.; Krushell, R. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J. Bone Jt. Surg. Br. 1991, 73, 389–394. [Google Scholar] [CrossRef]
- Gerber, C.; Hersche, O.; Farron, A. Isolated rupture of the subscapularis tendon: Results of operative repair. J. Bone Jt. Surg. Ser. A 1996, 78, 1015–1023. [Google Scholar] [CrossRef]
- Barth, J.R.H.; Burkhart, S.S.; De Beer, J.F. The Bear-Hug Test: A New and Sensitive Test for Diagnosing a Subscapularis Tear. Arthroscopy 2006, 22, 1076–1084. [Google Scholar] [CrossRef]
- O’Brien, S.J.; Pagnani, M.J.; Fealy, S.; McGlynn, S.R.; Wilson, J.B. The active compression test: A new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am. J. Sports Med. 1998, 26, 610–613. [Google Scholar] [CrossRef]
- Ebinger, N.; Magosch, P.; Lichtenberg, S.; Habermeyer, P. A New SLAP Test: The Supine Flexion Resistance Test. Arthroscopy 2008, 24, 500–505. [Google Scholar] [CrossRef]
- Yergason, R. Supination sign. J. Bone Jt. Surg. 1931, 13, 160. [Google Scholar]
- Gilcreest, E. Dislocation and elongation of the long head of the biceps brachii: An analysis of 100 cases. Surg. Gynecol. Obs. 1934, 58, 322–339. [Google Scholar]
- Neer, C.I. Impingement Lesions. Clin. Orthop. Relat. Res. 1983, 173, 70–77. [Google Scholar] [CrossRef]
- Hawkins, R.; Kennedy, J. Impingement syndrome in athletes. Am. J. Sports Med. 1980, 8, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Constant, C.; Murley, A. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Hudak, P.; Amadio, P.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Amstutz, H.; Sew Hoy, A.; Clark, I. UCLA anatomic total shoulder arthroplasty. Clin. Orthop. Relat. Res. 1981, 155, 7–20. [Google Scholar] [CrossRef]
- Taft, T.; Wilson, F.; Oglesby, J. Dislocation of the acromioclavicular joint. An end-result study. J. Bone Jt. Surg. Am. Vol. 1987, 69, 1045–1051. [Google Scholar] [CrossRef]
- Bin Abd Razak, H.R.; Yeo, E.N.; Yeo, W.; Lie, T.D. Short-term outcomes of arthroscopic TightRope® fixation are better than hook plate fixation in acute unstable acromioclavicular joint dislocations. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 869–875. [Google Scholar] [CrossRef]
- Athar, M.; Ashwood, N.; Arealis, G.; Hamlet, M.; Salt, E. Acromioclavicular joint disruptions: A comparison of two surgical approaches ‘hook’ and ‘rope’. J. Orthop. Surg. 2018, 26, 1–5. [Google Scholar] [CrossRef]
- Jensen, G.; Christoph, J.; Voigt, C. Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg. Sport Traumatol. Arthrosc. 2014, 22, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Rosslenbroich, S.B.; Schliemann, B.; Schneider, K.N.; Metzlaff, S.L.; Koesters, C.A.; Weimann, A.; Petersen, W.; Raschke, M.J. Minimally Invasive Coracoclavicular Ligament Reconstruction with a Flip-Button Technique (MINAR): Clinical and Radiological Midterm Results. Am. J. Sports Med. 2015, 43, 1751–1757. [Google Scholar] [CrossRef] [PubMed]
- Petersen, W.; Wellmann, M.; Rosslenbroich, S.; Zantop, T. Minimalinvasive Akromioklavikulargelenkrekonstruktion (MINAR). Oper. Orthopädie Traumatol. 2010, 22, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Yin, Z.; Gong, G.; Zhu, C.; Sun, C.; Liu, X. Comparison of hook plate with versus without double-tunnel coracoclavicular ligament reconstruction for repair of acute acromioclavicular joint dislocations: A prospective randomized controlled clinical trial. Int. J. Surg. 2018, 54, 18–23. [Google Scholar] [CrossRef]
- Le, P.V.M.; Cladiere, H.V.; Boyer, P.L.P. A comparison between two double—Button endoscopically assisted surgical techniques for the treatment acute acromioclavicular dislocations. Musculoskelet. Surg. 2018, 102, 73–79. [Google Scholar] [CrossRef]
- Beris, A.; Lykissas, M.; Kostas-agnantis, I.; Vekris, M.; Mitsionis, G. Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury 2013, 44, 288–292. [Google Scholar] [CrossRef]
- Tiefenboeck, T.M.; Boesmueller, S.; Popp, D.; Payr, S.; Joestl, J.; Binder, H.; Schurz, M.; Komjati, M.; Fialka, C.; Ostermann, R.C. The use of the LARS system in the treatment of AC joint instability—Long-term results after a mean of 7.4 years. Orthop. Traumatol. Surg. Res. 2018, 104, 749–754. [Google Scholar] [CrossRef]
- Lu, N.; Zhu, L.; Ye, T.; Chen, A. Evaluation of the coracoclavicular reconstruction using LARS artificial ligament in acute acromioclavicular joint dislocation. Knee Surg. Sport Traumatol. Arthrosc. 2014, 22, 2223–2227. [Google Scholar] [CrossRef]
- Gerhardt, C.; Kraus, N.; Greiner, S.; Scheibel, M. Arthroskopische Stabilisierung der akuten Schultereckgelenksprengung. Orthopade 2011, 40, 61–69. [Google Scholar] [CrossRef]
- Dimakopoulos, P.; Panagopoulos, A.; Syggelos, S.A.; Panagiotopoulos, E.; Lambiris, E. Double-Loop Suture Repair for Acute Acromioclavicular Joint Disruption. Am. J. Sports Med. 2006, 34, 1112–1119. [Google Scholar] [CrossRef]
- Cano-Martínez, J.A.; Nicolás-Serrano, G.; Bento-Gerard, J.; Picazo-Marín, F.; Andrés-Grau, J. Acute high-grade acromioclavicular dislocations treated with triple button device (MINAR): Preliminary results. Injury 2016, 47, 2512–2519. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | |
|---|---|
| Age (y) | 43 (19–63) * |
| Sex (m/f) | 62/3 |
| Rockwood Type | Type III n = 8 (16%) |
| Type IV n = 11 (21%) | |
| Type V n = 32 (63%) | |
| Time to surgery (d) | 7 (0–21) * |
| Follow up (mo) | 55 (29–90) * |
| Lost to FU | 14 (21.5%) |
| Overhead work | 21/65 (32%) |
| Previous shoulder surgery | none |
| Smoking | 8/65 (12%) |
| Sports (main) | Cycling n = 13 (20%) |
| Hiking n = 11 (17%) | |
| Soccer n = 7 (10%) | |
| Running n = 14 (22%) | |
| Other n = 18 (27%) | |
| None n = 2 (4%) | |
| Comorbidities | Art. Hypertension n = 1 |
| Hypothyreoidism n = 2 | |
| Hypercholesterolemia n = 1 | |
| Functional Outcome (FU) | ||
|---|---|---|
| Score | Value | Reference Value |
| Constant | 95 (±8.8) | 0–100 |
| DASH | 9.1 (±14.3) | 0–10 |
| UCLA | 31 (±4.9) | 100–0 |
| VAS | 0.9 (±0.1) | 1–0 |
| Satisfaction (n/%) | high n = 36 (71%) | |
| moderate n = 14 (27%) | ||
| no n = 1 (2%) | ||
| Radiological Outcome | |||
|---|---|---|---|
| prae OP | post OP | Follow-Up | |
| CC distance (mm) | 23.00 (±5.49) | 9.10 (±3.11) | 11.25 (±3.14) |
| AC distance (mm) | 11.25 (±4.47) | 4.25 (±2.14) | 5.82 (±2.78) |
| AC arthritis (n/%) | n.a. | n.a. | 4/51 (8%) |
| CC ligament calcification (n/%) | n.a. | n.a. | 19/51 (37%) |
| Functional Outcome after Nonrigid AC Joint Repair | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Technique | Number of Patients | Patient Age (y) | Interval Trauma to Surgery (d) | Follow Up (m) | Constant Score | DASH | UCLA |
| Wang et al. (2018) [1] | allogenic Tendon Graft | 8 | 49 (23–72) * | <21 | 29.8 (25–43) | 94.4 (86–100) | n.r. | 33.5 (30–35) |
| Yin et al. (2018) [44] | Tendon Graft (conjoined Tendon Autograft) | 25 | 46.28 (20–68) | 4.86 ± 1.17 | 19.92 ± 2.92 | 89.56 ± 2.80 | n.r. | n.r |
| Hann et al. (2017) [17] | Double TightRope + AC cerclage | 59 | 43.3 (24.4–56) * | <21 | 26.4 (20.3–61) * | 90 (33–100) * | n.r. | n.r |
| Vulliet et al. (2017) [45] | Double Tight Rope | 22 | 38.8 ± 8.7 | 3 ± 1.9 | 27.7 ± 8.3 | 94.3 ± 4.4 | 2.0 ± 2.6 | n.r |
| Beris et al. (2013) [46] | Single TightRope | 12 | 27.5 (19–39) | 5 (2–14) | 18.3 (12–30) | 94.8 (84–100) | 0.25 (0-3) | n.r. |
| Tiefenboeck et al. (2018) [47] | LARS | 47 | 37.3 (17–65) * | 8 (<14) | 90 (25–159) * | 93 (5–100) * | 2.6 (0–31) * | 35 (20–35) * |
| Lu et al. (2013) [48] | LARS | 24 | 31 (21–45) * | <42 | 36 (6–60) * | 94.5 ± 9.3 | n.r. | n.r. |
| Rosslenbroich et al. (2015) [42] | MINAR | 83 | 39 (17–80) * | 6 (0–22) | 39 (12–78) | 94.7 (61–100) | n.r. | n.r. |
| Breuer et al. (2018) | MINAR | 51 | 43 (19–63) | 7 (0–21) | 55 (29–90) * | 95 ±8.8 | 9.1 ± 14.3 | 31 ± 4.9 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Breuer, R.; Unterrainer, A.; Komjati, M.; Tiefenboeck, T.M.; Trieb, K.; Pirkl, C. Minimally Invasive AC Joint Reconstruction System (MINAR®) in Modified Triple-Button Technique for the Treatment of Acute AC Joint Dislocation. J. Clin. Med. 2019, 8, 1683. https://doi.org/10.3390/jcm8101683
Breuer R, Unterrainer A, Komjati M, Tiefenboeck TM, Trieb K, Pirkl C. Minimally Invasive AC Joint Reconstruction System (MINAR®) in Modified Triple-Button Technique for the Treatment of Acute AC Joint Dislocation. Journal of Clinical Medicine. 2019; 8(10):1683. https://doi.org/10.3390/jcm8101683
Chicago/Turabian StyleBreuer, Robert, Alexandra Unterrainer, Micha Komjati, Thomas M. Tiefenboeck, Klemens Trieb, and Christof Pirkl. 2019. "Minimally Invasive AC Joint Reconstruction System (MINAR®) in Modified Triple-Button Technique for the Treatment of Acute AC Joint Dislocation" Journal of Clinical Medicine 8, no. 10: 1683. https://doi.org/10.3390/jcm8101683
APA StyleBreuer, R., Unterrainer, A., Komjati, M., Tiefenboeck, T. M., Trieb, K., & Pirkl, C. (2019). Minimally Invasive AC Joint Reconstruction System (MINAR®) in Modified Triple-Button Technique for the Treatment of Acute AC Joint Dislocation. Journal of Clinical Medicine, 8(10), 1683. https://doi.org/10.3390/jcm8101683






