Geographic Differences in Phenotype and Treatment of Children with Sickle Cell Anemia from the Multinational DOVE Study
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Randomization and Masking
2.3. Statistical Analyses
3. Results
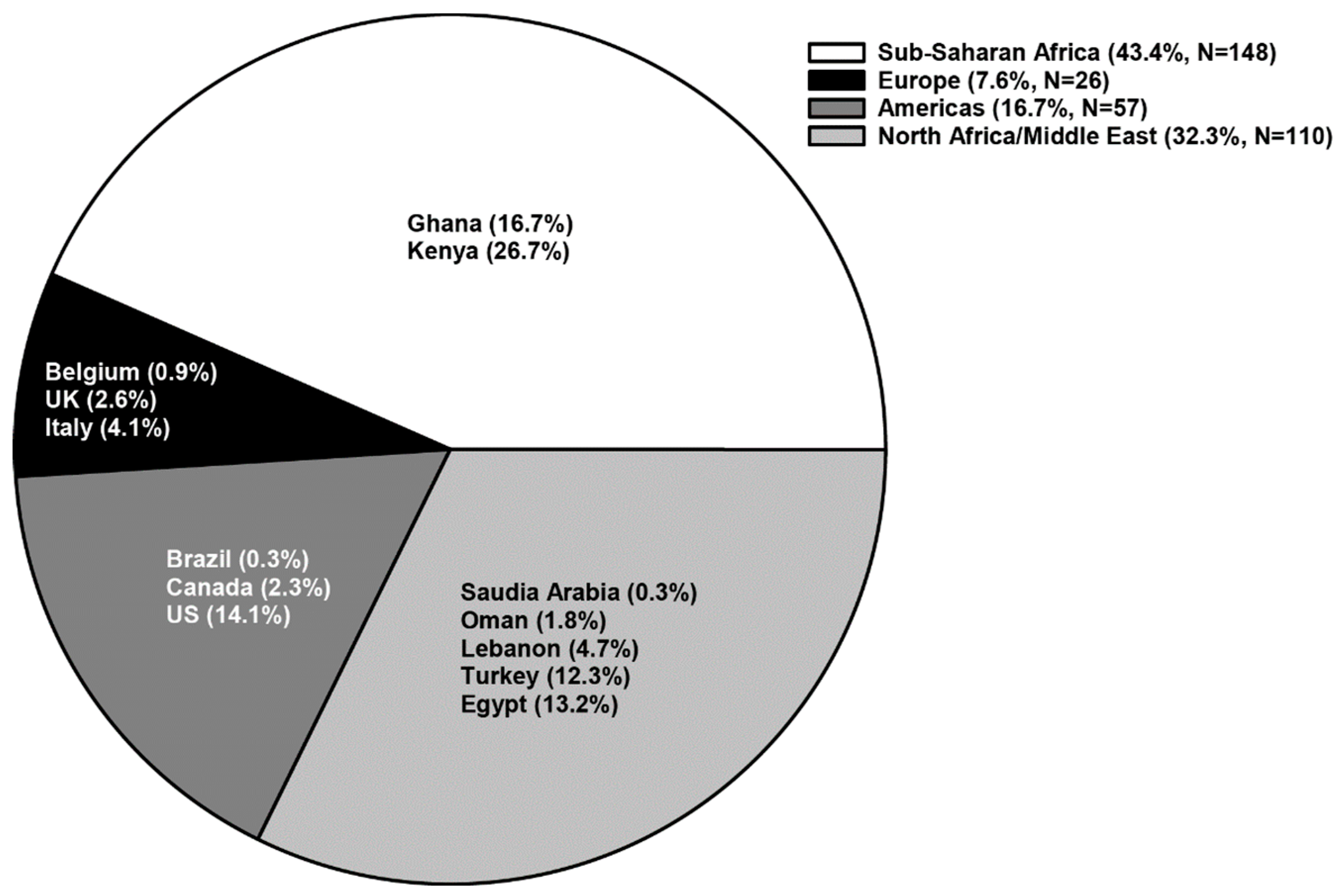
3.1. Demographics of the Study Population
3.2. Medical History and Baseline Clinical Characteristics
3.3. Baseline Laboratory Values
3.4. Vaso-Occlusive Crises during the Study
3.5. Serious Adverse Events during the Study
3.6. Therapeutic Interventions during the Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviation
| ACS | acute chest syndrome |
| BMI | body mass index |
| DOVE | Determining Effects of Platelet Inhibition on Vaso-Occlusive Events |
| HbSβ0 | haemoglobin Sβ (0) thalassemia |
| HbSS | homozygous hemoglobin S |
| HU | hydroxyurea |
| IV | intravenous |
| SAEs | serious adverse events |
| SCA | sickle cell anemia |
| SSA | Sub-Saharan Africa |
| VOCs | vaso-occlusive crisis |
References
- Piel, F.B.; Patil, A.P.; Howes, R.E.; Nyangiri, O.A.; Gething, P.W.; Dewi, M.; Temperley, W.H.; Williams, T.N.; Weatherall, D.J.; Hay, S.I. Global epidemiology of sickle haemoglobin in neonates: A contemporary geostatistical model-based map and population estimates. Lancet 2013, 381, 142–151. [Google Scholar] [CrossRef]
- Platt, O.S.; Thorington, B.D.; Brambilla, D.J.; Milner, P.F.; Rosse, W.F.; Vichinsky, E.; Kinney, T.R. Pain in sickle cell disease. Rates and risk factors. N. Engl. J. Med. 1991, 325, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Inati, A. Recent advances in improving the management of sickle cell disease. Blood Rev. 2009, 23 (Suppl. 1), S9–S13. [Google Scholar] [CrossRef]
- Habara, A.; Steinberg, M.H. Minireview: Genetic basis of heterogeneity and severity in sickle cell disease. Exp. Biol. Med. 2016, 241, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.; Gergen, P.J.; Moore, R.M., Jr. Geographic differences in mortality of young children with sickle cell disease in the United States. Public Health Rep. 1997, 112, 52–58. [Google Scholar] [PubMed]
- Wang, C.J.; Kavanagh, P.L.; Little, A.A.; Holliman, J.B.; Sprinz, P.G. Quality-of-care indicators for children with sickle cell disease. Pediatrics 2011, 128, 484–493. [Google Scholar] [CrossRef]
- Piel, F.B.; Tewari, S.; Brousse, V.; Analitis, A.; Font, A.; Menzel, S.; Chakravorty, S.; Thein, S.L.; Inusa, B.; Telfer, P.; et al. Associations between environmental factors and hospital admissions for sickle cell disease. Haematologica 2017, 102, 666–675. [Google Scholar] [CrossRef]
- Hoppe, C.C.; Styles, L.; Heath, L.E.; Zhou, C.; Jakubowski, J.A.; Winters, K.J.; Brown, P.B.; Rees, D.C.; Heeney, M.M. Design of the DOVE (Determining Effects of Platelet Inhibition on Vaso-Occlusive Events) trial: A global phase 3 double-blind, randomized, placebo-controlled, multicenter study of the efficacy and safety of prasugrel in pediatric patients with sickle cell anemia utilizing a dose titration strategy. Pediatr. Blood Cancer 2016, 63, 299–305. [Google Scholar]
- Heeney, M.M.; Hoppe, C.C.; Abboud, M.R.; Inusa, B.; Kanter, J.; Ogutu, B.; Brown, P.B.; Heath, L.E.; Jakubowski, J.A.; Zhou, C.; et al. A multinational trial of prasugrel for sickle cell vaso-occlusive events. N. Engl. J. Med. 2016, 374, 625–635. [Google Scholar] [CrossRef]
- Quinn, C.T. Minireview: Clinical severity in sickle cell disease: The challenges of definition and prognostication. Exp. Biol. Med. 2016, 241, 679–688. [Google Scholar] [CrossRef]
- Azar, S.; Wong, T.E. Sickle cell disease—A brief update. Med. Clin. North Am. 2017, 101, 375–393. [Google Scholar] [CrossRef] [PubMed]
- Kanter, J.; Heath, L.E.; Knorr, J.; Agbenyega, E.T.; Colombatti, R.; Dampier, C.; Hassab, H.; Manwani, D.; Robitaille, N.; Brown, P.B.; et al. Novel findings from the multinational DOVE study on geographic and age-related differences in pain perception and analgesic usage in children with sickle cell anaemia. Br. J. Haematol. 2019, 184, 1058–1061. [Google Scholar] [CrossRef] [PubMed]
- Rees, D.C.; Williams, T.N.; Gladwin, M.T. Sickle-cell disease. Lancet 2010, 376, 2018–2031. [Google Scholar] [CrossRef]
- Sant’Ana, P.G.; Araujo, A.M.; Pimenta, C.T.; Bezerra, M.L.; Junior, S.P.; Neto, V.M.; Dias, J.S.; Lopes, A.F.; Rios, D.R.; Pinheiro, M.B. Clinical and laboratory profile of patients with sickle cell anemia. Rev. Bras. Hematol. Hemoter. 2017, 39, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.G. The role of infection in the pathogenesis of vaso-occlusive crisis in patients with sickle cell disease. Mediterr. J. Hematol. Infect. Dis. 2011, 3, e2011028. [Google Scholar] [CrossRef] [PubMed]
- Mensah-Brown, H.E.; Abugri, J.; Asante, K.P.; Dwomoh, D.; Dosoo, D.; Atuguba, F.; Conway, D.J.; Awandare, G.A. Assessing the impact of differences in malaria transmission intensity on clinical and haematological indices in children with malaria. Malar. J. 2017, 16, 96. [Google Scholar] [CrossRef]
- Thompson, C.B.; Jakubowski, J.A. The pathophysiology and clinical relevance of platelet heterogeneity. Blood 1988, 72, 1–8. [Google Scholar] [CrossRef]
- Segal, J.B.; Moliterno, A.R. Platelet counts differ by sex, ethnicity, and age in the United States. Ann. Epidemiol. 2006, 16, 123–130. [Google Scholar] [CrossRef]
- Celik, T.; Unal, S.; Ekinci, O.; Ozer, C.; Ilhan, G.; Oktay, G.; Arica, V. Mean platelet volume can predict cerebrovascular events in patients with sickle cell anemia. Pak. J. Med. Sci. 2015, 31, 203–208. [Google Scholar] [CrossRef]
- Machado, N.O.; Grant, C.S.; Alkindi, S.; Daar, S.; Al-Kindy, N.; Al Lamki, Z.; Ganguly, S.S. Splenectomy for haematological disorders: A single center study in 150 patients from Oman. Int. J. Surg. 2009, 7, 476–481. [Google Scholar] [CrossRef]
- Owusu-Ofori, S.; Hirst, C. Splenectomy versus conservative management for acute sequestration crises in people with sickle cell disease. Cochrane Database Syst. Rev. 2013, 31, CD003425. [Google Scholar]
- Al-Salem, A.H. Splenic complications of sickle cell anemia and the role of splenectomy. ISRN Hematol. 2011, 2011, 864257. [Google Scholar] [CrossRef] [PubMed]
- (CDC) Centers for Disease Control and Prevention resource page. About Child and Teen BMI. 2015. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (accessed on 5 October 2018).
- Rodgers, G.P.; Walker, E.C.; Podgor, M.J. Is “relative” hypertension a risk factor for vaso-occlusive complications in sickle cell disease? Am. J. Med. Sci. 1993, 305, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Mohan, J.S.; Marshall, J.M.; Reid, H.L.; Serjeant, G.R. Daily variability in resting levels of cardiovascular variables in normal subjects and those with homozygous sickle cell disease. Clin. Auton. Res. 1995, 5, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Pegelow, C.H.; Colangelo, L.; Steinberg, M.; Wright, E.C.; Smith, J.; Phillips, G.; Vichinsky, E. Natural history of blood pressure in sickle cell disease: Risks for stroke and death associated with relative hypertension in sickle cell anemia. Am. J. Med. 1997, 102, 171–177. [Google Scholar] [CrossRef]
- Banker, A.; Bell, C.; Gupta-Malhotra, G.; Samuels, J. Blood pressure percentile charts to identify high or low blood pressure in children. BMC Pediatr. 2016, 16, 98. [Google Scholar] [CrossRef]
- Singh, P.C.; Ballas, S.K. Emerging drugs for sickle cell anemia. Expert Opin. Emerg. Drugs 2015, 20, 47–61. [Google Scholar] [CrossRef] [Green Version]
- Blood Safety and Availability. 2017. Available online: http://www.who.int/mediacentre/factsheets/fs279/en/ (accessed on 5 October 2018).

| Parameter Assessed | Geographic Regions a | Total (N = 341) | p-Value | |||
|---|---|---|---|---|---|---|
| SSA (N = 148) | Americas (N = 57) | North Africa/Middle East (N = 110) | Europe (N = 26) | |||
| Mean Age in Years (SD) | 9.7 (3.9) | 11.1 (4.2) | 12.0 (4.6) | 8.7 (4.3) | 10.6 (4.3) | 0.020 |
| Age Group (n (%)) | <0.001 | |||||
| 2 to <6 years | 32 (21.6) | 9 (15.8) | 17 (15.5) | 9 (34.6) | 67 (19.6) | |
| 6 to <12 years | 72 (48.6) | 22 (38.6) | 29 (26.4) | 9 (34.6) | 132 (38.7) | |
| 12 to <18 years | 44 (29.7) | 26 (45.6) | 64 (58.2) | 8 (30.8) | 142 (41.6) | |
| Gender (n (%)) | 0.733 | |||||
| Female | 75 (50.7) | 32 (56.1) | 52 (47.3) | 14 (53.8) | 173 (50.7) | |
| Race (n (%)) b | <0.001 | |||||
| White | 0 (0.0) | 1 (1.8) | 110 (100.0) | 5 (19.2) | 116 (34.1) | |
| Black or African American | 148 (100.0) | 54 (96.4) | 0 (0.0) | 20 (76.9) | 222 (65.3) | |
| Multiple | 0 (0.0) | 1 (1.8) | 0 (0.0) | 1 (3.8) | 2 (0.6) | |
| Parameter Assessed | Geographic Regions a | Total (N = 341) | p-Value | |||
|---|---|---|---|---|---|---|
| SSA (N = 148) | Americas (N = 57) | North Africa/Middle East (N = 110) | Europe (N = 26) | |||
| HU Use at Baseline, n (%) | 10 (6.8) | 52 (91.2) | 80 (72.7) | 11 (42.3) | 153 (44.9) | <0.001 |
| BMI (kg/m2), mean (SD) | 15.3 (2.0) | 18.1 (3.5) | 18.3 (3.6) | 16.5 (2.9) | 16.8 (3.2) | <0.001 |
| Blood Pressure, Systolic (mmHg), mean (SD) | 99.0 (9.7) | 108.0 (10.7) | 105.4 (11.7) | 105.6 (12.0) | 103.0 (11.3) | 0.004 |
| Blood Pressure, Diastolic (mmHg), mean (SD) | 58.3 (6.9) | 61.1 (7.3) | 62.9 (9.4) | 60.4 (8.5) | 60.4 (8.2) | 0.003 |
| No. of VOCs in Prior Year, mean (SD) | 3.4 (1.7) | 5.8 (13.5) | 3.2 (1.8) | 3.2 (1.6) | 3.7 (5.8) | 0.041 |
| Diagnosed with ACS Pre-enrollment, n (%) | 9 (6.1) | 38 (66.7) | 20 (18.2) | 9 (34.6) | 76 (22.3) | <0.001 |
| Diagnosed with Splenic Sequestration Pre-enrollment, n (%) | 7 (4.7) | 12 (21.1) | 10 (9.1) | 2 (7.7) | 31 (9.1) | 0.007 |
| Undergone Splenectomy Pre-enrollment, n (%) | 0 (0.0) | 11 (19.3) | 20 (18.2) | 1 (3.8) | 32 (9.4) | <0.001 |
| Parameter Assessed (Mean (SD)) | Geographic Regions a | p-Value | |||
|---|---|---|---|---|---|
| SSA (n = 131) | Americas (n = 4) | North Africa/Middle East (n = 28) | Europe (n = 15) | ||
| Total Bilirubin (µM/L) | 39.2 (27.2) | 24.8 (7.8) | 41.6 (29.6) | 33.8 (8.7) | 0.729 |
| Hemoglobin (mg/L) | 47 (0.6) | 62 (0.8) | 53 (1.0) | 52 (0.5) | <0.001 |
| Lactic Dehydrogenase (units/L) | 569.6 (159.9) | 554.7 (311.3) | 495.3 (216.9) | 519.4 (140.4) | 0.272 |
| Mean Cell Volume (fL) | 84.7 (10.2) | 89.3 (10.8) | 85.4 (11.6) | 85.5 (5.9) | 0.812 |
| Platelet Volume (fL) | 9.0 (0.7) | 10.1 (1.3) | 9.9 (1.4) | 10.1 (1.4) | <0.001 |
| Platelet Count (×109/L) | 440.3 (141.7) | 330.3 (167.8) | 332.2 (176.3) | 331.7 (91.5) | <0.001 |
| Reticulocyte Count (×109/L) | 318.6 (117.8) | 214.8 (75.4) | 238.9 (107.7) | 327.8 (101.1) | 0.004 |
| Leukocyte Count (×109/L) | 15.0 (4.4) | 11.6 (7.3) | 12.7 (6.0) | 14.0 (5.8) | 0.061 |
| Parameter Assessed (n (%)) | Geographic Regions a | ||||
|---|---|---|---|---|---|
| SSA (N = 148) | Americas (N = 57) | North Africa/Middle East (N = 110) | EuropeZ (N = 26) | Total (N = 341) | |
| Total Number of VOCs | 296 | 200 | 226 | 96 | 818 |
| Location of Medical Intervention b | |||||
| VOCs managed by outpatient hospital visit | 201 (67.9) | 10 (5.0) | 44 (19.5) | 6 (6.3) | 261 (31.9) |
| VOCs managed by inpatient hospital visit | 71 (24.0) | 89 (44.5) | 75 (33.2) | 53 (55.2) | 288 (35.2) |
| VOCs managed by home support visits c | 10 (3.4) | 18 (9.5) | 1 (0.5) | 16 (18.4) | 45 (5.7) |
| VOCs managed by telephone consultation c | 5 (1.7) | 52 (27.4) | 46 (21.1) | 5 (5.7) | 108 (13.8) |
| VOCs managed by emergency room visit | 9 (3.0) | 24 (12.0) | 58 (25.7) | 16 (16.7) | 107 (13.1) |
| Types of Medical Intervention | |||||
| VOCs requiring analgesics | 295 (99.7) | 199 (99.5) | 224 (99.1) | 96 (100.0) | 814 (99.5) |
| VOCs requiring IV fluids | 136 (45.9) | 113 (56.5) | 150 (66.4) | 46 (47.9) | 445 (54.4) |
| VOCs requiring transfusion | 19 (6.4) | 20 (10.0) | 42 (18.6) | 18 (18.8) | 99 (12.1) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inusa, B.P.D.; Colombatti, R.; Rees, D.C.; Heeney, M.M.; Hoppe, C.C.; Ogutu, B.; Hassab, H.M.; Zhou, C.; Yao, S.; Brown, P.B.; et al. Geographic Differences in Phenotype and Treatment of Children with Sickle Cell Anemia from the Multinational DOVE Study. J. Clin. Med. 2019, 8, 2009. https://doi.org/10.3390/jcm8112009
Inusa BPD, Colombatti R, Rees DC, Heeney MM, Hoppe CC, Ogutu B, Hassab HM, Zhou C, Yao S, Brown PB, et al. Geographic Differences in Phenotype and Treatment of Children with Sickle Cell Anemia from the Multinational DOVE Study. Journal of Clinical Medicine. 2019; 8(11):2009. https://doi.org/10.3390/jcm8112009
Chicago/Turabian StyleInusa, Baba Psalm Duniya, Raffaella Colombatti, David C. Rees, Matthew M. Heeney, Carolyn C. Hoppe, Bernhards Ogutu, Hoda M. Hassab, Chunmei Zhou, Suqin Yao, Patricia B. Brown, and et al. 2019. "Geographic Differences in Phenotype and Treatment of Children with Sickle Cell Anemia from the Multinational DOVE Study" Journal of Clinical Medicine 8, no. 11: 2009. https://doi.org/10.3390/jcm8112009
APA StyleInusa, B. P. D., Colombatti, R., Rees, D. C., Heeney, M. M., Hoppe, C. C., Ogutu, B., Hassab, H. M., Zhou, C., Yao, S., Brown, P. B., Heath, L. E., Jakubowski, J. A., & Abboud, M. R. (2019). Geographic Differences in Phenotype and Treatment of Children with Sickle Cell Anemia from the Multinational DOVE Study. Journal of Clinical Medicine, 8(11), 2009. https://doi.org/10.3390/jcm8112009





