Evaluation of Patellar Contact Pressure Changes after Static versus Dynamic Medial Patellofemoral Ligament Reconstructions Using a Finite Element Model
Abstract
:1. Introduction
2. Methods
2.1. Parametric FE Model of the PFJ
2.2. MPFLr Techniques
2.3. Simulation of the Different Surgical Techniques
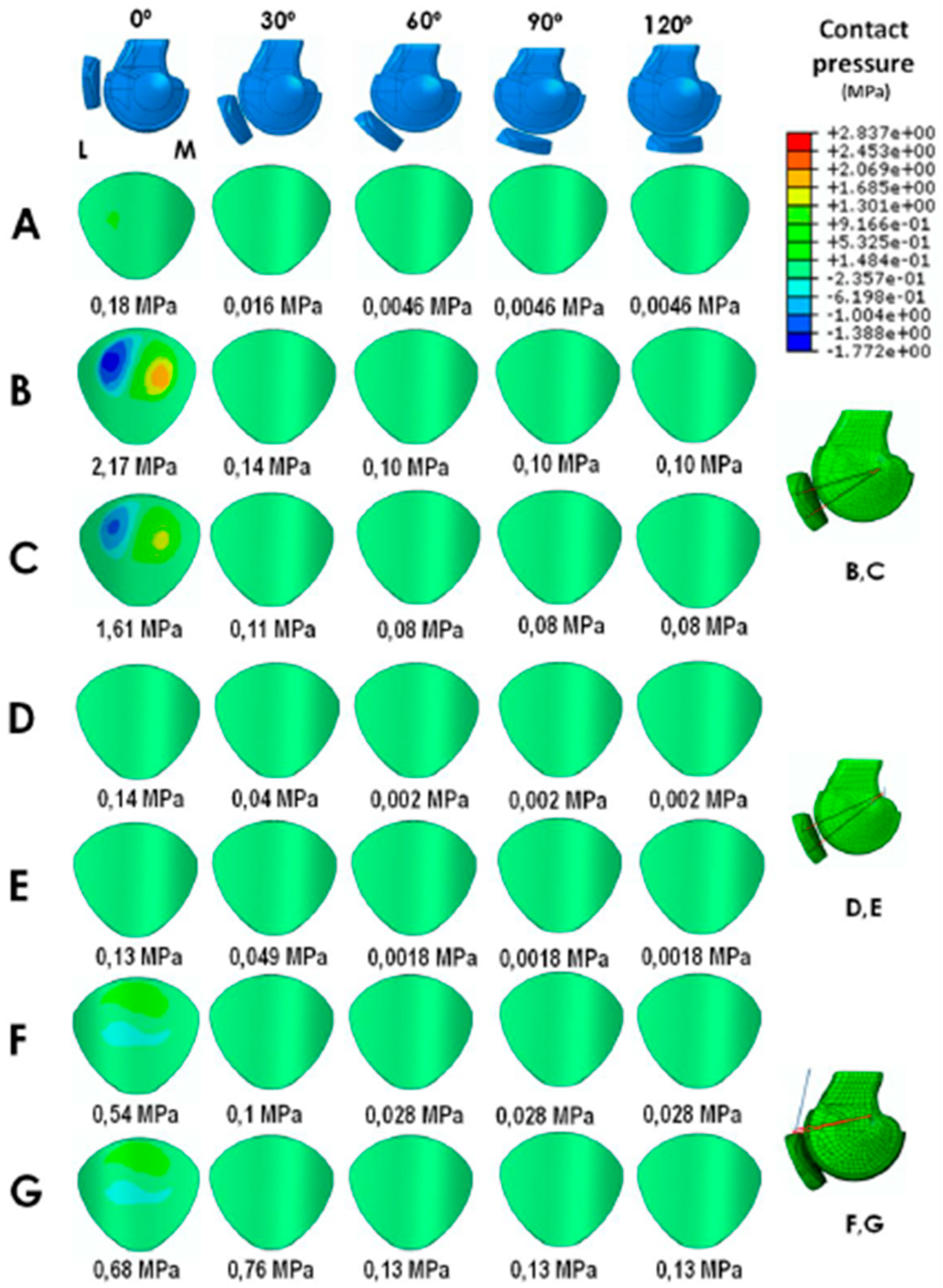
3. Results
3.1. Static Anatomical Technique
3.2. Dynamic MPFLr Techniques
4. Discussion
4.1. Clinical Relevance
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sanchis-Alfonso, V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J. Am. Acad. Orthop. Surg. 2014, 22, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Alfonso, V. How to deal with chronic patellar instability: What does the literature tell us? Sports Health 2016, 8, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Gravesen, K.S.; Kallemose, T.; Blønd, L.; Troelsen, A.; Barfod, K.W. Persistent morbidity after medial patellofemoral ligament reconstruction—A registry study with an eight-year follow-up on a nationwide cohort from 1996 to 2014. Knee 2018. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Berton, A.; Salvatore, G.; Migliorini, F.; Ciuffreda, M.; Nazarian, A.; Denaro, V. Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: Current indications, outcomes, and complications. Arthroscopy 2016, 32, 1421–1427. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.M.; Krych, A.J.; Johnson, N.R.; Mohan, R.; Stuart, M.J.; Dahm, D.L. Combined tibial tubercle osteotomy and medial patellofemoral ligament reconstruction for recurrent lateral patellar instability in patients with multiple anatomic risk factors. Arthroscopy 2018, 34, 2420–2426. [Google Scholar] [CrossRef]
- Nelitz, M.; Williams, S.R. Combined trochleoplasty and medial patellofemoral ligament reconstruction for patellofemoral instability. Oper. Orthop. Traumatol. 2015, 27, 495–504. [Google Scholar] [CrossRef]
- Arendt, E.A. MPFL reconstruction: The adductor sling approach. In Patellofemoral Pain, Instability, and Arthritis; Zaffagnini, S., Dejour, D., Arendt, E.A., Eds.; Springer: Berlin, Germany, 2010; pp. 175–179. [Google Scholar]
- Monllau, J.C.; Masferrer-Pino, A.; Ginovart, G.; Pérez-Prieto, D.; Gelber, P.E.; Sanchis-Alfonso, V. Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2453–2459. [Google Scholar] [CrossRef]
- Pérez-Prieto, D.; Capurro, B.; Gelber, P.E.; Ginovart, G.; Reina, F.; Sanchis-Alfonso, V.; Monllau, J.C. The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2420–2423. [Google Scholar] [CrossRef]
- Alm, L.; Krause, M.; Mull, C.; Frosch, K.H.; Akoto, R. Modified adductor sling technique: A surgical therapy for patellar instability in skeletally immature patients. Knee 2017, 24, 1282–1288. [Google Scholar] [CrossRef]
- Lind, M.; Enderlein, D.; Nielsen, T.; Christiansen, S.E.; Faunø, P. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 666–761. [Google Scholar] [CrossRef]
- Fulkerson, J.P.; Edgar, C. Medial quadriceps tendon-femoral ligament: Surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc. Tech. 2013, 12, e125–e128. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Alfonso, V.; Ramirez-Fuentes, C.; Montesinos-Berry, E.; Domenech, J.; Martí-Bonmatí, L. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2433–2441. [Google Scholar] [CrossRef] [PubMed]
- Smirk, C.; Morris, H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee 2003, 10, 221–227. [Google Scholar] [CrossRef]
- Beck, P.; Brown, N.A.; Greis, P.E.; Burks, R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am. J. Sports Med. 2007, 35, 1557–1563. [Google Scholar] [CrossRef]
- Stephen, J.M.; Kaider, D.; Lumpaopong, P.; Deehan, D.J.; Amis, A.A. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am. J. Sports Med. 2014, 42, 364–372. [Google Scholar] [CrossRef]
- Lorbach, O.; Zumbansen, N.; Kieb, M.; Efe, T.; Pizanis, A.; Kohn, D.; Haupert, A. Medial patello femoral ligament reconstruction: Impact of knee flexion angle dring graft fixation on dynamic patellofemoral contact pressure—a biomechanical study. Arthroscopy 2018, 34, 1072–1082. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Alastruey-López, D.; Ginovart, G.; Montesinos-Berry, E.; García-Castro, F.; Ramírez-Fuentes, C.; Monllau, J.C.; Alberich-Bayarri, A.; Pérez, M.A. Parametric finite element model of medial patellofemoral ligament reconstruction. Model development and clinical validation. J. Exp. Orthop. 2019, 6, 32. [Google Scholar] [CrossRef]
- Elías, J.J.; Cech, J.A.; Weinstein, D.M.; Cosgrea, A.J. Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am. J. Sports Med. 2005, 32, 1202–1208. [Google Scholar] [CrossRef]
- Elías, J.J.; Bratton, D.R.; Weinstein, D.M.; Cosgarea, A.J. Comparing two estimations of the quadriceps force distribution for use during patellofemoral simulation. J. Biomech. 2006, 39, 865–872. [Google Scholar] [CrossRef]
- Elias, J.J.; Cosgarea, A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: A computational analysis. Am. J. Sports Med. 2006, 34, 1478–1485. [Google Scholar] [CrossRef]
- Shah, K.S.; Saranathan, A.; Koya, B.; Elias, J.J. Finite element analysis to characterize how varying patellar loading influences pressure applied to cartilage: Model evaluation. Comput. Methods Biomech. Biomed. Eng. 2015, 18, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.A.; Duchman, K.R.; Grosland, N.M.; Bollier, M.J. Finite element analysis of patella alta: A patellofemoral instability model. Iowa Orthop. J. 2017, 37, 101–108. [Google Scholar] [PubMed]
- Watson, N.A.; Duchman, K.R.; Bollier, M.J.; Grosland, N.M. A finite element analysis of medial patellofemoral ligament reconstruction. Iowa Orthop. J. 2015, 35, 13–19. [Google Scholar]
- Cohen, Z.A.; Mow, V.C.; Henry, J.H.; Levine, W.N.; Ateshian, G.A. Templates of the cartilage layers of the patellofemoral joint and their use in the assessment of osteoarthritic cartilage damage. Osteoarthr. Cartil. 2003, 11, 569–579. [Google Scholar] [CrossRef]
- Ciccone, W.J., II; Bratton, D.R.; Weinstein, D.M.; Elias, J.J. Viscoelasticity and temperature variations decrease tension and stiffness of hamstring tendon grafts following anterior cruciate ligament reconstruction. J. Bone Jt. Surg. 2006, 88, 1071–1078. [Google Scholar] [CrossRef]
- Drez, D., Jr.; Edwards, T.B.; Williams, C.S. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 2001, 17, 298–306. [Google Scholar] [CrossRef]
- Blankevoort, L.; Huiskes, R. Ligament-bone interaction in a three dimensional model of the knee. J. Biomech. Eng. 1991, 113, 263–269. [Google Scholar] [CrossRef]
- Fernandez, J.; Hunter, P.; Shim, V.; Mithraratne, K. A Subject-Specific Framework to Inform Musculoskeletal Modeling: Outcomes from the IUPS Physiome Project. In Patient-Specific Computational Modeling. Lecture Notes in Computational Vision and Biomechanics; Calvo Lopez, B., Peña, E., Eds.; Springer: Dordrecht, The Netherlands, 2012; Volume 5, pp. 39–60. [Google Scholar]
- Besier, T.F.; Gold, G.E.; Delp, S.L.; Fredericson, M.; Beaupré, G.S. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. J. Orthop. Res. 2008, 26, 1627–1635. [Google Scholar] [CrossRef]
- Rood, A.; Hannink, G.; Lenting, A.; Groenen, K.; Koëter, S.; Verdonschot, N.; van Kampen, A.; Koëter, S.; Verdonschot, N.; van Kampen, A. Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am. J. Sports Med. 2015, 43, 2538–2544. [Google Scholar] [CrossRef]
- Tanaka, M.J.; Voss, A.; Fulkerson, J.P. The anatomic midpoint of the attachment of the medial patellofemoral complex. J. Bone Jt. Surg. 2016, 98, 1199–1205. [Google Scholar] [CrossRef]
- Tanaka, M.J.; Chahla, J.; Farr, J. 2nd Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018. [Google Scholar] [CrossRef]
- Parikh, S.N.; Nathan, S.T.; Wall, E.J.; Eismann, E.A. Complications of medial patellofemoral ligament reconstruction in young patients. Am. J. Sports Med. 2013, 41, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Schiphouwer, L.; Rood, A.; Tigchelaar, S.; Koëter, S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Segal, N.A.; Anderson, D.D.; Iyer, K.S.; Baker, J.; Torner, J.C.; Lynch, J.A.; Felson, D.T.; Lewis, C.E.; Brown, T.D. Baseline articular contact stress levels predict incident symptomatic knee osteoarthritis development in the MOST cohort. J. Orthop. Res. 2009, 27, 1562–1568. [Google Scholar] [CrossRef] [Green Version]
- Seitlinger, G.; Moroder, P.; Fink, C.; Wierer, G. Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction. Knee 2017, 24, 680–685. [Google Scholar] [CrossRef]
- Weinberger, J.M.; Fabricant, P.D.; Taylor, S.A.; Mei, J.Y.; Jones, K.J. Influence of graft source and configuration on revision rate and patient-reported outcomes after MPFL reconstruction: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2511–2519. [Google Scholar] [CrossRef]
- McNeilan, R.J.; Everhart, J.S.; Mescher, P.K.; Abouljoud, M.; Magnussen, R.A.; Flanigan, D.C. Graft choice in isolated medial patellofemoral ligament reconstruction: A systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy 2018, 34, 1340–1354. [Google Scholar] [CrossRef]
- Mountney, J.; Senavongse, W.; Amis, A.A.; Thomas, N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J. Bone Jt. Surg. 2005, 87, 36–40. [Google Scholar] [CrossRef] [Green Version]
- Hamner, D.L.; Brown, C.H., Jr.; Steiner, M.E.; Hecker, A.T.; Hayes, W.C. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: Biomechanical evaluation of the use of multiple strands and tensioning techniques. J. Bone Jt. Surg. 1999, 81, 549–557. [Google Scholar] [CrossRef] [Green Version]
- Klets, O.; Mononen, M.E.; Tanska, P.; Nieminen, M.T.; Korhonen, R.K.; Saarakkala, S. Comparison of different material models of articular cartilage in 3D computational modelling of the knee: Data from the Ostoarthrirtis Initiative (OAI). J. Biomech. 2016, 49, 3891–3900. [Google Scholar] [CrossRef] [Green Version]
- Yang, N.H.; Nayeb-Hashemi, H.; Canavan, P.K.; Vaziri, A. Effect of frontal plane tibiofemoral angle on the stress and strain at the knee cartilage during the stance phase of gait. J. Orthop. Res. 2010, 28, 1539–1547. [Google Scholar] [CrossRef]
- Peña, E.; del Palomar, A.P.; Calvo, B.; Martínez, M.; Doblaré, M. Computational modelling of diarthrodial joints. Physiological, pathological and pos-surgery simulations. Arch. Comput. Methods Eng. 2007, 14, 47–91. [Google Scholar] [CrossRef]
- Mononen, M.; Julkunen, P.; Töyräs, J.; Jurvelin, J.; Kiviranta, I.; Korhonen, R. Alterations in structure and properties of collagen network of osteoarthritic and repaired cartilage modify knee joint stresses. Biomech. Model. Mechanobiol. 2011, 10, 357–369. [Google Scholar] [CrossRef]
- Donahue, T.L.H.; Hull, M.; Rashid, M.M.; Jacobs, C.R. A finite element model of the human knee joint for the study of tibio-femoral contact. J. Biomech. Eng. 2002, 124, 273–280. [Google Scholar] [CrossRef]

| Material Properties | ||
|---|---|---|
| Stiffness (N/mm) | Poisson Ratio | |
| Quadriceps Tendon (QT) | 1350 | 0.3 |
| Patellar Tendon (PT) | 2000 | 0.3 |
| Lateral Retinaculum (LR) | 2 | 0.3 |
| Native Medial Patellofemoral Ligament (MPFL) | 12 | 0.3 |
| MPFL Reconstruction (Semitendinosus Autograft) | 100 | 0.3 |
| MPFL Reconstruction (Gracilis Autograft) | 80 | 0.3 |
| MQTFL Reconstruction (Semitendinosus Autograft) | 100 | 0.3 |
| MQTFL Reconstruction (Posterior Tibial Allograft) | 513 | 0.3 |
| Anatomic MPFLr (STATIC) | MPFLr Using the AMT as a Pulley (Superior Bundle) (DYNAMIC) | MPFLr Using the AMT as a Pulley (Inferior Bundle) (DYNAMIC) | MQFTLr (DYNAMIC) | |
|---|---|---|---|---|
| Flexion Angle (°) | Length (mm) | Length (mm) | Length (mm) | Length (mm) |
| 0 | 60.2 + | 61.1 + | 58.3 + | 65 + |
| 30 | 57.9 + | 60.9 + | 60.1 + | 63 + |
| 40 | 57.7 | 60.8 | 60.8 | 62.7 |
| 60 | 57.3 * | 60.7 * | 62.1 * | 62 * |
| 90 | 55.6 * | 60.4 * | 62.2 * | 62 * |
| 120 | 50.7 * | 55.8 * | 57 * | 62 * |
| Ligament Status | Flexion Angle (°) | Maximum MPFL Stress (MPa) | Maximum LR Stress (MPa) |
|---|---|---|---|
| INTACT MPFL | 0 | 8.85 | 1.52 |
| 30 | 0.78 | 0.15 | |
| ANATOMIC MPFLr Semitendinosus autograft | 0 | 74.72 | 1.51 |
| 30 | 6.55 | 0.14 | |
| ANATOMIC MPFLr Gracilis autograft | 0 | 58.78 | 1.51 |
| 30 | 5.12 | 0.14 | |
| MPFLr with AMT as a Pulley Semitendinosus autograft | 0 | 7.11 | 0.15 |
| 30 | 2.53 | 0.05 | |
| MPFLr with AMT as a Pulley Gracilis autograft | 0 | 6.35 | 0.15 |
| 30 | 2.10 | 0.05 | |
| MQTFLr Semitendinosus autograft | 0 | 66.70 | 1.42 |
| 30 | 9.36 | 0.23 | |
| MQTFLr Posterior Tibial allograft | 0 | 100.80 | 1.42 |
| 30 | 49.76 | 0.23 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanchis-Alfonso, V.; Ginovart, G.; Alastruey-López, D.; Montesinos-Berry, E.; Monllau, J.C.; Alberich-Bayarri, A.; Pérez, M.A. Evaluation of Patellar Contact Pressure Changes after Static versus Dynamic Medial Patellofemoral Ligament Reconstructions Using a Finite Element Model. J. Clin. Med. 2019, 8, 2093. https://doi.org/10.3390/jcm8122093
Sanchis-Alfonso V, Ginovart G, Alastruey-López D, Montesinos-Berry E, Monllau JC, Alberich-Bayarri A, Pérez MA. Evaluation of Patellar Contact Pressure Changes after Static versus Dynamic Medial Patellofemoral Ligament Reconstructions Using a Finite Element Model. Journal of Clinical Medicine. 2019; 8(12):2093. https://doi.org/10.3390/jcm8122093
Chicago/Turabian StyleSanchis-Alfonso, Vicente, Gerard Ginovart, Diego Alastruey-López, Erik Montesinos-Berry, Joan Carles Monllau, Angel Alberich-Bayarri, and María Angeles Pérez. 2019. "Evaluation of Patellar Contact Pressure Changes after Static versus Dynamic Medial Patellofemoral Ligament Reconstructions Using a Finite Element Model" Journal of Clinical Medicine 8, no. 12: 2093. https://doi.org/10.3390/jcm8122093





