Effects of a Combined Community Exercise Program in Obstructive Sleep Apnea Syndrome: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Experimental Section
2.1. Participants
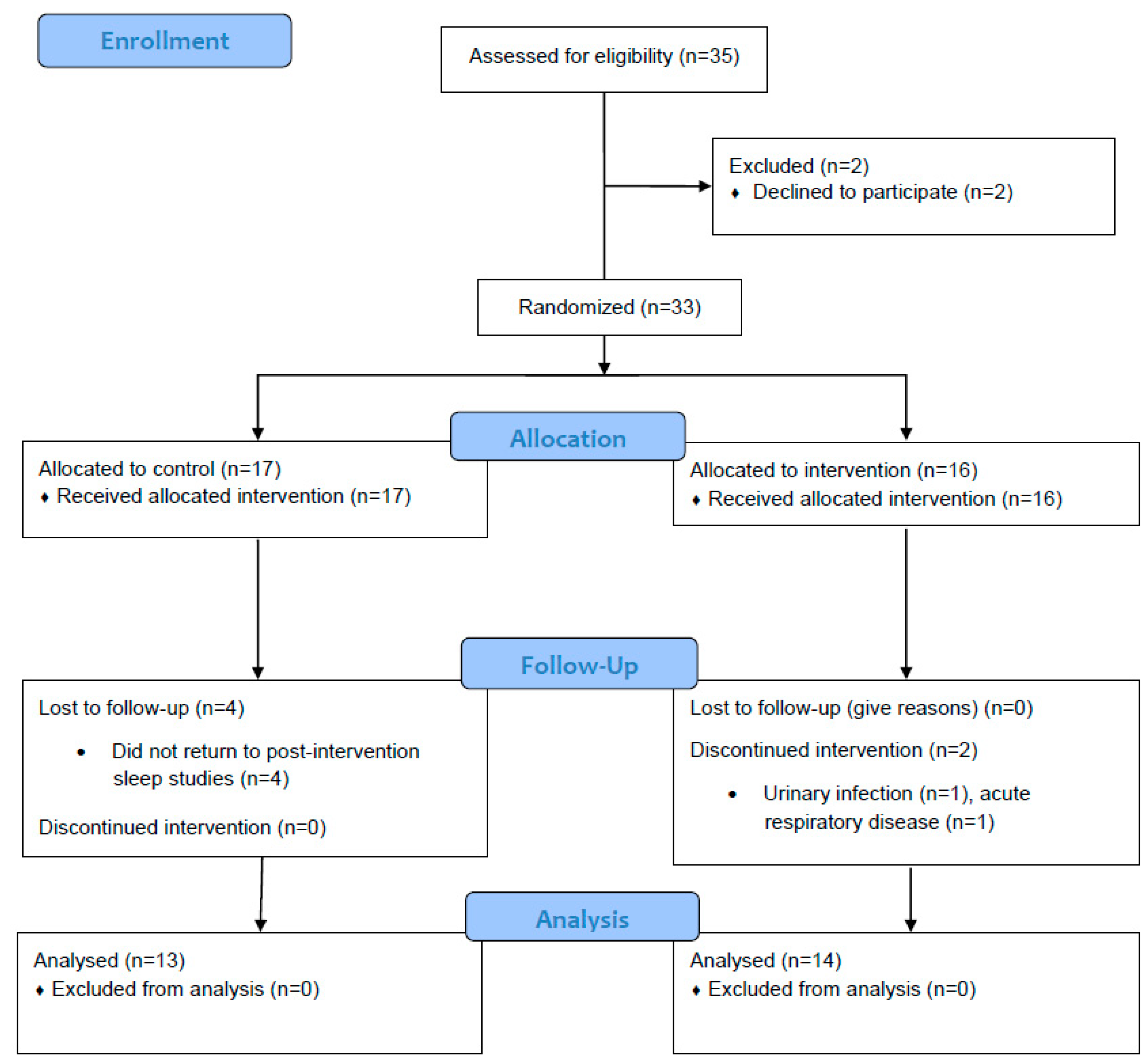
2.2. Study Design
2.3. Intervention
2.4. Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sánchez-de-la-Torre, M.; Campos-Rodríguez, F.; Barbé, F. Obstructive sleep apnoea and cardiovascular disease. LANCET Respir. Med. 2013, 1, 61–72. [Google Scholar] [CrossRef]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Farré, N.; Farré, R.; Gozal, D. Sleep apnea morbidity: A consequence of microbial-Inmune cross-talk? Chest 2018, 154, 754–759. [Google Scholar] [CrossRef]
- McEvoy, R.D.; Antic, N.A.; Heeley, E.; Luo, Y.; Ou, Q.; Zhang, X.; Mediano, O.; Chen, R.; Drager, L.F.; Liu, Z.; et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N. Engl. J. Med. 2016, 375, 919–931. [Google Scholar] [CrossRef]
- Epstein, L.J.; Kristo, D.; Strollo, P.J., Jr.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar] [PubMed]
- Toraldo, D.M.; Passali, D.; Sanna, A.; De Nuccio, F.; Conte, L.; De Benedetto, M. Cost-effectiveness strategies in OSAS management: A short review. Acta Otorhinolaryngol. Ital. 2017, 37, 447–453. [Google Scholar] [PubMed]
- Torres, G.; Turino, C.; Sapiña, E.; Sánchez-de-la-Torre, M.; Barbé, F. Sleep Apnea and Cardiovascular Morbidity—A Perspective. Curr. Sleep Med. Rep. 2018, 4, 79–87. [Google Scholar] [CrossRef]
- Strohl, K.P.; Brown, D.B.; Collop, N.; George, C.; Grunstein, R.; Han, F.; Kline, L.; Malhotra, A.; Pack, A.; Phillips, B.; et al. An official American Thoracic Society Clinical Practice Guideline: Sleep apnea, sleepiness, and driving risk in noncommercial drivers. An update of a 1994 Statement. Am. J. Respir. Crit. Care Med. 2013, 187, 1259–1266. [Google Scholar] [CrossRef]
- Kline, C.E.; Crowley, E.P.; Ewing, G.B.; Burch, J.B.; Blair, S.N.; Durstine, J.L.; Davis, J.M.; Youngstedt, S.D. The effect of exercise training on obstructive sleep apnea and sleep quality: A randomized controlled trial. Sleep 2011, 34, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Desplan, M.; Mercier, J.; Sabaté, M.; Ninot, G.; Prefaut, C.; Dauvilliers, Y. A comprehensive rehabilitation program improves disease severity in patients with obstructive sleep apnea syndrome: A pilot randomized controlled study. Sleep Med. 2014, 15, 906–912. [Google Scholar] [CrossRef]
- Aiello, K.D.; Caughey, W.G.; Nelluri, B.; Sharma, A.; Mookadam, F.; Mookadam, M. Effect of exercise training on sleep apnea: A systematic review and meta-analysis. Respir. Med. 2016, 116, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Camacho, M.; Chang, E.T.; Neighbors, C.L.P.; Noller, M.W.; Mack, D.; Capasso, R.; Kushida, C.A. Thirty-five alternatives to positive airway pressure therapy for obstructive sleep apnea: An overview of meta-analyses. Expert Rev. Respir. Med. 2018, 12, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.-X.; Jing, Q.; Wang, Y.-W.; Liang, C.; Zhang, W.-M.; Ye, X.-W.; Zhang, J.; Huang, Y.-Q.; Cheng, P. Clinical analysis of pharyngeal musculature and genioglossus exercising to treat obstructive sleep apnea and hypopnea syndrome. J. Zhejiang Univ. Sci. B 2015, 16, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, K.C.; Drager, L.F.; Genta, P.R.; Marcondes, B.F.; Lorenzi-Filho, G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 2009, 179, 962–966. [Google Scholar] [CrossRef]
- Iftikhar, I.H.; Kline, C.E.; Youngstedt, S.D. Effects of exercise training on sleep apnea: A meta-analysis. Lung 2014, 192, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Bailly, S.; Marillier, M.; Flore, P.; Borel, J.C.; Vivodtzev, I.; Doutreleau, S.; Verges, S.; Tamisier, R.; Pépin, J.L. Obstructive Sleep Apnea Syndrome, Objectively Measured Physical Activity and Exercise Training Interventions: A Systematic Review and Meta-Analysis. Front. Neurol. 2018, 9, 73. [Google Scholar] [CrossRef]
- Lindberg, E.; Gislason, T. Clinical review article: Epidemiology of sleep-related obstructive breathing. Sleep Med. Rev. 2000, 4, 411–433. [Google Scholar] [CrossRef] [PubMed]
- Thomasouli, M.A.; Brady, E.M.; Davies, M.J.; Hall, A.P.; Khunti, K.; Morris, D.H; Gray, L.J. The impact of diet and lifestyle management strategies for obstructive sleep apnoea in adults: A systematic review and meta-analysis of randomised controlled trials. Sleep Breath. 2013, 17, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Palta, M.; Dempsey, J.; Skatrud, J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000, 284, 3015–3021. [Google Scholar] [CrossRef]
- Sengul, Y.S.; Ozalevli, S.; Oztura, I.; Itil, O.; Baklan, B. The effect of exercise on obstructive sleep apnea: A randomized and controlled trial. Sleep Breath. 2011, 15, 49–56. [Google Scholar] [CrossRef]
- Redolfi, S.; Yumino, D.; Ruttanaumpawan, P.; Yau, B.; Su, M.C.; Lam, J.; Bradley, T.D. Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am. J. Respir. Crit. Care Med. 2009, 179, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Ieto, V.; Kayamori, F.; Montes, M.I.; Hirata, R.P.; Gregório, M.G.; Alencar, A.M.; Drager, L.F.; Genta, P.R.; Lorenzi-Filho, G. Effects of oropharyngeal exercises on snoring: A randomized trial. Chest 2015, 148, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.F.; Von Essen, S.G.; Fuchs, R.H.; McElligott, M. Exercise training effect on obstructive sleep apnea syndrome. Sleep Res. Online 1999, 3, 121–129. [Google Scholar]
- Barnes, M.; Goldsworthy, U.R.; Cary, B.A.; Hill, C.J. A diet and exercise program to improve clinical outcomes in patients with obstructive sleep apnea—A feasibility study. J. Clin. Sleep Med. 2009, 5, 409–415. [Google Scholar] [PubMed]
- Arbillaga-Etxarri, A.; Torrent-Pallicer, J.; Gimeno-Santos, E.; Barberán-Garcia, A.; Delgado, A.; Balcells, E.; Rodríguez, D.A.; Vilaró, J.; Vall-Casas, P.; Irurtia, A.; et al. Validation of Walking Trails for the Urban TrainingTM of Chronic Obstructive Pulmonary Disease Patients. PLoS ONE 2016, 11, e0146705. [Google Scholar] [CrossRef] [PubMed]
- Burkhead, L.M.; Sapienza, C.M.; Rosenbek, J.C. Strength-training exercise in dysphagia rehabilitation: Principles, procedures, and directions for future research. Dysphagia 2007, 22, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.; Gamaldo, C.; Harding, S.; Brooks, R.; Lloyd, R.; Vaughn, B.; Marcus, C.L. AASM Scoring Manual Version 2.2 Updates-New Sections for Scoring Infant Sleep Staging and Home Sleep Apnea Testing. J. Clin. Sleep Med. 2015, 11, 1253–1254. [Google Scholar] [CrossRef]
- Vilaró, J. Prueba de marcha de 6 minutos. In Manual de procedimientos SEPAR. Procedimientos de evaluación de la función pulmonar -II-; Burgos Rincón, F., Casan Clara, P., Eds.; SEPAR: Mallorca, Spain, 2004; pp. 100–113. [Google Scholar]
- Troosters, T.; Gosselink, R.; Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 1999, 14, 270–274. [Google Scholar] [CrossRef] [Green Version]
- Chiner, E.; Arriero, J.; Signes-Costa, J.; Marco, J.; Fuentes, I. Validation of the Spanish version of the Epworth Sleepiness Scale in patients with a sleep apnea syndrome. Arch. Bronconeumol. 1999, 35, 422–427. [Google Scholar] [CrossRef]
- Catalán, P.; Martínez, A.; Herrejón, A.; Chiner, E.; Martínez-García, M.Á.; Sancho-Chust, J.N.; Peris, R.; Senent, C.; Blanquer, R.; Tomás, J.M. Consistencia interna y validez de la versión española del cuestionario de calidad de vida específico para el síndrome de apneas-hipopneas del sueño Quebec Sleep Questionnaire. Arch. Bronconeumol. 2012, 48, 107–113. (In Spanish) [Google Scholar] [CrossRef]
- Herrero, M.J.; Blanch, J.; Peri, J.M.; De Pablo, J.; Pintor, L.; Bulbena, A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen. Hosp. Psychiat. 2003, 25, 277–283. [Google Scholar] [CrossRef]
- Neumannova, K.; Hobzova, M.; Sova, M.; Prasko, J. Pulmonary rehabilitation and oropharyngeal exercises as an adjunct therapy in obstructive sleep apnea: A randomized controlled trial. Sleep Med. 2018, 52, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.A.; Wellman, A.; Sands, S.A.; Owens, R.; Eckert, D.; White, D.; Malhotra, A. Obstructive sleep apnea in older adults is a distinctly different physiological phenotype. Sleep 2014, 37, 1227A–1236A. [Google Scholar] [CrossRef] [PubMed]
- Saboisky, J.P.; Stashuk, D.W.; Hamilton-Wright, A.; Trinder, J.; Nandedkar, S.; Malhotra, A. Effects of aging on genioglossus motor units in humans. PLoS ONE 2014, 9, e104572. [Google Scholar] [CrossRef]
- Andersen, J.L. Muscle fibre type adaptation in the elderly human muscle. Scand. J. Med. Sci. Sports 2003, 13, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Deley, G.; Kervio, G.; Van Hoecke, J.; Verges, B.; Grassi, B.; Casillas, J.M. Effects of a one-year exercise training program in adults over 70 years old: A study with a control group. Aging Clin. Exp. Res. 2007, 19, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Vlietstra, L.; Hendrickx, W.; Waters, D.L. Exercise interventions in healthy older adults with sarcopenia: A systematic review and meta-analysis. Australas. J. Ageing 2018, 37, 169–183. [Google Scholar] [CrossRef]

| Control (n = 13) | Intervention (n = 14) | p-Value | |
|---|---|---|---|
| Anthropometric data | |||
| Age, years | 67 (53–74.5) | 64.5 (51.8–74) | 0.793 |
| Males, % | 57.1 | 53.8 | |
| Body weight, Kg | 82 (70–87.5) | 86 (80.5–90.5) | 0.116 |
| Height, cm | 166.6 ± 9.3 | 163.8 ± 8.3 | 0.458 |
| BMI, Kg/m2 | 27.1 (25.1–35.9) | 31.3 (27.5–35.0) | 0.375 |
| Neck circumference, cm | 38 (37–41.5) | 40 (37–41.5) | 0.616 |
| Waist circumference, cm | 107 (97–114.5) | 108.5 (102.5–114) | 0.519 |
| Hip circumference, cm | 96 (91.5–107.5) | 97 (93.5–109) | 0.720 |
| Polysomnographic data | |||
| AHI/h | 37 (25.5–43.5) | 30.5 (22.5–41.3) | 0.325 |
| CT90 | 22 (3.5–28.5) | 12 (4–21.3) | 0.239 |
| ODI/h | 34 (29.5–44.5) | 30 (22.3–39.8) | 0.280 |
| Exercise Capacity | |||
| 6MWD, m | 529.8 ± 102.7 | 548.2 ± 83.9 | 0.550 |
| Questionnaires | |||
| ESS | 8 (6.5–11) | 8 (3–13) | 0.756 |
| QSQ | |||
| Total score | 172 (133–186.5) | 180.5 (151.3–200) | 0.430 |
| Daytime Sleepiness | 36 (29.5–37.5) | 38 (29.3–40.3) | 0.488 |
| Diurnal symptoms | 50 (43.5–62) | 59.5 (45–66) | 0.430 |
| Nocturnal symptoms | 35 (26.5–38) | 35 (29.8–42.3) | 0.430 |
| Emotions | 30 (19.5–31) | 27 (21.8–29.3) | 0.375 |
| Social interactions | 23 (17–24) | 23 (21–25) | 0.583 |
| HAD | |||
| Total score | 14 (6–23.5) | 9 (3.8–18.8) | 0.550 |
| Anxiety | 8 (6–12.5) | 6 (2.8–10) | 0.325 |
| Depression | 6 (1–9) | 2.5 (1–8) | 0.720 |
| Intervention Group (n = 14) | Control Group (n = 13) | |||||
|---|---|---|---|---|---|---|
| Baseline | After 8 Weeks | p-Value * | Baseline | After 8 Weeks | p-Value * | |
| Anthropometric data | ||||||
| Body weight, Kg | 86 (80.5–90.5) | 85.3 (77–88.3) | 0.003 | 82 (70–87.5) | 81 (70–86.5) | 0.233 |
| BMI, Kg/m2 | 31.3 (27.5–35) | 30.2 (27.3–34.7) | 0.003 | 27.1 (25.1–35.9) | 27.1 (25.1–35.6) | 0.237 |
| Neck circumference, cm | 40 (37–41.5) | 38.8 (37.4–40.5) | 0.056 | 38 (37–41.5) | 40 (36.3–41.3) | 0.878 |
| Waist circumference, cm | 108.5 (102–114) | 107 (99–113.5) | 0.022 | 107 (97–114.5) | 106 (99.5–115) | 0.791 |
| Hip circumference, cm | 97 (93.5–109) | 98.5 (92.8–108.8) | 0.514 | 96 (91.5–107.5) | 95 (92.3–106) | 0.150 |
| Polysomnographic data | ||||||
| AHI/h | 30.5 (22.5–41.3) | 34.5 (14.5–45) | 0.875 | 37 (25.5–43.5) | 43 (28–46) | 0.529 |
| CT90 | 12 (4–21.3) | 7 (3.8–23.3) | 0.423 | 22 (3.5–28.5) | 13 (5.6–25) | 0.625 |
| ODI/h | 30 (22.3–39.8) | 30.5 (14.8–45.3) | 0.780 | 34 (29.5–44.5) | 38 (25.5–44) | 0.944 |
| Exercise Capacity | ||||||
| 6MWD, m | 548.2 ± 83.9 | 567.1 ± 85.3 | 0.020 | 529.8 ± 102.7 | 519.8 ± 108.0 | 0.249 |
| Questionnaires | ||||||
| ESS | 8 (3–13) | 8 (4–10.3) | 0.634 | 8 (6.5–11) | 7 (6.5–10.5) | 0.500 |
| QSQ | ||||||
| Total score | 180.5 (151–200) | 186 (153.8–201) | 0.572 | 172 (133–186.5) | 176 (130–200) | 0.388 |
| Daytime Sleepiness | 38 (29.3–40.3) | 37 (34.3–40) | 0.422 | 36 (29.5–37.5) | 36 (29.5–39.5) | 0.916 |
| Diurnal symptoms | 59.5 (45–66) | 56 (48.5–61.3) | 0.889 | 50 (43.5–62) | 53 (36.5–63) | 0.937 |
| Nocturnal symptoms | 35 (29.8–42.3) | 39 (32.3–42.5) | 0.170 | 35 (26.5–38) | 35 (30–41.5) | 0.116 |
| Emotions | 27 (21.8–29.3) | 28.5 (24.5–30.5) | 0.169 | 30 (19.5–31) | 30 (19.5–32) | 0.641 |
| Social interactions | 23 (21–25) | 21.5 (18.8–24.3) | 0.431 | 23 (17–24) | 23 (19.5–25.5) | 0.372 |
| HAD | ||||||
| Total score | 9 (3.8–18.8) | 10 (5.8–15.6) | 0.783 | 14 (6–23.5) | 12 (6–24) | 0.350 |
| Anxiety | 6 (2.8–10) | 7.5 (4–9.3) | 0.916 | 8 (6–12.5) | 7 (4.5–12) | 0.126 |
| Depression | 2.5 (1–8) | 3 (1.8–6.5) | 0.587 | 6 (1–9) | 6 (1.5–11.5) | 0.142 |
| Group < 60 years (n = 6) | Group > 60 years (n = 8) | |||||
|---|---|---|---|---|---|---|
| Baseline | After 8 Weeks | p-Value * | Baseline | After 8 Weeks | p-Value * | |
| Anthropometric data | ||||||
| Body weight, kg | 90 (81.3–101.5) | 86.5 (77–100.5) | 0.042 | 84 (71.5–86.8) | 82.6 (71–86.6) | 0.027 |
| BMI, kg/m2 | 33.1 (28.7–37) | 32.1 (27.6–35.9) | 0.043 | 29.6 (25–34) | 29.3 (25–33.4) | 0.028 |
| Neck circumference, cm | 38.5 (35.8–40.3) | 38.8 (35.8–40) | 0.655 | 40.5 (37.8–44.5) | 38.5 (37.6–44.3) | 0.072 |
| Waist circumference, cm | 113 (102.3–125.8) | 113.5 (98.5–123.3) | 0.144 | 108 (100.3–109.8) | 106.5 (100.3–107.8) | 0.088 |
| Hip circumference, cm | 97 (88.8–111) | 92 (87.5–112.5) | 0.414 | 99.5 (95.5–113) | 101 (94.8–110.3) | 0.833 |
| Polysomnographic data | ||||||
| AHI/h | 29.5 (21.8–48.3) | 15.5 (11–34) | 0.028 | 31.5 (21–38.8) | 43.5 (24.8–48) | 0.017 |
| CT90 | 4.5 (3.8–10) | 4 (2.5–11) | 0.498 | 14.5 (11.5–21.8) | 16.5 (6–51) | 0.173 |
| ODI/h | 25 (15–35) | 15.5 (12.5–32.5) | 0.223 | 33 (25.8–43.3) | 41.5 (24.3–46.8) | 0.441 |
| Exercise capacity | ||||||
| 6MWD, m | 585.0 ± 63.0 | 597.8 ± 70.1 | 0.173 | 520.7 ± 90.6 | 544.0 ± 92.7 | 0.036 |
| Questionnaires | ||||||
| ESS | 9 (6.8–19) | 10.5 (4–19.5) | 0.666 | 6.5 (3–11.8) | 7.5 (2.3–8.8) | 0.523 |
| QSQ | ||||||
| Total score | 185.5 (150.8–201) | 171.5 (142.5–194.5) | 0.046 | 177 (136.3–200) | 186.5 (170–201) | 0.069 |
| Daytime Sleepiness | 38.5 (28–40.3) | 37.5 (25.8–40) | 0.074 | 35 (25.8–40.3) | 37 (35–41) | 0.058 |
| Diurnal symptoms | 61 (45–66) | 52 (45.8–62.5) | 0.223 | 56.5 (39.3–65.5) | 58.5 (49–61.8) | 0.233 |
| Nocturnal symptoms | 38 (32.3–44) | 38 (32.3–44.3) | 0.914 | 35 (25.3–38.3) | 40 (32–41.8) | 0.061 |
| Emotions | 26 (21.5–30) | 26.5 (20–30.3) | 0.683 | 27.5 (21.3–29.8) | 30 (26.3–31.5) | 0.040 |
| Social interactions | 23 (19.8–25.5) | 19 (13.8–23.5) | 0.116 | 23 (19–24.8) | 22.5 (20.3–24.8) | 0.526 |
| HAD | ||||||
| Total score | 9.5 (2.8–25) | 11 (7.8–24.3) | 0.236 | 9 (5–16) | 8 (5.3–15) | 1.000 |
| Anxiety | 8 (2–11.8) | 8 (6–11.8) | 0.750 | 5.5 (3.5–9.25) | 5 (4–9) | 0.932 |
| Depression | 1.5 (0.8–11.8) | 3 (1.8–11) | 0.285 | 3.5 (1.3–7) | 3 (1.3–6) | 0.829 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Castro, R.; Vilaró, J.; Martí, J.-D.; Garmendia, O.; Gimeno-Santos, E.; Romano-Andrioni, B.; Embid, C.; Montserrat, J.M. Effects of a Combined Community Exercise Program in Obstructive Sleep Apnea Syndrome: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 361. https://doi.org/10.3390/jcm8030361
Torres-Castro R, Vilaró J, Martí J-D, Garmendia O, Gimeno-Santos E, Romano-Andrioni B, Embid C, Montserrat JM. Effects of a Combined Community Exercise Program in Obstructive Sleep Apnea Syndrome: A Randomized Clinical Trial. Journal of Clinical Medicine. 2019; 8(3):361. https://doi.org/10.3390/jcm8030361
Chicago/Turabian StyleTorres-Castro, Rodrigo, Jordi Vilaró, Joan-Daniel Martí, Onintza Garmendia, Elena Gimeno-Santos, Bárbara Romano-Andrioni, Cristina Embid, and Josep M. Montserrat. 2019. "Effects of a Combined Community Exercise Program in Obstructive Sleep Apnea Syndrome: A Randomized Clinical Trial" Journal of Clinical Medicine 8, no. 3: 361. https://doi.org/10.3390/jcm8030361
APA StyleTorres-Castro, R., Vilaró, J., Martí, J.-D., Garmendia, O., Gimeno-Santos, E., Romano-Andrioni, B., Embid, C., & Montserrat, J. M. (2019). Effects of a Combined Community Exercise Program in Obstructive Sleep Apnea Syndrome: A Randomized Clinical Trial. Journal of Clinical Medicine, 8(3), 361. https://doi.org/10.3390/jcm8030361






