Effectiveness of an Attachment-Informed Working Alliance in Interdisciplinary Pain Therapy
Abstract
:1. Introduction
- (1)
- Patients in IG1 and IG2, who both receive an attachment-informed multidisciplinary treatment, will report a larger mean reduction in pain intensity between pre-treatment, post-treatment, and follow-up assessments than patients in the TAU group who receive state-of-the-art multidisciplinary treatment.
- (2)
- As the interventions (IG1 and IG2) are specifically designed to improve the working alliance, we expect higher ratings for the working alliance in IG1 and IG2 compared to TAU.
- (3)
- The quality of the working alliance will be the core mechanism of change in IG1 and IG2; that is, it will be the mediating variable between intervention and outcome.
- (4)
- As patients with higher levels of insecure attachment might not profit from the alliance in the same way as securely attached patients, we expect this mediation effect to be moderated by insecure attachment.
2. Materials and Methods
2.1. Participants
2.2. Inclusion and Exclusion Criteria
- High C-Reactive Protein (CRP) levels as an indicator of rheumatoid arthritis;
- Acute inflammation of the spine;
- A tumor;
- A diagnosis of psychosis;
- A diagnosis of a bipolar or neurological disorder;
- Insufficient ability to communicate in German.
2.3. Design
2.4. Interdisciplinary Multimodal Pain Treatment
2.5. Attachment-Informed Training
2.6. Outcome Measures
2.6.1. Pain Visual Analogue Scale (VAS)
2.6.2. Oswestry Low Back Pain Disability Questionnaire [43]
2.6.3. Experiences in Close Relationships Scale Revised 12—German Version (ECR-RD12) [47]
2.6.4. Inpatient and Day-Clinic Experience Scale—German Version (German TSEB/English IDES) [50]
2.7. Statistical Analyses
3. Results
3.1. Treatment’s Main Effects Analysis
3.2. Mediational Effects Analysis
3.3. Moderated Mediational Effects Analysis
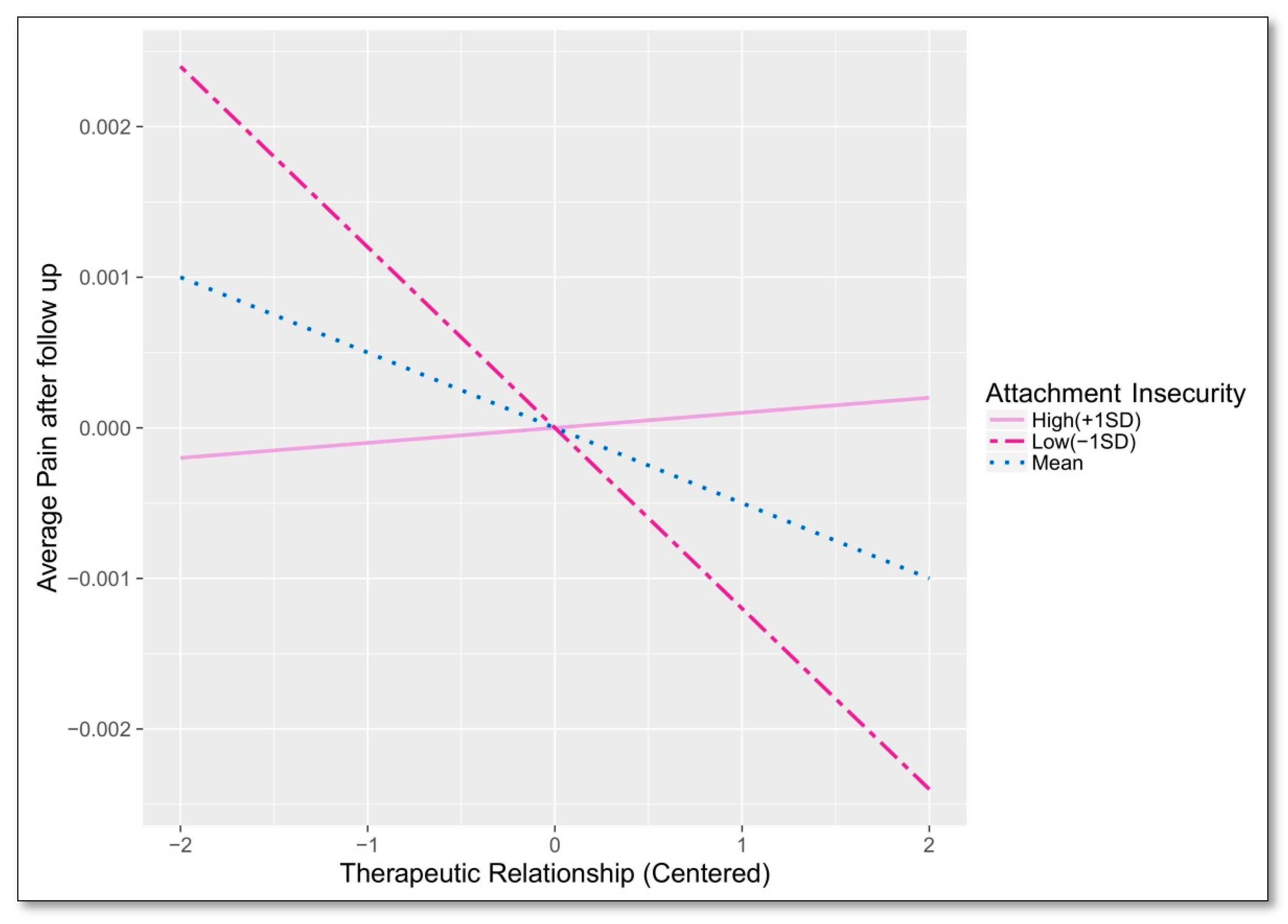
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gatchel, R.J.; Turk, D.C. Psychosocial Factors in Pain: Critical Perspectives; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Flor, H.; Hermann, C. Biopsychosocial models of pain. Prog. Pain Res. Manag. 2004, 27, 47–78. [Google Scholar]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581. [Google Scholar] [CrossRef]
- Meredith, P.; Ownsworth, T.; Strong, J. A review of the evidence linking adult attachment theory and chronic pain: Presenting a conceptual model. Clin. Psychol. Rev. 2008, 28, 407–429. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.; Hunter, J. An integrated approach to the formulation and psychotherapy of medically unexplained symptoms: Meaning-and attachment-based intervention. Am. J. Psychother. 2004, 58, 17. [Google Scholar] [CrossRef]
- Graetz, C.; Ehrenthal, J.C.; Senf, D.; Semar, K.; Herzog, W.; Dörfer, C.E. Influence of psychological attachment patterns on periodontal disease—A pilot study with 310 compliant patients. J. Clin. Periodontol. 2013, 40, 1087–1094. [Google Scholar] [CrossRef]
- Ciechanowski, P.S.; Katon, W.J.; Russo, J.E.; Walker, E.A. The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. Am. J. Psychiatry 2001, 158, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Ciechanowski, P.; Russo, J.; Katon, W.; Von Korff, M.; Ludman, E.; Lin, E.; Simon, G.; Bush, T. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom. Med. 2004, 66, 720–728. [Google Scholar] [CrossRef]
- Porter, L.S.; Davis, D.; Keefe, F.J. Attachment and pain: Recent findings and future directions. Pain 2007, 128, 195–198. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, L.A.; Murphy, P.D.; Bailey, S.J. Associations between adult attachment dimensions and attitudes toward pain behaviour. Pain Res. Manag. 2010, 15, 378–384. [Google Scholar] [CrossRef]
- Schmidt, S.; Nachtigall, C.; Wuethrich-Martone, O.; Strauss, B. Attachment and coping with chronic disease. J. Psychosom. Res. 2002, 53, 763–773. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment styles among young adults: A test of a four-category model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef] [PubMed]
- Mikulincer, M.; Shaver, P.R. Attachment in Adulthood: Structure, Dynamics, and Change; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Fraley, R.C.; Waller, N.G.; Brennan, K.A. An item response theory analysis of self-report measures of adult attachment. J. Pers. Soc. Psychol. 2000, 78, 350. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.W.; Bartholomew, K. Models of the self and other: Fundamental dimensions underlying measures of adult attachment. J. Pers. Soc. Psychol. 1994, 67, 430. [Google Scholar] [CrossRef]
- Ditzen, B.; Schmidt, S.; Strauss, B.; Nater, U.M.; Ehlert, U.; Heinrichs, M. Adult attachment and social support interact to reduce psychological but not cortisol responses to stress. J. Psychosom. Res. 2008, 64, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Meredith, P.; Strong, J.; Feeney, J.A. Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain 2006, 123, 146–154. [Google Scholar] [CrossRef]
- McWilliams, L.A.; Cox, B.J.; Enns, M.W. Impact of adult attachment styles on pain and disability associated with arthritis in a nationally representative sample. Clin. J. Pain 2000, 16, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, I.; Sullivan, M.J. Attachment and pain outcomes in adolescents: The mediating role of pain catastrophizing and anxiety. J. Pain 2010, 11, 160–171. [Google Scholar] [CrossRef]
- Pfeifer, A.-C.; Penedo, J.M.G.; Ehrenthal, J.C.; Neubauer, E.; Amelung, D.; Schroeter, C.; Schiltenwolf, M. Impact of attachment behavior on the treatment process of chronic pain patients. J. Pain Res. 2018, 11, 2653. [Google Scholar] [CrossRef] [PubMed]
- Davies, K.A.; Macfarlane, G.J.; McBeth, J.; Morriss, R.; Dickens, C. Insecure attachment style is associated with chronic widespread pain. Pain 2009, 143, 200–205. [Google Scholar] [CrossRef]
- Ciechanowski, P.; Sullivan, M.; Jensen, M.; Romano, J.; Summers, H. The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain 2003, 104, 627–637. [Google Scholar] [CrossRef]
- Andersen, T.E. Does attachment insecurity affect the outcomes of a multidisciplinary pain management program? The association between attachment insecurity, pain, disability, distress, and the use of opioids. Soc. Sci. Med. 2012, 74, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Meredith, P.J.; Strong, J.; Feeney, J.A. Adult attachment variables predict depression before and after treatment for chronic pain. Eur. J. Pain 2007, 11, 164–170. [Google Scholar] [CrossRef]
- Pfeifer, A.-C.; Ehrenthal, J.; Neubauer, E.; Gerigk, C.; Schiltenwolf, M. Einfluss des Bindungsverhaltens auf chronischen und somatoformen SchmerzImpact of attachment behavior on chronic and somatoform pain. Der Schmerz 2016, 30, 444–456. [Google Scholar] [CrossRef] [PubMed]
- Kowal, J.; McWilliams, L.A.; Péloquin, K.; Wilson, K.G.; Henderson, P.R.; Fergusson, D.A. Attachment insecurity predicts responses to an interdisciplinary chronic pain rehabilitation program. J. Behav. Med. 2015, 38, 518–526. [Google Scholar] [CrossRef]
- Gillath, O.; Karantzas, G.C.; Fraley, R.C. Adult Attachment: A Concise Introduction to Theory and Research; Academic Press: Cambridge, MA, USA, 2016. [Google Scholar]
- Byng-Hall, J. Evolving Ideas about Narrative: Re-editing the Re-editing of Family Mythology. J. Fam. Ther. 1998, 20, 133–142. [Google Scholar] [CrossRef]
- Slade, A. The move from categories to process: Attachment phenomena and clinical evaluation. Infant Ment. Health J. 2004, 25, 269–283. [Google Scholar] [CrossRef]
- Harris, T. Implications of attachment theory for working in psychoanalytic psychotherapy. Int. Forum Psychoanal. 2004, 13, 147–156. [Google Scholar] [CrossRef]
- Meyer, B.; Pilkonis, P.A. An attachment model of personality disorders. Major Theories Pers. Disord. 2005, 2, 231–281. [Google Scholar]
- Wallin, D.J. Attachment in Psychotherapy; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Obegi, J.H.; Berant, E. Attachment Theory and Research in Clinical Work with Adults; Guilford press: New York, NY, USA, 2010. [Google Scholar]
- Caspar, F.; Grossmann, C.; Unmüssig, C.; Schramm, E. Complementary therapeutic relationship: Therapist behavior, interpersonal patterns, and therapeutic effects. Psychother. Res. 2005, 15, 91–102. [Google Scholar] [CrossRef]
- Diamond, G.S.; Reis, B.F.; Diamond, G.M.; Siqueland, L.; Isaacs, L. Attachment-based family therapy for depressed adolescents: A treatment development study. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Bateman, A.W.; Fonagy, P. The development of an attachment-based treatment program for borderline personality disorder. Bull. Menninger Clin. 2003, 67, 187. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.M.; Whiffen, V.E. Attachment Processes in Couple and Family Therapy; Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Geller, J.D.; Farber, B.A. Attachment style, representations of psychotherapy, and clinical interventions with insecurely attached clients. J. Clin. Psychol. 2015, 71, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.N.; Ellison, W.D.; Scott, L.N.; Bernecker, S.L. Attachment style. J. Clin. Psychol. 2011, 67, 193–203. [Google Scholar] [CrossRef]
- Carlsson, A.M. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983, 16, 87–101. [Google Scholar] [CrossRef]
- Bijur, P.E.; Silver, W.; Gallagher, E.J. Reliability of the visual analog scale for measurement of acute pain. Acad. Emerg. Med. 2001, 8, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Gaul, C.; Mette, E.; Schmidt, T.; Grond, S. Practicability of a German version of the “Oswestry Low Back Pain Disability Questionnaire”. A questionnaire to assess disability caused by back pain. Schmerz 2008, 22, 51–58. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef]
- Davidson, M.; Keating, J. Oswestry disability questionnaire (ODQ). Aust. J. Physiother. 2005, 51, 270. [Google Scholar] [CrossRef]
- Firch, E.; Brooks, D.; Stratford, P.; Mayo, N. Physical Rehabilitation Outcome Measures; BC Decker Inc.: Hamilton, ON, Canada, 2002. [Google Scholar]
- Brenk-Franz, K.; Ehrenthal, J.; Freund, T.; Schneider, N.; Strauß, B.; Tiesler, F.; Schauenburg, H.; Gensichen, J. Evaluation of the short form of “Experience in Close Relationships” (Revised, German Version “ECR-RD12”)-A tool to measure adult attachment in primary care. PLoS ONE 2018, 13, e0191254. [Google Scholar] [CrossRef]
- Ehrenthal, J.C.; Dinger, U.; Lamla, A.; Funken, B.; Schauenburg, H. Evaluation der deutschsprachigen Version des Bindungsfragebogens „Experiences in Close Relationships—Revised”(ECR-RD). PPmP-Psychother. Psychosom. Med. Psychol. 2009, 59, 215–223. [Google Scholar] [CrossRef]
- Wei, M.; Russell, D.W.; Mallinckrodt, B.; Vogel, D.L. The Experiences in Close Relationship Scale (ECR)-short form: Reliability, validity, and factor structure. J. Pers. Assess. 2007, 88, 187–204. [Google Scholar] [CrossRef] [PubMed]
- Dinger, U.; Schauenburg, H.; Ehrenthal, J.C.; Nicolai, J.; Mander, J.; Sammet, I. Inpatient and Day-Clinic Experience Scale (IDES)-a Psychometric Evaluation/Tageskliniks-und Stationserfahrungsbogen–eine psychometrische Evaluation. Z. Psychosom. Med. Psychother. 2015, 61, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Corp, I. IBM SPSS Statistics for Windows; Version 22.0; IBM Corp.: Armonk, NY, USA, 2013. [Google Scholar]
- Team, R.C. R: A language and environment for statistical computing. 2013. [Google Scholar]
- Enders, C.K. Applied Missing Data Analysis; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Buuren, S.V.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2010, 45, 1–68. [Google Scholar] [CrossRef]
- White, I.R.; Royston, P.; Wood, A.M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2011, 30, 377–399. [Google Scholar] [CrossRef] [PubMed]
- Raudenbush, S.W. HLM 6: Hierarchical Linear and Nonlinear Modeling; Scientific Software International: Skokie, IL, USA, 2004. [Google Scholar]
- Raudenbush, S.W.; Bryk, A.S. Hierarchical Linear Models: Applications and Data Analysis Methods; Sage: Thousand Oaks, CA, USA, 2002; Volume 1. [Google Scholar]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2012; Volume 998. [Google Scholar]
- Singer, J.D.; Willett, J.B. Applied longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Smith, J.Z.; Sayer, A.G.; Goldberg, A.E. Multilevel modeling approaches to the study of LGBT-parent families: Methods for dyadic data analysis. In LGBT-Parent Families; Springer: Berlin/Heidelberg, Germany, 2013; pp. 307–323. [Google Scholar]
- Barnett, R.C.; Marshall, N.L.; Raudenbush, S.W.; Brennan, R.T. Gender and the relationship between job experiences and psychological distress: A study of dual-earner couples. J. Pers. Soc. Psychol. 1993, 64, 794. [Google Scholar] [CrossRef]
- Kenward, M.G.; Roger, J.H. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 1997, 53, 983–997. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Kolb, L.C. Attachment behavior and pain complaints. Psychosomatics 1982, 23, 413–425. [Google Scholar] [CrossRef]
- Smith, A.E.; Msetfi, R.M.; Golding, L. Client self rated adult attachment patterns and the therapeutic alliance: A systematic review. Clin. Psychol. Rev. 2010, 30, 326–337. [Google Scholar] [CrossRef]
- Damasio, A. Human behaviour: Brain trust. Nature 2005, 435, 571–572. [Google Scholar] [CrossRef]
- Nickel, R.; Egle, U.T. Manualisierte psycho-dynamisch-interaktionelle Gruppentherapie. Psychotherapeut 2001, 46, 11–19. [Google Scholar] [CrossRef]
- van IJzendoorn, M.H.; Juffer, F.; Duyvesteyn, M.G. Breaking the intergenerational cycle of insecure attachment: A review of the effects of attachment-based interventions on maternal sensitivity and infant security. J. Child Psychol. Psychiatry 1995, 36, 225–248. [Google Scholar] [CrossRef] [PubMed]
- Blatt, S.J.; Zuroff, D.C.; Hawley, L.L.; Auerbach, J.S. Predictors of sustained therapeutic change. Psychother. Res. 2010, 20, 37–54. [Google Scholar] [CrossRef] [PubMed]
- Barber, J.P.; Luborsky, L.; Gallop, R.; Crits-Christoph, P.; Frank, A.; Weiss, R.D.; Thase, M.E.; Connolly, M.B.; Gladis, M.; Foltz, C. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J. Consult. Clin. Psychol. 2001, 69, 119. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.K.; Fuertes, J.N.; Keitel, M.; Phillips, R. The role of patient attachment and working alliance on patient adherence, satisfaction, and health-related quality of life in lupus treatment. Patient Educ. Couns. 2011, 85, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Horvath, A.O.; Del Re, A.; Flückiger, C.; Symonds, D. Alliance in Individual Psychotherapy. Psychotherapy 2011, 48, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Bateman, A.; Fonagy, P. Mentalization-Based Treatment for Personality Disorders: A Practical Guide; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Bateman, A.; Fonagy, P. 8-Year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. Am. J. Psychiatry 2008, 165, 631–638. [Google Scholar] [CrossRef]
- Jørgensen, C.R.; Freund, C.; Bøye, R.; Jordet, H.; Andersen, D.; Kjølbye, M. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: A randomized trial. Acta Psychiatr. Scand. 2013, 127, 305–317. [Google Scholar] [CrossRef]
- Simpson, S.H.; Eurich, D.T.; Majumdar, S.R.; Padwal, R.S.; Tsuyuki, R.T.; Varney, J.; Johnson, J.A. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006, 333, 15. [Google Scholar] [CrossRef]
- Simpson, R.J. Challenges for improving medication adherence. JAMA 2006, 296, 2614–2616. [Google Scholar] [CrossRef]
- Mikail, S.F.; Henderson, P.R.; Tasca, G.A. An interpersonally based model of chronic pain: An application of attachment theory. Clin. Psychol. Rev. 1994, 14, 1–16. [Google Scholar] [CrossRef]





| Variable | TAU n = 159 | IG1 n = 163 | IG2 n = 52 | Statistical Test | p Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| M/% | SD | M/% | SD | M/% | SD | ||||
| Age | 66.67 | 12.04 | 58.90 | 13.01 | 67.31 | 12.90 | F(2,367) = 0.81 | 0.45 | |
| Gender | Female | 54% | - | 54% | - | 52% | - | χ2(2) = 2.50 | 0.29 |
| Marital status | Married | 61% | - | 58% | - | 58% | - | χ2(2) = 0.32 | 0.85 |
| Divorced | 18% | - | 15% | - | 21% | - | χ2(2) = 0.99 | 0.61 | |
| Single | 15% | - | 21% | - | 19% | - | χ2(2) = 1.84 | 0.40 | |
| Widowed | 6% | - | 6% | - | 2% | - | χ2(2) = 1.49 | 0.47 | |
| Employment | Currently working | 47% | - | 45% | - | 67% | - | χ2(2) = 9.88 | 0.01* |
| Unemployed | 53% | - | 55% | - | 33% | - | χ2(2) = 9.88 | 0.01* | |
| Old-age pension | 71% | - | 70% | - | 58% | - | χ2(2) = 3.46 | 0.17 | |
| Disability pension | 15% | - | 18% | - | 27% | - | χ2(2) = 370 | 0.16 | |
| Education | Lower/middle secondary | 81% | - | 86% | - | 77% | - | χ2(2) = 2.34 | 0.27 |
| College/university | 19% | - | 14% | - | 23% | - | χ2(2) = 2.34 | 0.27 | |
| Variable | TAU | IG1 | IG2 | Statistical Test | p Value | |||
|---|---|---|---|---|---|---|---|---|
| M/% | SD | M/% | SD | M/% | SD | |||
| Age | 53.56 | 12.04 | 54.45 | 13.01 | 51.92 | 12.90 | F(2,367) = 0.81 | 0.45 |
| Female | 66.7% | - | 58.9% | - | 67.31 | - | χ2(2) = 2.50 | 0.29 |
| Average Pain | 6.44 | 1.80 | 6.74 | 1.79 | 6.29 | 1.75 | F(2,371) = 1.80 | 0.17 |
| Current Pain | 5.97 | 2.08 | 6.04 | 2.26 | 5.38 | 2.22 | F(2,364) = 1.83 | 0.16 |
| ECR-RD12 Anxiety | 2.30 | 1.39 | 2.40 | 1.39 | 2.37 | 1.38 | F(2,338) = 0.21 | 0.81 |
| ECR-RD12 Avoidance | 2.46 | 1.22 | 2.54 | 1.17 | 2.43 | 1.19 | F(2,340) = 0.22 | 0.81 |
| I | Gender | Average Pain | Current Pain | Physical Functioning | ECR-RD12 Anxiety | ECR-RD12 Avoidance |
|---|---|---|---|---|---|---|
| Age | 0.12 * | 0.15 ** | 0.12 * | 0.25 *** | −0.06 | 0.19 *** |
| Gender | 0.05 | 0.06 | 0.09 | 0.01 | 0.08 | |
| Average Pain | 0.70 *** | 0.42 *** | 0.01 | 0.02 | ||
| Current Pain | 0.44 *** | 0 | 0.05 | |||
| Physical Functioning | 0.05 | 0.1 | ||||
| ECR-RD12 Anxiety | 0.22 *** |
| Fixed Effect | Coefficient | Standard Error | t-Ratio | Approx. df | p |
|---|---|---|---|---|---|
| For Intercept, β0 | |||||
| Intercept | 4.823 | 0.116 | 41.556 | 358 | <0.001 |
| IG1 vs. IG2 | −0.923 | 0.269 | −2.11 | 358 | 0.058 |
| ECR-RD12 Anxiety | −0.132 | 0.092 | −1.429 | 358 | 0.154 |
| IG2 x ECR-RD12 Anxiety | 0.522 | 0.224 | 2.322 | 358 | 0.021 |
| For Piece 1 slope, β1 | |||||
| Intercept | −0.364 | 0.026 | −13.529 | 358 | <0.001 |
| IG1 vs. IG2 | 0.028 | 0.073 | 0.396 | 358 | 0.693 |
| ECR-RD12 Anxiety | 0.013 | 0.020 | 0.660 | 358 | 0.510 |
| IG2 x ECR-RD12 Anxiety | −0.052 | 0.064 | −0.812 | 358 | 0.417 |
| For Piece 2 slope, β2 | |||||
| Intercept | 0.018 | 0.005 | 3.332 | 358 | <0.001 |
| IG1 vs. IG2 | −0.024 | 0.016 | −1.498 | 358 | 0.135 |
| ECR-RD12 Anxiety | 0.001 | 0.004 | 0.023 | 358 | 0.981 |
| IG2 x ECR-RD12 Anxiety | −0.021 | 0.011 | −1.774 | 358 | 0.077 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pfeifer, A.-C.; Meredith, P.; Schröder-Pfeifer, P.; Gomez Penedo, J.M.; Ehrenthal, J.C.; Schroeter, C.; Neubauer, E.; Schiltenwolf, M. Effectiveness of an Attachment-Informed Working Alliance in Interdisciplinary Pain Therapy. J. Clin. Med. 2019, 8, 364. https://doi.org/10.3390/jcm8030364
Pfeifer A-C, Meredith P, Schröder-Pfeifer P, Gomez Penedo JM, Ehrenthal JC, Schroeter C, Neubauer E, Schiltenwolf M. Effectiveness of an Attachment-Informed Working Alliance in Interdisciplinary Pain Therapy. Journal of Clinical Medicine. 2019; 8(3):364. https://doi.org/10.3390/jcm8030364
Chicago/Turabian StylePfeifer, Ann-Christin, Pamela Meredith, Paul Schröder-Pfeifer, Juan Martin Gomez Penedo, Johannes C. Ehrenthal, Corinna Schroeter, Eva Neubauer, and Marcus Schiltenwolf. 2019. "Effectiveness of an Attachment-Informed Working Alliance in Interdisciplinary Pain Therapy" Journal of Clinical Medicine 8, no. 3: 364. https://doi.org/10.3390/jcm8030364
APA StylePfeifer, A. -C., Meredith, P., Schröder-Pfeifer, P., Gomez Penedo, J. M., Ehrenthal, J. C., Schroeter, C., Neubauer, E., & Schiltenwolf, M. (2019). Effectiveness of an Attachment-Informed Working Alliance in Interdisciplinary Pain Therapy. Journal of Clinical Medicine, 8(3), 364. https://doi.org/10.3390/jcm8030364







