Esthetic Rehabilitation of Maxillary Anterior Teeth, Including an Immediate Provisionalization with an Implant-Supported Fixed Dental Prosthesis
Abstract
:1. Introduction
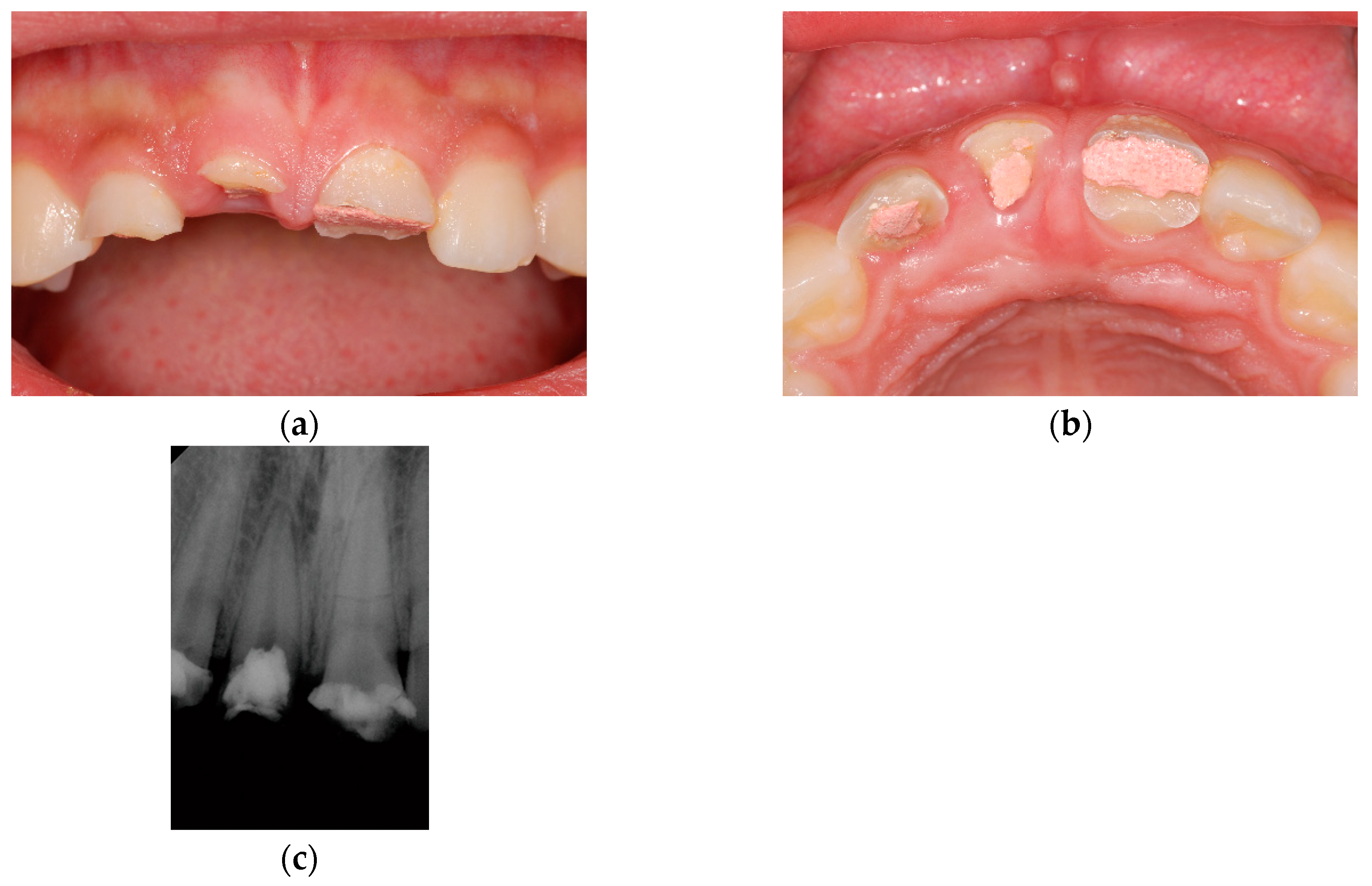
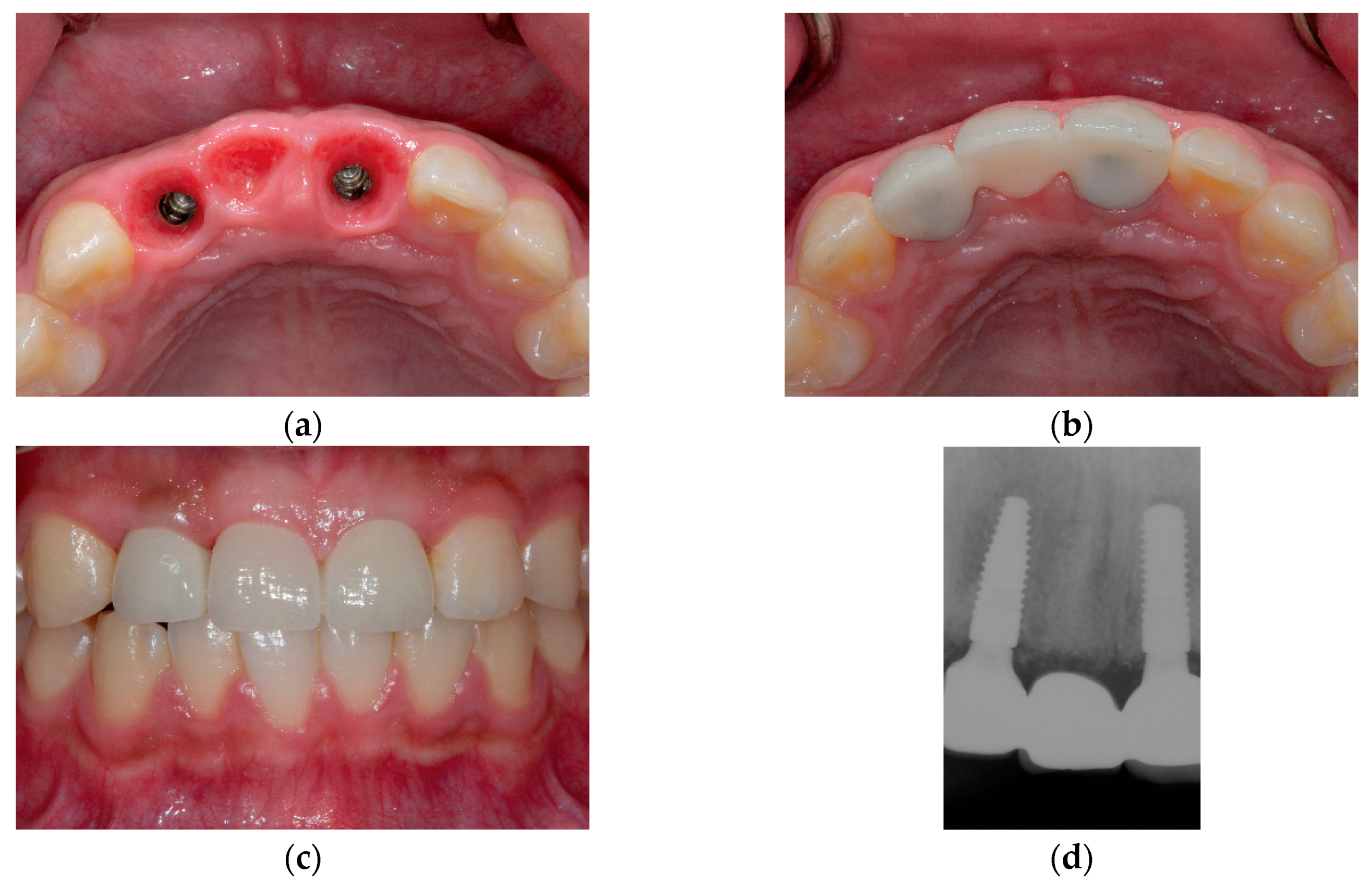
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S. Dental implants: The last 100 years. J. Oral Maxillofac. Surg. 2018, 76, 11–26. [Google Scholar] [CrossRef]
- Patel, N. Integrating three-dimensional digital technologies for comprehensive implant dentistry. J. Am. Dent. Assoc. 2010, 141 (Suppl. S2), 20S–24S. [Google Scholar] [CrossRef]
- Zimmermann, M.; Mehl, A.; Mormann, W.H.; Reich, S. Intraoral scanning systems—A current overview. Int. J. Comput. Dent. 2015, 18, 101–129. [Google Scholar]
- Marchack, C.B.; Chew, L.K. The 10-year evolution of guided surgery. J. Calif. Dent. Assoc. 2015, 43, 131–134. [Google Scholar] [PubMed]
- Sarment, D.P.; Sukovic, P.; Clinthorne, N. Accuracy of implant placement with a stereolithographic surgical guide. Int. J. Oral Maxillofac. Implant. 2003, 18, 571–577. [Google Scholar]
- Deeb, G.R.; Allen, R.K.; Hall, V.P.; Whitley, D., 3rd; Laskin, D.M.; Bencharit, S. How accurate are implant surgical guides produced with desktop stereolithographic 3-dimentional printers? J. Oral Maxillofac. Surg. 2017, 75, e2551–e2559. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, H.J.; Wichmann, M.; Hamel, J.; Schlegel, K.A.; Eitner, S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method-a combined in vivo-in vitro technique using cone-beam ct (part ii). J. Cranio Maxillofac. Surg. 2010, 38, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Rangel, F.A.; Maal, T.J.J.; de Koning, M.J.J.; Bronkhorst, E.M.; Berge, S.J.; Kuijpers-Jagtman, A.M. Integration of digital dental casts in cone beam computed tomography scans-a clinical validation study. Clin. Oral Investig. 2018, 22, 1215–1222. [Google Scholar] [CrossRef]
- Garber, D.A.; Belser, U.C. Restoration-driven implant placement with restoration-generated site development. Compend. Contin. Educ. Dent. 1995, 16, 798–802. [Google Scholar]
- Pesun, I.J.; Gardner, F.M. Fabrication of a guide for radiographic evaluation and surgical placement of implants. J. Prosthet. Dent. 1995, 73, 548–552. [Google Scholar] [CrossRef]
- Almog, D.M.; Torrado, E.; Meitner, S.W. Fabrication of imaging and surgical guides for dental implants. J. Prosthet. Dent. 2001, 85, 504–508. [Google Scholar] [CrossRef]
- Kopp, K.C.; Koslow, A.H.; Abdo, O.S. Predictable implant placement with a diagnostic/surgical template and advanced radiographic imaging. J. Prosthet. Dent. 2003, 89, 611–615. [Google Scholar] [CrossRef]
- Ritter, L.; Neugebauer, J.; Dreiseidler, T.; Rothamel, D.; Cizek, J.; Karapetian, V.E.; Mischkowski, R.A.; Bindl, A.; Zoller, J.E. 3D X-ray meets CAD/CAM dentistry: A novel procedure for virtual dental implant planning. Int. J. Comput. Dent. 2009, 12, 29–40. [Google Scholar] [PubMed]
- Lanis, A.; Alvarez Del Canto, O. The combination of digital surface scanners and cone beam computed tomography technology for guided implant surgery using 3shape implant studio software: A case history report. Int. J. Prosthodont. 2015, 28, 169–178. [Google Scholar] [CrossRef]
- Stimmelmayr, M.; Guth, J.F.; Erdelt, K.; Edelhoff, D.; Beuer, F. Digital evaluation of the reproducibility of implant scanbody fit—An in vitro study. Clin. Oral Investig. 2012, 16, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Van Nimwegen, W.G.; Goene, R.J.; van Daelen, A.C.; Stellingsma, K.; Raghoebar, G.M.; Meijer, H.J. Immediate implant placement and provisionalisation in the aesthetic zone. J. Oral Rehabil. 2016, 43, 745–752. [Google Scholar] [CrossRef]
- De Bruyn, H.; Raes, S.; Ostman, P.O.; Cosyn, J. Immediate loading in partially and completely edentulous jaws: A review of the literature with clinical guidelines. Periodontology 2014, 66, 153–187. [Google Scholar] [CrossRef] [PubMed]
- Levin, B.P. Immediate temporization of immediate implants in the esthetic zone: Evaluating survival and bone maintenance. Compend. Contin. Educ. Dent. 2011, 32, 58–60. [Google Scholar]
- Bruno, V.; Badino, M.; Sacco, R.; Catapano, S. The use of a prosthetic template to maintain the papilla in the esthetic zone for immediate implant placement by means of a radiographic procedure. J. Prosthet. Dent. 2012, 108, 394–397. [Google Scholar] [CrossRef]
- Bruno, V.; O’Sullivan, D.; Badino, M.; Catapano, S. Preserving soft tissue after placing implants in fresh extraction sockets in the maxillary esthetic zone and a prosthetic template for interim crown fabrication: A prospective study. J. Prosthet. Dent. 2014, 111, 195–202. [Google Scholar] [CrossRef]
- Sohn, D.S.; Bae, M.S.; Heo, J.U.; Park, J.S.; Yea, S.H.; Romanos, G.E. Retrospective multicenter analysis of immediate provisionalization using one-piece narrow-diameter (3.0-mm) implants. Int. J. Oral Maxillofac. Implant. 2011, 26, 163–168. [Google Scholar]
- Lauritano, D.; Grassi, R.; di Stasio, D.; Lucchese, A.; Petruzzi, M. Successful mandible rehabilitation of lower incisors with one-piece implants. J. Med. Case Rep. 2014, 8, 406. [Google Scholar] [CrossRef]
- Siadat, H.; Alikhasi, M.; Beyabanaki, E. Interim prosthesis options for dental implants. J. Prosthodont. 2017, 26, 331–338. [Google Scholar] [CrossRef] [PubMed]
- AlKudmani, H.; Al Jasser, R.; Andreana, S. Is bone graft or guided bone regeneration needed when placing immediate dental implants? A systematic review. Implant. Dent. 2017, 26, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Hammerle, C.H.; Lang, N.P. Single stage surgery combining transmucosal implant placement with guided bone regeneration and bioresorbable materials. Clin. Oral Implant. Res. 2001, 12, 9–18. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Gaudioso, L.; Bunino, M.; Dalmasso, P. Long-term stability of soft tissues following alveolar ridge preservation: 10-year results of a prospective study around nonsubmerged implants. Int. J. Periodontics Restor. Dent. 2014, 34, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, K.L. Extraction site management using a natural bone mineral containing collagen: Rationale and retrospective case study. Int. J. Periodontics Restor. Dent. 2009, 29, 489–497. [Google Scholar]
- Levin, B.P.; Wilk, B.L. Immediate provisionalization of immediate implants in the esthetic zone: A prospective case series evaluating implant survival, esthetics, and bone maintenance. Compend. Contin. Educ. Dent. 2013, 34, 352–361. [Google Scholar] [PubMed]
- Testori, T.; Galli, F.; Capelli, M.; Zuffetti, F.; Esposito, M. Immediate nonocclusal versus early loading of dental implants in partially edentulous patients: 1-year results from a multicenter, randomized controlled clinical trial. Int. J. Oral Maxillofac. Implant. 2007, 22, 815–822. [Google Scholar]
- Schincaglia, G.P.; Marzola, R.; Giovanni, G.F.; Chiara, C.S.; Scotti, R. Replacement of mandibular molars with single-unit restorations supported by wide-body implants: Immediate versus delayed loading. A randomized controlled study. Int. J. Oral Maxillofac. Implant. 2008, 23, 474–480. [Google Scholar]
- Cooper, L.F.; Raes, F.; Reside, G.J.; Garriga, J.S.; Tarrida, L.G.; Wiltfang, J.; Kern, M.; de Bruyn, H. Comparison of radiographic and clinical outcomes following immediate provisionalization of single-tooth dental implants placed in healed alveolar ridges and extraction sockets. Int. J. Oral Maxillofac. Implant. 2010, 25, 1222–1232. [Google Scholar]
- Hinds, K.F. Custom impression coping for an exact registration of the healed tissue in the esthetic implant restoration. Int. J. Periodontics Restor. Dent. 1997, 17, 584–591. [Google Scholar]
- Buskin, R.; Salinas, T.J. Transferring emergence profile created from the provisional to the definitive restoration. Pract. Periodontics Aesthetic Dent. 1998, 10, 1171–1179; quiz 1180. [Google Scholar]
- Stumpel, L.J.; Haechler, W.; Bedrossian, E. Customized abutments to shape and transfer peri-implant soft-tissue contours. J. Calif. Dent. Assoc. 2000, 28, 301–309. [Google Scholar] [PubMed]
- Jansen, C.E. Guided soft tissue healing in implant dentistry. J. Calif. Dent. Assoc. 1995, 23, 57–58, 60, 62 passim. [Google Scholar] [PubMed]
- Chee, W.W.; Cho, G.C.; Ha, S. Replicating soft tissue contours on working casts for implant restorations. J. Prosthodont. 1997, 6, 218–220. [Google Scholar] [CrossRef]
- Neale, D.; Chee, W.W. Development of implant soft tissue emergence profile: A technique. J. Prosthet. Dent. 1994, 71, 364–368. [Google Scholar] [CrossRef]
- Elian, N.; Tabourian, G.; Jalbout, Z.N.; Classi, A.; Cho, S.C.; Froum, S.; Tarnow, D.P. Accurate transfer of peri-implant soft tissue emergence profile from the provisional crown to the final prosthesis using an emergence profile cast. J. Esthet. Restor. Dent. 2007, 19, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Joda, T. Time-dependent supraimplant mucosa changes: Short communication. Int. J. Oral Maxillofac. Implant. 2015, 30, 619–621. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Arnold, D.; Ball, J.; Brusco, D.; Triaca, A.; Verna, C. Treatment strategies for infraoccluded dental implants. J. Prosthet. Dent. 2015, 113, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Gotfredsen, K.; Carlsson, G.E.; Jokstad, A.; Arvidson Fyrberg, K.; Berge, M.; Bergendal, B.; Bergendal, T.; Ellingsen, J.E.; Gunne, J.; Hofgren, M.; et al. Implants and/or teeth: Consensus statements and recommendations. J. Oral Rehabil. 2008, 35 (Suppl. S1), 2–8. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, L.J.; Cronin, R.J., Jr. Adult growth, aging, and the single-tooth implant. Int. J. Oral Maxillofac. Implant. 2000, 15, 252–260. [Google Scholar]





| Digital Intraoral Impressions | First | Second | Third | Fourth | Fifth |
|---|---|---|---|---|---|
| Time points | Immediately after extraction | 2 months after implant placement | 4 months after implant placement | 6 months after implant placement | 1 year after implant placement |
| Treatments provided | Extraction, immediate implant placement, and immediate provisionalization | Exchange of provisional restoration | Final impression-making | Placement of definitive restoration | Routine follow-up |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, K.C.; Paik, J.; Kim, J.-H. Esthetic Rehabilitation of Maxillary Anterior Teeth, Including an Immediate Provisionalization with an Implant-Supported Fixed Dental Prosthesis. J. Clin. Med. 2019, 8, 428. https://doi.org/10.3390/jcm8040428
Oh KC, Paik J, Kim J-H. Esthetic Rehabilitation of Maxillary Anterior Teeth, Including an Immediate Provisionalization with an Implant-Supported Fixed Dental Prosthesis. Journal of Clinical Medicine. 2019; 8(4):428. https://doi.org/10.3390/jcm8040428
Chicago/Turabian StyleOh, Kyung Chul, Jeongwon Paik, and Jee-Hwan Kim. 2019. "Esthetic Rehabilitation of Maxillary Anterior Teeth, Including an Immediate Provisionalization with an Implant-Supported Fixed Dental Prosthesis" Journal of Clinical Medicine 8, no. 4: 428. https://doi.org/10.3390/jcm8040428





