Impact of Different Titanium Implant Thread Designs on Bone Healing: A Biomechanical and Histometric Study with an Animal Model
Abstract
:1. Introduction
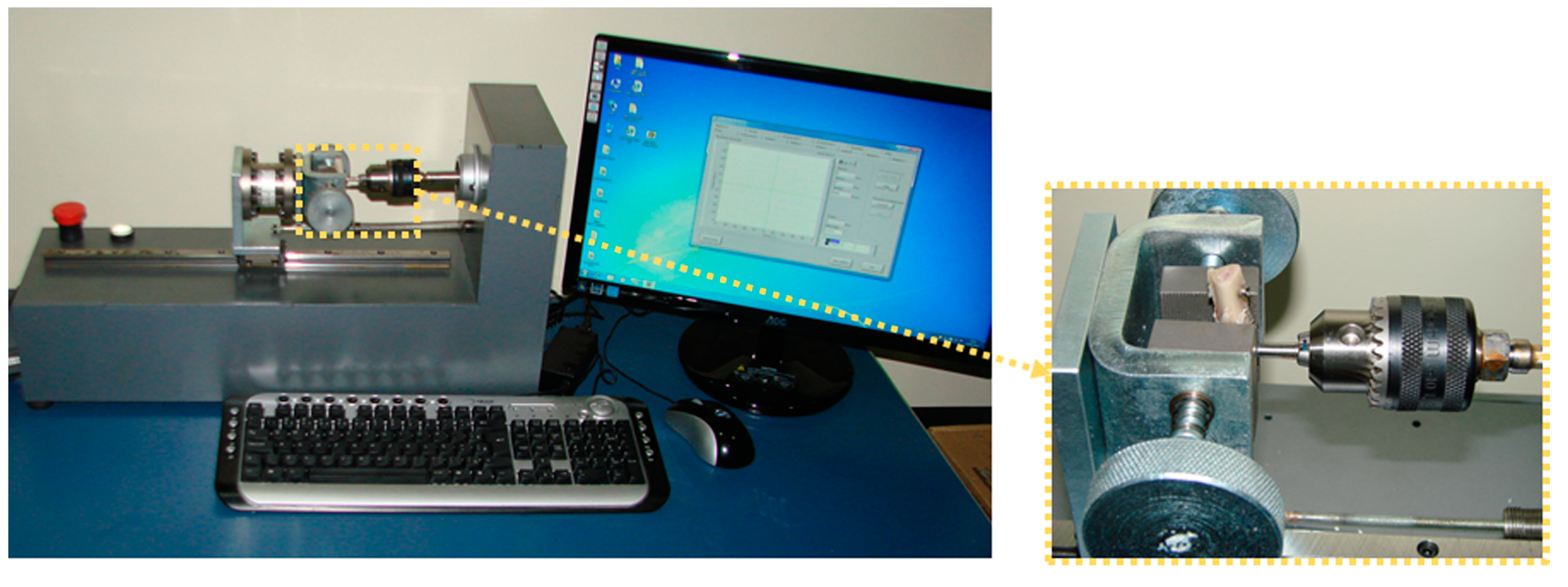
2. Experimental Section
Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Perrotti, V.; Ravera, L.; Ricci, L.; Doi, K.; Piattelli, A.; Shibli, J.; Iezzi, G. Radiographic comparison of periimplant bone resorption and assessment of survival rates of 2 implant systems: A 10-year prospective multicenter study. Implant Dent. 2015, 24, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Iaculli, F.; Piattelli, A.; Mangano, F. Fixed restorations supported by Morse-taper connection implants: A retrospective clinical study with 10–20 years of follow-up. Clin. Oral Implants Res. 2015, 26, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Ozan, O.; Yilmaz, B.; Ersoy, A.E. Determination of Bone Quality of 372 Implant Recipient Sites Using Hounsfield Unit from Computerized Tomography: A Clinical Study. Clin. Implant Dent. Relat. Res. 2008, 10, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Drage, N.A.; Palmer, R.M.; Blake, G.; Wilson, R.; Crane, F.; Fogelman, I. A comparison of bone mineral density in the spine, hip and jaws of edentulous subjects. Clin. Oral Implant Res. 2007, 18, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Brink, J.; Meraw, S.J.; Sarment, D.P. Influence of implant diameter on surrounding bone. Clin. Oral Implants Res. 2007, 18, 563–568. [Google Scholar] [CrossRef] [Green Version]
- Chong, L.; Khocht, A.; Suzuki, J.B.; Gaughan, J. Effect of implant design on initial stability of tapered implants. J. Oral Implantol. 2009, 35, 130–135. [Google Scholar] [CrossRef]
- Chun, H.J.; Cheong, S.Y.; Han, J.H.; Heo, S.J.; Chung, J.P.; Rhyu, I.C.; Choi, Y.C.; Baik, H.K.; Ku, Y.; Kim, M.H. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J. Oral Rehabil. 2002, 29, 565–574. [Google Scholar] [CrossRef]
- Eraslan, O.; Inan, O. The effect of thread design on stress distribution in a solid screw implant: A 3D finite element analysis. Clin. Oral Investig. 2010, 14, 411–416. [Google Scholar] [CrossRef]
- Martinez, H.; Davarpanah, M.; Missika, P.; Celletti, R.; Lazzara, R. Optimal implant stabilization in low density bone. Clin. Oral Implants Res. 2001, 12, 423–432. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Pérez-Albacete Martínez, C.; Piattelli, A.; Shibli, J.A.; Markovic, A.; Calvo Guirado, J.L. The influence of three different apical implant designs at stability and osseointegration process: Experimental study in rabbits. Clin. Oral Implants Res. 2017, 28, 355–361. [Google Scholar] [CrossRef]
- Gehrke, S.A.; da Silva, U.T.; Del Fabbro, M. Does Implant Design Affect Implant Primary Stability? A Resonance Frequency Analysis-Based Randomized Split-Mouth Clinical Trial. J. Oral Implantol. 2015, 41, e281–e286. [Google Scholar] [CrossRef] [PubMed]
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.L. The effect of thread pattern upon implant osseointegration. Clin. Oral Implants Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campos, F.E.; Gomes, J.B.; Marin, C.; Teixeira, H.S.; Suzuki, M.; Witek, L.; Zanetta-Barbosa, D.; Coelho, P.G. Effect of drilling dimension on implant placement torque and early osseointegration stages: An experimental study in dogs. J. Oral Maxillofac. Surg. 2012, 70, e43–e50. [Google Scholar] [CrossRef] [PubMed]
- Jimbo, R.; Janal, M.N.; Marin, C.; Giro, G.; Tovar, N.; Coelho, P.G. The effect of implant diameter on osseointegration utilizing simplified drilling protocols. Clin. Oral Implants Res. 2014, 25, 1295–1300. [Google Scholar] [CrossRef]
- Coelho, P.G.; Jimbo, R. Osseointegration of metallic devices: current trends based on implant hardware design. Arch. Biochem. Biophys. 2014, 561, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Dedavid, B.A.; Aramburú, J.S.; Pérez-Díaz, L.; Guirado, J.L.C.; Canales, P.M.; De Aza, P.N. Effect of Different Morphology of Titanium Surface on the Bone Healing in Defects Filled Only with Blood Clot: A New Animal Study Design. BioMed Res. Int. 2018, 2018, 4265474. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Granato, R.; Suzuki, M.; Gil, J.N.; Janal, M.N.; Coelho, P.G. Histomorphologic and histomorphometric evaluation of various endosseous implant healing chamber configurations at early implantation times: A study in dogs. Clin. Oral Implants Res. 2010, 21, 577–583. [Google Scholar] [CrossRef]
- Barros, R.R.; Novaes, A.B., Jr.; Papalexiou, V.; Souza, S.L.; Taba, M., Jr.; Palioto, D.B.; Grisi, M.F. Effect of biofunctionalized implant surface on osseointegration: A histomorphometric study in dogs. Braz. Dent. J. 2009, 20, 91–98. [Google Scholar] [CrossRef]
- Oliveira, P.S.; Rodrigues, J.A.; Shibli, J.A.; Piattelli, A.; Iezzi, G.; Perrotti, V. Influence of osteoporosis on the osteocyte density of human mandibular bone samples: A controlled histological human study. Clin. Oral Implants Res. 2016, 27, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Orsini, E.; Giavaresi, G.; Trirè, A.; Ottani, V.; Salgarello, S. Dental implant thread pitch and its influence on the osseointegration process: An in vivo comparison study. Int. J. Oral Maxillofac. Implants 2012, 27, 383–392. [Google Scholar] [PubMed]
- Pearce, A.I.; Richards, R.G.; Milz, S.; Schneider, E.; Pearce, S.G. Animal models for implant biomaterial research in bone: A review. Eur. Cell. Mater. 2007, 13, 1–10. [Google Scholar] [CrossRef]
- Steigenga, J.; Al-Shammari, K.; Misch, C.; Nociti, F.H., Jr.; Wang, H.-L. Effects of implant thread geometry on percentage of osseointegration and resistance to reverse torque in the tibia of rabbits. J. Periodontol. 2004, 75, 1233–1241. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Prados-Frutos, J.C.; Prados-Privado, M.; Calvo-Guirado, J.L.; Aramburú Júnior, J.; Pérez-Díaz, L.; Mazón, P.; Aragoneses, J.M.; De Aza, P.N. Biomechanical and Histological Analysis of Titanium (Machined and Treated Surface) Versus Zirconia Implant Materials: An In Vivo Animal Study. Materials 2019, 12, 856. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Taschieri, S.; Del Fabbro, M.; Coelho, P.G. Positive Biomechanical Effects of Titanium Oxide for Sandblasting Implant Surface as an Alternative to Aluminium Oxide. J. Oral Implantol. 2015, 41, 515–522. [Google Scholar] [CrossRef]
- Ivanoff, C.J.; Sennerby, L.; Johansson, C.; Rangert, B.; Lekholm, U. Influence of implant diameters on the integration of screw implants. An experimental study in the rabbit. Int. J. Oral Maxillofac. Surg. 1997, 26, 141–148. [Google Scholar] [CrossRef]
- Bonfante, E.A.; Granato, R.; Marin, C.; Suzuki, M.; Oliveira, S.R.; Giro, G.; Coelho, P.G. Early bone healing and biomechanical fixation of dual acid-etched and as-machined implants with healing chambers: An experimental study in dogs. Int. J. Oral Maxillofac. Implants 2011, 26, 75–82. [Google Scholar] [PubMed]
- Soto-Peñaloza, D.; Caneva, M.; Viña-Almunia, J.; Martín-de-Llano, J.J.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Bone-Healing Pattern on the Surface of Titanium Implants at Cortical and Marrow Compartments in Two Topographic Sites: An Experimental Study in Rabbits. Materials 2018, 12, 85. [Google Scholar] [CrossRef]
- Buser, D.; Broggini, N.; Wieland, M.; Schenk, R.K.; Denzer, A.J.; Cochran, D.L.; Hoffmann, B.; Lussi, A.; Steinemann, S.G. Enhanced bone apposition to a chemically modified SLA titanium surface. J. Dent. Res. 2004, 83, 529–533. [Google Scholar] [CrossRef] [PubMed]
- De Lima Cavalcanti, J.H.; Matos, P.C.; Depes de Gouvêa, C.V.; Carvalho, W.; Calvo-Guirado, J.L.; Aragoneses, J.M.; Pérez-Díaz, L.; Gehrke, S.A. In Vitro Assessment of the Functional Dynamics of Titanium with Surface Coating of Hydroxyapatite Nanoparticles. Materials 2019, 12, 840. [Google Scholar] [CrossRef] [PubMed]
- Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Precht, C.; Kloss, F.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of Dental Implant Surface Modifications on Osseointegration. BioMed Res. Int. 2016, 2016, 6285620. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, C.J.; Majeska, R.J.; Schaffler, M.B. Osteocyte density in woven bone. Bone 2004, 35, 1095–1099. [Google Scholar] [CrossRef] [PubMed]











| Parameter | G1 | G2 | G3 |
|---|---|---|---|
| Mean ± SD | 73.9 ± 3.51 | 71.5 ± 4.33 | 73.3 ± 4.15 |
| Median (range) | 73.5 (60–81) | 72.0 (63–80) | 73.4 (59–80) |
| Group | BIC% ± SD | Median |
|---|---|---|
| G1 | 51.8 ± 9.39 | 55.7 |
| G2 | 52.6 ± 8.12 | 51.6 |
| G3 | 57.4 ± 7.58 | 58.5 |
| Group Comparison | Mean of Difference | t | Significant p < 0.05 | 95% Confidence Interval of Difference |
|---|---|---|---|---|
| G1 vs. G2 | −0.8400 | 0.2237 | No | −10.43 to 8.747 |
| G1 vs. G3 | −5.580 | 1.486 | No | −15.17 to 4.007 |
| G2 vs. G3 | −4.740 | 1.262 | No | −14.33 to 4.847 |
| Group Comparison | Mean of Difference | t | Significant p < 0.05 | 95% Confidence Interval of Difference |
|---|---|---|---|---|
| G1 vs. G2 | −3.140 | 0.8608 | No | −12.45 to 6.170 |
| G1 vs. G3 | −14.21 | 3.896 | Yes | −23.52 to −4.900 |
| G2 vs. G3 | −11.07 | 3.035 | Yes | −20.38 to −1.760 |
| Group Comparison | Mean of Difference | t | Significant p < 0.05 | 95% Confidence Interval of Difference |
|---|---|---|---|---|
| G1 vs. G2 | −1.630 | 0.7889 | No | −6.904 to 3.644 |
| G1 vs. G3 | −5.970 | 2.889 | Yes | −11.24 to −0.6963 |
| G2 vs. G3 | −4.340 | 2.101 | No | −9.614 to 0.9337 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gehrke, S.A.; Eliers Treichel, T.L.; Pérez-Díaz, L.; Calvo-Guirado, J.L.; Aramburú Júnior, J.; Mazón, P.; de Aza, P.N. Impact of Different Titanium Implant Thread Designs on Bone Healing: A Biomechanical and Histometric Study with an Animal Model. J. Clin. Med. 2019, 8, 777. https://doi.org/10.3390/jcm8060777
Gehrke SA, Eliers Treichel TL, Pérez-Díaz L, Calvo-Guirado JL, Aramburú Júnior J, Mazón P, de Aza PN. Impact of Different Titanium Implant Thread Designs on Bone Healing: A Biomechanical and Histometric Study with an Animal Model. Journal of Clinical Medicine. 2019; 8(6):777. https://doi.org/10.3390/jcm8060777
Chicago/Turabian StyleGehrke, Sergio Alexandre, Tiago Luis Eliers Treichel, Letícia Pérez-Díaz, Jose Luis Calvo-Guirado, Jaime Aramburú Júnior, Patricia Mazón, and Piedad N. de Aza. 2019. "Impact of Different Titanium Implant Thread Designs on Bone Healing: A Biomechanical and Histometric Study with an Animal Model" Journal of Clinical Medicine 8, no. 6: 777. https://doi.org/10.3390/jcm8060777
APA StyleGehrke, S. A., Eliers Treichel, T. L., Pérez-Díaz, L., Calvo-Guirado, J. L., Aramburú Júnior, J., Mazón, P., & de Aza, P. N. (2019). Impact of Different Titanium Implant Thread Designs on Bone Healing: A Biomechanical and Histometric Study with an Animal Model. Journal of Clinical Medicine, 8(6), 777. https://doi.org/10.3390/jcm8060777









