The Effect of Donors’ Demographic Characteristics in Renal Function Post-Living Kidney Donation. Analysis of a UK Single Centre Cohort
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
Meeting Presentation
Abbreviations
| BMI | Body Mass Index |
| CKD-EPI | Chronic Kidney Disease Epidemiology Collaboration |
| ECD | Extended Criteria Donor |
| eGFR | estimated Glomerular Filtration Rate |
| ESRD | End Stage Renal Disease |
| LD | Living Donor |
| LRD | Living Related Donor |
| LURD | Living Unrelated Donor |
| RR | Relative Risk |
| WHO | World Health Organization |
References
- Shapiro, R. End-stage renal disease in 2010: Innovative approaches to improve outcomes in transplantation. Nat. Rev. Nephrol. 2011, 7, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, A.R.; Lafranca, J.A.; Claessens, L.A.; Imamdi, R.M.; IJzermans, J.N.; Betjes, M.G.; Dor, F.J. Shifting paradigms in eligibility criteria for live kidney donation: A systematic review. Kidney Int. 2015, 87, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Lafranca, J.A.; Hagen, S.M.; Dols, L.F.; Arends, L.R.; Weimar, W.; IJzermans, J.N.; Dor, F.J. Systematic review and meta-analysis of the relation between body mass index and short-term donor outcome of laparoscopic donor nephrectomy. Kidney Int. 2013, 83, 931–939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locke, J.E.; Reed, R.D.; Massie, A.; MacLennan, P.A.; Sawinski, D.; Kumar, V.; Segev, D.L. Obesity increases the risk of end-stage renal disease among living kidney donors. Kidney Int. 2017, 91, 699–703. [Google Scholar] [CrossRef] [PubMed]
- Naik, A.S.; Cibrik, D.M.; Sakhuja, A.; Samaniego, M.; Lu, Y.; Shahinian, V.; Lentine, K.L. Temporal trends, center-level variation, and the impact of prevalent state obesity rates on acceptance of obese living kidney donors. Am. J. Transplant. 2018, 18, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Bellini, M.I.; Koutroutsos, K.; Galliford, J.; Herbert, P.E. One-Year Outcomes of a Cohort of Renal Transplant Patients Related to BMI in a Steroid-Sparing Regimen. Transplant. Direct 2017, 3, e330. [Google Scholar] [CrossRef] [PubMed]
- Fehrman-Ekholm, I.; Norden, G.; Lennerling, A.; Rizell, M.; Mjornstedt, L.; Wramner, L.; Olausson, M. Incidence of end-stage renal disease among live kidney donors. Transplantation 2006, 82, 1646–1648. [Google Scholar] [CrossRef]
- Janki, S.; Dols, L.F.; Timman, R.; Mulder, E.E.; Dooper, I.M.; van de Wetering, J.; IJzermans, J.N. Five-year follow-up after live donor nephrectomy—Cross-sectional and longitudinal analysis of a prospective cohort within the era of extended donor eligibility criteria. Transpl. Int. Off. J. Eur. Soc. Organ Transplant. 2017, 30, 266–276. [Google Scholar] [CrossRef]
- Ibrahim, H.N.; Foley, R.; Tan, L.; Rogers, T.; Bailey, R.F.; Guo, H.; Matas, A.J. Long-term consequences of kidney donation. New Engl. J. Med. 2009, 360, 459–469. [Google Scholar] [CrossRef]
- Dols, L.F.; Kok, N.F.; Roodnat, J.I.; Tran, T.C.; Terkivatan, T.; Zuidema, W.C.; IJzermans, J.N.M. Living kidney donors: Impact of age on long-term safety. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2011, 11, 737–742. [Google Scholar] [CrossRef]
- Dols, L.F.; Weimar, W.; Ijzermans, J.N. Long-term consequences of kidney donation. New Engl. J. Med. 2009, 360, 2371–2372. [Google Scholar] [PubMed]
- Wainright, J.L.; Robinson, A.M.; Wilk, A.R.; Klassen, D.K.; Cherikh, W.S.; Stewart, D.E. Risk of ESRD in Prior Living Kidney Donors. Am. J. Transplant. 2018, 18, 1129–1139. [Google Scholar] [CrossRef] [PubMed]
- Unger, L.W.; Feka, J.; Sabler, P.; Rasoul-Rockenschaub, S.; Gyori, G.; Hofmann, M.; Salat, A. High BMI and male sex as risk factor for increased short-term renal impairment in living kidney donors—Retrospective analysis of 289 consecutive cases. Int. J. Surg. (Lond. Engl.) 2017, 46, 172–177. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, L.M.; Ramond, A.; Oliver-Williams, C.; Willeit, P.; Paige, E.; Trotter, P.; Evans, J.; Wadstrom, J.; Nicholson, M.; Collett, D.; Di Angelantonio, E. Mid- and Long-Term Health Risks in Living Kidney Donors: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2018, 20, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Massie, A.B.; Muzaale, A.D.; Luo, X.; Chow, E.K.H.; Locke, J.E.; Nguyen, A.Q.; Segev, D.L. Quantifying Postdonation Risk of ESRD in Living Kidney Donors. J. Am. Soc. Nephrol. JASN 2017, 28, 2749–2755. [Google Scholar] [CrossRef] [PubMed]
- Research Tissue Banks and Research Databases. Available online: https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/research-tissue-banks-and-research-databases/ (accessed on 19 November 2018).
- Metzger, R.A.; Delmonico, F.L.; Feng, S.; Port, F.K.; Wynn, J.J.; Merion, R.M. Expanded criteria donors for kidney transplantation. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2003, 3, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Gaillard, F.; Courbebaisse, M.; Kamar, N.; Rostaing, L.; Jacquemont, L.; Hourmant, M.; Janbon, B. Impact of estimation versus direct measurement of predonation glomerular filtration rate on the eligibility of potential living kidney donors. Kidney Int. 2019, 95, 896–904. [Google Scholar] [CrossRef]
- Transplant Activity Report. Available online: https://www.organdonation.nhs.uk/supporting-my-decision/statistics-about-organ-donation/transplant-activity-report/ (accessed on 15 March 2019).
- Von Zur-Muhlen, B.; Berglund, D.; Yamamoto, S.; Wadstrom, J. Single-centre long-term follow-up of live kidney donors demonstrates preserved kidney function but the necessity of a structured lifelong follow-up. Upsala J. Med. Sci. 2014, 119, 236–241. [Google Scholar] [CrossRef]
- Mjoen, G.; Hallan, S.; Hartmann, A.; Foss, A.; Midtvedt, K.; Oyen, O.; Line, P.D. Long-term risks for kidney donors. Kidney Int. 2014, 86, 162–167. [Google Scholar] [CrossRef] [Green Version]
- Kiberd, B.A.; Tennankore, K.K. Lifetime risks of kidney donation: A medical decision analysis. BMJ Open 2017, 7, e016490. [Google Scholar] [CrossRef]
- Stevens, L.A.; Coresh, J.; Greene, T.; Levey, A.S. Assessing kidney function—Measured and estimated glomerular filtration rate. New Engl. J. Med. 2006, 354, 2473–2483. [Google Scholar] [CrossRef] [PubMed]
- Grams, M.E.; Sang, Y.; Levey, A.S.; Matsushita, K.; Ballew, S.; Chang, A.R.; Shalev, V. Kidney-Failure Risk Projection for the Living Kidney-Donor Candidate. New Engl. J. Med. 2016, 374, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Bellini, M.I.; Paoletti, F.; Herbert, P.E. Obesity and bariatric intervention in patients with chronic renal disease. J. Int. Med. Res. 2019, 300060519843755. [Google Scholar] [CrossRef] [PubMed]
- British Transplant Society. Guidelines for Living Donor Kidney Transplantation, 4th ed.; British Transplant Society: Macclesfield, UK, 2018. [Google Scholar]
- Haugen, A.J.; Langberg, N.E.; Dahle, D.O.; Pihlstrøm, H.; Birkeland, K.I.; Reisaeter, A.; Midtvedt, K.; Hartmann, A.; Holdaas, H.; Mjøen, G. Long-term risk for kidney donors with hypertension at donation—A retrospective cohort study. Transpl. Int. 2019. [Google Scholar] [CrossRef] [PubMed]
- Matas, A.J. Transplantation: Increased ESRD and mortality risk for kidney donors? Nat. Rev. Nephrol. 2014, 10, 130–131. [Google Scholar] [CrossRef] [PubMed]
- Muzaale, A.D.; Massie, A.B.; Anjum, S.; Liao, C.; Garg, A.X.; Lentine, K.L.; Segev, D.L. Recipient Outcomes Following Transplantation of Allografts from Live Kidney Donors Who Subsequently Developed End-Stage Renal Disease. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transplant. Surg. 2016, 16, 3532–3539. [Google Scholar] [CrossRef] [PubMed]
- Lei, H.H.; Perneger, T.V.; Klag, M.J.; Whelton, P.K.; Coresh, J. Familial aggregation of renal disease in a population-based case-control study. J. Am. Soc. Nephrol. Jasn. 1998, 9, 1270–1276. [Google Scholar]
- O’Dea, D.F.; Murphy, S.W.; Hefferton, D.; Parfrey, P.S. Higher risk for renal failure in first-degree relatives of white patients with end-stage renal disease: A population-based study. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 1998, 32, 794–801. [Google Scholar] [CrossRef]
- Skrunes, R.; Svarstad, E.; Reisaeter, A.V.; Vikse, B.E. Familial clustering of ESRD in the Norwegian population. Clin. J. Am. Soc. Nephrol. CJASN 2014, 9, 1692–1700. [Google Scholar] [CrossRef]
- Lentine, K.L.; Schnitzler, M.A.; Garg, A.X.; Xiao, H.; Axelrod, D.; Tuttle-Newhall, J.E.; Segev, D.L. Race, Relationship and Renal Diagnoses After Living Kidney Donation. Transplantation 2015, 99, 1723–1729. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, C.L.; Gross, C.R.; Messersmith, E.E.; Hong, B.A.; Gillespie, B.W.; Hill-Callahan, P.; Odim, J. Emotional and Financial Experiences of Kidney Donors over the Past 50 Years: The RELIVE Study. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 2221–2231. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| eGFR Donation | |||
|---|---|---|---|
| Mean ± St. Dev. | p Value | Table N % | |
| Sex | |||
| Female | 87 ± 22 | <0.001 | 57 |
| Male | 95 ± 32 | 43 | |
| Ethnicity | |||
| Asian | 91 ± 19 | <0.001 | 25 |
| African | 103 ± 23 | 15 | |
| Caucasian | 87 ± 28 | 60 | |
| Graft Type | |||
| LRD | 91 ± 26 | 0.94 | 56 |
| LURD | 90 ± 29 | 44 | |
| Age (years) | 46 ± 13 | 100 | |
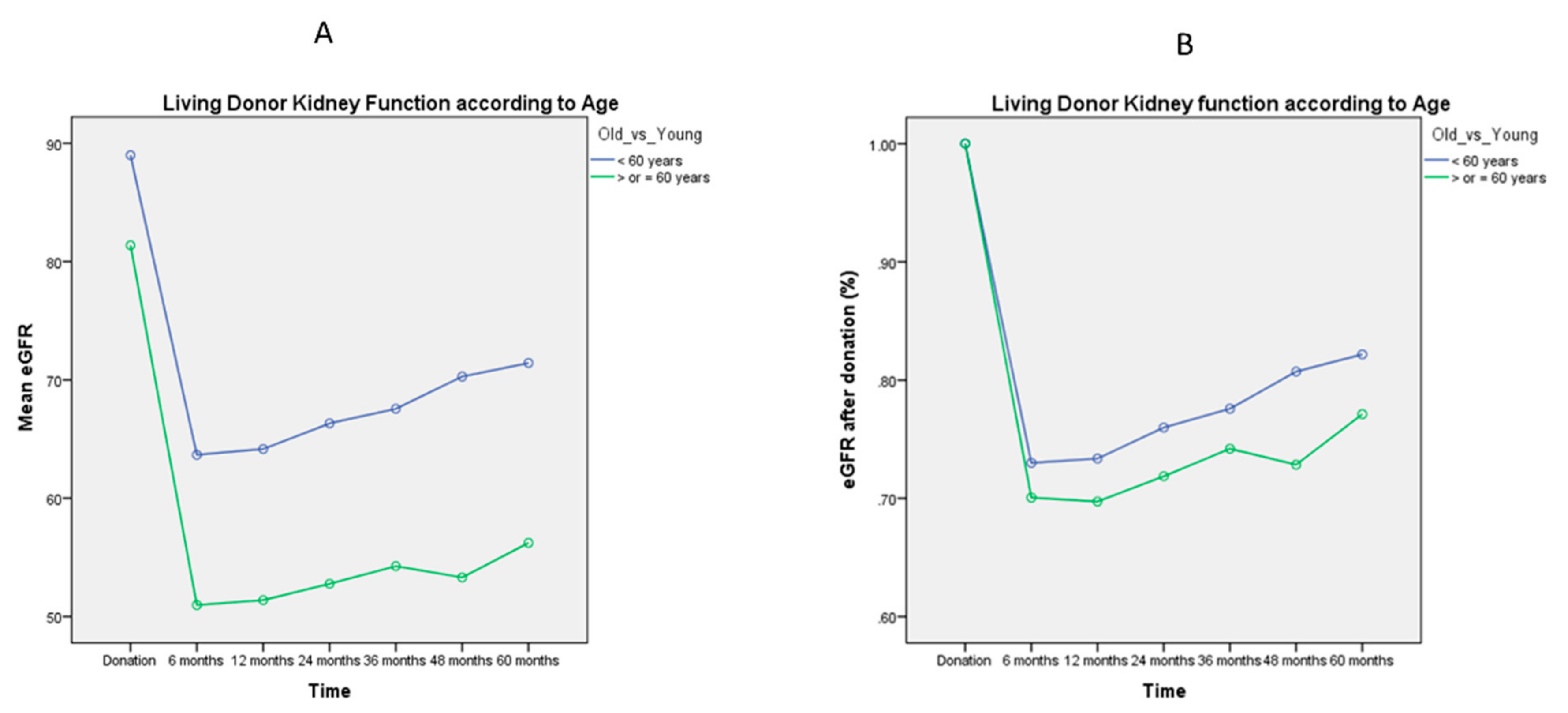
| < 60 years | 93 ± 24 | <0.001 | 85 |
| > or = 60 years | 80 ± 39 | 15 | |
| WHO classification BMI (kg/m2) | 27 ± 5 | 100 | |
| BMI < 25 | 92 ± 29 | 0.5 | 36 |
| 25 < or = BMI < or = 29 | 91 ± 30 | 38 | |
| BMI > or = 30 | 89 ± 20 | 26 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellini, M.I.; Charalampidis, S.; Stratigos, I.; Dor, F.J.M.F.; Papalois, V. The Effect of Donors’ Demographic Characteristics in Renal Function Post-Living Kidney Donation. Analysis of a UK Single Centre Cohort. J. Clin. Med. 2019, 8, 883. https://doi.org/10.3390/jcm8060883
Bellini MI, Charalampidis S, Stratigos I, Dor FJMF, Papalois V. The Effect of Donors’ Demographic Characteristics in Renal Function Post-Living Kidney Donation. Analysis of a UK Single Centre Cohort. Journal of Clinical Medicine. 2019; 8(6):883. https://doi.org/10.3390/jcm8060883
Chicago/Turabian StyleBellini, Maria Irene, Sotiris Charalampidis, Ioannis Stratigos, Frank J.M.F. Dor, and Vassilios Papalois. 2019. "The Effect of Donors’ Demographic Characteristics in Renal Function Post-Living Kidney Donation. Analysis of a UK Single Centre Cohort" Journal of Clinical Medicine 8, no. 6: 883. https://doi.org/10.3390/jcm8060883
APA StyleBellini, M. I., Charalampidis, S., Stratigos, I., Dor, F. J. M. F., & Papalois, V. (2019). The Effect of Donors’ Demographic Characteristics in Renal Function Post-Living Kidney Donation. Analysis of a UK Single Centre Cohort. Journal of Clinical Medicine, 8(6), 883. https://doi.org/10.3390/jcm8060883








