Early Parental Death and Risk of Psychosis in Offspring: A Six-Country Case-Control Study
Abstract
1. Introduction
2. Experimental Section
2.1. Study Population
2.2. Variables
2.2.1. Case/Control Status
2.2.2. Early Parental Death
2.2.3. Ethnic Group
2.2.4. Other Variables
2.3. Statistical Analysis
3. Results
3.1. Prevalence of Early Parental Death
3.2. Early Parental Death and Odds of Psychosis
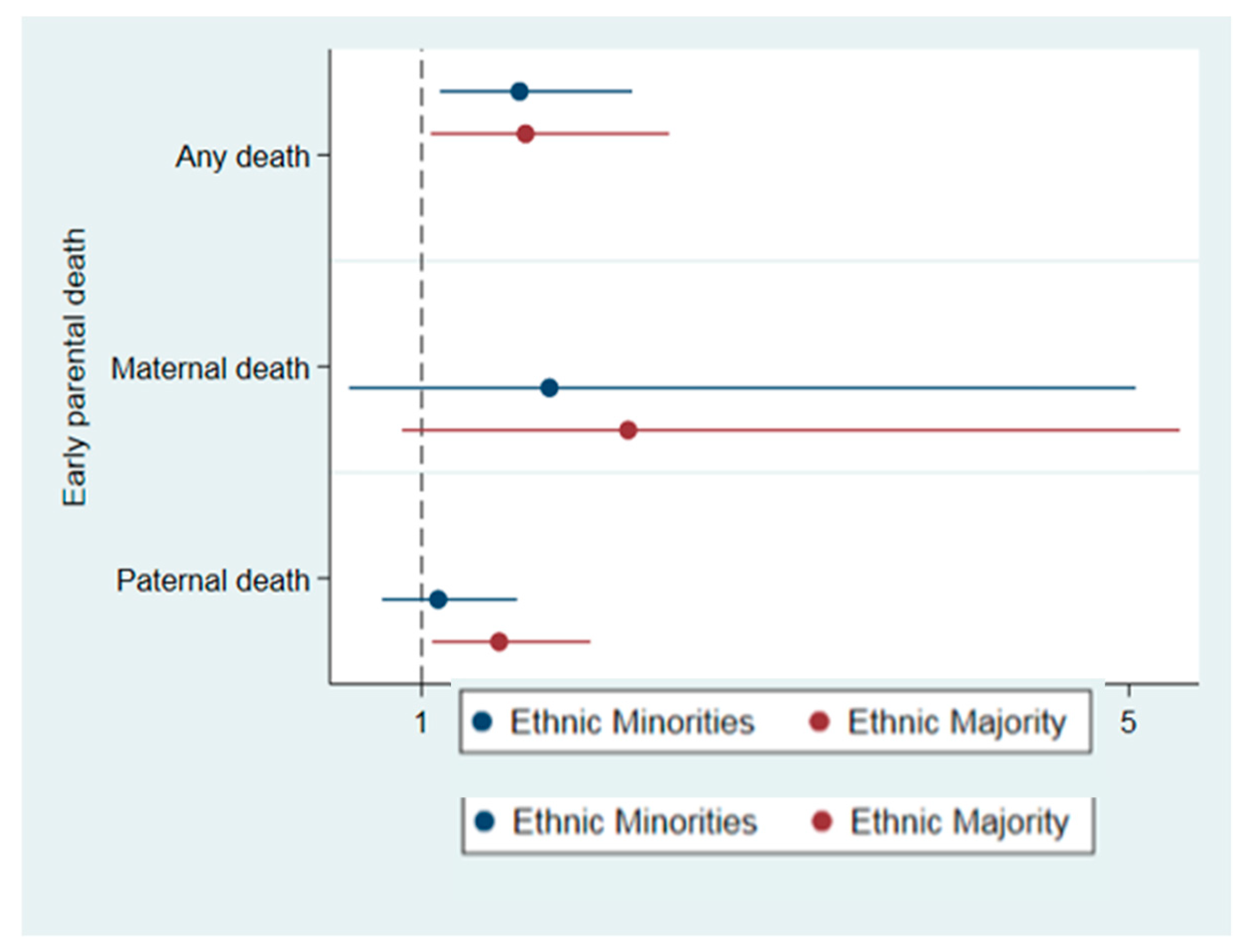
3.3. Differences by Ethnic Group
4. Discussion
4.1. Type and Timing of Early Parental Death
4.1.1. Maternal versus Paternal Death
4.1.2. Single versus Both Deaths
4.1.3. Child’s Age at Parental Death
4.2. Differences by Ethnic Group
4.3. Limitations
4.4. Implications
4.4.1. Cascading Consequences
4.4.2. Investigating Inequities
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Granville-Grossman, K.L. Early Bereavement and Schizophrenia. Br. J. Psychiatry 1966, 112, 1027–1034. [Google Scholar] [CrossRef]
- Varese, F.; Smeets, F.; Drukker, M.; Lieverse, R.; Lataster, T.; Viechtbauer, W.; Read, J.; Van Os, J.; Bentall, R.P. Childhood Adversities Increase the Risk of Psychosis: A Meta-analysis of Patient-Control, Prospective- and Cross-sectional Cohort Studies. Schizophr. Bull. 2012, 38, 661–671. [Google Scholar] [CrossRef]
- Stilo, S.A.; Gayer-Anderson, C.; Beards, S.; Hubbard, K.; Onyejiaka, A.; Keraite, A.; Borges, S.; Mondelli, V.; Dazzan, P.; Pariante, C.; et al. Further evidence of a cumulative effect of social disadvantage on risk of psychosis. Psychol. Med. 2017, 47, 913–924. [Google Scholar] [CrossRef]
- Abel, K.M.; Heuvelman, H.P.; Jorgensen, L.; Magnusson, C.; Wicks, S.; Susser, E.; Hallkvist, J.; Dalman, C. Severe bereavement stress during the prenatal and childhood periods and risk of psychosis in later life: Population based cohort study. BMJ 2014, 348, 7679. [Google Scholar] [CrossRef]
- Clarke, M.C.; Tanskanen, A.; Huttunen, M.O.; Cannon, M. Sudden death of father or sibling in early childhood increases risk for psychotic disorder. Schizophr. Res. 2013, 143, 363–366. [Google Scholar] [CrossRef]
- Class, Q.A.; Abel, K.M.; Khashan, A.S.; Rickert, M.E.; Dalman, C.; Larsson, H.; Hultman, C.M.; Långström, N.; Lichtenstein, P.; D’Onofrio, B.M. Offspring psychopathology following preconception, prenatal and postnatal maternal bereavement stress. Psychol. Med. 2014, 44, 71–84. [Google Scholar] [CrossRef]
- Laursen, T.M.; Munk-Olsen, T. A Comparison of Selected Risk Factors for Unipolar Depressive Disorder, Bipolar Affective Disorder, Schizoaffective Disorder, and Schizophrenia from a Danish Population-Based Cohort. J. Clin. Psychiatry 2007, 68, 1673–1681. [Google Scholar] [CrossRef]
- Liang, H.; Olsen, J.; Yuan, W.; Cnattingus, S.; Vestergaard, M.; Obel, C.; Gissler, M.; Li, J. Early life bereavement and schizophrenia: A nationwide cohort study in Denmark and Sweden. Medicine 2016, 95, 1–8. [Google Scholar] [CrossRef]
- Sørensen, H.J.; Nielsen, P.R.; Pedersen, C.B.; Benros, M.E.; Nordentoft, M.; Mortensen, P.B. Population impact of familial and environmental risk factors for schizophrenia: A nationwide study. Schizophr. Res. 2014, 153, 214–219. [Google Scholar] [CrossRef]
- Wilcox, H.C.; Kuramoto, S.J.; Lichtenstein, P.; Langström, N.; Brent, D.A.; Runeson, B. Psychiatric Morbidity, Violent Crime, and Suicide Among Children and Adolescents Exposed to Parental Death. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 514–523. [Google Scholar]
- 1Agid, O.; Shapira, B.; Zislin, J.; Ritsner, M.; Hanin, B.; Murad, H.; Troudart, T.; Bloch, M.; Heresco-Levy, U.; Lerer, B. Environment and vulnerability to major psychiatric illness: A case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol. Psychiatry 1999, 4, 163–172. [Google Scholar]
- Birtchnell, J. Is there a scientifically acceptable alternative to the epidemiological study of familial factors in mental illness? Soc. Sci. Med. (1967) 1974, 8, 335–350. [Google Scholar] [CrossRef]
- Dowdney, L. Annotation: Childhood Bereavement Following Parental Death. J. Child Psychol. Psychiatry 2000, 41, 819–830. [Google Scholar] [CrossRef]
- Finkelstein, H. The long-term effects of early parent death: A review. J. Clin. Psychol. 1988, 44, 3–9. [Google Scholar] [CrossRef]
- Furukawa, T.; Mizukawa, R.; Hirai, T.; Fujihara, S.; Kitamura, T.; Takahashi, K. Childhood parental loss and schizophrenia: Evidence against pathogenic but for some pathoplastic effects. Psychiatry Res. 1998, 81, 353–362. [Google Scholar] [CrossRef]
- Jacobs, J.R.; Bovasso, G.B. Re-Examining the Long-Term Effects of Experiencing Parental Death in Childhood on Adult Psychopathology. J. Nerv. Ment. Dis. 2009, 197, 24–27. [Google Scholar] [CrossRef]
- Ragan, P.V.; McGlashan, T.H. Childhood parental death and adult psychopathology. Am. J. Psychiatry 1986, 143, 153–157. [Google Scholar]
- Schiffman, J.; Abrahamson, A.; Cannon, T.; Labrie, J.; Parnas, J.; Schulsinger, F.; Mednick, S. Early Rearing Factors in Schizophrenia. Int. J. Ment. Heal. 2001, 30, 3–16. [Google Scholar] [CrossRef]
- Tennant, C.; Bebbington, P.; Hurry, J. Parental death in childhood and risk of adult depressive disorders: A review. Psychol. Med. 1980, 10, 289–299. [Google Scholar] [CrossRef]
- Tremblay, G.C.; Israel, A.C. Children’s adjustment to parental death. Clin. Psychol. Sci. Pract. 1998, 5, 424–438. [Google Scholar] [CrossRef]
- Watt, N.F.; Nicholi, A. Early death of a parent as an etiological factor in schizophrenia. Am. J. Orthopsychiatry 1979, 49, 465–473. [Google Scholar] [CrossRef]
- Luecken, L.J.; Roubinov, D.S. Pathways to Lifespan Health Following Childhood Parental Death. Soc. Pers. Psychol. Compass 2012, 6, 243–257. [Google Scholar] [CrossRef]
- Morgan, C.; Kirkbride, J.; Leff, J.; Craig, T.; Hutchinson, G.; McKenzie, K.; Morgan, K.; Dazzan, P.; Doody, G.A.; Jones, P.; et al. Parental separation, loss and psychosis in different ethnic groups: A case-control study. Psychol. Med. 2007, 37, 495–503. [Google Scholar] [CrossRef]
- Cantor-Graae, E.; Selten, J.-P. Schizophrenia and Migration: A Meta-Analysis and Review. Am. J. Psychiatry 2005, 162, 12–24. [Google Scholar] [CrossRef]
- Jongsma, H.E.; Gayer-Anderson, C.; Lasalvia, A.; Quattrone, D.; Mulè, A.; Szöke, A.; Selten, J.; et al. Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry 2018, 75, 36–46. [Google Scholar] [CrossRef]
- Leaune, E.; Dealberto, M.J.; Luck, D.; Grot, S.; Zeroug-Vial, H.; Poulet, E.; Brunelin, J. Ethnic minority position and migrant status as risk factors for psychotic symptoms in the general population: A meta-analysis. Psychol. Med. 2019, 49, 545–558. [Google Scholar] [CrossRef]
- McGrath, J.; Saha, S.; Welham, J.; El Saadi, O.; MacCauley, C.; Chant, D. A systematic review of the incidence of schizophrenia: The distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004, 2, 13. [Google Scholar] [CrossRef]
- Umberson, D.; Olson, J.S.; Crosnoe, R.; Liu, H.; Pudrovska, T.; Donnelly, R. Death of family members as an overlooked source of racial disadvantage in the United States. Proc. Natl. Acad. Sci. USA 2017, 114, 915–920. [Google Scholar] [CrossRef]
- Umberson, D. Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors. J. Heal. Soc. Behav. 2017, 58, 405–420. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and health: Evidence and needed research. Annu Rev Public Health 2019, 40, 1–21. [Google Scholar] [CrossRef]
- Di Forti, M.; Quattrone, D.; Freeman, T.P.; Tripoli, G.; Gayer-Anderson, C.; Quigley, H.; Rodriguez, V.; E Jongsma, H.; Ferraro, L.; La Cascia, C.; et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): A multicentre case-control study. Lancet Psychiatry 2019, 6, 427–436. [Google Scholar] [CrossRef]
- Bifulco, A.; Brown, G.W.; Harris, T.O. Childhood Experience of Care and Abuse (CECA): A Retrospective Interview Measure. J. Child Psychol. Psychiatry 1994, 35, 1419–1435. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: Station, TX, USA.
- Bowlby, J. Attachment and loss: Retrospect and prospect. Am. J. Orthopsychiatry 1982, 52, 664–678. [Google Scholar] [CrossRef] [PubMed]
- Birtchnell, J. The interrelationship between social class, early parent death, and mental illness. Psychol. Med. 1972, 2, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.M.; Bhavsar, V.; Tripoli, G.; Howes, O. 30 Years on: How the Neurodevelopmental Hypothesis of Schizophrenia Morphed Into the Developmental Risk Factor Model of Psychosis. Schizophr. Bull. 2017, 43, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Schut, H.; Stroebe, W. Health outcomes of bereavement. Lancet 2007, 370, 1960–1973. [Google Scholar] [CrossRef]
- Dopp, A.R.; Cain, A.C. The role of peer relationships in parental bereavement during childhood and adolescence. Death Stud. 2012, 36, 41–60. [Google Scholar] [CrossRef]
- Rostila, M. Commentary: Childhood parental loss and adulthood health: Discussing the role of parental cause of death, child’s age at death and historical context. Soc. Sci. Med. 2015, 131, 190–192. [Google Scholar] [CrossRef]
- Hjorthøj, C.; Stürup, A.E.; McGrath, J.J.; Nordentoft, M. Years of potential life lost and life expectancy in schizophrenia: A systematic review and meta-analysis. Lancet Psychiatry 2017, 4, 295–301. [Google Scholar] [CrossRef]
- Laursen, T.M.; Munk-Olsen, T.; Gasse, C. Chronic Somatic Comorbidity and Excess Mortality Due to Natural Causes in Persons with Schizophrenia or Bipolar Affective Disorder. PLoS ONE 2011, 6, e24597. [Google Scholar] [CrossRef]
- Laursen, T.M.; Nordentoft, M.; Mortensen, P.B. Excess Early Mortality in Schizophrenia. Annu. Rev. Clin. Psychol. 2014, 10, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, P.; Gondek, T.M.; Królicka-Deręgowska, A.; Misiak, B.; Adamowski, T.; Kiejna, A. CAUSES OF MORTALITY IN SCHIZOPHRENIA: AN UPDATED REVIEW OF EUROPEAN STUDIES. Psychiatr. Danub. 2017, 29, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R. Stress and the Mental Health of Populations of Color: Advancing Our Understanding of Race-related Stressors. J. Heal. Soc. Behav. 2018, 59, 466–485. [Google Scholar] [CrossRef] [PubMed]
- Pearlin, L.I.; Schieman, S.; Fazio, E.M.; Meersman, S.C. Stress, Health, and the Life Course: Some Conceptual Perspectives. J. Heal. Soc. Behav. 2005, 46, 205–219. [Google Scholar] [CrossRef]

| All (n = 2549) | Case vs. Control (n = 1072 Cases) | Minority vs. Majority (n = 698 Minorities) | ||||||
|---|---|---|---|---|---|---|---|---|
| Total n | Total % | Case % | Control % | p-Value | Min % | Maj % | p-Value | |
| Catchment site | ||||||||
| London | 416 | 16.3 | 17.7 | 15.3 | 30.5 | 11.0 | ||
| Cambridge | 150 | 5.9 | 4.1 | 7.2 | 2.3 | 7.2 | ||
| Amsterdam | 195 | 7.7 | 8.8 | 6.8 | 13.3 | 5.5 | ||
| Gouda/Voorhout | 209 | 8.2 | 9.3 | 7.4 | 2.7 | 10.3 | ||
| Madrid | 77 | 3.0 | 3.6 | 2.6 | 1.6 | 3.6 | ||
| Barcelona | 67 | 2.6 | 2.9 | 2.4 | 0.7 | 3.4 | ||
| Oviedo | 78 | 3.1 | 3.6 | 2.6 | 1.9 | 3.5 | ||
| Valencia | 80 | 3.1 | 4.6 | 2.1 | 1.1 | 3.9 | ||
| Créteil | 152 | 6.0 | 5.0 | 6.6 | 11.0 | 4.1 | ||
| Puy de Dôme | 61 | 2.4 | 1.4 | 3.1 | 0.7 | 3.0 | ||
| Bologne | 132 | 5.2 | 6.3 | 4.3 | 2.4 | 6.2 | ||
| Palermo | 155 | 6.1 | 5.1 | 6.8 | 1.6 | 7.8 | ||
| Ribeirão Preto | 492 | 19.3 | 17.8 | 20.4 | 28.5 | 15.8 | ||
| Santiago | 66 | 2.6 | 2.6 | 2.6 | 0.1 | 3.5 | ||
| Verona | 163 | 6.4 | 5.3 | 7.2 | 0.6 | 8.6 | ||
| Cuenca | 56 | 2.2 | 1.7 | 2.6 | 0.9 | 2.7 | ||
| Age at assessment * | 34.0 (12.2) | 31.3 (10.6) | 36.1 (12.9) | <0.001 | 31.4 (10.9) | 35.0 (12.5) | <0.001 | |
| Sex | ||||||||
| Female | 1193 | 46.8 | 38.4 | 52.9 | <0.001 | 45.7 | 47.2 | 0.487 |
| Male | 1356 | 53.2 | 61.6 | 47.1 | 54.3 | 52.8 | ||
| Ethnicity | ||||||||
| White | 1850 | 72.6 | 64.3 | 78.7 | <0.001 | 100 | 0 | <0.001 |
| Black | 282 | 11.1 | 15.3 | 8.0 | 0 | 40.4 | ||
| Mixed | 223 | 8.8 | 10.0 | 7.9 | 0 | 31.9 | ||
| Asian | 66 | 2.6 | 3.1 | 2.2 | 0 | 9.5 | ||
| North African | 69 | 2.7 | 4.2 | 1.6 | 0 | 9.9 | ||
| Another | 58 | 2.3 | 3.2 | 1.6 | 0 | 8.3 | ||
| Parental psychosis | ||||||||
| No | 2181 | 96.0 | 92.8 | 98.3 | <0.001 | 95.8 | 96.1 | 0.741 |
| Yes | 90 | 4.0 | 7.2 | 1.7 | 4.2 | 3.9 | ||
| Parental death | ||||||||
| No | 2331 | 91.5 | 89.4 | 93.0 | <0.001 | 86.5 | 93.4 | <0.001 |
| Yes | 218 | 8.5 | 10.6 | 7.0 | 13.5 | 6.6 | ||
| Type of death | ||||||||
| Mother | 60 | 2.4 | 3.3 | 1.7 | 0.005 | 3.6 | 1.9 | <0.001 |
| Father | 158 | 5.4 | 6.2 | 4.8 | 7.7 | 4.4 | ||
| Both | 21 | 0.8 | 1.2 | 0.5 | 2.2 | 0.3 | ||
| Child’s age | ||||||||
| Age in years * | 8.92 (5.11) | 9.32 (5.14) | 8.49 (5.06) | 0.236 | 9.37 (5.21) | 8.52 (5.00) | 0.226 | |
| 0–5 years | 62 | 29.0 | 26.1 | 32.0 | 0.133 | 26.4 | 31.2 | 0.338 |
| 6–10 years | 58 | 27.1 | 23.4 | 31.1 | 24.2 | 29.5 | ||
| 11–16 years | 94 | 43.9 | 50.5 | 36.9 | 49.4 | 39.3 | ||
| Unadjusted | Age- and Sex-Adjusted | Fully Adjusted * | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Parental death | |||||||||
| No | Reference | Reference | Reference | ||||||
| Yes | 1.37 | 1.09, 1.72 | 0.007 | 1.63 | 1.33, 1.99 | <0.001 | 1.54 | 1.23, 1.92 | <0.001 |
| Type of death | |||||||||
| Mother | 1.81 | 0.89, 3.71 | 0.103 | 2.02 | 1.03, 3.95 | 0.041 | 2.27 | 1.18, 4.37 | 0.001 |
| Father | 1.12 | 0.89, 1.43 | 0.330 | 1.33 | 1.02, 1.72 | 0.034 | 1.14 | 0.79, 1.64 | 0.481 |
| Both | 2.37 | 1.14, 4.94 | 0.022 | 3.80 | 2.47, 5.83 | <0.001 | 4.42 | 2.57, 7.60 | <0.001 |
| Child’s age | |||||||||
| 0–5 years | Reference | Reference | Reference | ||||||
| 5–10 years | 0.85 | 0.37, 1.98 | 0.713 | 0.96 | 0.45, 2.07 | 0.924 | 1.26 | 0.53, 3.00 | 0.597 |
| 11–16 years | 1.68 | 0.76, 3.72 | 0.202 | 1.88 | 1.03, 3.45 | 0.040 | 2.03 | 1.02, 4.04 | 0.044 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misra, S.; Gelaye, B.; Koenen, K.C.; Williams, D.R.; Borba, C.P.C.; Quattrone, D.; Di Forti, M.; La Cascia, C.; La Barbera, D.; Tarricone, I.; et al. Early Parental Death and Risk of Psychosis in Offspring: A Six-Country Case-Control Study. J. Clin. Med. 2019, 8, 1081. https://doi.org/10.3390/jcm8071081
Misra S, Gelaye B, Koenen KC, Williams DR, Borba CPC, Quattrone D, Di Forti M, La Cascia C, La Barbera D, Tarricone I, et al. Early Parental Death and Risk of Psychosis in Offspring: A Six-Country Case-Control Study. Journal of Clinical Medicine. 2019; 8(7):1081. https://doi.org/10.3390/jcm8071081
Chicago/Turabian StyleMisra, Supriya, Bizu Gelaye, Karestan C. Koenen, David R. Williams, Christina P.C. Borba, Diego Quattrone, Marta Di Forti, Caterina La Cascia, Daniele La Barbera, Ilaria Tarricone, and et al. 2019. "Early Parental Death and Risk of Psychosis in Offspring: A Six-Country Case-Control Study" Journal of Clinical Medicine 8, no. 7: 1081. https://doi.org/10.3390/jcm8071081
APA StyleMisra, S., Gelaye, B., Koenen, K. C., Williams, D. R., Borba, C. P. C., Quattrone, D., Di Forti, M., La Cascia, C., La Barbera, D., Tarricone, I., Berardi, D., Szöke, A., Arango, C., Tortelli, A., de Haan, L., Velthorst, E., Bobes, J., Bernardo, M., Sanjuán, J., ... Morgan, C. (2019). Early Parental Death and Risk of Psychosis in Offspring: A Six-Country Case-Control Study. Journal of Clinical Medicine, 8(7), 1081. https://doi.org/10.3390/jcm8071081





