Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain
Abstract
1. Introduction
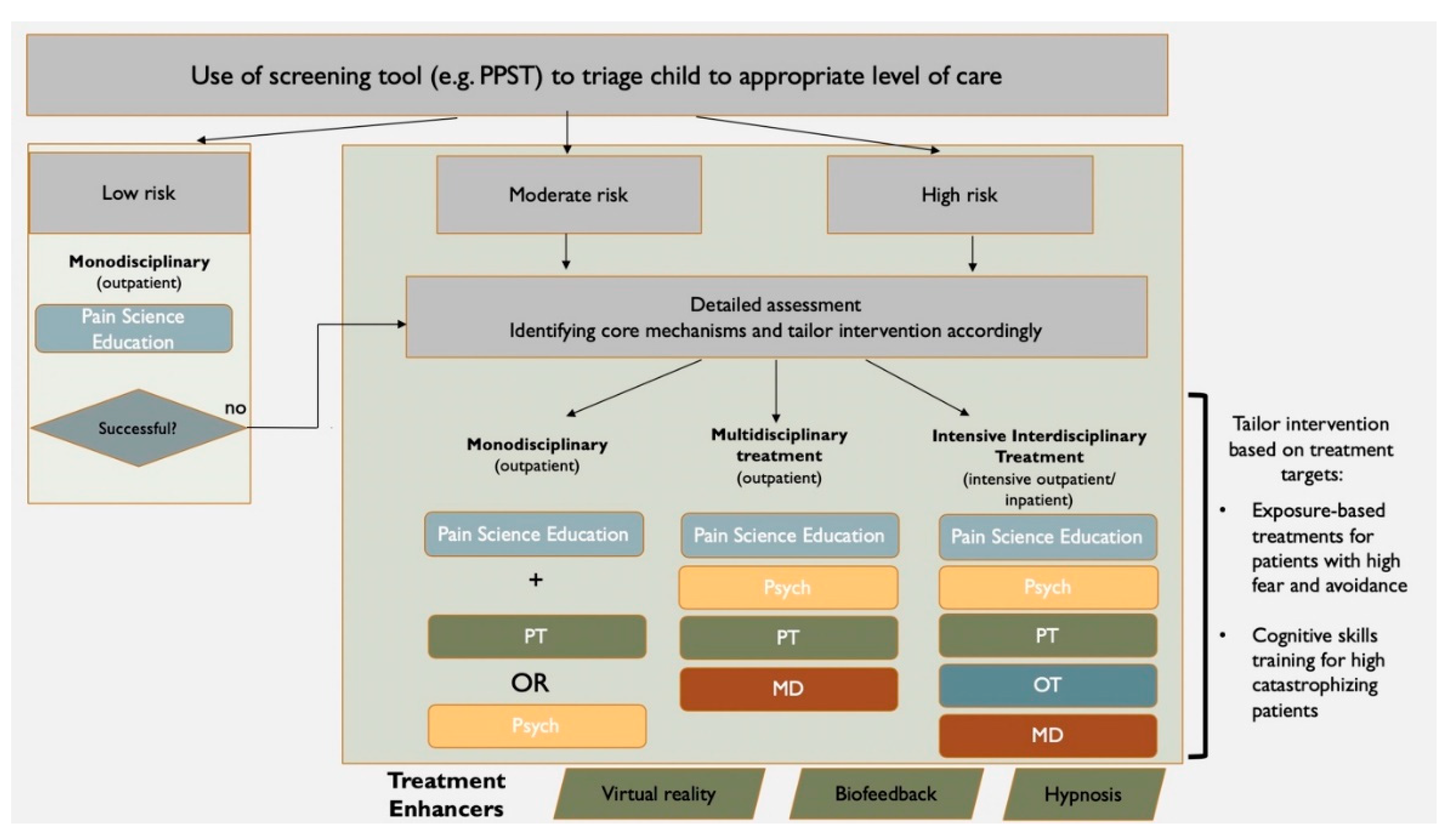
2. State of the Art of Rehabilitation for Pediatric Chronic Pain
2.1. Pain Related Education
Pain Science Education
2.2. Physiological Self-Regulation Training
Mindfulness-Based Stress Reduction and Yoga
2.3. Cognitive Skills Training
2.4. Behavioral Exposure
2.5. Parent Coaching
2.6. Physical Therapy
2.7. Occupational Therapy
2.8. Addressing Comorbidities
2.9. Interdisciplinary Outpatient Pain Treatment
2.10. Intensive Interdisciplinary Pain Treatment
2.11. Emerging Pain Treatment Intervention Formats
2.12. Summary of Rehabilitative Treatments for Pediatric Chronic Pain
3. Promising Directions for Clinical Practice
4. Promising Directions for Research
5. Conclusions
Key Messages
- Comprehensive multidisciplinary and interdisciplinary treatment based on behavioral medicine approaches are needed for children and adolescents with persistent pain.
- Pain Science Education is commonly implemented with several resources currently available, yet evidence for its use is scarce.
- Unique to pediatric rehabilitative approaches is the emphasis on including parents to optimize treatment outcomes.
- Innovative pain treatment intervention formats such as mobile applications and virtual reality enhance the delivery and reach of evidence-based tools.
- Comprehensive multidisciplinary/interdisciplinary treatment based on contemporary understanding of pain (neuro) science are needed for children and adolescents with persistent pain.
Author Contributions
Funding
Conflicts of Interest
References
- Huguet, A.; Miro, J. The severity of chronic pediatric pain: An epidemiological study. J. Pain 2008, 9, 226–236. [Google Scholar] [CrossRef]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M. Impact of recurrent and chronic pain on child and family daily functioning: A critical review of the literature. J. Dev. Behav. Pediatr. 2000, 21, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The biopsychosocial model and the education of health professionals. Ann. N. Y. Acad. Sci. 1978, 310, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Revivo, G.; Amstutz, D.K.; Gagnon, C.M.; McCormick, Z.L. Interdisciplinary Pain Management Improves Pain and Function in Pediatric Patients with Chronic Pain Associated with Joint Hypermobility Syndrome. PM R 2019, 11, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Wren, A.A.; Ross, A.C.; D’Souza, G.; Almgren, C.; Feinstein, A.; Marshall, A.; Golianu, B. Multidisciplinary Pain Management for Pediatric Patients with Acute and Chronic Pain: A Foundational Treatment Approach When Prescribing Opioids. Children (Basel) 2019, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Clinch, J.; Eccleston, C. Chronic musculoskeletal pain in children: Assessment and management. Rheumatology (Oxford) 2009, 48, 466–474. [Google Scholar] [CrossRef]
- Odell, S.; Logan, D.E. Pediatric pain management: The multidisciplinary approach. J. Pain Res. 2013, 6, 785–790. [Google Scholar] [CrossRef]
- Simons, L.E.; Logan, D.E.; Chastain, L.; Cerullo, M. Engagement in multidisciplinary interventions for pediatric chronic pain: Parental expectations, barriers, and child outcomes. Clin. J. Pain 2010, 26, 291–299. [Google Scholar] [CrossRef]
- Palermo, T.M. Cognitive Behaioral Therapy for Chronic Pain in Children and Adolescents; Oxford Press: New York, NY, USA, 2012. [Google Scholar]
- Williams, A.C.; Eccleston, C.; Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2012, 11, CD007407. [Google Scholar] [CrossRef]
- Simons, L.E.; Basch, M.C. State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain Manag. 2016, 6, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Palermo, T.M.; Williams, A.C.; Lewandowski Holley, A.; Morley, S.; Fisher, E.; Law, E. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef]
- Fisher, E.; Heathcote, L.C.; Palermo, T.M.; Williams, A.C.; Lau, J.; Eccleston, C. Systematic review and meta-analysis of psychological therapies for children with chronic pain. J. Pediatr. Psychol. 2014, 39, 763–782. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Eccleston, C.; Lewandowski, A.S.; Williams, A.C.; Morley, S. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: An updated meta-analytic review. Pain 2010, 148, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Sieberg, C.B.; Smith, A.; White, M.; Manganella, J.; Sethna, N.; Logan, D.E. Changes in Maternal and Paternal Pain-Related Attitudes, Behaviors, and Perceptions across Pediatric Pain Rehabilitation Treatment: A Multilevel Modeling Approach. J. Pediatr. Psychol. 2017, 42, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Celedon, X.; Amari, A.; Ward, C.; Prestwich, S.; Slifer, K.J. Children and adolescents with chronic pain and functional disability: Use of a behavioral rehabilitation approach. Curr. Phys. Med. Rehabil. Rep. 2014, 2, 86–92. [Google Scholar] [CrossRef]
- De Blecourt, A.C.; Schiphorst Preuper, H.R.; Van Der Schans, C.P.; Groothoff, J.W.; Reneman, M.F. Preliminary evaluation of a multidisciplinary pain management program for children and adolescents with chronic musculoskeletal pain. Disabil. Rehabil. 2008, 30, 13–20. [Google Scholar] [CrossRef]
- Hechler, T.; Kanstrup, M.; Holley, A.L.; Simons, L.E.; Wicksell, R.; Hirschfeld, G.; Zernikow, B. Systematic Review on Intensive Interdisciplinary Pain Treatment of Children With Chronic Pain. Pediatrics 2015, 136, 115–127. [Google Scholar] [CrossRef]
- Simons, L.E.; Sieberg, C.B.; Conroy, C.; Randall, E.T.; Shulman, J.; Borsook, D.; Berde, C.; Sethna, N.F.; Logan, D.E. Children with Chronic Pain: Response Trajectories after Intensive Pain Rehabilitation Treatment. J. Pain 2018, 19, 207–218. [Google Scholar] [CrossRef]
- Landry, B.W.; Fischer, P.R.; Driscoll, S.W.; Koch, K.M.; Harbeck-Weber, C.; Mack, K.J.; Wilder, R.T.; Bauer, B.A.; Brandenburg, J.E. Managing Chronic Pain in Children and Adolescents: A Clinical Review. PM R 2015, 7, S295–S315. [Google Scholar] [CrossRef]
- Banez, G.A. Chronic abdominal pain in children: What to do following the medical evaluation. Curr. Opin. Pediatr. 2008, 20, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Lynch-Jordan, A.M.; Sil, S.; Cunningham, N.; Kashikar-Zuck, S.; Goldschneider, K.R. Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain 2014, 155, 1955–1961. [Google Scholar] [CrossRef] [PubMed]
- Kemani, M.K.; Kanstrup, M.; Jordan, A.; Caes, L.; Gauntlett-Gilbert, J. Evaluation of an intensive interdisciplinary pain treatment based on acceptance and commitment therapy for adolescents with chronic pain and their parents: A nonrandomized clinical trial. J. Pediatr. Psychol. 2018, 43, 981–994. [Google Scholar] [CrossRef] [PubMed]
- Heathcote, L.C.; Pate, J.W.; Park, A.L.; Leake, H.B.; Moseley, G.L.; Kronman, C.A.; Fischer, M.; Timmers, I.; Simons, L.E. Pain neuroscience education on YouTube. PeerJ 2019, 7, e6603. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L.; Butler, D.S. Fifteen Years of Explaining Pain: The Past, Present, and Future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef]
- Pas, R.; Meeus, M.; Malfliet, A.; Baert, I.; Van Oosterwijck, S.; Leysen, L.; Nijs, J.; Ickmans, K. Development and feasibility testing of a Pain Neuroscience Education program for children with chronic pain: Treatment protocol. Braz. J. Phys. Ther. 2018, 22, 248–253. [Google Scholar] [CrossRef]
- Eccleston, C.; Morley, S.; Williams, A.; Yorke, L.; Mastroyannopoulou, K. Systematic review of randomised controlled trials of psychological therapy for chronic pain in children and adolescents, with a subset meta-analysis of pain relief. Pain 2002, 99, 157–165. [Google Scholar] [CrossRef]
- Scharff, L.; Marcus, D.A.; Masek, B.J. A controlled study of minimal-contact thermal biofeedback treatment in children with migraine. J. Pediatr. Psychol. 2002, 27, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, P.J.; Liossi, C.; Ewart, B.; Hatira, P.; Kosmidis, V. Hypnosis in the alleviation of procedure related pain and distress in paediatric oncology patients. Contemp. Hypn. 1998, 15, 199–207. [Google Scholar] [CrossRef]
- Liossi, C.; Hatira, P. Clinical hypnosis in the alleviation of procedure-related pain in pediatric oncology patients. Int. J. Clin. Exp. Hypn. 2003, 51, 4–28. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.T.; Barabasz, A.; Barabasz, M. Comparison of hypnosis and distraction in severely ill children undergoing painful medical procedures. J. Couns. Psychol. 1996, 43, 187. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Lynch-Jordan, A.; Mezoff, A.G.; Farrell, M.K.; Cohen, M.B.; Kashikar-Zuck, S. Importance of addressing anxiety in youth with functional abdominal pain: Suggested guidelines for physicians. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 469. [Google Scholar] [CrossRef]
- Evans, S.; Moieni, M.; Taub, R.; Subramanian, S.K.; Tsao, J.C.; Sternlieb, B.; Zeltzer, L.K. Iyengar yoga for young adults with rheumatoid arthritis: Results from a mixed-methods pilot study. J. Pain Symptom. Manag. 2010, 39, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Jastrowski Mano, K.E.; Salamon, K.S.; Hainsworth, K.R.; Anderson Khan, K.J.; Ladwig, R.J.; Davies, W.H.; Weisman, S.J. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Altern. Ther. Health Med. 2013, 19, 8–14. [Google Scholar]
- Eccleston, C.; Fisher, E.; Law, E.; Bartlett, J.; Palermo, T.M. Psychological interventions for parents of children and adolescents with chronic pain. Cochrane Database Syst. Rev. 2015, 4. [Google Scholar] [CrossRef]
- Kanstrup, M.; Wicksell, R.; Kemani, M.; Wiwe Lipsker, C.; Lekander, M.; Holmström, L. A clinical pilot study of individual and group treatment for adolescents with chronic pain and their parents: Effects of acceptance and commitment therapy on functioning. Children 2016, 3, 30. [Google Scholar] [CrossRef] [PubMed]
- Wicksell, R.K.; Melin, L.; Olsson, G.L. Exposure and acceptance in the rehabilitation of adolescents with idiopathic chronic pain—A pilot study. Eur. J. Pain 2007, 11, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Wicksell, R.K.; Melin, L.; Lekander, M.; Olsson, G.L. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quailty of life in longstanding pediatric pain—A randomized controlled trial. Pain 2009, 141, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Beals-Erickson, S.; Bromberg, M.; Law, E.; Chen, M. A single arm pilot trial of brief cognitive behavioral therapy for insomnia in adolescents with physical and psychiatric comorbidities. J. Clin. Sleep Med. 2017, 13, 401–410. [Google Scholar] [CrossRef]
- Law, E.F.; Fales, J.L.; Beals-Erickson, S.E.; Failo, A.; Logan, D.; Randall, E.; Weiss, K.; Durkin, L.; Palermo, T.M. A Single-Arm Feasibility Trial of Problem-Solving Skills Training for Parents of Children with Idiopathic Chronic Pain Conditions Receiving Intensive Pain Rehabilitation. J. Pediatr. Psychol. 2017, 42, 422–433. [Google Scholar] [CrossRef]
- Palermo, T.M.; Law, E.; Bromberg, M.; Fales, J.L.; Eccleston, C.; Wilson, A.C. Problem solving skills training for parents of children with chronic pain: A pilot randomized controlled trial. Pain 2016, 157, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Pielech, M.; Vowles, K.; Wicksell, R.K. Acceptance and commitment therapy for pediatric chronic pain: Theory and application. Children 2017, 4, 10. [Google Scholar] [CrossRef]
- Zeltzer, L.K.; Zeltzer, P. Pain in Children and Young Adults: The Journey Back to Normal. Two Pediatricians’ Mind-Body Guide for Parents; Shilysca Press: Encino, CA, USA, 2016. [Google Scholar]
- Kempert, H.; Benore, E.; Heines, R. Easily Administered Patient-Reported Outcome Measures: Adolescents’ Perceived Functional Changes After Completing an Intensive Chronic Pain Rehabilitation Program. Arch. Phys. Med. Rehabil. 2017, 98, 58–63. [Google Scholar] [CrossRef]
- Mirek, E.; Logan, D.; Boullard, K.; Hall, A.M.; Staffa, S.J.; Sethna, N. Physical Therapy Outcome Measures for Assessment of Lower Extremity Chronic Pain-Related Function in Pediatrics. Pediatr. Phys. Ther. 2019, 31, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Kempert, H.; Benore, E.; Heines, R. Physical and occupational therapy outcomes: Adolescents’ change in functional abilities using objective measures and self-report. Scand. J. Pain 2017, 14, 60–66. [Google Scholar] [CrossRef]
- Eccleston, Z.; Eccleston, C. Interdisciplinary management of adolescent chronic pain: Developing the role of physiotherapy. Physiotherapy 2004, 90, 77–81. [Google Scholar] [CrossRef]
- Kashikar-Zuck, S.; Black, W.R.; Pfeiffer, M.; Peugh, J.; Williams, S.E.; Ting, T.V.; Thomas, S.; Kitchen, K.; Myer, G.D. Pilot randomized trial of integrated cognitive-behavioral therapy and neuromuscular training for juvenile fibromyalgia: The FIT Teens Program. J. Pain 2018, 19, 1049–1062. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.T.; Thomas, S.; DiCesare, C.; Pfeiffer, M.; Sil, S.; Ting, T.V.; Williams, S.E.; Myer, G.D.; Kashikar-Zuck, S. A pilot study of biomechanical assessment before and after an integrative training program for adolescents with juvenile fibromyalgia. Pediatr. Rheumatol. Online J. 2016, 14, 43. [Google Scholar] [CrossRef]
- Dekker, C.; Goossens, M.E.; Bastiaenen, C.H.; Verbunt, J.A. Study protocol for a multicentre randomized controlled trial on effectiveness of an outpatient multimodal rehabilitation program for adolescents with chronic musculoskeletal pain (2B Active). BMC Musculoskelet. Disord. 2016, 17, 317. [Google Scholar] [CrossRef]
- Coakley, R.M.; Wihak, T.; Kossowsky, J.; Iversen, C.; Donado, C. The Comfort Ability Pain Management Workshop: A Preliminary, Nonrandomized Investigation of a Brief, Cognitive, Biobehavioral, and Parent Training Intervention for Pediatric Chronic Pain. J. Pediatr. Psychol. 2018, 43, 252–265. [Google Scholar] [CrossRef]
- Bonnert, M.; Olén, O.; Lalouni, M.; Hedman-Lagerlöf, E.; Särnholm, J.; Serlachius, E.; Ljótsson, B. Internet-Delivered Exposure-Based Cognitive-Behavioral Therapy for Adolescents With Functional Abdominal Pain or Functional Dyspepsia: A Feasibility Study. Behav. Ther. 2019, 50, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; de la Vega, R.; Dudeney, J.; Murray, C.; Law, E. Mobile health intervention for self-management of adolescent chronic pain (WebMAP mobile): Protocol for a hybrid effectiveness-implementation cluster randomized controlled trial. Contemp. Clin. Trials 2018, 74, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.N.; Lalloo, C.; Harris, L.; Isaac, L.; Campbell, F.; Brown, S.; Ruskin, D.; Gordon, A.; Galonski, M.; Pink, L.R. iCanCope with Pain™: User-centred design of a web-and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Res. Manag. 2014, 19, 257–265. [Google Scholar] [CrossRef]
- Won, A.S.; Tataru, C.A.; Cojocaru, C.M.; Krane, E.J.; Bailenson, J.N.; Niswonger, S.; Golianu, B. Two virtual reality pilot studies for the treatment of pediatric CRPS. Pain Med. 2015, 16, 1644–1647. [Google Scholar] [CrossRef] [PubMed]
- Won, A.S.; Bailey, J.; Bailenson, J.; Tataru, C.; Yoon, I.A.; Golianu, B. Immersive Virtual Reality for Pediatric Pain. Children (Basel) 2017, 4, 52. [Google Scholar] [CrossRef]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Malfliet, A.; Kregel, J.; Coppieters, I.; De Pauw, R.; Meeus, M.; Roussel, N.; Cagnie, B.; Danneels, L.; Nijs, J. Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: A randomized clinical trial. JAMA Neurol. 2018, 75, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L. Joining forces-combining cognition-targeted motor control training with group or individual pain physiology education: A successful treatment for chronic low back pain. J. Man. Manip. Ther. 2003, 11, 88–94. [Google Scholar] [CrossRef]
- Moseley, G.L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust. J. Physiother. 2002, 48, 297–302. [Google Scholar] [CrossRef]
- Malfliet, A.; Kregel, J.; Meeus, M.; Roussel, N.; Danneels, L.; Cagnie, B.; Dolphens, M.; Nijs, J. Blended-learning pain neuroscience education for people with chronic spinal pain: Randomized controlled multicenter trial. Phys. Ther. 2017, 98, 357–368. [Google Scholar] [CrossRef]
- Nijs, J.; Van Wilgen, C.P.; Van Oosterwijck, J.; van Ittersum, M.; Meeus, M. How to explain central sensitization to patients with ‘unexplained’chronic musculoskeletal pain: Practice guidelines. Man. Ther. 2011, 16, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Malfliet, A.; Ickmans, K.; Baert, I.; Meeus, M. Treatment of central sensitization in patients with ‘unexplained’chronic pain: An update. Expert Opin. Pharmacother. 2014, 15, 1671–1683. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Puentedura, E.J.; Diener, I.; Peoples, R.R. Preoperative therapeutic neuroscience education for lumbar radiculopathy: A single-case fMRI report. Physiother. Theory Pract. 2015, 31, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Zimney, K.; Louw, A.; Puentedura, E.J. Use of Therapeutic Neuroscience Education to address psychosocial factors associated with acute low back pain: A case report. Physiother. Theory Pract. 2014, 30, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Pate, J.W.; Hush, J.M.; Hancock, M.J.; Moseley, G.L.; Butler, D.S.; Simons, L.E.; Pacey, V. A child’s concept of pain: An international survey of pediatric pain experts. Children 2018, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L. A pain neuromatrix approach to patients with chronic pain. Man. Ther. 2003, 8, 130–140. [Google Scholar] [CrossRef]
- Gold, J.I.; Yetwin, A.K.; Mahrer, N.E.; Carson, M.C.; Griffin, A.T.; Palmer, S.N.; Joseph, M.H. Pediatric chronic pain and health-related quality of life. J. Pediatr. Nurs. 2009, 24, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Robins, H.; Perron, V.; Heathcote, L.C.; Simons, L.E. Pain neuroscience education: State of the art and application in pediatrics. Children (Basel) 2016, 4, 43. [Google Scholar] [CrossRef]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019. [Google Scholar] [CrossRef] [PubMed]
- Andias, R.; Neto, M.; Silva, A.G. The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: A school-based pilot, randomized and controlled study. Physiother. Theory Pract. 2018, 34, 682–691. [Google Scholar] [CrossRef]
- Kashikar-Zuck, S.; Vaught, M.H.; Goldschneider, K.R.; Graham, T.B.; Miller, J.C. Depression, coping, and functional disability in juvenile primary fibromyalgia syndrome. J. Pain 2002, 3, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.L.; Von Baeyer, C.L.; McGrath, P.J. Online psychological treatment for pediatric recurrent pain: A randomized evaluation. J. Pediatr. Psychol. 2006, 31, 724–736. [Google Scholar] [CrossRef] [PubMed]
- Anbar, R.D. Hypnosis in pediatrics: Applications at a pediatric pulmonary center. BMC Pediatr. 2002, 2, 11. [Google Scholar] [CrossRef]
- Delivet, H.; Dugue, S.; Ferrari, A.; Postone, S.; Dahmani, S. Efficacy of Self-hypnosis on Quality of Life For Children with Chronic Pain Syndrome. Int. J. Clin. Exp. Hypn. 2018, 66, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Shigaki, C.L.; Glass, B.; Schopp, L.H. Mindfulness-based stress reduction in medical settings. J. Clin. Psychol. Med. Settings 2006, 13, 209–216. [Google Scholar] [CrossRef]
- Zernicke, K.A.; Campbell, T.S.; Blustein, P.K.; Fung, T.S.; Johnson, J.A.; Bacon, S.L.; Carlson, L.E. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: A randomized wait-list controlled trial. Int. J. Behav. Med. 2013, 20, 385–396. [Google Scholar] [CrossRef]
- Field, T.; Hernandez-Reif, M.; Seligmen, S.; Krasnegor, J.; Sunshine, W.; Rivas-Chacon, R.; Schanberg, S.; Kuhn, C. Juvenile rheumatoid arthritis: Benefits from massage theraphy. J. Pediatr. Psychol. 1997, 22, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Suresh, S.; Wang, S.; Porfyris, S.; Kamasinski-sol, R.; Steinhorn, D.M. Massage therapy in outpatient pediatric chronic pain patients: Do they facilitate significant reductions in levels of distress, pain, tension, discomfort, and mood alterations? Paediatr. Anaesth. 2008, 18, 884–887. [Google Scholar] [CrossRef]
- Beck, J.S. Cognitive Behavior Therapy: Basics and Beyond; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Coyne, L.W.; McHugh, L.; Martinez, E.R. Acceptance and commitment therapy (ACT): Advances and applications with children, adolescents, and families. Child Adolesc. Psychiatr. Clin. N. Am. 2011, 20, 379–399. [Google Scholar] [CrossRef]
- Gauntlett-Gilbert, J.; Connell, H.; Clinch, J.; McCracken, L.M. Acceptance and values-based treatment of adolescents with chronic pain: Outcomes and their relationship to acceptance. J. Pediatr. Psychol. 2013, 38, 72–81. [Google Scholar] [CrossRef]
- Wicksell, R.K.; Olsson, G.L.; Hayes, S.C. Mediators of change in acceptance and commitment therapy for pediatric chronic pain. Pain 2011, 152, 2792–2801. [Google Scholar] [CrossRef] [PubMed]
- Masuda, A.; Feinstein, A.; Wendell, J.W.; Sheehan, S.T. Cognitive defusion versus thought distraction: A clinical rationale, training, and experiential exercise in altering psychological impacts of negative self-referential thoughts. Behav. Modif. 2010, 34, 520–538. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, W.E.; Folwer, R.S.; Lehmann, J.F.; D’elateur, B.J. Some implications of learning in problems of chronic pain. J. Chronic Dis. 1968, 21, 179–190. [Google Scholar] [CrossRef]
- Walker, L.S. The evolution of research on recurrent abdominal pain: History, assumptions, and a conceptual model. Prog. Pain Res. Manag. 1999, 13, 141–172. [Google Scholar]
- Simons, L.E.; Kaczynski, K.J. The Fear Avoidance model of chronic pain: Examination for pediatric application. J. Pain 2012, 13, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.; Linton, S.J. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain 2012, 153, 1144–1147. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Sieberg, C.B.; Carpino, E.; Logan, D.; Berde, C. The Fear of Pain Questionnaire (FOPQ): Assessment of pain-related fear among children and adolescents with chronic pain. J. Pain 2011, 12, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Goubert, L.; Simons, L.E. Cognitive styles and processes in paediatric pain. In Oxford Textbook of Pediatric Pain; Oxford University Press: Oxford, UK, 2013; pp. 95–101. [Google Scholar]
- Vlaeyen, J.W.S.; Morley, S.J.; Linton, S.J.; Boersma, K.; de Jong, J. Pain-Related Fear: Exposure-Based Treatment of Chronic Pain; IASP Press: Washington, DC, USA, 2012. [Google Scholar]
- Vlaeyen, J.W.; de Jong, J.; Geilen, M.; Heuts, P.H.T.G.; van Breukelen, G. Graded exposure in vivo in the treatment of pain-related fear: A replicated single-case experimental design in four patients with chronic low back pain. Behav. Res. Ther. 2001, 39, 151–166. [Google Scholar] [CrossRef]
- Simons, L.E.; Vlaeyen, J.W.S.; Declercq, L.; Smith, A.L.; Beebe, J.; Hogan, M.; Li, E.; Kronman, C.; Mahmud, F.; Corey, J.; et al. Avoid or engage? Outcomes of graded exposure in youth with chronic pain utilizing multi-level modeling of a single-case randomized design. Pain 2019. submitted. [Google Scholar]
- Hechler, T.; Dobe, M.; Damschen, U.; Blankenburg, M.; Schroeder, S.; Kosfelder, J.; Zernikow, B. The pain provocation technique for adolescents with chronic pain: Preliminary evidence for its effectiveness. Pain Med. 2010, 11, 897–910. [Google Scholar] [CrossRef]
- Gruszka, P.; Schaan, L.; Adolph, D.; Pane-Farre, C.A.; Benke, C.; Schneider, S.; Hechler, T. Defence reponse mobilization in response to provocation or imagery of interoceptive sensations in adolescents with chronic pain: A study protocol. Pain Rep. 2018, 3. [Google Scholar] [CrossRef]
- Palermo, T.M.; Eccleston, C. Parents of children and adolescents with chronic pain. Pain 2009, 146, 15. [Google Scholar] [CrossRef]
- Law, E.F.; Fisher, E.; Eccleston, C.; Palermo, T.M. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Simons, L.E.; Smith, A.; Kaczynski, K.; Basch, M. Living in fear of your child’s pain: The Parent Fear of Pain Questionnaire. Pain 2015, 156, 694–702. [Google Scholar] [CrossRef]
- Coakley, R.M. When Your Child Hurts: Effective Stratgies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain; Yale University Press: New Haven, CT, USA, 2016. [Google Scholar]
- Zeltzer, L.K.; Blackett Schlank, C. Conquering Your Child’s Chronic Pain; HarperCollins: New York, NY, USA, 2005. [Google Scholar]
- Palermo, T.M.; Law, E. Managing Your Child’s Chronic Pain; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Sherry, D.D.; Wallace, C.A.; Kelley, C.; Kidder, M.; Sapp, L. Short-and long-term outcomes of children with complex regional pain syndrome type I treated with exercise therapy. Clin. J. Pain 1999, 15, 218–223. [Google Scholar] [CrossRef]
- Eccleston, C.; Connell, H.; Carmichael, N. Residential Treatment Settings for Adolescent Chronic Pain Management; Humana Press: Totowa, NJ, USA, 2006. [Google Scholar]
- Hechler, T.; Ruhe, A.-K.; Schmidt, P.; Hirsch, J.; Wager, J.; Dobe, M.; Krummenauer, F.; Zernikow, B. Inpatient-based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: Randomized controlled trial of efficacy and economic effects. Pain 2014, 155, 118–128. [Google Scholar] [CrossRef]
- Flor, H.; Fydrich, T.; Turk, D.C. Efficacy of multidisciplinary pain treatment centers: A meta-analytic review. Pain 1992, 49, 221–230. [Google Scholar] [CrossRef]
- Logan, D.E.; Carpino, E.A.; Chiang, G.; Condon, M.; Firn, E.; Gaughan, V.J. A day-hospital approach to treatment of pediatric complex regional pain syndrome: Initial functional outcomes. Clin. J. Pain 2012, 28. [Google Scholar] [CrossRef]
- Lee, B.H.; Scharff, L.; Sethna, N.; McCarthy, C.F.; Scott-Sutherland, J.; Shea, A.M.; Sullivan, P.; Meier, P.; Zurakowski, D.; Masek, B.J.; et al. Physical therapy and cognitive-behavioral treatment for complex regional pain syndromes. J. Pediatr. 2002, 141, 135–140. [Google Scholar] [CrossRef]
- Valrie, C.R.; Bromberg, M.H.; Palermo, T.; Schanberg, L.E. A systematic review of sleep in pediatric pain populations. J. Dev. Behav. Pediatr. 2013, 34, 120–128. [Google Scholar] [CrossRef]
- Palermo, T.M.; Kiska, R. Subjective sleep disturbances in adolescents with chronic pain: Relationship to daily functioning and quality of life. J. Pain 2005, 6, 201–207. [Google Scholar] [CrossRef]
- McGrath, P.J.; Frager, G. Psychological barriers to optimal pain management in infants and children. Clin. J. Pain 1996, 12, 135–141. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Jagpal, A.; Tran, S.T.; Kashikar-Zuck, S.; Goldschneider, K.R.; Coghill, R.C.; Lynch-Jordan, A.M. Anxiety adversely impacts response to cognitive behavioral therapy in children with chronic pain. J. Pediatr. 2016, 171, 227–233. [Google Scholar] [CrossRef]
- Van Tilburg, M.A.; Spence, N.J.; Whitehead, W.E.; Bangdiwala, S.; Goldston, D.B. Chronic pain in adolescents is associated with suicidal thoughts and behaviors. J. Pain 2011, 12, 1032–1039. [Google Scholar] [CrossRef]
- Evans, J.R.; Benore, E.; Banez, G.A. Conversion disorder and pediatric chronic pain—Talking through the challenges. Pediatr. Pain Lett. 2015, 17, 16–20. [Google Scholar]
- Eccleston, C.; Malleson, P.N.; Clinch, J.; Connell, H.; Sourbut, C. Chronic pain in adolescents: Evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch. Dis. Child 2003, 88, 881–885. [Google Scholar] [CrossRef]
- Simons, L.E.; Sieberg, C.B.; Pielech, M.; Conroy, C.; Logan, D.E. What does it take? Comparing intensive rehabilitation to outpatient treatment for children with significant pain-related disability. J. Pediatr. Psychol. 2012, 38, 213–223. [Google Scholar] [CrossRef]
- Maynard, C.S.; Amari, A.; Wieczorek, B.; Christensen, J.R.; Slifer, K.J. Interdisciplinary behavioral rehabilitation of pediatric pain-associated disability: Retrospective review of an inpatient treatment protocol. J. Pediatr. Psychol. 2009, 35, 128–137. [Google Scholar] [CrossRef]
- Hechler, T.; Blankenburg, M.; Dobe, M.; Kosfelder, J.; Hübner, B.; Zernikow, B. Effectiveness of a multimodal inpatient treatment for pediatric chronic pain: A comparison between children and adolescents. Eur. J. Pain 2010, 14, 91–97. [Google Scholar] [CrossRef]
- Mahrer, N.E.; Gold, J.I.; Luu, M.; Herman, P.M. A cost-analysis of an interdisciplinary pediatric chronic pain clinic. J. Pain 2018, 19, 158–165. [Google Scholar] [CrossRef]
- Palermo, T.M.; Wilson, A.C.; Peters, M.; Lewandowski, A.S.; Somhegyi, H. Randomized controlled trial of an Internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain 2009, 146, 205–213. [Google Scholar] [CrossRef]
- Lin, J.; Klatt, L.-I.; McCracken, L.M.; Baumeister, H. Psychological flexibility mediates the effect of an online-based acceptance and commitment therapy for chronic pain: An investigation of change processes. Pain 2018, 159, 663–672. [Google Scholar] [CrossRef]
- Fisher, E.; Law, E.F.; Palermo, T.M.; Eccleston, C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2014, 2014, CD011118. [Google Scholar]
- Riva, G.; Baños, R.M.; Botella, C.; Mantovani, F.; Gaggioli, A. Transforming experience: The potential of augmented reality and virtual reality for enhancing personal and clinical change. Front. Psychiatry 2016, 7, 164. [Google Scholar] [CrossRef]
- Matamala-Gomez, M.; Diaz Gonzalez, A.M.; Slater, M.; Sanchez-Vives, M.V. Decreasing Pain Ratings in Chronic Arm Pain Through Changing a Virtual Body: Different Strategies for Different Pain Types. J. Pain 2019. [Google Scholar] [CrossRef]
- Simons, L.E.; Smith, A.; Ibagon, C.; Coakley, R.M.; Logan, D.E.; Schecter, N.; Borsook, D.; Hill, J.C. Pediatric Pain Screen Tool (PPST): Rapid identification of risk in youth with pain complaints. Pain 2015, 156, 1511–1518. [Google Scholar] [CrossRef]
| Evidence Supporting Interventions | Examples of Resources | |
|---|---|---|
| Individual Outpatient Interventions | ||
| Pain Science Education | Heathcote et al., 2019 ** [25]; Moseley & Butler [26], 2015; Pas et al., 2018 [27] * | Tame the Beast What is Pain? The Mysterious Science of Pain PNE4Kids A Journey to Learn About Pain |
| Physiological Self-Regulation Training | Eccleston et al., 2002 [28] ** | |
| Biofeedback | Benore and Banez, 2013 [29]; McKenna et al., 2015 [30] * | Breathe2Relax BellyBio |
| Progressive Muscle Relaxation | Palermo, 2012 [10] | Progressive Muscle Relaxation Script |
| Self-Hypnosis | Liossi et al., 2003 [31]; Tome-Pires & Miro, 2012 [32]; | |
| Guided Imagery | Van Tilburg et al., 2009 [33] * | |
| Mindfulness-based Stress Reduction (MBSR) and Yoga | Evans et al., 2010 [34]; Jastrowski Mano et al., 2013 [35] * | |
| Cognitive Skills Training | Eccleston et al., 2015 [36] **; Fisher et al., 2014 [14] **; Palermo et al., 2010 [15] ** | |
| Behavioral Exposure | Kanstrup et al., 2017 [37]; Kemani et al., 2018 [24]; Wicksell et al., 2007 [38] *; Wicksell et al., 2009 [39] | |
| Cognitive Behavioral Therapy for Insomnia (CBT-I) | Palermo et al., 2017 [40] * | iSleep App CBT-I App |
| Parent Coaching | Eccleston et al., 2014 [36] **; Palermo, 2012 [10] | Conquering Your Child’s Chronic Pain Managing Your Child’s Chronic Pain When Your Child Hurts Pain in Children and Young Adults: The Journey Back to Normal |
| Problem-Solving Skills Training | Law et al., 2017 [41]; Palermo et al., 2016 [42] * | |
| Multi-component Treatment Packages | ||
| Cognitive-Behavioral Therapy | Eccleston et al., 2014 [36] **; Fisher et al., 2014 [14] **; Palermo et al., 2010 [15] ** | Cognitive-Behavioral Therapy for Chronic Pain in Children and Adolescents |
| Acceptance and Commitment Therapy | Pielech et al., 2017 [43]; Wicksell et al., 2009 [39] | Acceptance and Mindfulness Treatments for Children and Adolescents |
| Physical Therapy | ||
| Strength and Endurance Training | Eccleston and Eccleston, 2004 [44]; Kempert et al., 2017b [45]; Mirek et al., 2019 [46] | |
| Gait and Posture Training | ||
| Occupational Therapy | ||
| Independence with Activities of Daily Living | Kempert et al., 2017a [47]; Kempert et al., 2017b [45] | |
| Desensitization | Sherry et al., 1999 [48] | |
| Interdisciplinary Outpatient Pain Treatment | ||
| FIT Teens | Kashikar-Zuck et al., 2018 [49] *; Tran et al., 2016 [50] * | |
| 2B Active | Dekker et al., 2016 [51] | |
| GET Living | GET Living, NCT: 03699007 | |
| Intensive Interdisciplinary Pain Treatment (IIPT) | Hechler et al., 2015 [19] ** | |
| Emerging Pain Treatment Intervention Formats | ||
| One-day workshops | Coakley et al., 2018 [52] | The Comfort Ability |
| Internet and mobile applications | Bonnert et al., 2019 [53]; Palermo et al., 2018 [54]; Stinson et al., 2014 [55] | |
| Virtual Reality | Won et al., 2015 [56] *; Won et al., 2017 [57] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harrison, L.E.; Pate, J.W.; Richardson, P.A.; Ickmans, K.; Wicksell, R.K.; Simons, L.E. Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. J. Clin. Med. 2019, 8, 1267. https://doi.org/10.3390/jcm8091267
Harrison LE, Pate JW, Richardson PA, Ickmans K, Wicksell RK, Simons LE. Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. Journal of Clinical Medicine. 2019; 8(9):1267. https://doi.org/10.3390/jcm8091267
Chicago/Turabian StyleHarrison, Lauren E., Joshua W. Pate, Patricia A. Richardson, Kelly Ickmans, Rikard K. Wicksell, and Laura E. Simons. 2019. "Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain" Journal of Clinical Medicine 8, no. 9: 1267. https://doi.org/10.3390/jcm8091267
APA StyleHarrison, L. E., Pate, J. W., Richardson, P. A., Ickmans, K., Wicksell, R. K., & Simons, L. E. (2019). Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. Journal of Clinical Medicine, 8(9), 1267. https://doi.org/10.3390/jcm8091267







