Identification of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) Cutoff Scores for Impaired Sexual Function in Women with Pelvic Floor Disorders
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Applied Questionnaires
2.2. Statistical Analysis
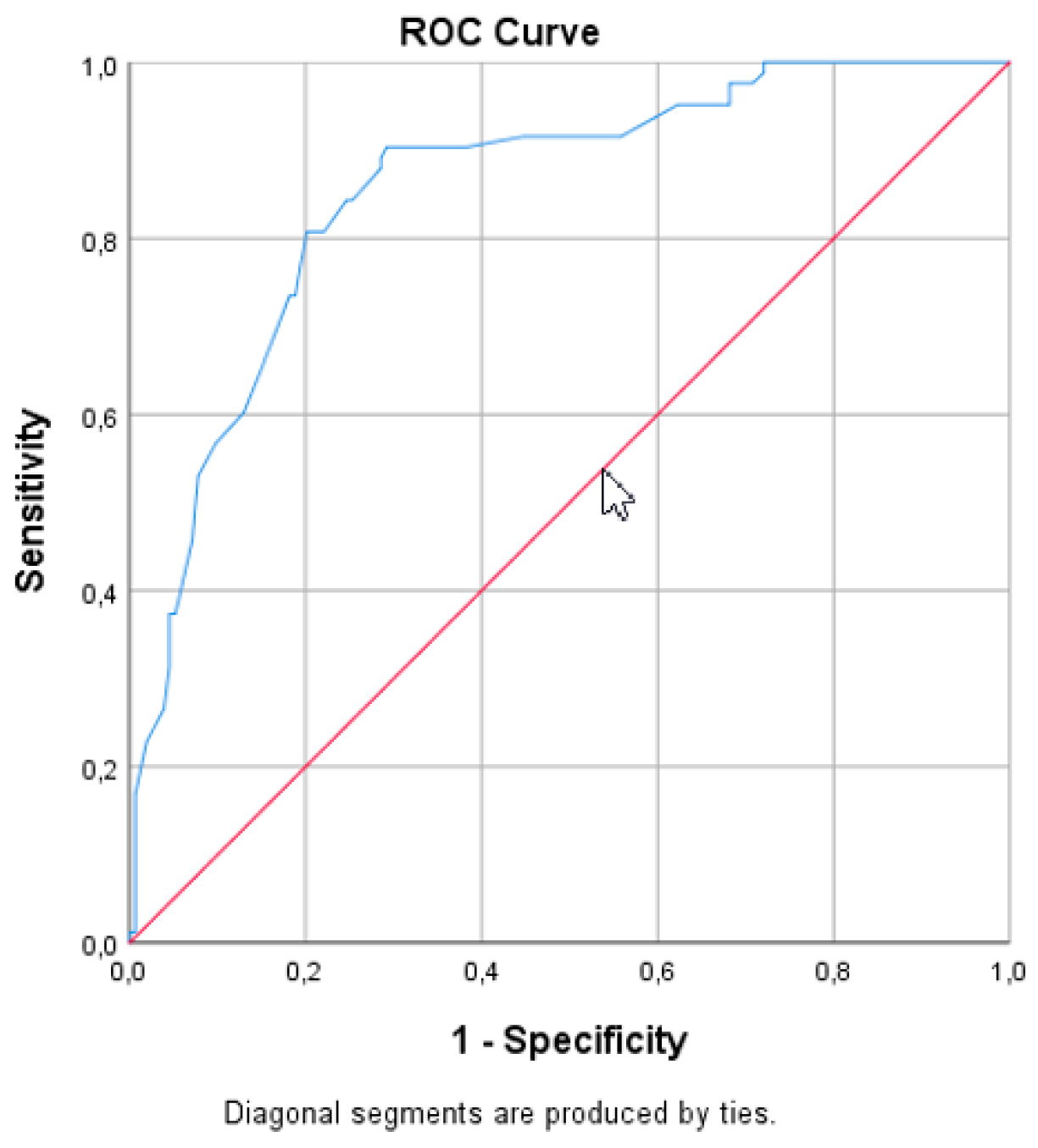
3. Results
4. Discussion
5. Concluding Message
Author Contributions
Funding
Conflicts of Interest
References
- Wu, J.M.; Vaughan, C.P.; Goode, P.S.; Redden, D.T.; Burgio, K.L.; Richter, H.E.; Markland, A.D. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet. Gynecol. 2014, 123, 141–148. [Google Scholar] [CrossRef] [Green Version]
- Salonia, A.; Zanni, G.; Nappi, R.E.; Briganti, A.; Dehò, F.; Fabbri, F.; Colombo, R.; Guazzoni, G.; Di Girolamo, V.; Rigatti, P.; et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: Results of a cross-sectional study. Eur. Urol. 2004, 45, 642–648. [Google Scholar] [CrossRef]
- Li-Yun-Fong, R.J.; Larouche, M.; Hyakutake, M.; Koenig, N.; Lovatt, C.; Geoffrion, R.; Brotto, L.A.; Lee, T.; Cundiff, G.W. Is Pelvic Floor Dysfunction an Independent Threat to Sexual Function? A Cross-Sectional Study in Women with Pelvic Floor Dysfunction. J. Sex. Med. 2017, 14, 226–237. [Google Scholar] [CrossRef]
- Handa, V.L.; Cundiff, G.; Chang, H.H.; Helzlsouer, K.J. Female sexual function and pelvic floor disorders. Obstet. Gynecol. 2008, 111, 1045–1052. [Google Scholar] [CrossRef] [Green Version]
- Bradley, S.L.; Weidner, A.C.; Siddiqui, N.Y.; Gandhi, M.P.; Wu, J.M. Shifts in national rates of inpatient prolapse surgery emphasize current coding inadequacies. Female Pelvic Med. Reconstr. Surg. 2011, 17, 204–208. [Google Scholar] [CrossRef] [Green Version]
- Løwenstein, E.; Ottesen, B.; Gimbel, H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int. Urogynecol. J. 2015, 26, 49–55. [Google Scholar] [CrossRef]
- Wilkins, M.F.; Wu, J.M. Lifetime risk of surgery for stress urinary incontinence or pelvic organ prolapse. Minerva Ginecol. 2017, 69, 171–177. [Google Scholar]
- Kammerer-Doak, D. Assessment of sexual function in women with pelvic floor dysfunction. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2009, 20 (Suppl. 1), S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Wiegel, M.; Meston, C.; Rosen, R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. J. Sex. Marital Ther. 2005, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Miotla, P.; Cartwright, R.; Skorupska, K.; Bogusiewicz, M.; Markut-Miotla, E.; Futyma, K.; Rechberger, T. Impact of intravesical onabotulinumtoxinA on sexual function in women with OAB. Neurourol. Urodyn. 2017, 36, 1564–1569. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.G.; Rockwood, T.H.; Constantine, M.L.; Thakar, R.; Kammerer-Doak, D.N.; Pauls, R.N.; Parekh, M.; Ridgeway, B.; Jha, S.; Pitkin, J.; et al. A new measure of sexual function in women with pelvic floor disorders (PFD): The Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). Int. Urogynecol. J. 2013, 24, 1091–1103. [Google Scholar] [CrossRef] [PubMed]
- Grzybowska, M.E.; Wydra, D.G. Is voluntary pelvic floor muscles contraction important for sexual function in women with pelvic floor disorders? Neurourol. Urodyn. 2019, 38, 2001–2009. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.G.; Pauls, R.N.; Thakar, R.; Morin, M.; Kuhn, A.; Petri, E.; Fatton, B.; Whitmore, K.; Kingsberg, S.A.; Lee, J. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for the assessment of sexual health of women with pelvic floor dysfunction. Int. Urogynecol. J. 2018, 29, 647–666. [Google Scholar] [CrossRef] [PubMed]
- Haylen, B.T.; Maher, C.F.; Barber, M.D.; Camargo, S.; Dandolu, V.; Digesu, A.; Goldman, H.B.; Huser, M.; Milani, A.L.; Moran, P.A.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourol. Urodyn. 2016, 35, 137–168. [Google Scholar] [CrossRef] [PubMed]
- Nowosielski, K.; Wróbel, B.; Sioma-Markowska, U.; Poręba, R. Development and validation of the Polish version of the Female Sexual Function Index in the Polish population of females. J. Sex. Med. 2013, 10, 386–395. [Google Scholar] [CrossRef]
- Neijenhuijs, K.I.; Hooghiemstra, N.; Holtmaat, K.; Aaronson, N.K.; Groenvold, M.; Holzner, B.; Terwee, C.B.; Cuijpers, P.; Verdonck-de Leeuw, I.M. The Female Sexual Function Index (FSFI)-A Systematic Review of Measurement Properties. J. Sex. Med. 2019, 16, 640–660. [Google Scholar] [CrossRef]
- Rockwood, T.H.; Constantine, M.L.; Adegoke, O.; Rogers, R.G.; McDermott, E.; Davila, G.W.; Domoney, C.; Jha, S.; Kammerer-Doak, D.; Lukacz, E.S.; et al. The PISQ-IR: Considerations in scale scoring and development. Int. Urogynecol. J. 2013, 24, 1105–1122. [Google Scholar] [CrossRef]
- Grzybowska, M.E.; Piaskowska-Cala, J.; Wydra, D.G. Polish translation and validation of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). Int. Urogynecol. J. 2019, 30, 55–64. [Google Scholar] [CrossRef] [Green Version]
- International Urogynecological Association (IUGA). Available online: https://www.iuga.org/publications/pisq-ir-papers (accessed on 15 December 2019).
- Constantine, M.L.; Pauls, R.N.; Rogers, R.R.; Rockwood, T.H. Validation of a single summary score for the Prolapse/Incontinence Sexual Questionnaire-IUGA revised (PISQ-IR). Int. Urogynecol. J. 2017, 28, 1901–1907. [Google Scholar] [CrossRef]
- Kelleher, C.J.; Cardozo, L.D.; Khullar, V.; Salvatore, S. A new questionnaire to assess the quality of life of urinary incontinent women. Br. J. Obstet. Gynaecol. 1997, 104, 1374–1379. [Google Scholar] [CrossRef]
- Diaz, D.C.; Robinson, D.; Bosch, R.; Costantiini, E.; Ctterill, N.; Espuña-Pons, M.; Kocjancic, E.; Lemos, N.; Tarcan, T.; Yoshida, M. Patient-reported outcome assessment. In Incontinence, 6th ed.; Abrams, P., Cardozo, L., Wagg, A., Wein, A., Eds.; ICUD ICS: Tokyo, Japan, 2017; Volume 1, pp. 541–670. [Google Scholar]
- Mamik, M.M.; Rogers, R.G.; Qualls, C.R.; Morrow, J.D. The minimum important difference for the Pelvic Organ Prolapse-Urinary Incontinence Sexual Function Questionnaire. Int. Urogynecol. J. 2014, 25, 1321–1326. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, L.; Gamble, T.; Sanses, T.V.; van Raalte, H.; Carberry, C.; Jakus, S.; Kambiss, S.; McAchran, S.; Pham, T.; Aschkenazi, S.; et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J. Sex. Med. 2009, 6, 2286–2291. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, A.; Weir, N.; Tangyotkajohn, U.; Jacques, A.; Thompson, J.; Briffa, K. Help-seeking behaviour for pelvic floor dysfunction in women over 55: Drivers and barriers. Int. Urogynecol. J. 2018, 29, 1645–1653. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Domain | Questions | Minimum Score | Maximum Score |
|---|---|---|---|
| Desire | 1, 2 | 1.2 | 6.0 |
| Arousal | 3, 4, 5, 6 | 0 | 6.0 |
| Lubrication | 7, 8, 9, 10 | 0 | 6.0 |
| Orgasm | 11, 12, 13 | 0 | 6.0 |
| Satisfaction | 14, 15, 16 | 0.8 | 6.0 |
| Pain | 17, 18, 19 | 0 | 6.0 |
| Sexually Active (SA) Domains | SA–21 Items | Questions | Minimum Score | Maximum Score |
|---|---|---|---|---|
| Arousal Orgasm | SA-AO, 4 items | Q 7, 8a, 10, 11 | 1 | 5 |
| Condition-specific | SA-CS, 3 items | Q 8b, 8c, 9 | 1 | 5 |
| Partner-related | SA-PR, 3 items | Q 13, 14a,14b | 1/− * | 4/− * |
| Desire | SA-D, 3 items | Q 15, 16, 17 | 1 | 5 |
| Condition Impact | SA-CI, 4 items | Q 18, 20b, 20c, 20d | 1 | 4 |
| Global Quality | SA-GQ, 4 items | Q 19a, 19b, 19c, 20a | 1 | 4.8 |
| Summary Score | 1.545 | 3.909 | ||
| 1.722 ** | 3.888 ** | |||
| Variable | FSFI < 26.55 (n = 143) | FSFI > 26.55 (n = 83) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 56.8 ± 10.8 | 56.3 ± 10.6 | 0.72 a |
| BMI (kg/m2), mean ± SD | 27.8 ± 4.6 | 26.7 ± 4.0 | 0.06 a |
| Postmenopausal n (%) | 107 (74.8) | 50 (60.2) | 0.02 b |
| Education n (%) | 0.09 b | ||
| Primary | 9 (6.3) | 1 (1.2) | |
| Secondary | 79 (55.2) | 41 (49.4) | |
| Higher | 55 (38.5) | 41 (49.4) | |
| Parity, mean ± SD (median) | 2.4 ± 1.0 (2) | 2.1 ± 0.8 (2) | 0.02 a |
| Vaginal delivery | 131 (91.6) | 69 (83.1) | 0.09 b |
| Cesarean delivery | 2 (1.4) | 4 (4.8) | |
| Both | 10 (7.0) | 8 (9.6) | |
| None | − | 2 (2.4) | |
| Marital status n (%) | 0.54 b | ||
| married | 131 (91.6) | 74 (89.2) | |
| partnership | 12 (8.4) | 9 (10.8) | |
| Previous surgical history | |||
| None | 93 (65.0) | 58 (69.9) | 0.47 b |
| Hysterectomy | 29 (20.3) | 9 (10.8) | 0.08 b |
| Prior prolapse surgery | 35 (24.5) | 17 (20.5) | 0.49 b |
| Prior anti-UI surgery | 7 (4.9) | 5 (6.0) | 0.71 b |
| Clinical diagnosis n (%) | |||
| Only UI | 34 (23.8) | 19 (22.9) | 0.62 b |
| Only POP | 56 (39.2) | 32 (38.5) | |
| UI and POP | 53 (37.1) | 31 (37.3) | |
| FI | 18 (12.6) | 5 (6.0) | 0.11 b |
| POP-Q n (%) | 0.08 b | ||
| 0 | 2 (1.4) | 6 (7.2) | |
| I | 7 (4.9) | 7 (8.4) | |
| II | 52 (36.4) | 21 (25.3) | |
| III | 68 (47.6) | 42 (50.6) | |
| IV | 14 (9.8) | 7 (8.4) |
| Variable | FSFI < 26.55 (n = 143) | FSFI > 26.55 (n = 83) | p-Value |
|---|---|---|---|
| PISQ-IR SA Mean ± SD | |||
| Arousal Orgasm | 2.77 ± 0.65 | 3.71 ± 0.54 | 0.000 a |
| Condition-specific | 4.11 ± 0.97 | 4.38 ± 0.70 | 0.017 a |
| Partner-related | 3.21 ± 0.50 | 3.50 ± 0.41 | 0.000 a |
| Desire | 2.70 ± 0.68 | 3.29 ± 0.56 | 0.000 a |
| Condition Impact | 2.45 ± 0.78 | 2.99 ± 0.77 | 0.000 a |
| Global Quality | 2.78 ± 0.90 | 3.64 ± 1.01 | 0.000 a |
| PISQ-IR Summary Score | 2.55 ± 0.38 | 3.06 ± 0.31 | 0.000a |
| FSFI Mean ± SD | |||
| Desire | 2.76 ± 0.91 | 3.84 ± 0.87 | 0.000 a |
| Arousal | 3.09 ± 0.96 | 4.74 ± 0.72 | 0.000 a |
| Lubrication | 3.56 ± 1.10 | 5.13 ± 0.80 | 0.000 a |
| Orgasm | 3.33 ± 1.23 | 5.13 ± 0.70 | 0.000 a |
| Satisfaction | 3.98 ± 1.06 | 5.30 ± 0.79 | 0.000 a |
| Pain | 3.94 ± 1.34 | 5.44 ± 0.69 | 0.000 a |
| Total Score | 20.65 ± 4.34 | 29.58 ± 2.01 | 0.000 a |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzybowska, M.E.; Futyma, K.; Wydra, D. Identification of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) Cutoff Scores for Impaired Sexual Function in Women with Pelvic Floor Disorders. J. Clin. Med. 2020, 9, 13. https://doi.org/10.3390/jcm9010013
Grzybowska ME, Futyma K, Wydra D. Identification of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) Cutoff Scores for Impaired Sexual Function in Women with Pelvic Floor Disorders. Journal of Clinical Medicine. 2020; 9(1):13. https://doi.org/10.3390/jcm9010013
Chicago/Turabian StyleGrzybowska, Magdalena Emilia, Konrad Futyma, and Dariusz Wydra. 2020. "Identification of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) Cutoff Scores for Impaired Sexual Function in Women with Pelvic Floor Disorders" Journal of Clinical Medicine 9, no. 1: 13. https://doi.org/10.3390/jcm9010013
APA StyleGrzybowska, M. E., Futyma, K., & Wydra, D. (2020). Identification of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) Cutoff Scores for Impaired Sexual Function in Women with Pelvic Floor Disorders. Journal of Clinical Medicine, 9(1), 13. https://doi.org/10.3390/jcm9010013





