Correlation of Micro-Computed Tomography Assessment of Valvular Mineralisation with Histopathological and Immunohistochemical Features of Calcific Aortic Valve Disease
Abstract
:1. Introduction
2. Experimental Section
2.1. Patients and Tissue Specimens
2.2. Micro-Computed Tomography
2.3. Histological Analysis
2.4. Immunohistochemistry
2.5. Statistical Analysis
3. Results
3.1. Population
3.2. Distribution of the μCT Measurements
3.3. The Extent of Calcification as Measured by μCT is Different According to Clinical Characteristics of the Patients
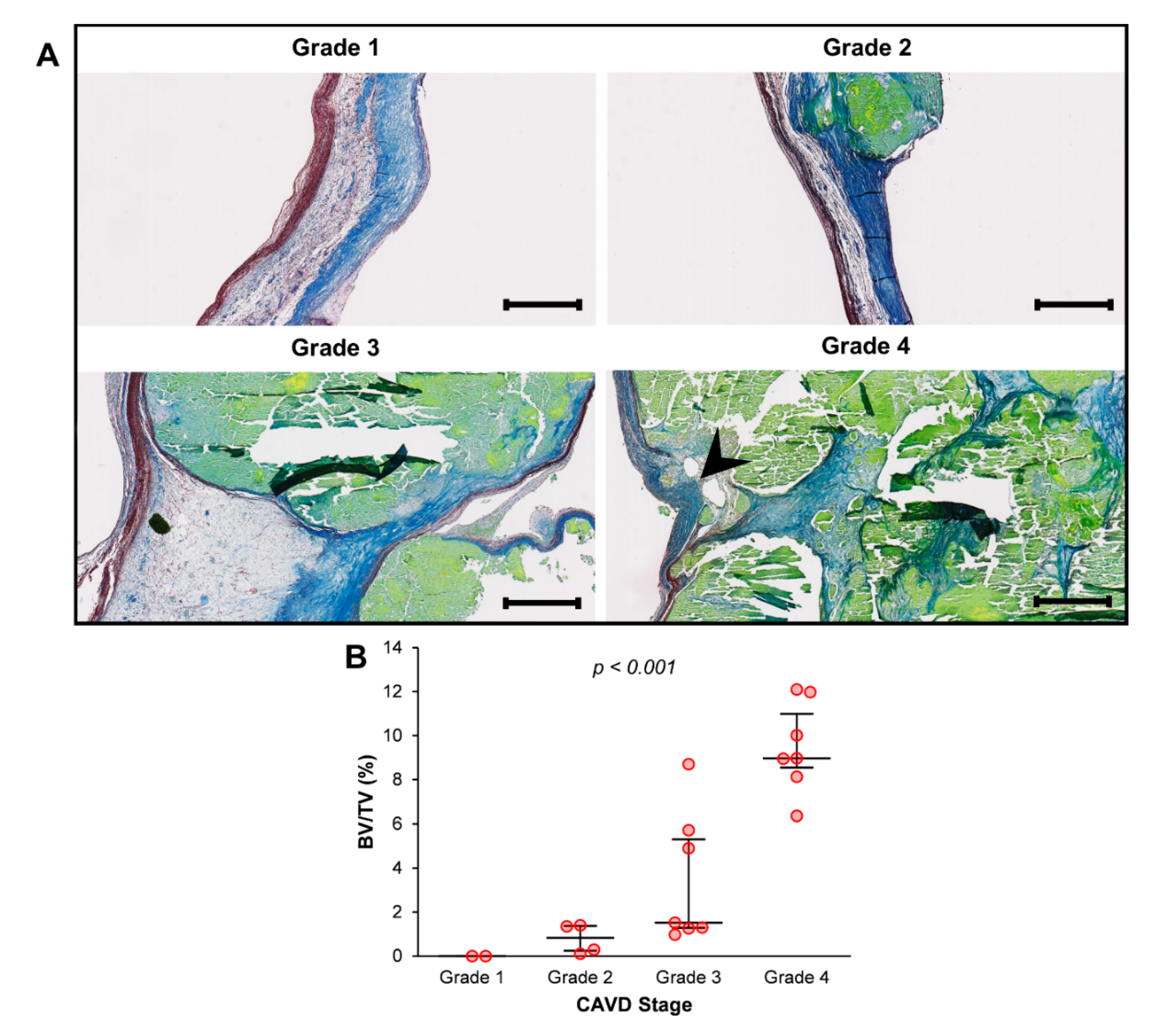
3.4. The Extent of Calcification as Measured by μCT Correlates with the Degree of Structural Change according to Histology
3.5. Macrophage Infiltration Correlates with the Extent of Calcification as Measured by μCT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Danielsen, R.; Aspelund, T.; Harris, T.B.; Gudnason, V. The prevalence of aortic stenosis in the elderly in Iceland and predictions for the coming decades: The AGES-Reykjavik study. Int. J. Cardiol. 2014, 176, 916–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendez-Bailon, M.; Lorenzo-Villalba, N.; Muñoz-Rivas, N.; de Miguel-Yanes, J.M.; de Miguel-Diez, J.; Comin-Colet, J.; Hernandez-Barrera, V.; Jimenez-Garcia, R.; Lopez-de-Andres, A. Transcatheter aortic valve implantation and surgical aortic valve replacement among hospitalized patients with and without type 2 diabetes mellitus in Spain (2014–2015). Cardiovasc. Diabetol. 2017, 16, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carabello, B.A.; Paulus, W.J. Aortic stenosis. Lancet 2009, 373, 956–966. [Google Scholar] [CrossRef]
- Lindman, B.R.; Clavel, M.A.; Mathieu, P.; Iung, B.; Lancellotti, P.; Otto, C.M.; Pibarot, P. Calcific aortic stenosis. Nat. Rev. Dis. Primers 2016, 2, 16006. [Google Scholar] [CrossRef] [Green Version]
- Olsson, M.; Thyberg, J.; Nilsson, J. Presence of oxidized low density lipoprotein in nonrheumatic stenotic aortic valves. Arterioscler. Thromb. Vasc. Biol. 1999, 19, 1218–1222. [Google Scholar] [CrossRef] [Green Version]
- Zheng, K.H.; Tsimikas, S.; Pawade, T.; Kroon, J.; Jenkins, W.S.A.; Doris, M.K.; White, A.C.; Timmers, N.; Hjortnaes, J.; Rogers, M.A.; et al. Lipoprotein(a) and Oxidized Phospholipids Promote Valve Calcification in Patients With Aortic Stenosis. J. Am. Coll. Cardiol. 2019, 73, 2150–2162. [Google Scholar] [CrossRef]
- Cote, N.; Mahmut, A.; Bosse, Y.; Couture, C.; Page, S.; Trahan, S.; Boulanger, M.C.; Fournier, D.; Pibarot, P.; Mathieu, P. Inflammation is associated with the remodeling of calcific aortic valve disease. Inflammation 2013, 36, 573–581. [Google Scholar] [CrossRef]
- Helske, S.; Syvaranta, S.; Kupari, M.; Lappalainen, J.; Laine, M.; Lommi, J.; Turto, H.; Mayranpaa, M.; Werkkala, K.; Kovanen, P.T.; et al. Possible role for mast cell-derived cathepsin G in the adverse remodelling of stenotic aortic valves. Eur. Heart J. 2006, 27, 1495–1504. [Google Scholar] [CrossRef] [Green Version]
- Bakhshian Nik, A.; Hutcheson, J.D.; Aikawa, E. Extracellular vesicles as mediators of cardiovascular calcification. Front. Cardiovasc. Med. 2017, 4, 78. [Google Scholar] [CrossRef] [Green Version]
- Jansen, F.; Xiang, X.; Werner, N. Role and function of extracellular vesicles in calcific aortic valve disease. Eur. Heart J. 2017, 38, 2714–2716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohler, E.R., III; Gannon, F.; Reynolds, C.; Zimmerman, R.; Keane, M.G.; Kaplan, F.S. Bone formation and inflammation in cardiac valves. Circulation 2001, 103, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Rajamannan, N.M.; Subramaniam, M.; Rickard, D.; Stock, S.R.; Donovan, J.; Springett, M.; Orszulak, T.; Fullerton, D.A.; Tajik, A.J.; Bonow, R.O.; et al. Human aortic valve calcification is associated with an osteoblast phenotype. Circulation 2003, 107, 2181–2184. [Google Scholar] [CrossRef] [PubMed]
- Messika-Zeitoun, D.; Aubry, M.C.; Detaint, D.; Bielak, L.F.; Peyser, P.A.; Sheedy, P.F.; Turner, S.T.; Breen, J.F.; Scott, C.; Tajik, A.J.; et al. Evaluation and clinical implications of aortic valve calcification measured by electron-beam computed tomography. Circulation 2004, 110, 356–362. [Google Scholar] [CrossRef] [Green Version]
- Koos, R.; Mahnken, A.H.; Sinha, A.M.; Wildberger, J.E.; Hoffmann, R.; Kuhl, H.P. Preliminary experience in the assessment of aortic valve calcification by ECG-gated multislice spiral computed tomography. Int. J. Cardiol. 2005, 102, 195–200. [Google Scholar] [CrossRef]
- Cueff, C.; Serfaty, J.M.; Cimadevilla, C.; Laissy, J.P.; Himbert, D.; Tubach, F.; Duval, X.; Iung, B.; Enriquez-Sarano, M.; Vahanian, A.; et al. Measurement of aortic valve calcification using multislice computed tomography: Correlation with haemodynamic severity of aortic stenosis and clinical implication for patients with low ejection fraction. Heart 2011, 97, 721–726. [Google Scholar] [CrossRef]
- Chitsaz, S.; Gundiah, N.; Blackshear, C.; Tegegn, N.; Yan, K.S.; Azadani, A.N.; Hope, M.; Tseng, E.E. Correlation of calcification on excised aortic valves by micro-computed tomography with severity of aortic stenosis. J. Heart Valve. Dis. 2012, 21, 320–327. [Google Scholar]
- Mazur, P.; Wypasek, E.; Gaweda, B.; Sobczyk, D.; Kapusta, P.; Natorska, J.; Malinowski, K.P.; Tarasiuk, J.; Bochenek, M.; Wronski, S.; et al. Stenotic Bicuspid and Tricuspid Aortic Valves—Micro-Computed Tomography and Biological Indices of Calcification. Circ. J. 2017, 81, 1043–1050. [Google Scholar] [CrossRef] [Green Version]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS); Vahanian, A.; Alfieri, O.; Andreotti, F.; Antunes, M.J.; Baron-Esquivias, G.; Baumgartner, H.; Borger, M.A.; Carrel, T.P.; et al. Guidelines on the management of valvular heart disease (version 2012). Eur. Heart J. 2012, 33, 2451–2496. [Google Scholar] [CrossRef] [Green Version]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press. 2014, 23, 3–16. [Google Scholar] [CrossRef]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Bairey Merz, C.N.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2889–2934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33 (Suppl. 1), S62–S69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ‘Kidney Disease: Improving Global Outcomes’ Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 5–14. [Google Scholar]
- Dempster, D.W.; Compston, J.E.; Drezner, M.K.; Glorieux, F.H.; Kanis, J.A.; Malluche, H.; Meunier, P.J.; Ott, S.M.; Recker, R.R.; Parfitt, A.M. Standardized nomenclature, symbols, and units for bone histomorphometry: A 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J. Bone Miner. Res. 2013, 28, 2–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García del Moral, R. Laboratorio de Anatomía Patológica; McGraw-Hill Interamericana de España: Madrid, Spain, 2003. [Google Scholar]
- Warren, B.A.; Yong, J.L. Calcification of the aortic valve: Its progression and grading. Pathology 1997, 29, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruifrok, A.C.; Johnston, D.A. Quantification of histochemical staining by color deconvolution. Anal. Quant. Cytol. Histol. 2001, 23, 291–299. [Google Scholar]
- Thery, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750. [Google Scholar] [CrossRef] [Green Version]
- Baietti, M.F.; Zhang, Z.; Mortier, E.; Melchior, A.; Degeest, G.; Geeraerts, A.; Ivarsson, Y.; Depoortere, F.; Coomans, C.; Vermeiren, E.; et al. Syndecan-syntenin-ALIX regulates the biogenesis of exosomes. Nat. Cell Biol. 2012, 14, 677–685. [Google Scholar] [CrossRef]
- Higgins, C.L.; Marvel, S.A.; Morrisett, J.D. Quantification of calcification in atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1567–1576. [Google Scholar] [CrossRef] [Green Version]
- Boughner, D.R.; Thornton, M.; Dunmore-Buyze, J.; Holdsworth, D.W. The radiographic quantitation of aortic valve calcification: Implications for assessing bioprosthetic valve calcification in vitro. Physiol. Meas. 2000, 21, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Dullin, C.; Ufartes, R.; Larsson, E.; Martin, S.; Lazzarini, M.; Tromba, G.; Missbach-Guentner, J.; Pinkert-Leetsch, D.; Katschinski, D.M.; Alves, F. µCT of ex-vivo stained mouse hearts and embryos enables a precise match between 3D virtual histology, classical histology and immunochemistry. PLoS ONE 2017, 12, e0170597. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Stallons, M.V.; Wirrig-Schwendeman, E.E.; Hassel, K.R.; Conway, S.J.; Yutzey, K.E. Bone Morphogenetic Protein Signaling Is Required for Aortic Valve Calcification. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 1398–1405. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, I.; Moraca, F.M.; Sciangula, A.; Aquila, S.; Mazzulla, S. HIF-1α and VEGF: Immunohistochemical profile and possible function in human aortic valve stenosis. Ultrastruct. Pathol. 2015, 39, 198–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- New, S.E.; Goettsch, C.; Aikawa, M.; Marchini, J.F.; Shibasaki, M.; Yabusaki, K.; Libby, P.; Shanahan, C.M.; Croce, K.; Aikawa, E. Macrophage-derived matrix vesicles: An alternative novel mechanism for microcalcification in atherosclerotic plaques. Circ. Res. 2013, 113, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Rashdan, N.A.; Zhu, D.; Milne, E.M.; Ajuh, P.; Milne, G.; Helfrich, M.H.; Lim, K.; Prasad, S.; Lerman, D.A.; et al. End stage renal disease-induced hypercalcemia may promote aortic valve calcification via Annexin VI enrichment of valve interstitial cell derived-matrix vesicles. J. Cell. Physiol. 2017, 232, 2985–2995. [Google Scholar] [CrossRef] [Green Version]
- Leroyer, A.S.; Isobe, H.; Leseche, G.; Castier, Y.; Wassef, M.; Mallat, Z.; Binder, B.R.; Tedgui, A.; Boulanger, C.M. Cellular origins and thrombogenic activity of microparticles isolated from human atherosclerotic plaques. J. Am. Coll. Cardiol. 2007, 49, 772–777. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.L.; Chang, H.H.; Huang, P.J.; Wang, W.C.; Lin, S.Y. Different Calcification Stage in Each Cusp of a Calcified Tricuspid Aortic Valve. Circ. J. 2017, 81, 1953–1955. [Google Scholar] [CrossRef] [Green Version]
- Solache-Berrocal, G.; Barral, A.; Martín, M.; Román-García, P.; Llosa, J.; Naves-Díaz, M.; Cannata-Andía, J.; Rodríguez, I. The association of MMP1 1G > 2G polymorphism with aortic valve calcification. Rev. Osteoporos. Metab. Miner. 2016, 8, 115–120. [Google Scholar] [CrossRef]



| Total | Type of Aortic Valve Disease | p-Value | |||
|---|---|---|---|---|---|
| Regurgitation | Stenosis | Mixed | |||
| N = 57 | N = 6 | N = 38 | N = 13 | ||
| Age, years | 69.6 (11.1) | 70.5 (7.6) | 70.7 (10.8) | 66.0 (13.1) | 0.415 |
| Sex | |||||
| Male | 33 (57.9) | 5 (83.3) | 20 (52.6) | 8 (61.5) | 0.425 |
| Female | 24 (42.1) | 1 (16.7) | 18 (47.4) | 5 (38.5) | |
| Valve Anatomy | |||||
| Tricuspid | 41 (71.9) | 6 (100.0) | 27 (71.1) | 8 (61.5) | 0.188 |
| Bicuspid | 11 (19.3) | 0 (0.0) | 6 (15.8) | 5 (38.5) | |
| Other | 5 (8.8) | 0 (0.0) | 5 (13.2) | 0 (0.0) | |
| BMI, kg/m2 | 29.6 (4.3) | 29.3 (3.3) | 29.8 (4.1) | 29.3 (5.5) | 0.913 |
| Smoker Status | |||||
| Non-Smoker | 35 (61.4) | 2 (33.3) | 24 (63.1) | 9 (69.2) | 0.108 |
| Former Smoker | 13 (22.8) | 4 (66.7) | 8 (21.1) | 1 (7.7) | |
| Current Smoker | 9 (15.8) | 0 (0.0) | 6 (15.8) | 3 (23.1) | |
| Hypertension | |||||
| Yes | 40 (70.2) | 6 (100.0) | 22 (57.9) | 12 (92.3) | 0.019 |
| No | 17 (29.8) | 0 (0.0) | 16 (42.1) | 1 (7.7) | |
| Hyperlipidaemia | |||||
| Yes | 25 (43.9) | 3 (50.0) | 17 (44.7) | 5 (38.5) | 0.923 |
| No | 32 (56.1) | 3 (50.0) | 21 (55.3) | 8 (61.5) | |
| Diabetes | |||||
| Yes | 11 (19.3) | 1 (16.7) | 8 (21.1) | 2 (15.4) | 1.000 |
| No | 46 (80.7) | 5 (83.3) | 30 (79.8) | 11 (84.6) | |
| eGFR, mL/min/1.73 m2 | 76.3 (18.9) | 63.9 (13.0) | 76.1 (19.1) | 83.0 (18.5) | 0.121 |
| Echocardiography | |||||
| Mean Gradient, mmHg | 47.3 (15.0) | 28.2 (25.1) | 50.9 (11.6) | 43.4 (15.6) | 0.007 |
| Peak Jet Velocity, m/s | 4.3 (0.8) | 3.2 (1.5) | 4.5 (0.5) | 4.2 (0.8) | 0.002 |
| LVEF | |||||
| Preserved | 48 (84.2) | 5 (83.3) | 30 (79.8) | 13 (100.0) | 0.731 |
| Mildly Reduced | 2 (3.5) | 0 (0.0) | 2 (5.3) | 0 (0.0) | |
| Moderately Reduced | 5 (8.8) | 1 (16.7) | 4 (10.5) | 0 (0.0) | |
| Severely Reduced | 2 (3.5) | 0 (0.0) | 2 (5.3) | 0 (0.0) | |
| BV/TV | p-Value | |
|---|---|---|
| % | ||
| Sex | ||
| Male | 4.0 (3.6) | 0.379 |
| Female | 4.8 (2.9) | |
| Diagnosis | ||
| Stenosis | 5.1 (3.5) | 0.006 |
| Regurgitation | 0.3 (0.5) | |
| Mixed | 3.8 (2.3) | |
| Valve Anatomy | ||
| Tricuspid | 3.6 (3.0) | 0.020 |
| Bicuspid | 6.7 (3.0) | |
| Other | 4.9 (4.4) | |
| Ascending Aorta | ||
| Normal | 3.8 (3.0) | < 0.001 |
| Dilated | 8.7 (2.6) | |
| Hypertension | ||
| Yes | 3.6 (2.9) | 0.070 |
| No | 6.0 (3.7) | |
| Hyperlipidaemia | ||
| Yes | 4.2 (3.5) | 0.816 |
| No | 4.4 (3.2) | |
| Diabetes | ||
| Yes | 4.4 (3.3) | 0.472 |
| No | 3.9 (3.6) | |
| Chronic Kidney Disease | ||
| Yes | 3.8 (3.5) | 0.574 |
| No | 4.5 (3.3) | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solache-Berrocal, G.; Barral-Varela, A.M.; Areces-Rodríguez, S.; Junco-Vicente, A.; Vallina-Álvarez, A.; Corte-Torres, M.D.; Valdivielso, J.M.; Llosa, J.C.; Morís, C.; Martín, M.; et al. Correlation of Micro-Computed Tomography Assessment of Valvular Mineralisation with Histopathological and Immunohistochemical Features of Calcific Aortic Valve Disease. J. Clin. Med. 2020, 9, 29. https://doi.org/10.3390/jcm9010029
Solache-Berrocal G, Barral-Varela AM, Areces-Rodríguez S, Junco-Vicente A, Vallina-Álvarez A, Corte-Torres MD, Valdivielso JM, Llosa JC, Morís C, Martín M, et al. Correlation of Micro-Computed Tomography Assessment of Valvular Mineralisation with Histopathological and Immunohistochemical Features of Calcific Aortic Valve Disease. Journal of Clinical Medicine. 2020; 9(1):29. https://doi.org/10.3390/jcm9010029
Chicago/Turabian StyleSolache-Berrocal, Guillermo, Ana María Barral-Varela, Sheila Areces-Rodríguez, Alejandro Junco-Vicente, Aitana Vallina-Álvarez, María Daniela Corte-Torres, José Manuel Valdivielso, Juan Carlos Llosa, César Morís, María Martín, and et al. 2020. "Correlation of Micro-Computed Tomography Assessment of Valvular Mineralisation with Histopathological and Immunohistochemical Features of Calcific Aortic Valve Disease" Journal of Clinical Medicine 9, no. 1: 29. https://doi.org/10.3390/jcm9010029
APA StyleSolache-Berrocal, G., Barral-Varela, A. M., Areces-Rodríguez, S., Junco-Vicente, A., Vallina-Álvarez, A., Corte-Torres, M. D., Valdivielso, J. M., Llosa, J. C., Morís, C., Martín, M., & Rodríguez, I. (2020). Correlation of Micro-Computed Tomography Assessment of Valvular Mineralisation with Histopathological and Immunohistochemical Features of Calcific Aortic Valve Disease. Journal of Clinical Medicine, 9(1), 29. https://doi.org/10.3390/jcm9010029





