Whole Ovary Cryopreservation and Transplantation: A Systematic Review of Challenges and Research Developments in Animal Experiments and Humans
Abstract
1. Introduction
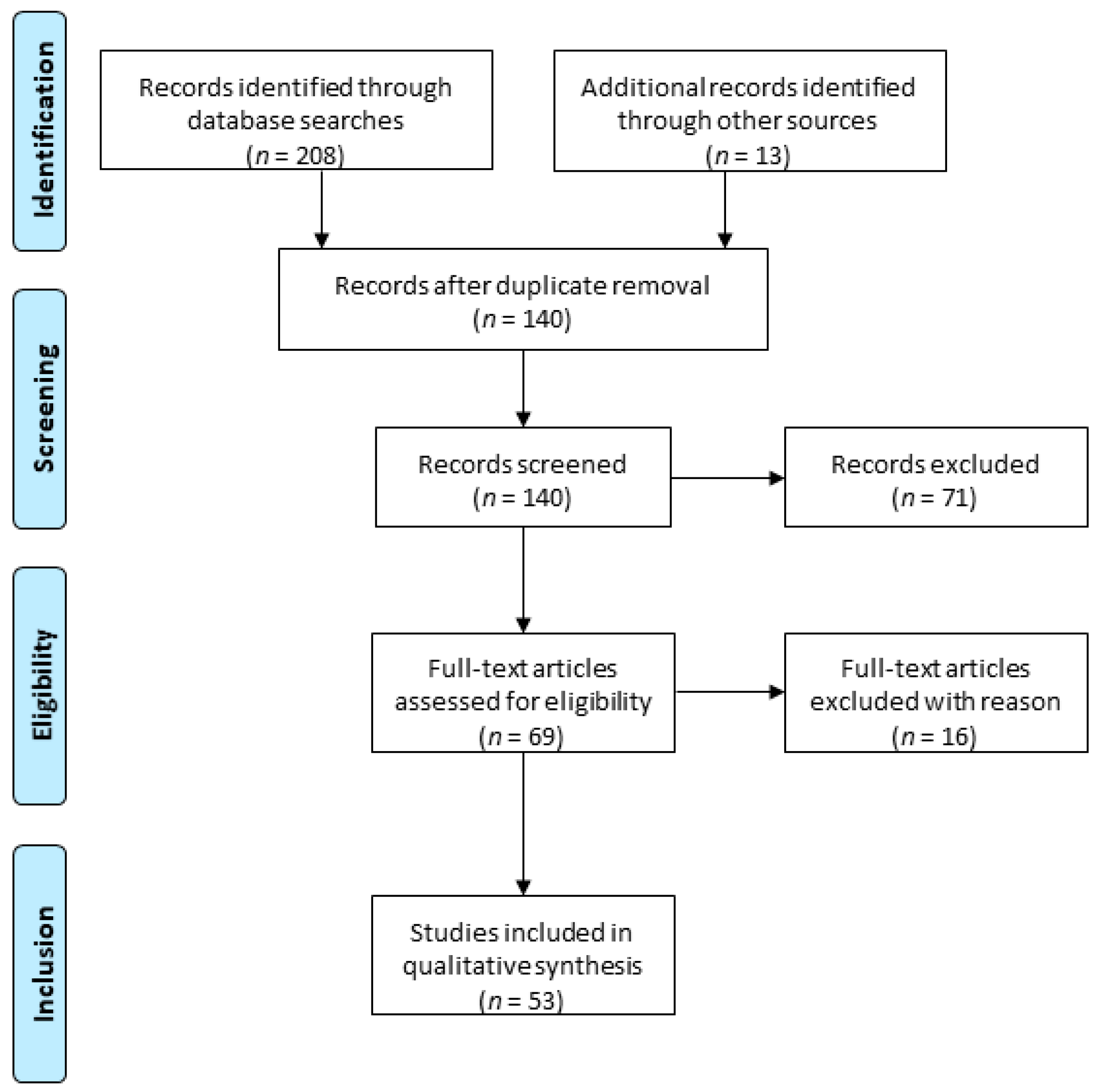
2. Methodology
3. Challenges and Solutions
3.1. Whole Ovary Removal
3.2. Freezing of a Whole Ovary
3.2.1. Freezing Challenges
3.2.2. Freezing Solutions
Slow freezing
Vitrification
Directional freezing
3.3. Vascular Transplantation of a Whole Ovary
3.3.1. Vascular Transplantation Challenges
3.3.2. Vascular Transplantation Solutions
Rodents
Sheep
4. What Has Been Done in Humans So Far?
4.1. Fresh Whole Ovary Transplantation
4.2. Whole ovary Removal with a View to Cryopreservation
4.3. Cryopreservation of the Human Ovary
4.4. Recipient Pedicle Selection for Vascular Transplantation
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Global Cancer Observatory. 2018. Available online: http://gco.iarc.fr (accessed on 9 June 2020).
- Howell, S.; Shalet, S. Gonadal damage from chemotherapy and radiotherapy. Endocrinol. Metab. Clin. N. Am. 1998, 27, 927–943. [Google Scholar] [CrossRef]
- Meirow, D.; Nugent, D. The effects of radiotherapy and chemotherapy on female reproduction. Hum. Reprod. Update 2001, 7, 535–543. [Google Scholar] [CrossRef]
- Kanumakala, S.; Warne, G.L.; Zacharin, M.R. Evolving hypopituitarism following cranial irradiation. J. Paediatr. Child. Health 2003, 39, 232–235. [Google Scholar] [CrossRef]
- Wallace, W.H.; Anderson, R.A.; Irvine, D.S. Fertility preservation for young patients with cancer: Who is at risk and what can be offered? Lancet Oncol. 2005, 6, 209–218. [Google Scholar] [CrossRef]
- Donnez, J.; Dolmans, M.M. Fertility preservation in women. N. Engl. J. Med. 2017, 377, 1657–1665. [Google Scholar] [CrossRef]
- Arian, S.E.; Goodman, L.; Flyckt, R.L.; Falcone, T. Ovarian transposition: A surgical option for fertility preservation. Fert. Steril. 2017, 107, e15. [Google Scholar] [CrossRef]
- Crafton, S.M.; Cohn, D.E.; Llamocca, E.N.; Louden, E.; Rhoades, J.; Felix, A.S. Fertility-sparing surgery and survival among reproductive-age women with epithelial ovarian cancer in 2 cancer registries. Cancer 2020, 126, 1217–1224. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Dolmans, M.M. Fertility preservation in women. Nat. Rev. Endocrinol. 2013, 9, 735–749. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Squifflet, J.; Jadoul, P.; Lousse, J.C.; Dolmans, M.M.; Donnez, O. Fertility preservation in women with ovarian endometriosis. Front. Biosci. 2012, 4, 1654–1662. [Google Scholar] [CrossRef]
- Raffi, F.; Metwally, M.; Amer, S. The impact of excision of ovarian endometrioma on ovarian reserve: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2012, 97, 3146–3154. [Google Scholar] [CrossRef] [PubMed]
- Chapman, C.; Cree, L.; Shelling, A.N. The genetics of premature ovarian failure: Current perspectives. Int. J. Womens Health 2015, 7, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Beck-Peccoz, P.; Persani, L. Premature ovarian failure. Orphanet. J. Rare Dis. 2006, 1, 9. [Google Scholar] [CrossRef] [PubMed]
- Faubion, S.S.; Kuhle, C.L.; Shuster, L.T.; Rocca, W.A. Long-term health consequences of premature or early menopause and considerations for management. Climacteric 2015, 18, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: A committee opinion. Fertil. Steril. 2019, 112, 1022–1033. [Google Scholar] [CrossRef] [PubMed]
- Dolmans, M.M. Recent advances in fertility preservation and counseling for female cancer patients. Expert Rev. Anticancer. Ther. 2018, 18, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Wallace, W.H.B.; Smith, A.G.; Kelsey, T.W.; Edgar, A.E.; Anderson, R.A. Fertility preservation for girls and young women with cancer: Population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014, 15, 1129–1136. [Google Scholar] [CrossRef]
- Donnez, J.; Martinez-Madrid, B.; Jadoul, P.; Van Langendonckt, A.; Demylle, D.; Dolmans, M.M. Ovarian tissue cryopreservation and transplantation: A review. Hum. Reprod. Update 2006, 12, 519–535. [Google Scholar] [CrossRef]
- Jadoul, P.; Guilmain, A.; Squifflet, J.; Luyckx, M.; Votino, R.; Wyns, C.; Dolmans, M.M. Efficacy of ovarian tissue cryopreservation for fertility preservation: Lessons learned from 545 cases. Hum. Reprod. 2017, 32, 1046–1054. [Google Scholar] [CrossRef]
- Gellert, S.E.; Pors, S.E.; Kristensen, S.G.; Bay-Bjørn, A.M.; Ernst, E.; Andersen, C.Y. Transplantation of frozen-thawed ovarian tissue: An update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J. Assist. Reprod. Genet. 2018, 35, 561–570. [Google Scholar] [CrossRef]
- Roness, H.; Meirow, D. FERTILITY PRESERVATION: Follicle reserve loss in ovarian tissue transplantation. Reproduction 2019, 158, F35–F44. [Google Scholar] [CrossRef]
- Dolmans, M.M.; Falcone, T.; Patrizio, P. Importance of patient selection to analyze in vitro fertilization outcome with transplanted cryopreserved ovarian tissue. Fertil. Steril. 2020, 114, 279–280. [Google Scholar] [CrossRef] [PubMed]
- Demeestere, I.; Simon, P.; Emiliani, S.; Delbaere, A.; Englert, Y. Fertility preservation: Successful transplantation of cryopreserved ovarian tissue in a young patient previously treated for Hodgkin’s Disease. Oncologist 2007, 12, 1437–1442. [Google Scholar] [CrossRef] [PubMed]
- Meirow, D.; Levron, J.; Eldar-Geva, T.; Hardan, I.; Fridman, E.; Yemini, Z.; Dor, J. Monitoring the ovaries after autotransplantation of cryopreserved ovarian tissue: Endocrine studies, in vitro fertilization cycles, and live birth. Fertil. Steril. 2007, 87, 418-e7–418-e15. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Dolmans, M.M. Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J. Assist. Reprod. Genet. 2015, 32, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Van der Elst, J.; Van den Broecke, R.; Dhont, M. Early massive follicle loss and apoptosis in heterotopically grafted newborn mouse ovaries. Hum. Reprod. 2002, 17, 605–611. [Google Scholar] [CrossRef]
- Dolmans, M.M.; Martinez-Madrid, B.; Gadisseux, E.; Guiot, Y.; Yuan, W.Y.; Torre, A.; Camboni, A.; Van Langendonckt, A.; Donnez, J. Short-term transplantation of isolated human ovarian follicles and cortical tissue into nude mice. Reproduction 2007, 134, 253–262. [Google Scholar] [CrossRef]
- Hancke, K.; Walker, E.; Strauch, O.; Göbel, H.; Hanjalic-Beck, A.; Denschlag, D. Ovarian transplantation for fertility preservation in a sheep model: Can follicle loss be prevented by antiapoptotic sphingosine-1-phosphate administration? Gynecol. Endocrinol. 2009, 25, 839–843. [Google Scholar] [CrossRef]
- Dath, C.; Van Eyck, A.S.; Dolmans, M.M.; Romeu, L.; Delle Vigne, L.; Donnez, J.; Van Langendonckt, A. Xenotransplantation of human ovarian tissue to nude mice: Comparison between four grafting sites. Hum. Reprod. 2010, 25, 1734–1743. [Google Scholar] [CrossRef]
- Gavish, Z.; Spector, I.; Peer, G.; Schlatt, S.; Wistuba, J.; Roness, H.; Meirow, D. Follicle activation is a significant and immediate cause of follicle loss after ovarian tissue transplantation. J. Assist. Reprod Genet. 2018, 35, 61–69. [Google Scholar] [CrossRef]
- Baird, D.T.; Webb, R.; Campbell, B.K.; Harkness, L.M.; Gosden, R.G. Long-term ovarian function in sheep after ovariectomy and transplantation of autografts stored at -196 C. Endocrinology 1999, 140, 462–471. [Google Scholar] [CrossRef]
- Van Eyck, A.S.; Jordan, B.F.; Gallez, B.; Heilier, J.F.; Van Langendonckt, A.; Donnez, J. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. Fertil. Steril. 2009, 92, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Van Eyck, A.S.; Bouzin, C.; Feron, O.; Romeu, L.; Van Langendonckt, A.; Donnez, J.; Dolmans, M.M. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in a murine model. Fertil. Steril. 2010, 93, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Bedaiwy, M.A.; Shahin, A.Y.; Falcone, T. Reproductive organ transplantation: Advances and controversies. Fertil. Steril. 2008, 90, 2031–2055. [Google Scholar] [CrossRef] [PubMed]
- Bromer, J.G.; Patrizio, P. Fertility preservation: The rationale for cryopreservation of the whole ovary. Semin. Reprod. Med. 2009, 27, 465–471. [Google Scholar] [CrossRef]
- Brannström, M.; Milenkovic, M. Whole ovary cryopreservation with vascular transplantation—A future development in female oncofertility. Middle East. Fertil. Soc. J. 2010, 15, 125–138. [Google Scholar] [CrossRef]
- Arav, A.; Patrizio, P. Techniques of Cryopreservation for Ovarian Tissue and Whole Ovary. Clin. Med. Insights Reprod. Health 2019, 13, 1179558119884945. [Google Scholar] [CrossRef]
- Campbell, B.K.; Hernandez-Medrano, J.; Onions, V.; Pincott-Allen, C.; Aljaser, F.; Fisher, J.; McNeilly, A.S.; Webb, R.; Picton, H.M. Restoration of ovarian function and natural fertility following the cryopreservation and autotransplantation of whole adult sheep ovaries. Hum. Reprod. 2014, 29, 1749–1763. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Imhof, M.; Bergmeister, H.; Lipovac, M.; Rudas, M.; Hofstetter, G.; Huber, J. Orthotopic microvascular reanastomosis of whole cryopreserved ovine ovaries resulting in pregnancy and live birth. Fertil. Steril. 2006, 85, 1208–1215. [Google Scholar] [CrossRef]
- Torre, A.; Vertu-Ciolino, D.; Mazoyer, C.; Selva, J.; Lornage, J.; Salle, B. Safeguarding Fertility With Whole Ovary Cryopreservation and Microvascular Transplantation: Higher Follicular Survival With Vitrification Than With Slow Freezing in a Ewe Model. Transplantation 2016, 100, 1889–1897. [Google Scholar] [CrossRef]
- Jadoul, P.; Donnez, J.; Dolmans, M.M.; Squifflet, J.; Lengelé, B.; Martinez-Madrid, B. Laparoscopic ovariectomy for whole human ovary cryopreservation: Technical aspects. Fertil. Steril. 2007, 87, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Ploteau, S.; Rogez, J.M.; Donnez, J.; Lengelé, B. Which are the ideal donor and recipient vessels for a whole ovarian transplantation? Fertil. Steril. 2011, 95, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Isachenko, V.; Isachenko, E.; Peters, D.; Mallmann, P.; Morgenstern, B.; Kellerwessel, E.; Otarbaev, M.; Baikoshkarova, S.; Shalakhmetova, T.; Rahimi, G. In vitro perfusion of whole bovine ovaries by freezing medium: Effect of perfusion rate and elapsed time after extraction. Clin. Lab. 2013, 59, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Isachenko, V.; Isachenko, E.; Sanchez, R.; Dattena, M.; Mallmann, P.; Rahimi, G. Cryopreservation of whole ovine ovaries with pedicles as a model for human: Parameters of perfusion with simultaneous saturations by cryoprotectants. Clin. Lab. 2015, 61, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Westphal, J.R.; Gerritse, R.; Braat, D.D.M.; Beerendonk, C.C.M.; Peek, R. Complete protection against cryodamage of cryopreserved whole bovine and human ovaries using DMSO as a cryoprotectant. J. Assist. Reprod. Genet. 2017, 34, 1217–1229. [Google Scholar] [CrossRef]
- Jeremias, E.; Bedaiwy, M.A.; Gurunluoglu, R.; Biscotti, C.V.; Siemionow, M.; Falcone, T. Heterotopic autotransplantation of the ovary with microvascular anastomosis: A novel surgical technique. Fertil. Steril. 2002, 77, 1278–1282. [Google Scholar] [CrossRef]
- Bedaiwy, M.A.; Jeremias, E.; Gurunluoglu, R.; Hussein, M.R.; Siemianow, M.; Biscotti, C.; Falcone, T. Restoration of ovarian function after autotransplantation of intact frozen-thawed sheep ovaries with microvascular anastomosis. Fertil. Steril. 2003, 79, 594–602. [Google Scholar] [CrossRef]
- Bedaiwy, M.A.; Falcone, T. Harvesting and autotransplantation of vascularized ovarian grafts: Approaches and techniques. Reprod. Biomed. Online 2007, 14, 360–371. [Google Scholar] [CrossRef]
- Grazul-Bilska, A.T.; Banerjee, J.; Yazici, I.; Borowczyk, E.; Bilski, J.J.; Sharma, R.K.; Siemionov, M.; Falcone, T. Morphology and function of cryopreserved whole ovine ovaries after heterotopic autotransplantation. Reprod. Biol. Endocrinol. 2008, 6, 16. [Google Scholar] [CrossRef]
- Silber, S.J.; Grudzinskas, G.; Gosden, R.G. Successful pregnancy after microsurgical transplantation of an intact ovary. N. Engl. J. Med. 2008, 359, 2617–2618. [Google Scholar] [CrossRef]
- Fahy, G.M.; Wowk, B.; Wu, J. Cryopreservation of complex systems: The missing link in the regenerative medicine supply chain. Rejuvenation Res. 2006, 9, 279–291. [Google Scholar] [CrossRef]
- Woods, E.J.; Benson, J.D.; Agca, Y.; Critser, J.K. Fundamental cryobiology of reproductive cells and tissues. Cryobiology 2004, 48, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Gacitua, H.; Arav, A. Successful pregnancies with directional freezing of large volume buck semen. Theriogenology 2005, 63, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Pegg, D.E. Principles of cryopreservation. Methods Mol. Biol. 2007, 368, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Gavish, Z.; Ben-Haim, M.; Arav, A. Cryopreservation of whole murine and porcine livers. Rejuvenation Res. 2008, 11, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Arav, A.; Natan, Y. Directional freezing: A solution to the methodological challenges to preserve large organs. Semin. Reprod. Med. 2009, 27, 438–442. [Google Scholar] [CrossRef]
- Bruinsma, B.G.; Uygun, K. Subzero organ preservation: The dawn of a new ice age? Curr. Opin. Organ. Transplant. 2017, 22, 281–286. [Google Scholar] [CrossRef]
- Finger, E.B.; Bischof, J.C. Cryopreservation by vitrification: A promising approach for transplant organ banking. Curr Opin Organ. Transplant. 2018, 23, 353–360. [Google Scholar] [CrossRef]
- Imhof, M.; Hofstetter, G.; Bergmeister, I.H.; Rudas, M.; Kain, R.; Lipovac, M.; Huber, J. Cryopreservation of a whole ovary as a strategy for restoring ovarian function. J. Assist. Reprod Genet. 2004, 21, 459–465. [Google Scholar] [CrossRef][Green Version]
- Wallin, A.; Ghahremani, M.; Dahm-Kähler, P.; Brännström, M. Viability and function of the cryopreserved whole ovary: In vitro studies in the sheep. Hum. Reprod. 2009, 24, 1684–1694. [Google Scholar] [CrossRef]
- Milenkovic, M.; Wallin, A.; Ghahremani, M.; Brännström, M. Whole sheep ovary cryopreservation: Evaluation of a slow freezing protocol with dimethylsulphoxide. J. Assist. Reprod Genet. 2011, 28, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Rubinsky, B.; Pegg, D.E. A mathematical model for the freezing process in biological tissue. Proc. R Soc. Lond. B Biol. Sci. 1988, 234, 343–358. [Google Scholar] [CrossRef]
- Brännström, M.; Díaz-García, C. Transplantation of female genital organs. J. Obstet. Gynaecol. Res. 2011, 37, 271–291. [Google Scholar] [CrossRef] [PubMed]
- Pegg, D.E. The relevance of ice crystal formation for the cryopreservation of tissues and organs. Cryobiology 2020, 93, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.; Ma, A.; Xu, D.; Daloze, P.; Chen, H. Cryopreservation of vascularized ovary: An evaluation of histology and function in rats. Microsurgery 2008, 28, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Courbière, B.; Caquant, L.; Mazoyer, C.; Franck, M.; Lornage, J.; Salle, B. Difficulties improving ovarian functional recovery by microvascular transplantation and whole ovary vitrification. Fertil. Steril. 2009, 91, 2697–2706. [Google Scholar] [CrossRef] [PubMed]
- Onions, V.J.; Webb, R.; McNeilly, A.S.; Campbell, B.K. Ovarian endocrine profile and long-term vascular patency following heterotopic autotransplantation of cryopreserved whole ovine ovaries. Hum. Reprod. 2009, 24, 2845–2855. [Google Scholar] [CrossRef] [PubMed]
- Fahy, G.M.; Wowk, B.; Wu, J.; Phan, J.; Rasch, C.; Chang, A.; Zendejas, E. Cryopreservation of organs by vitrification: Perspectives and recent advances. Cryobiology 2004, 48, 157–178, Erratum in: Cryobiology 2005, 50, 344. [Google Scholar] [CrossRef]
- Courbière, B.; Odagescu, V.; Baudot, A.; Massardier, J.; Mazoyer, C.; Salle, B.; Lornage, J. Cryopreservation of the ovary by vitrification as an alternative to slow-cooling protocols. Fertil. Steril. 2006, 86, 1243–1251. [Google Scholar] [CrossRef]
- Baudot, A.; Courbière, B.; Odagescu, V.; Salle, B.; Mazoyer, C.; Massardier, J.; Lornage, J. Towards whole sheep ovary cryopreservation. Cryobiology 2007, 55, 236–248. [Google Scholar] [CrossRef]
- Gerritse, R.; Beerendonk, C.C.; Tijink, M.S.; Heetkamp, A.; Kremer, J.A.; Braat, D.D.; Westphal, J.R. Optimal perfusion of an intact ovary as a prerequisite for successful ovarian cryopreservation. Hum. Reprod. 2008, 23, 329–335. [Google Scholar] [CrossRef]
- Torre, A.; Ben Brahim, F.; Popowski, T.; Boudjenah, R.; Salle, B.; Lornage, J. Factors related to unstained areas in whole ewe ovaries perfused with a metabolic marker. Hum. Reprod. 2013, 28, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Gerritse, R.; Beerendonk, C.C.; Westphal, J.R.; Bastings, L.; Braat, D.D.; Peek, R. Glucose/lactate metabolism of cryopreserved intact bovine ovaries as a novel quantitative marker to assess tissue cryodamage. Reprod Biomed. Online 2011, 23, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Isachenko, V.; Rahimi, G.; Dattena, M.; Mallmann, P.; Baikoshkarova, S.; Kellerwessel, E.; Otarbaev, M.; Shalakhmetova, T.; Isachenko, E. Whole ovine ovaries as a model for human: Perfusion with cryoprotectants in vivo and in vitro. Biomed. Res. Int. 2014, 2014, 409019. [Google Scholar] [CrossRef]
- Pegg, D.E. Perfusion of rabbit kidneys with cryoprotective agents. Cryobiology 1972, 9, 411–419. [Google Scholar] [CrossRef]
- Courbière, B.; Massardier, J.; Salle, B.; Mazoyer, C.; Guerin, J.F.; Lornage, J. Follicular viability and histological assessment after cryopreservation of whole sheep ovaries with vascular pedicle by vitrification. Fertil. Steril. 2005, 84, 1065–1071. [Google Scholar] [CrossRef]
- Onions, V.J.; Webb, R.; Pincott-Allen, C.; Picton, H.M.; Campbell, B.K. The effects of whole ovarian perfusion and cryopreservation on endothelial cell-related gene expression in the ovarian medulla and pedicle. Mol. Hum. Reprod. 2013, 19, 205–215. [Google Scholar] [CrossRef]
- Onions, V.J.; Mitchell, M.R.; Campbell, B.K.; Webb, R. Ovarian tissue viability following whole ovine ovary cryopreservation: Assessing the effects of sphingosine-1-phosphate inclusion. Hum. Reprod. 2008, 23, 606–618. [Google Scholar] [CrossRef][Green Version]
- Munn, C.S.; Kiser, L.C.; Wetzner, S.M.; Baer, J.E. Ovary volume in young and premenopausal adults: US determination. Work in progress. Radiology 1986, 159, 731–732. [Google Scholar] [CrossRef]
- Martinez-Madrid, B.; Dolmans, M.M.; Van Langendonckt, A.; Defrère, S.; Donnez, J. Freeze-thawing intact human ovary with its vascular pedicle with a passive cooling device. Fertil. Steril. 2004, 82, 1390–1394. [Google Scholar] [CrossRef]
- Martinez-Madrid, B.; Camboni, A.; Dolmans, M.M.; Nottola, S.; Van Langendonckt, A.; Donnez, J. Apoptosis and ultrastructural assessment after cryopreservation of whole human ovaries with their vascular pedicle. Fertil. Steril. 2007, 87, 1153–1165. [Google Scholar] [CrossRef]
- Gerritse, R.; Peek, R.; Sweep, F.; Thomas, C.; Braat, D.; Kremer, J.; Westphal, J.R.; Beerendonk, C. In vitro 17ß-oestradiol release as a marker for follicular survival in cryopreserved intact bovine ovaries. Cryo Lett. 2010, 31, 318–328. [Google Scholar]
- Zhang, J.M.; Sheng, Y.; Cao, Y.Z.; Wang, H.Y.; Chen, Z.J. Cryopreservation of whole ovaries with vascular pedicles: Vitrification or conventional freezing? J. Assist. Reprod. Genet. 2011, 28, 445–452. [Google Scholar] [CrossRef]
- Zhang, J.M.; Sheng, Y.; Cao, Y.Z.; Wang, H.Y.; Chen, Z.J. Effects of cooling rates and ice-seeding temperatures on the cryopreservation of whole ovaries. J. Assist. Reprod. Genet. 2011, 28, 627–633. [Google Scholar] [CrossRef]
- Du, T.; Chao, L.; Zhao, S.; Chi, L.; Li, D.; Shen, Y.; Shi, Q.; Deng, X. Successful cryopreservation of whole sheep ovary by using DMSO-free cryoprotectant. J. Assist. Reprod. Genet. 2015, 32, 1267–1275. [Google Scholar] [CrossRef]
- Fahy, G.M.; MacFarlane, D.R.; Angell, C.A.; Meryman, H.T. Vitrification as an approach to cryopreservation. Cryobiology 1984, 21, 407–426. [Google Scholar] [CrossRef]
- Yavin, S.; Arav, A. Measurement of essential physical properties of vitrification solutions. Theriogenology 2007, 67, 81–89. [Google Scholar] [CrossRef]
- Torre, A.; Momier, M.; Mazoyer, C.; Selva, J.; Salle, B.; Lornage, J. Validation of a new metabolic marker to assess the vascular viability of vitrified whole sheep ovaries. Hum. Reprod. 2012, 27, 1811–1821. [Google Scholar] [CrossRef][Green Version]
- Carvalho, A.A.; Faustino, L.R.; Silva, C.M.; Castro, S.V.; Lopes, C.A.; Santos, R.R.; Báo, S.N.; Figueiredo, J.R.; Rodrigues, A.P. Novel wide-capacity method for vitrification of caprine ovaries: Ovarian Tissue Cryosystem (OTC). Anim. Reprod. Sci. 2013, 138, 220–227. [Google Scholar] [CrossRef]
- Zhang, J.M.; Zhang, Y.C.; Ruan, L.H.; Wang, H.C. Optimizing cryoprotectant perfusion conditions for intact ovary: A bovine model. J. Assist. Reprod. Genet. 2012, 29, 1255–1260. [Google Scholar] [CrossRef]
- Gao, H.H.; Li, Z.P.; Wang, H.P.; Zhang, L.F.; Zhang, J.M. Cryopreservation of whole bovine ovaries: Comparisons of different thawing protocols. Eur J. Obstet. Gynecol. Reprod. Biol. 2016, 204, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Rall, W.F. Factors affecting the survival of mouse embryos cryopreserved by vitrification. Cryobiology 1987, 24, 387–402. [Google Scholar] [CrossRef]
- Arav, A.; Natan, D. Directional freezing of reproductive cells and organs. Reprod. Domest. Anim. 2012, 47, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Arav, A.; Revel, A.; Nathan, Y.; Bor, A.; Gacitua, H.; Yavin, S.; Gavish, Z.; Uri, M.; Elami, A. Oocyte recovery, embryo development and ovarian function after cryopreservation and transplantation of whole sheep ovary. Hum. Reprod. 2005, 20, 3554–3559. [Google Scholar] [CrossRef]
- Maffei, S.; Galeati, G.; Pennarossa, G.; Brevini, T.A.L.; Gandolfi, F. Extended ex vivo culture of fresh and cryopreserved whole sheep ovaries. Reprod. Fertil. Dev. 2016, 28, 1893–1903. [Google Scholar] [CrossRef]
- Maffei, S.; Hanenberg, M.; Pennarossa, G.; Silva, J.R.; Brevini, T.A.; Arav, A.; Gandolfi, F. Direct comparative analysis of conventional and directional freezing for the cryopreservation of whole ovaries. Fertil. Steril. 2013, 100, 1122–1131. [Google Scholar] [CrossRef]
- Maffei, S.; Pennarossa, G.; Brevini, T.A.; Arav, A.; Gandolfi, F. Beneficial effect of directional freezing on in vitro viability of cryopreserved sheep whole ovaries and ovarian cortical slices. Hum. Reprod. 2014, 29, 114–124. [Google Scholar] [CrossRef]
- Patrizio, P.; Gavish, Z.; Martel, M.; Azodi, M.; Silber, S.; Arav, A. Whole human ovaries cryopreservation using a novel multi-gradient freezing device. Fertil. Steril. 2007, 88, S355. [Google Scholar] [CrossRef]
- Patrizio, P.; Bromer, J.; Johnson, J.; Martel, M.; Silber, S.; Arav, A. Cryopreservation of eleven whole human ovaries: Histology, immunohistochemistry and technical details. Fertil. Steril. 2008, 90, S38. [Google Scholar] [CrossRef]
- Lotz, L.; Hauenstein, T.; Nichols-Burns, S.M.; Strissel, P.; Hoffmann, I.; Findeklee, S.; Dittrich, R.; Beckmann, M.W.; Oppelt, P.G. Comparison of Whole Ovary Cryotreatments for Fertility Preservation. Reprod. Domest. Anim. 2015, 50, 958–964. [Google Scholar] [CrossRef]
- Arav, A.; Gavish, Z.; Elami, A.; Natan, Y.; Revel, A.; Silber, S.; Gosden, R.G.; Patrizio, P. Ovarian function 6 years after cryopreservation and transplantation of whole sheep ovaries. Reprod. Biomed. Online 2010, 20, 48–52, Erratum in: Reprod. Biomed. Online 2017, 35, 751. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.R.; Hendrickson, M.; Lash, S.; Shelby, J. Pregnancy after tubo-ovarian transplantation. Obstet. Gynecol. 1987, 70, 229–234. [Google Scholar] [CrossRef]
- Wang, X.; Bilolo, K.K.; Qi, S.; Xu, D.; Jiang, W.; Vu, M.D.; Chen, H. Restoration of fertility in oophorectomized rats after tubo-ovarian transplantation. Microsurgery 2002, 22, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Shao, J.; Hua, K.; Wang, X. Modified Model of Whole Ovary Transplantation in Rats. Transplant. Proc. 2018, 50, 3881–3886. [Google Scholar] [CrossRef] [PubMed]
- Winston, R.M.; Browne, J.C. Pregnancy following autograft transplantation of Fallopian tube and ovary in the rabbit. Lancet 1974, 2, 494–495. [Google Scholar] [CrossRef]
- Green, C.J.; Simpkin, S.; Grimaldi, G. Pregnancy after autografting and allografting vascularized ovaries and en bloc vascularized ovaries with adnexa in rabbits. Br. J. Obstet. Gynaecol. 1982, 89, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Denjean, R.; Boeckx, W.; Gordts, S.; Brosens, I. Ovarian transplantation by selective microvascular anastomoses in the rabbit. Br. J. Obstet. Gynaecol. 1982, 89, 652–656. [Google Scholar] [CrossRef]
- Al Chalabi, H.A. Allotransplantation of the rabbit ovary: Experimental observations and their clinical relevance. J. Obstet. Gynaecol. 1991, 11, 137–144. [Google Scholar] [CrossRef]
- Carmona, F.; Balasch, J.; González-Merlo, J. Ovarian function, tubal viability and pregnancy after tubo-ovarian transplantation in the rabbit. Hum. Reprod. 1993, 8, 929–931. [Google Scholar] [CrossRef]
- Meraz, M.M.; Revilla, C.M.; Martínez, C.J.; Islas-Andrade, S.; Aburto, E.M. Restoration of endocrine function and fertility with a tubo-ovarian autotransplant as the anatomical-functional unit in rabbits using a vascular microsurgical technique. Transplant. Proc. 2006, 38, 945–951. [Google Scholar] [CrossRef]
- Meraz, M.M.; Gracida, C.J.; Melchor, J.L.; Revilla, C.M.; De Buen, N.; Aburto, E.M. Restoration of endocrine function and ovulation after a heterotopic ovarian transplant in the inguinal region of rabbits using a vascular microsurgical technique. Transplant. Proc. 2006, 38, 952–957. [Google Scholar] [CrossRef]
- Meraz, M.M.; Juárez, C.G.; Monsalve, C.R.; Martínez-Chequer, J.C.; Duvignau, J.M.; Fernández, E.M.; Montoya, S.; Betancour, E.T. Restoration of endocrine function and fertility with orthotopic tubal-ovarian allotransplant as the anatomical-functional unit in rabbits. J. Invest. Surg. 2008, 21, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Zhang, X.; Chen, W.; Xie, C.; Chen, W.; Cheng, P.; Zhou, Y.; Chen, B. Developmental Status: Impact of Short-Term Ischemia on Follicular Survival of Whole Ovarian Transplantation in a Rabbit Model. PLoS ONE 2015, 10, e0135049. [Google Scholar] [CrossRef] [PubMed]
- Goding, J.R.; McCracken, J.A.; Baird, D.T. Study of ovarian function in ewe by means of a vascular autotransplantation technique. J. Endocrinol. 1967, 39, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Goding, J.R.; Baird, D.T.; Cumming, I.A.; McCracken, J.A. Functional assessment of autotransplanted endocrine organs. Acta Endocrinol. Suppl. (Copenh.) 1972, 158, 169–199. [Google Scholar] [CrossRef]
- Souza, C.J.; Campbell, B.K.; Baird, D.T. Follicular dynamics and ovarian steroid secretion in sheep during the follicular and early luteal phases of the estrous cycle. Biol. Reprod. 1997, 56, 483–488. [Google Scholar] [CrossRef]
- Campbell, B.K.; Mann, G.E.; McNeilly, A.S.; Baird, D.T. The pattern of ovarian inhibin, estradiol, and androstenedione secretion during the estrous cycle of the ewe. Endocrinology 1990, 127, 227–235. [Google Scholar] [CrossRef]
- Campbell, B.K.; Dobson, H.; Baird, D.T.; Scaramuzzi, R.J. Examination of the relative role of FSH and LH in the mechanism of ovulatory follicle selection in sheep. J. Reprod. Fertil. 1999, 117, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.K.; Kendall, N.R.; Baird, D.T. The effect of the presence and pattern of luteinizing hormone stimulation on ovulatory follicle development in sheep. Biol. Reprod. 2007, 76, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Wranning, C.A.; Marcickiewicz, J.; Enskog, A.; Dahm-Kähler, P.; Hanafy, A.; Brännström, M. Fertility after autologous ovine uterine-tubal-ovarian transplantation by vascular anastomosis to the external iliac vessels. Hum. Reprod. 2010, 25, 1973–1979. [Google Scholar] [CrossRef] [PubMed]
- Harrison, F.A.; Heap, R.B. Ovarian activity in a pig after autotransplantation of an ovary. J. Physiol. 1972, 226, 39P. [Google Scholar] [PubMed]
- Harrison, F.A. Reproductive behaviour in the pig after autotransplantation of the ovary by vascular anastomoses. Q J. Exp Physiol. 1982, 67, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Paldi, E.; Gal, D.; Barzilai, A.; Hampel, N.; Malberger, E. Genital organs. Auto and homotransplantation in forty dogs. Int J. Fertil. 1975, 20, 5–12. [Google Scholar]
- Scott, J.R.; Keye, W.R.; Poulson, A.M.; Reynolds, W.A. Microsurgical ovarian transplantation in the primate. Fertil. Steril. 1981, 36, 512–515. [Google Scholar] [CrossRef]
- Johannesson, L.; Enskog, A.; Dahm-Kähler, P.; Hanafy, A.; Chai, D.C.; Mwenda, J.M.; Díaz-García, C.; Olausson, M.; Brännström, M. Uterus transplantation in a non-human primate: Long-term follow-up after autologous transplantation. Hum. Reprod. 2012, 27, 1640–1648. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chen, H.; Yin, H.; Kim, S.S.; Lin Tan, S.; Gosden, R.G. Fertility after intact ovary transplantation. Nature 2002, 415, 385. [Google Scholar] [CrossRef]
- Yin, H.; Wang, X.; Kim, S.S.; Chen, H.; Lin Tan, S.; Gosden, R.G. Transplantation of intact rat gonads using vascular anastomosis: Effects of cryopreservation, ischemia and genotype. Hum. Reprod. 2003, 18, 1165–1172. [Google Scholar] [CrossRef]
- Ding, Y.; Shao, J.L.; Li, J.W.; Zhang, Y.; Hong, K.H.; Hua, K.Q.; Wang, X. Successful fertility following optimized perfusion and cryopreservation of whole ovary and allotransplantation in a premature ovarian insufficiency rat model. J. Ovarian. Res. 2018, 11, 35. [Google Scholar] [CrossRef]
- Chen, C.H.; Chen, S.G.; Wu, G.J.; Wang, J.; Yu, C.P.; Liu, J.Y. Autologous heterotopic transplantation of intact rabbit ovary after frozen banking at −196 °C. Fertil. Steril. 2006, 86, 1059–1066. [Google Scholar] [CrossRef]
- Revel, A.; Elami, A.; Bor, A.; Yavin, S.; Natan, Y.; Arav, A. Whole sheep ovary cryopreservation and transplantation. Fertil. Steril. 2004, 82, 1714–1715. [Google Scholar] [CrossRef]
- Leporrier, M.; von Theobald, P.; Roffe, J.L.; Muller, G. A new technique to protect ovarian function before pelvic irradiation. Heterotopic ovarian autotransplantation. Cancer 1987, 60, 2201–2204. [Google Scholar] [CrossRef]
- Hilders, C.G.; Baranski, A.G.; Peters, L.; Ramkhelawan, A.; Trimbos, J.B. Successful human ovarian autotransplantation to the upper arm. Cancer 2004, 101, 2771–2778. [Google Scholar] [CrossRef] [PubMed]
- Mhatre, P.; Mhatre, J.; Magotra, R. Ovarian transplant: A new frontier. Transplant. Proc. 2005, 37, 1396–1398. [Google Scholar] [CrossRef] [PubMed]
- López-Monjardin, H.; de la Peña-Salcedo, J.A. Techniques for management of size discrepancies in microvascular anastomosis. Microsurgery 2000, 20, 162–166. [Google Scholar] [CrossRef]
- Turker, T.; Tsai, T.M.; Thirkannad, S. Size discrepancy in vessels during microvascular anastomosis: Two techniques to overcome this problem. Hand. Surg. 2012, 17, 413–417. [Google Scholar] [CrossRef]
- Mohammad, M.; Adjei, B.; George, S.; Alfeky, H.; Mostafa, A.; Dimovelis, I.; El-Gawad, A. Microsurgery and Vessel Caliber Mismatch: A Review of Microsurgery Anastomosis Techniques to Overcome Vessel Diameter Discrepancy. J. Orthoplastic Surg. 2020, 3, 87–95. [Google Scholar]
- Zeebregts, C.J.; Heijmen, R.H.; van den Dungen, J.J.; van Schilfgaarde, R. Non-suture methods of vascular anastomosis. Br. J. Surg. 2003, 90, 261–271. [Google Scholar] [CrossRef]
- Ilie, V.; Haddad, R.; Moisidis, E. Sutureless Microvascular Anastomosis: Literature Review. Int. Microsurg. J. 2019, 3, 1. [Google Scholar] [CrossRef]
- Guibert, E.E.; Petrenko, A.Y.; Balaban, C.L.; Somov, A.Y.; Rodriguez, J.V.; Fuller, B.J. Organ Preservation: Current Concepts and New Strategies for the Next Decade. Transfus. Med. Hemother. 2011, 38, 125–142. [Google Scholar] [CrossRef]
- Milenkovic, M.; Gharemani, M.; Bergh, A.; Wallin, A.; Mölne, J.; Fazlagic, E.; Eliassen, E.; Kahn, J.; Brännström, M. The human postmenopausal ovary as a tool for evaluation of cryopreservation protocols towards whole ovary cryopreservation. J. Assist. Reprod. Genet. 2011, 28, 453–460. [Google Scholar] [CrossRef]
- Dolmans, M.M.; Luyckx, V.; Donnez, J.; Andersen, C.Y.; Greve, T. Risk of transferring malignant cells with transplanted frozen-thawed ovarian tissue. Fertil. Steril. 2013, 99, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Rosendahl, M.; Greve, T.; Andersen, C.Y. The safety of transplanting cryopreserved ovarian tissue in cancer patients: A review of the literature. J. Assist. Reprod. Genet. 2013, 30, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Dolmans, M.M.; Masciangelo, R. Risk of transplanting malignant cells in cryopreserved ovarian tissue. Minerva Ginecol. 2018, 70, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Vanacker, J.; Luyckx, V.; Amorim, C.; Dolmans, M.M.; Van Langendonckt, A.; Donnez, J.; Camboni, A. Should we isolate human preantral follicles before or after cryopreservation of ovarian tissue? Fertil. Steril. 2013, 99, 1363–1368.e2. [Google Scholar] [CrossRef]
- Stahler, E.; Spatling, L.; Bethge, H.D.; Daume, E.; Buchholz, R. Induction of ovulation in human ovaries perfused in vitro. Arch. Gynakol. 1974, 217, 1–15. [Google Scholar] [CrossRef]
- Lambertsen, C.J., Jr.; Greenbaum, D.F.; Wright, K.H.; Wallach, E.E. In vitro studies of ovulation in the perfused rabbit ovary. Fertil. Steril. 1976, 27, 178–187. [Google Scholar] [CrossRef]
- Hamada, Y.; Bronson, R.A.; Wright, K.H.; Wallach, E.E. Ovulation in the perfused rabbit ovary: The influence of prostaglandins and prostaglandin inhibitors. Biol. Reprod. 1977, 17, 58–63. [Google Scholar] [CrossRef]
- Hamada, Y.; Wright, K.H.; Wallach, E.E. The effects of progesterone and human chorionic gonadotropin on ovulation in the in vitro perfused rabbit ovary. Fertil. Steril. 1979, 32, 335–339. [Google Scholar] [CrossRef]
- Wallach, E.E.; Wright, K.H.; Hamada, Y. Investigation of mammalian ovulation with an in vitro perfused rabbit ovary preparation. Am. J. Obstet. Gynecol. 1978, 132, 728–738. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Wright, K.H.; Santulli, R.; Wallach, E.E. Ovulation and ovum maturation in the rabbit ovary perfused in vitro. Biol. Reprod. 1981, 24, 483–490. [Google Scholar] [CrossRef]
- Koos, R.D.; Jaccarino, F.J.; Magaril, R.A.; Le Maire, W.J. Perfusion of the rat ovary in vitro: Methodology, induction of ovulation, and pattern of steroidogenesis. Biol. Reprod. 1984, 30, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Sogn, J.; Abrahamsson, G.; Janson, P.O. Release of cyclic AMP and progesterone from the isolated perfused luteal ovary of the PMSG treated rat. Acta Endocrinol. (Copenh.) 1984, 106, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Sogn, J.H.; Curry, T.E., Jr.; Brännström, M.; Lemaire, W.J.; Koos, R.D.; Papkoff, H.; Janson, P.O. Inhibition of follicle-stimulating hormone-induced ovulation by indomethacin in the perfused rat ovary. Biol. Reprod. 1987, 36, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M.; Johansson, B.M.; Sogn, J.; Janson, P.O. Characterization of an in vitro perfused rat ovary model: Ovulation rate, oocyte maturation, steroidogenesis and influence of PMSG priming. Acta Physiol. Scand. 1987, 130, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Brännström, M.; Flaherty, S. Methodology and characterization of an in vitro perfusion model for the mouse ovary. J. Reprod. Fertil. 1995, 105, 177–183. [Google Scholar] [CrossRef]
- Cobo, A.; García-Velasco, J.A.; Coello, A.; Domingo, J.; Pellicer, A.; Remohí, J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil. Steril. 2016, 105, 755–764.e8. [Google Scholar] [CrossRef]
- Werthessen, N.T.; Schwenk, E.; Baker, C. Biosynthesis of estrone and beta-estradiol in the perfused ovary. Science 1953, 117, 380–381. [Google Scholar] [CrossRef][Green Version]
- Zanotelli, M.R.; Henningsen, J.D.; Hopkins, P.M.; Dederich, A.P.; Herman, T.; Puccinelli, T.J.; Salih, S.M. An ovarian bioreactor for in vitro culture of the whole bovine ovary: A preliminary report. J. Ovarian. Res. 2016, 9, 47. [Google Scholar] [CrossRef]
| Species | Ovarian Volume (Mean ± SD) | Tissue Architecture Compared to the Human Ovary | Ovulation Pattern | Cycle Length (Days) |
|---|---|---|---|---|
| Human | 6.5 ± 2.9 cm3 (Munn et al. 1986) | Not applicable | Mono-ovulatory | 28–32 |
| Cow | 14.3 ± 5.7 cm3 (Gerritse et al. 2008) | Similar to human | Mono-, diovulatory | 21 |
| Pig | 7.3 ± 2.2 cm3 (Gerritse et al. 2008) | Less fibrous | Multi-ovulatory | 18–24 |
| Sheep | 1.0 ± 0.4 cm3 (Gerritse et al. 2008) | Similar to human | Mono-, triovulatory | 16–17 (seasonal) |
| Advantages | Disadvantages | |
|---|---|---|
| Slow freezing | Small amounts of cryoprotectant | Prone to intracellular ice formation Non-uniform cooling gradient between the core and periphery |
| Vitrification | No crystallization, amorphous state of liquids | Large amounts of cryoprotectant |
| Directional freezing | Controlled and uniform cooling gradient between the core and periphery | New technique, very few studies reported in the literature |
| Species | Reference | Freezing Procedure | Transplantation | Follow-Up | Outcomes of WOCT |
|---|---|---|---|---|---|
| Rodents | Rat: Wang et al. 2002b, Yin et al. 2003 | Slow freezing | Orthotopic, end-to-side (aorto-aortic and cava-caval) | ≥60 days |
|
| Rabbit: Chen et al. 2006 | Slow freezing | Heterotopic (groin pocket), end-to-end (ovarian vessels to inferior epigastric vessels) | 6 months |
| |
| Rat: Qi et al. 2008 | Slow freezing | Orthotopic, end-to-side (aorto-aortic and cava-caval) | ≥42 days |
| |
| Rat: Ding et al. 2018b | Slow freezing | Orthotopic, end-to-side (aorto-aortic and cava-caval) | 8 months |
| |
| Sheep | Bedaiwy et al. 2003 | Slow freezing | Heterotopic (rectus muscle), end-to-end (ovarian vessels to inferior epigastric vessels) | 8–10 days |
|
| Revel et al. 2004, Arav et al. 2005, 2010 | Directional freezing | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 6 years |
| |
| Imhof et al. 2006 | Slow freezing | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 18–19 months |
| |
| Bedaiwy and Falcone, 2007 | Slow freezing | Heterotopic (rectus muscle), ovarian vessels to inferior epigastric vessels | 8–10 days | Successful vascular patency after 8–10 days:
| |
| Grazul-Bilska et al. 2008 | Slow freezing | Heterotopic (rectus muscle), end-to-end (ovarian vessels to inferior epigastric vessels) | 5 months |
| |
| Courbière et al. 2009 | Vitrification | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 12 months |
| |
| Onions et al. 2009 | Slow freezing | Heterotopic (neck), end-to-side (aortic patch to carotid artery and ovarian vein to jugular vein) | 7 months |
| |
| Onions et al. 2013 | Slow freezing | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 7 days |
| |
| Campbell et al. 2014 | Slow freezing | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 3 months |
| |
| Slow freezing | Orthotopic, end-to-side (ovarian vessels to uterine vessels) | 11–23 months |
| ||
| Torre et al. 2016 | Slow freezing vs. Vitrification | Orthotopic, end-to-end (ovarian vessels to contralateral ovarian vessels) | 3 years |
|
| Reference | Number | Freezing Method | Investigated Outcomes |
|---|---|---|---|
| Martinez-Madrid et al. 2004, 2007 | 3 | Slow freezing | Follicular, stromal and vascular viability, histological morphology, apoptosis, ultrastructural assessment |
| Patrizio et al. 2007, 2008 | 11 | Directional freezing | Apoptosis, histological morphology |
| Milenkovic et al. 2011b | 10 (postmenopausal ovaries) | Slow freezing | Histological morphology, ultrastructural assessment, androgen production during in vitro perfusion |
| Westphal et al. 2017 | 3 | Slow freezing | Follicular and vascular viability, histological morphology, glucose uptake during tissue fragment culture |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hossay, C.; Donnez, J.; Dolmans, M.-M. Whole Ovary Cryopreservation and Transplantation: A Systematic Review of Challenges and Research Developments in Animal Experiments and Humans. J. Clin. Med. 2020, 9, 3196. https://doi.org/10.3390/jcm9103196
Hossay C, Donnez J, Dolmans M-M. Whole Ovary Cryopreservation and Transplantation: A Systematic Review of Challenges and Research Developments in Animal Experiments and Humans. Journal of Clinical Medicine. 2020; 9(10):3196. https://doi.org/10.3390/jcm9103196
Chicago/Turabian StyleHossay, Camille, Jacques Donnez, and Marie-Madeleine Dolmans. 2020. "Whole Ovary Cryopreservation and Transplantation: A Systematic Review of Challenges and Research Developments in Animal Experiments and Humans" Journal of Clinical Medicine 9, no. 10: 3196. https://doi.org/10.3390/jcm9103196
APA StyleHossay, C., Donnez, J., & Dolmans, M.-M. (2020). Whole Ovary Cryopreservation and Transplantation: A Systematic Review of Challenges and Research Developments in Animal Experiments and Humans. Journal of Clinical Medicine, 9(10), 3196. https://doi.org/10.3390/jcm9103196






