Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Setting
2.3. Patients
2.4. Ethics
2.5. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 3 May 2020).
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Pericàs, J.M.; Hernández-Meneses, M.; Sheahan, T.P.; Quintana, E.; Ambrosioni, J.; Sandoval, E.; Falces, C.; Marcos, M.A.; Tuset, M.; Vilella, A.; et al. COVID-19: From Epidemiology to Treatment. Eur Heart J. 2020, 41, 2092–2112. [Google Scholar] [CrossRef]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 Respiratory Distress. JAMA 2020, 323, 2329–2330. [Google Scholar] [CrossRef]
- Bikdeli, B.; Madhavan, M.V.; Jimenez, D.; Chuich, T.; Dreyfus, I.; Driggin, E.; Nigoghossian, C.D.; Ageno, W.; Madjid, M.; Guo, Y.; et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-up. J. Am. Coll. Cardiol. 2020, 75, 2950–2973. [Google Scholar] [CrossRef]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Peng, P.; Lei, C.; Li, S.; Chen, R.; Zhong, N. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef]
- Sanders, J.M.; Monogue, M.L.; Jodlowski, T.Z.; Cutrell, J.B. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 323, 1824–1836. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; The Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Dermatol. Venereol. 2020. [Google Scholar] [CrossRef]
- Diaz-Guimaraens, B.; Dominguez-Santas, M.; Suarez-Valle, A.; Pindado-Ortega, C.; Selda-Enriquez, G.; Bea-Ardebol, S.; Fernandez-Nieto, D. Petechial Skin Rash Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020, 156, 820–822. [Google Scholar] [CrossRef]
- Sanchez, A.; Sohier, P.; Benghanem, S.; L’Honneur, A.-S.; Rozenberg, F.; Dupin, N.; Garel, B. Digitate Papulosquamous Eruption Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020, 156, 819–820. [Google Scholar] [CrossRef]
- Piccolo, V.; Neri, I.; Filippeschi, C.; Oranges, T.; Argenziano, G.; Battarra, V.C.; Berti, S.; Manunza, F.; Belloni Fortina, A.; Di Lernia, V.; et al. Chilblain-like lesions during COVID-19 epidemic: A preliminary study on 63 patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e291–e293. [Google Scholar] [CrossRef]
- Fernandez-Nieto, D.; Jimenez-Cauhe, J.; Suarez-Valle, A.; Moreno-Arrones, O.M.; Saceda-Corralo, D.; Arana-Raja, A.; Ortega-Quijano, D. Characterization of acute acro-ischemic lesions in non-hospitalized patients: A case series of 132 patients during the COVID-19 outbreak. J. Am. Acad. Dermatol. 2020, 83, e61–e63. [Google Scholar] [CrossRef]
- Recalcati, S.; Barbagallo, T.; Frasin, L.A.; Prestinari, F.; Cogliardi, A.; Provero, M.C.; Dainese, E.; Vanzati, A.; Fantini, F. Acral cutaneous lesions in the Time of COVID-19. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e346–e347. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Galván Casas, C.; Català, A.; Carretero Hernández, G.; Rodríguez-Jiménez, P.; Fernández Nieto, D.; Rodríguez-Villa Lario, A.; Navarro Fernández, I.; Ruiz-Villaverde, R.; Falkenhain, D.; Llamas Velasco, M.; et al. Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 2020, 183, 71–77. [Google Scholar] [CrossRef]
- Marzano, A.V.; Genovese, G.; Fabbrocini, G.; Pigatto, P.; Monfrecola, G.; Piraccini, B.M.; Veraldi, S.; Rubegni, P.; Cusini, M.; Caputo, V.; et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: Multicenter case series of 22 patients. J. Am. Acad. Dermatol. 2020, 83, 280–285. [Google Scholar] [CrossRef]
- Zhang, Y.; Cao, W.; Xiao, M.; Li, Y.J.; Yang, Y.; Zhao, J.; Zhou, X.; Jiang, W.; Zhao, Y.Q.; Zhang, S.Y.; et al. [Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia]. Zhonghua Xueyexue Zazhi 2020, 41, E006. [Google Scholar]
- Zhang, Y.; Xiao, M.; Zhang, S.; Xia, P.; Cao, W.; Jiang, W.; Chen, H.; Ding, X.; Zhao, H.; Zhang, H.; et al. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N. Engl. J. Med. 2020, 382, e38. [Google Scholar] [CrossRef]
- Manalo, I.F.; Smith, M.K.; Cheeley, J.; Jacobs, R. A Dermatologic Manifestation of COVID-19: Transient Livedo Reticularis. J. Am. Acad. Dermatol. 2020, 83, 700. [Google Scholar] [CrossRef]
- Gibbs, M.B.; English, J.C.; Zirwas, M.J. Livedo reticularis: An update. J. Am. Acad. Dermatol. 2005, 52, 1009–1019. [Google Scholar] [CrossRef]
- Bosch-Amate, X.; Giavedoni, P.; Podlipnik, S.; Andreu-Febrer, C.; Sanz-Beltran, J.; Garcia-Herrera, A.; Alós, L.; Mascaró, J.M., Jr. Retiform purpura as a dermatological sign of COVID-19 coagulopathy. J. Eur. Acad. Dermatol. Venereol. 2020. [Google Scholar] [CrossRef]
- Cordoro, K.M.; Reynolds, S.D.; Wattier, R.; McCalmont, T.H. Clustered Cases of Acral Perniosis: Clinical Features, Histopathology and Relationship to COVID-19. Pediatr. Dermatol. 2020, 37, 419–423. [Google Scholar] [CrossRef]
- Wang, M.L.; Chan, M.P. Comparative Analysis of Chilblain Lupus Erythematosus and Idiopathic Perniosis: Histopathologic Features and Immunohistochemistry for CD123 and CD30. Am. J. Dermatopathol. 2018, 40, 265–271. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet Lond. Engl. 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Laurence, J.; Sanders, S.; Crowson, N.; Grossman, M.; Harp, J.; Nuovo, G. The differing pathophysiologies that underlie COVID-19 associated perniosis and thrombotic retiform purpura: A case series. Br. J. Dermatol. 2020. [Google Scholar] [CrossRef]
- Colmenero, I.; Santonja, C.; Alonso-Riaño, M.; Noguera-Morel, L.; Hernández-Martín, A.; Andina, D.; Wiesner, T.; Rodríguez-Peralto, J.L.; Requena, L.; Torrelo, A. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: Histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br. J. Dermatol. 2020. [Google Scholar] [CrossRef]
- Figueras-Nart, I.; Mascaró, J.M.; Solanich, X.; Hernández-Rodríguez, J. Dermatologic and Dermatopathologic Features of Monogenic Autoinflammatory Diseases. Front. Immunol. 2019, 10, 2448. [Google Scholar] [CrossRef]
- Trouillet-Assant, S.; Viel, S.; Gaymard, A.; Pons, S.; Richard, J.-C.; Perret, M.; Villard, M.; Brengel-Pesce, K.; Lina, B.; Mezidi, M.; et al. Type I IFN immunoprofiling in COVID-19 patients. J. Allergy Clin. Immunol. 2020, 146, 206–208. [Google Scholar] [CrossRef]
- Capusan, T.M.; Herrero-Moyano, M.; Fraga, J.; Llamas-Velasco, M. Clinico-Pathological Study of 4 Cases of Pseudoherpetic Grover Disease: The Same as Vesicular Grover Disease. Am. J. Dermatopathol. 2018, 40, 445–448. [Google Scholar] [CrossRef]
- Llamas-Velasco, M.; Chicharro, P.; Rodríguez-Jiménez, P.; Martos-Cabrera, L.; De Argila, D.; Fernández-Figueras, M.; Fraga, J. Reply to “Clinical and histological characterization of vesicular COVID-19 rashes: A prospective study in a tertiary care hospital”: Pseudoherpetic Grover disease seems to appear in patients with COVID-19 infection. Clin. Exp. Dermatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Figueras, M.-T.; Puig, L.; Cannata, P.; Cuatrecases, M.; Quer, A.; Ferrándiz, C.; Ariza, A. Grover disease: A reappraisal of histopathological diagnostic criteria in 120 cases. Am. J. Dermatopathol. 2010, 32, 541–549. [Google Scholar] [CrossRef]


| Patient characteristics | Chilblain-Like (n = 17) | Generalized Maculo-Papular Eruption (n = 12) | Grover´s Disease and Other Papulo-Vesicular Eruptions (n = 8) | Urticarial Eruption (n = 4) | Livedo Reticularis (n = 4) | Other * (n = 13) | Total (n = 58) |
|---|---|---|---|---|---|---|---|
| Female sex, n (%) | 7 (41%) | 6 (50%) | 4 (50%) | 3 (75%) | 1 (25%) | 6 (46%) | 27 (47%) |
| Median age, years (IQR) | 29 (24.8, 47.4) | 61 (51, 71.7) | 48 (37.6, 61.8) | 67 (51.3, 78.1) | 72 (64.7, 75.3) | 67 (59.4, 71.7) | 55 (38.7, 69.3) |
| Immunosuppression, n (%) | 1 (6%) | 1 (8%) | 0 | 0 | 0 | 2 (15%) | 4 (7%) |
| Hypertension, n (%) | 0 | 2 (17%) | 3 (37%) | 1 (25%) | 2 (50%) | 4 (31%) | 12(21%) |
| COVID-19 diagnosis, n (%) | |||||||
| Confirmed | 7 (41%) | 10 (83%) | 6 (75%) | 4 (100%) | 4 (100%) | 10 (77%) | 41 (71%) |
| rt-PCR positive | 3 (43%) | 9 (90%) | 4 (67%) | 3 (75%) | 3 (75%) | 7 (64%) | 29 (71%) |
| Serology positive | 4 (57%) | 2 (20%) | 2 (100%) | 1 (25%) | 1 (25%) | 3 (100%) | 13 (32%) |
| Highly suspected | 10 (59%) | 2 (17%) | 2 (25%) | 0 | 0 | 3 (23%) | 17 (29%) |
| COVID-19 symptoms other than cutaneous, n (%) | 9 (53%) | 12 (100%) | 8 (100%) | 4 (100%) | 4 (100%) | 13 (100%) | 50 (86%) |
| Chest X-ray performed, n (%) | 5 | 11 | 8 | 4 | 4 | 13 | 44 |
| Normal | 3 (60%) | 1 (9%) | 1 (12%) | 1 (25%) | 0 | 1 (8%) | 7 (16%) |
| Unilateral interstitial infiltrates | 0 | 0 | 0 | 0 | 0 | 2 (16.7%) | 2 (4.5%) |
| Bilateral interstitial infiltrates | 2 (40%) | 10 (91%) | 6 (75%) | 3 (75%) | 4 (100%) | 8 (67%) | 33 (75%) |
| Other | 0 | 0 | 1 (12%) | 0 | 0 | 1 (8%) | 2 (4%) |
| Blood test with altered values suggesting COVID-19, n (%) | 3 (19%) | 11 (100%) | 7 (87%) | 2 (100%) | 3 (100%) | 13 (100%) | 39 (74%) |
| Skin biopsy performed, n (%) | 12 (71%) | 11 (92%) | 6 (75%) | 4 (100%) | 4 (100%) | 5 (38%) | 42 (72%) |
| DIF performed, n (%) | 11 (65%) | 3 (25%) | 4 (50%) | 3 (75%) | 4 (100%) | 5 (38%) | 30 (52%) |
| “Antiviral” treatment, n (%) | 1 (6%) | 10 (83%) | 6 (75%) | 4 (100%) | 4 (100%) | 11 (85%) | 36 (62%) |
| Anti-inflammatory treatment, n (%) | 1 (6%) | 10 (83%) | 6 (75%) | 4 (100%) | 4 (100%) | 11 (85%) | 36 (62%) |
| Hospitalization required | 2 (11.8%) | 10 (83.3%) | 6 (75%) | 4 (100%) | 4 (100%) | 12 (92.3%) | 38 (65.5%) |
| ICU required | 1 (6%) | 4 (33%) | 3 (37%) | 3 (75%) | 2 (50%) | 6 (46%) | 19 (33%) |
| In-hospital mortality | 0 | 0 | 6 (75%) | 0 | 0 | 2 (5%) | 2 (3%) |
| Patient characteristics | Chilblain-Like (n = 17) | Others (n = 41) | p Value |
|---|---|---|---|
| Female sex, n (%) | 7 (41%) | 20 (49%) | 0.773 |
| Median age, years (IQR) | 29 (24, 47) | 63 (50, 74) | <0.001 |
| Immunosuppression, n (%) | 1 (6%) | 3 (7%) | 1.000 |
| Hypertension, n (%) | 0 | 12 (29%) | 0.012 |
| ACE-i and ARBs use | 0 | 6 (15%) | 0.166 |
| COVID-19 diagnosis, n (%) | 0.003 | ||
| Confirmed | 7 (41.2%) | 34 (82.9%) | |
| Highly suspected | 10 (58.8%) | 7 (17.1%) | |
| COVID-19 symptoms other than cutaneous, n (%) | |||
| Fever | 4 (23%) | 35 (85%) | <0.001 |
| Cough | 6 (35%) | 26 (63%) | 0.050 |
| Dyspnea | 1 (6%) | 23 (56%) | <0.001 |
| Asthenia | 1 (6%) | 15 (37%) | 0.023 |
| Myalgias | 1 (6%) | 14 (34%) | 0.045 |
| Diarrhea | 1 (6%) | 12 (29%) | 0.082 |
| Ageusia | 2 (12%) | 8 (19%) | 0.707 |
| Anosmia | 2 (12%) | 5 (12%) | 1.000 |
| Headache | 0 | 4 (10%) | 0.310 |
| Vomit | 0 | 3 (7%) | 0.548 |
| Chest X-ray performed, n (%) | 5 (29%) | 39 (95%) | <0.0010.060 |
| Normal | 3 (60%) | 4 (10%) | |
| Unilateral interstitial infiltrates | 0 | 2 (5%) | |
| Bilateral interstitial infiltrates | 2 (40%) | 31 (79%) | |
| Other | 0 | 2 (5%) | |
| COVID-19 related parameters | |||
| C-Reactive protein, median mg/dL (IQR) | 0.4 (0.4, 0.4) | 5.9 (3.0, 14.9) | 0.011 |
| Lymphocytes, median cells ^106/L (IQR) | 1800 (1200, 2000) | 800 (600, 1200) | <0.001 |
| Ferritin, median ng/mL (IQR) | 87.5 (40, 197.2) | 615 (232.5, 905.2) | 0.013 |
| LDH, median U/L (IQR) | 177 (164.2, 190.8) | 299 (243.0, 415.0) | 0.120 |
| D-dimer, median ng/mL (IQR) | 200 (200, 300) | 800 (500, 2000) | 0.297 |
| ESR, median mm/h (IQR) | 5 (4, 7) | 38.0 (29, 61.8) | <0.001 |
| Autoimmunity test performed, n (%) | |||
| Anti-nuclear antibodies | 15 (88.2) | 22 (53.6) | |
| Positive | 3 (20%) | 1 (4%) | 0.283 |
| Anti-Ro antibodies | 12 (70%) | 20 (49%) | |
| Positive | 0 | 0 | NC |
| Antibeta-2-glycoprotein antibodies, IgM | 15 (88.23) | 24 (58.53) | |
| Positive | 0 | 0 | NC |
| Antibeta-2-glycoprotein antibodies, IgG | 15 (88.2) | 24 (58.5) | |
| Positive | 1 (7%) | 2 (8%) | 1.000 |
| Anticardiolipin antibodies, IgM | 15 (88.2) | 24 (58.5) | |
| Positive | 0 | 0 | NC |
| Anticardiolipin antibodies, IgG | 15 (88.2) | 24 (58.5) | |
| Positive | 2 (13%) | 2 (8%) | 0.631 |
| Skin biopsy performed, n (%) | 12 (77%) | 30 (73%) | 1.000 |
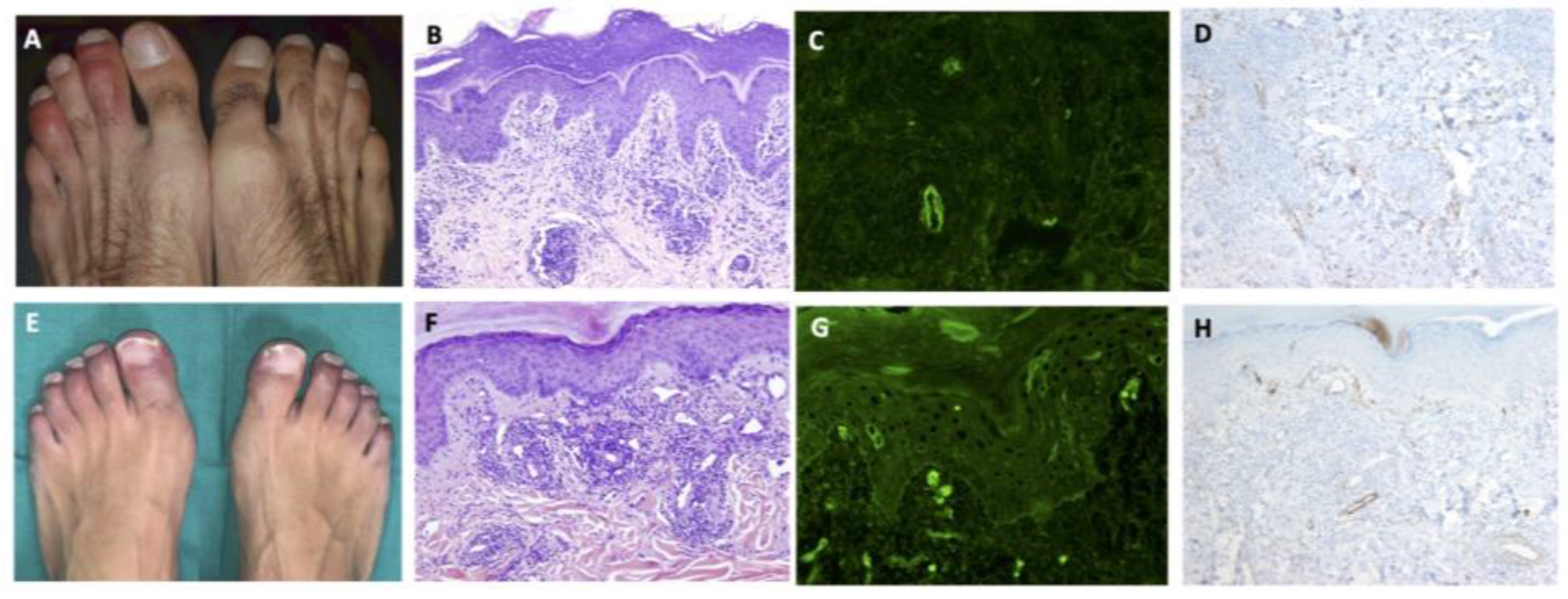
| Histological pattern according to HE stains | 0.003 | ||
| Chilblain-like pattern | 10 (83%) | 0 | |
| Spongiotic dermatitis | 0 | 8 (27%) | |
| Interface + spongiotic dermatitis | 0 | 6 (20%) | |
| Grover´s disease pattern | 0 | 3 (10%) | |
| Urticariform | 0 | 2 (7%) | |
| Interface dermatitis | 0 | 2 (7%) | |
| Pityrosporum folliculitis | 0 | 2 (7%) | |
| Subcorneal pustulosis | 0 | 2 (%) | |
| Psoriasiform | 1 (8%) | 0 | |
| Thrombotic microangiopathy | 1 (8%) | 1 (3%) | |
| Other | 0 | 4 (13%) | |
| Mucin deposits | 9 (75%) | 1 (3%) | <0.001 |
| Epidermal atrophy | 3 (25%) | 2 (7%) | 0.131 |
| DIF performed, n (%) | 11 (65%) | 19 (46%) | 0.024 |
| Lichenoid | 0 | 2 (10.5%) | |
| Lichenoid + vasculopathic | 3 (27%) | 0 | |
| Negative | 4 (36%) | 14 (74%) | |
| Vasculopathic | 4 (36%) | 3 (15.8%) | <0.001 |
| IHQ Anti-C9 deposits in dermal vessels performed, n (%) | 11 (64.7) | 22 (53.5) | |
| Positive | 10 (91%) | 5 (23%) | <0.001 |
| Treatment | |||
| Hydroxychloroquine | 1 (6%) | 35 (85%) | <0.001 |
| Azithromycin | 0 | 34 (83%) | <0.001 |
| Lopinavir/ritonavir | 1 (6%) | 29 (71%) | <0.001 |
| Systemic corticosteroids | 1 (6%) | 24 (58%) | <0.001 |
| Tocilizumab | 1 (6%) | 14 (34%) | 0.045 |
| Remdesivir | 0 | 5 (12%) | 0.308 |
| Anakinra | 0 | 5 (12%) | 0.308 |
| Siltuximab | 0 | 2 (5%) | 1.000 |
| Hospitalization required | 2 (12%) | 36 (88%) | <0.001 |
| ICU required | 1 (6%) | 18 (44%) | 0.005 |
| Mortality | 0 | 2 (5%) | 1.000 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giavedoni, P.; Podlipnik, S.; Pericàs, J.M.; Fuertes de Vega, I.; García-Herrera, A.; Alós, L.; Carrera, C.; Andreu-Febrer, C.; Sanz-Beltran, J.; Riquelme-Mc Loughlin, C.; et al. Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity. J. Clin. Med. 2020, 9, 3261. https://doi.org/10.3390/jcm9103261
Giavedoni P, Podlipnik S, Pericàs JM, Fuertes de Vega I, García-Herrera A, Alós L, Carrera C, Andreu-Febrer C, Sanz-Beltran J, Riquelme-Mc Loughlin C, et al. Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity. Journal of Clinical Medicine. 2020; 9(10):3261. https://doi.org/10.3390/jcm9103261
Chicago/Turabian StyleGiavedoni, Priscila, Sebastián Podlipnik, Juan M. Pericàs, Irene Fuertes de Vega, Adriana García-Herrera, Llúcia Alós, Cristina Carrera, Cristina Andreu-Febrer, Judit Sanz-Beltran, Constanza Riquelme-Mc Loughlin, and et al. 2020. "Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity" Journal of Clinical Medicine 9, no. 10: 3261. https://doi.org/10.3390/jcm9103261
APA StyleGiavedoni, P., Podlipnik, S., Pericàs, J. M., Fuertes de Vega, I., García-Herrera, A., Alós, L., Carrera, C., Andreu-Febrer, C., Sanz-Beltran, J., Riquelme-Mc Loughlin, C., Riera-Monroig, J., Combalia, A., Bosch-Amate, X., Morgado-Carrasco, D., Pigem, R., Toll-Abelló, A., Martí-Martí, I., Rizo-Potau, D., Serra-García, L., ... Mascaró, J. M., Jr. (2020). Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity. Journal of Clinical Medicine, 9(10), 3261. https://doi.org/10.3390/jcm9103261









