Pre-Hospital Lactatemia Predicts 30-Day Mortality in Patients with Septic Shock—Preliminary Results from the LAPHSUS Study
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Ethical Considerations
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Main Measurement
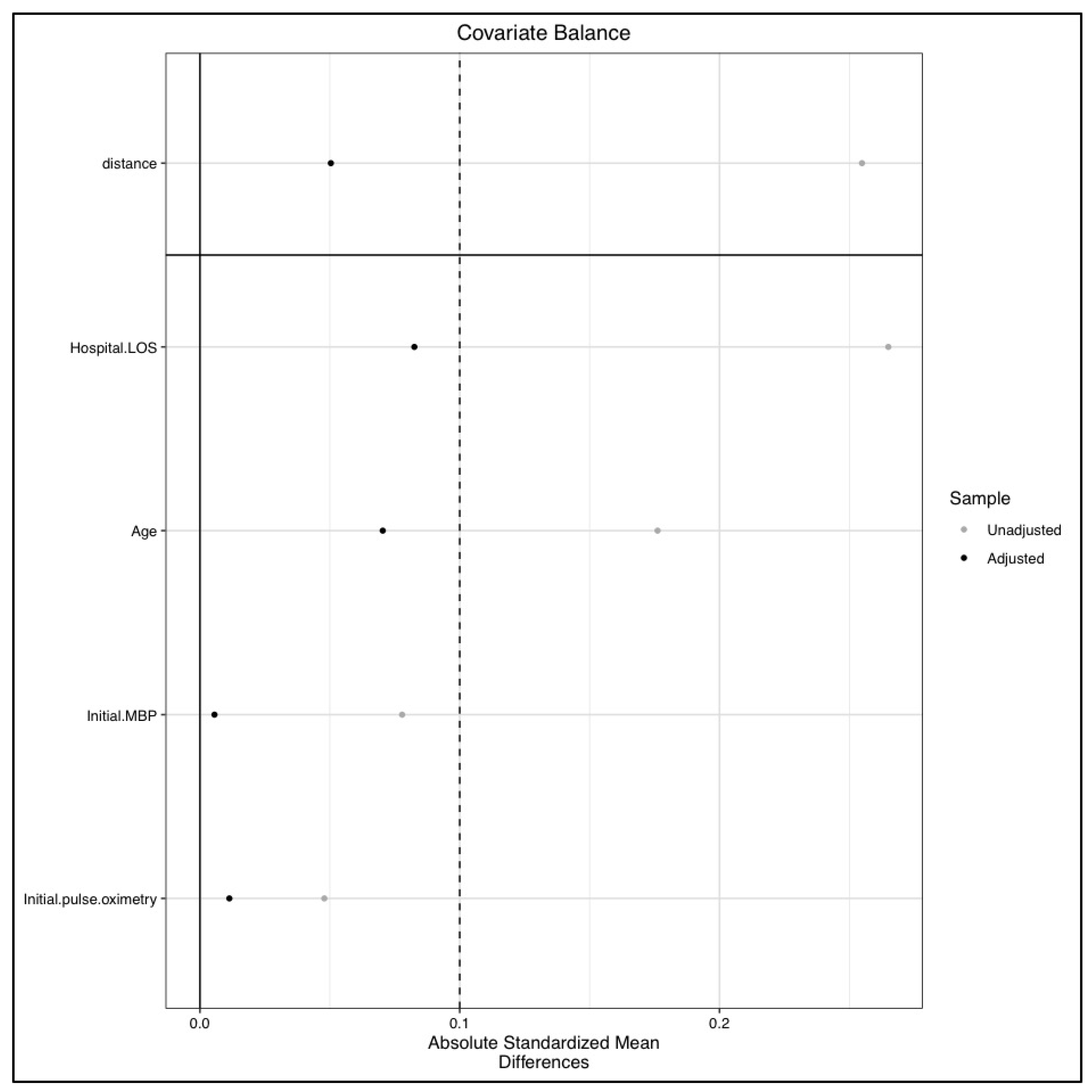
3.3. Propensity Score Matching Analysis
3.4. Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.J.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Gaieski, D.; Edwards, J.M.; Kallan, M.J.; Carr, B.G. Benchmarking the Incidence and Mortality of Severe Sepsis in the United States. Crit. Care Med. 2013, 41, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [Green Version]
- Liu, V.; Escobar, G.J.; Greene, J.D.; Soule, J.; Whippy, A.; Angus, D.C.; Iwashyna, T.J. Hospital Deaths in Patients With Sepsis From 2 Independent Cohorts. JAMA 2014, 312, 90–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busani, S.; Damiani, E.; Cavazzuti, I.; Donati, A.; Girardis, M. Intravenous immunoglobulin in septic shock: Review of the mechanisms of action and meta-analysis of the clinical effectiveness. Minerva Anestesiol. 2016, 82, 559–572. [Google Scholar]
- Luhr, R.; Cao, Y.; Söderquist, B.; Cajander, S. Trends in sepsis mortality over time in randomised sepsis trials: A systematic literature review and meta-analysis of mortality in the control arm, 2002–2016. Crit. Care 2019, 23, 241. [Google Scholar] [CrossRef] [Green Version]
- Sakr, Y.; Elia, C.; Mascia, L.; Barberis, B.; Cardellino, S.; Livigni, S.; Fiore, G.; Filippini, C.; Ranieri, V.M. Epidemiology and outcome of sepsis syndromes in Italian ICUs: A muticentre, observational cohort study in the region of Piedmont. Minerva Anestesiol. 2013, 79, 993–1002. [Google Scholar]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Brun-Buisson, C.; Meshaka, P.; Pinton, P.; Vallet, B.; EPISEPSIS Study Group. EPISEPSIS: A reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004, 30, 580–588. [Google Scholar] [CrossRef] [Green Version]
- Pottecher, T.; Calvat, S.; Dupont, H.; Durand-Gasselin, J.; Gerbeaux, P. Haemodynamic management of severe sepsis: Recommendations of the French Intensive Care Societies (SFAR/SRLF) Consensus Conference, 13 October 2005, Paris, France. Crit. Care 2006, 10, 311. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.M.; Evans, L.E.; Rhodes, A. The Surviving Sepsis Campaign Bundle: 2018 update. Intensive Care Med. 2018, 46, 925–928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- April, M.D.; Donaldson, C.; Tannenbaum, L.I.; Moore, T.; Aguirre, J.; Pingree, A.; Lantry, J.H. Emergency department septic shock patient mortality with refractory hypotension vs hyperlactatemia: A retrospective cohort study. Am. J. Emerg. Med. 2017, 35, 1474–1479. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Jaeschke, R.; Levy, M.M.; Rhodes, A.; Annane, D.; Gerlach, H.; Opal, S.M.; Sevransky, J.E.; Sprung, C.L.; Douglas, I.S.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock, 2012. Intensive Care Med. 2013, 39, 165–228. [Google Scholar] [CrossRef]
- Cicarelli, D.D.; Vieira, J.E.; Bensenor, F.E. Lactate as a predictor of mortality and multiple organ failure in patients with the systemic inflammatory response syndrome. Rev. Bras. Anestesiol. 2007, 57, 630–638. [Google Scholar] [PubMed] [Green Version]
- Gaieski, D.F.; Goyal, M. Serum lactate as a predictor of mortality in emergency department patients with infection: Does the lactate level tell the whole story? Ann. Emerg. Med. 2005, 46, 561–562. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, M.E.; Miltiades, A.N.; Gaieski, D.F.; Goyal, M.; Fuchs, B.D.; Shah, C.V.; Bellamy, S.L.; Christie, J.D. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit. Care Med. 2009, 37, 1670–1677. [Google Scholar] [CrossRef]
- Shankar-Hari, M.; Phillips, G.S.; Levy, M.L.; Seymour, C.W.; Liu, V.X.; Deutschman, C.S.; Angus, D.C.; Rubenfeld, G.D.; Singer, M.; Force, S.D.T. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 775–787. [Google Scholar] [CrossRef]
- Léguillier, T.; Jouffroy, R.; Boisson, M.; Boussaroque, A.; Chenevier-Gobeaux, C.; Chaabouni, T.; Vivien, B.; Nivet-Antoine, V.; Beaudeux, J.-L. Lactate POCT in mobile intensive care units for septic patients? A comparison of capillary blood method versus venous blood and plasma-based reference methods. Clin. Biochem. 2018, 55, 9–14. [Google Scholar] [CrossRef]
- Jouffroy, R.; Saade, A.; Muret, A.; Philippe, P.; Michaloux, M.; Carli, P.; Vivien, B. Fluid resuscitation in pre-hospital management of septic shock. Am. J. Emerg. Med. 2018, 36, 1754–1758. [Google Scholar] [CrossRef]
- Adnet, F.; Lapostolle, F. International EMS Systems: France. Resuscitation 2004, 63, 7–9. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef] [PubMed]
- Jouffroy, R.; Tourtier, J.P.; Debaty, G.; Bounes, V.; Gueye-Ngalgou, P.; Vivien, B. Contribution of the Pre-Hospital Blood Lactate Level in the Pre-Hospital Orientation of Septic Shock: The LAPHSUS Study. Turk. J. Anaesthesiol. Reanim. 2020, 48, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Bakker, J.; Coffernils, M.; Leon, M.; Gris, P.; Vincent, J.-L. Blood Lactate Levels Are Superior to Oxygen-Derived Variables in Predicting Outcome in Human Septic Shock. Chest 1991, 99, 956–962. [Google Scholar] [CrossRef] [PubMed]
- Gernardin, G.; Pradier, C.; Tiger, F.; Deloffre, P.; Mattei, M. Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensive Care Med. 1996, 22, 17–25. [Google Scholar] [CrossRef]
- Casserly, B.; Phillips, G.; Schorr, C.A.; Dellinger, R.P.; Townsend, S.R.; Osborn, T.M.; Reinhart, K.; Selvakumar, N.; Levy, M.M. Lactate measurements in sepsis-induced tissue hypoperfusion: Results from the Surviving Sepsis Campaign database. Crit. Care Med. 2015, 43, 567–573. [Google Scholar] [CrossRef]
- Cecconi, M.; De Backer, D.; Antonelli, M.; Beale, R.; Bakker, J.; Hofer, C.; Jaeschke, R.; Mebazaa, A.; Pinsky, M.R.; Teboul, J.-L.; et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014, 40, 1795–1815. [Google Scholar] [CrossRef]
- Dugas, M.-A.; Proulx, F.; De Jaeger, A.; Lacroix, J.; Lambert, M. Markers of tissue hypoperfusion in pediatric septic shock. Intensive Care Med. 2000, 26, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Bellomo, R.; Marik, P.; Kellum, J.A.; Salon, J.E.; Igah, I.; Ihediwa, U.; Uzoigwe, C.E.; Windpessl, M.; Wallner, M.; Kraut, J.A.; et al. Lactic Acidosis. N. Engl. J. Med. 2015, 372, 1076–1079. [Google Scholar] [CrossRef]
- Lokhandwala, S.; Moskowitz, A.; Lawniczak, R.; Giberson, T.; Cocchi, M.N.; Donnino, M.W. Disease heterogeneity and risk stratification in sepsis-related occult hypoperfusion: A retrospective cohort study. J. Crit. Care 2015, 30, 531–536. [Google Scholar] [CrossRef] [Green Version]
- Marecaux, G.; Pinsky, M.R.; Dupont, E.; Kahn, R.J.; Vincent, J.L. Blood lactate levels are better prognostic indicators than TNF and IL-6 levels in patients with septic shock. Intensive Care Med. 1996, 22, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, N.I.; Howell, M.D.; Talmor, D.; Nathanson, L.A.; Lisbon, A.; Wolfe, R.E.; Weiss, J.W. Serum Lactate as a Predictor of Mortality in Emergency Department Patients with Infection. Ann. Emerg. Med. 2005, 45, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Stacpoole, P.W.; Wright, E.C.; Baumgartner, T.G.; Bersin, R.M.; Buchalter, S.; Curry, S.H.; Duncan, C.; Harman, E.M.; Henderson, G.N.; Jenkinson, S.; et al. Natural history and course of acquired lactic acidosis in adults. Am. J. Med. 1994, 97, 47–54. [Google Scholar] [CrossRef]
- Swenson, K.E.; Dziura, J.D.; Aydin, A.; Reynolds, J.; Wira, C.R. Evaluation of a novel 5-group classification system of sepsis by vasopressor use and initial serum lactate in the emergency department. Intern. Emerg. Med. 2017, 13, 257–268. [Google Scholar] [CrossRef]
- Nouland, D.P.A.V.D.; Brouwers, M.C.G.J.; Stassen, P.M. Prognostic value of plasma lactate levels in a retrospective cohort presenting at a university hospital emergency department. BMJ Open 2017, 7, e011450. [Google Scholar] [CrossRef] [Green Version]
- Yaghoubian, A. Use of Admission Serum Lactate and Sodium Levels to Predict Mortality in Necrotizing Soft-Tissue Infections. Arch. Surg. 2007, 142, 840. [Google Scholar] [CrossRef] [Green Version]
- Vink, E.E.; Bakker, J. Practical Use of Lactate Levels in the Intensive Care. J. Intensive Care Med. 2017, 33, 159–165. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [Green Version]
- Ait-Oufella, H.; Bige, N.; Boëlle, P.Y.; Pichereau, C.; Alves, M.; Bertinchamp, R.; Baudel, J.L.; Galbois, A.; Maury, E.; Guidet, B. Capillary refill time exploration during septic shock. Intensive Care Med. 2014, 40, 958–964. [Google Scholar] [CrossRef]
- Ait-Oufella, H.; Lemoinne, S.; Boelle, P.Y.; Galbois, A.; Baudel, J.L.; Lemant, J.; Joffre, J.; Margetis, D.; Guidet, B.; Maury, E.; et al. Mottling score predicts survival in septic shock. Intensive Care Med. 2011, 37, 801–807. [Google Scholar] [CrossRef]
- Jouffroy, R.; Saade, A.; Tourtier, J.P.; Gueye, P.; Bloch-Laine, E.; Ecollan, P.; Carli, P.; Vivien, B. Skin mottling score and capillary refill time to assess mortality of septic shock since pre-hospital setting. Am. J. Emerg. Med. 2019, 37, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Askim, Å.; Moser, F.; Gustad, L.T.; Stene, H.; Gundersen, M.; Åsvold, B.O.; Dale, J.; Bjørnsen, L.P.; Damås, J.K.; Solligård, E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality —A prospective study of patients admitted with infection to the emergency department. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 56. [Google Scholar] [CrossRef]
- Dorsett, M.; Kroll, M.; Smith, C.S.; Asaro, P.; Liang, S.Y.; Moy, H.P. qSOFA Has Poor Sensitivity for Prehospital Identification of Severe Sepsis and Septic Shock. Prehosp. Emerg. Care 2017, 21, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Takahashi, T.; Haga, Y.; Nishikawa, T. Comparative study on quick sequential organ failure assessment, systemic inflammatory response syndrome and the shock index in prehospital emergency patients: Single-site retrospective study. Acute Med. Surg. 2019, 6, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Koyama, S.; Yamaguchi, Y.; Gibo, K.; Nakayama, I.; Ueda, S. Use of prehospital qSOFA in predicting in-hospital mortality in patients with suspected infection: A retrospective cohort study. PLoS ONE 2019, 14, e0216560. [Google Scholar] [CrossRef] [Green Version]
- Lane, D.J.; Lin, S.; Scales, D.C. Classification versus Prediction of Mortality Risk using the SIRS and qSOFA Scores in Patients with Infection Transported by Paramedics. Prehosp. Emerg. Care 2019, 24, 282–289. [Google Scholar] [CrossRef]
- Silcock, D.J.; Corfield, A.R.; Staines, H.; Rooney, K.D. Superior performance of National Early Warning Score compared with quick Sepsis-related Organ Failure Assessment Score in predicting adverse outcomes: A retrospective observational study of patients in the prehospital setting. Eur. J. Emerg. Med. 2019, 26, 433–439. [Google Scholar] [CrossRef] [Green Version]
- Ayar, P.V.; DeLay, M.; Avondo, A.; Duchateau, F.-X.; Nadiras, P.; Lapostolle, F.; Chouihed, T.; Freund, Y. Prognostic value of prehospital quick sequential organ failure assessment score among patients with suspected infection. Eur. J. Emerg. Med. 2019, 26, 329–333. [Google Scholar] [CrossRef]


| Overall Population (n = 177) | Living (n = 118) | Deceased (n = 59) | p Value | |
|---|---|---|---|---|
| Age (years) | 70 ± 14 | 68 ± 14 | 74 ± 13 | 0.009 * |
| Weight (kg) | 70 ± 15 | 71 ± 15 | 69 ± 14 | 0.346 |
| Size (cm) | 171 ± 8 | 171 ± 8 | 170 ± 9 | 0.827 |
| SBP (mmHg) | 101 ± 55 | 103 ± 65 | 97 ± 26 | 0.483 |
| DBP (mmHg) | 58 ± 22 | 60 ± 23 | 56 ± 20 | 0.345 |
| MBP (mmHg) | 71 ± 23 | 72 ± 24 | 69 ± 20 | 0.486 |
| HR (beats.min−1) | 116 ± 29 | 117 ± 29 | 113 ± 31 | 0.386 |
| RR (movements.min−1) | 30 (24–40) | 30 (22–40) | 32 (25–38) | 0.676 |
| Pulse oximetry (%) | 92 (84–96) | 91 (85–96) | 92 (83–95) | 0.568 |
| Body core temperature (°C) | 38.3 (36.0–39.2) | 38.4 (36.7–39.4) | 38.2 (35.6–39.0) | 0.521 |
| Glycemia (mmol/L) | 8.8 (6.3–12.1) | 9.1 (6.9–12.3) | 7.3 (5.4–9.7) | 0.031 * |
| Glasgow coma scale | 14 (12–15) | 14 (12–15) | 14 (11–15) | 0.560 |
| Blood lactate level (mmol/L) | 6.3 ± 3.7 | 5.9 ± 3.5 | 7.1 ± 4.0 | <0.001 * |
| Pre-hospital fluid expansion (mL) | 1039 ± 587 | 1067 ± 592 | 980 ± 575 | 0.360 |
| Norepinephrine administration | 64 (36%) | 44 (37%) | 20 (34%) | 0.838 |
| Norepinephrine dose | 1.0 (0.5–2.0) | 1.0 (0.5–2.0) | 1.0 (0.7–2.0) | 0.670 |
| Pre-hospital duration (min) | 83 ± 29 | 83 ± 29 | 83 ± 29 | 0.970 |
| In-ICU length of stay (days) | 6 (3–10) | 7 (4–10) | 6 (2–10) | 0.146 |
| In-hospital length of stay (days) | 14 (8–22) | 17 (10–29) | 7 (2–13) | <0.001 * |
| SOFA score | 8 (4–11) | 6 (3–10) | 10 (8–12) | <0.001 * |
| SAPS2 score | 58 ± 22 | 53 ± 19 | 70 ± 25 | <0.001 * |
| Male gender | 124 (70%) | 85 (72%) | 39 (66%) | 0.743 |
| High blood pressure | 78 (44%) | 52 (44%) | 26 (44%) | 0.775 |
| Coronaropathy | 25 (22%) | 15 (13%) | 10 (17%) | 0.981 |
| Chronic cardiac failure | 21 (12%) | 11 (9%) | 10 (17%) | 0.113 |
| Diabetes mellitus | 46 (26%) | 36 (31%) | 10 (17%) | 0.081 |
| HIV infection | 6 (3%) | 4 (3%) | 2 (3%) | 0.952 |
| Cancer history | 53 (30%) | 36 (31%) | 17 (29%) | 0.981 |
| COPD | 17 (10%) | 11 (9%) | 6 (10%) | 0.774 |
| Chronic renal failure | 19 (11%) | 11 (9%) | 8 (14%) | 0.332 |
| Pre-hospital AB administration | 54 (31%) | 37 (31%) | 17 (29%) | 0.890 |
| Origin | n (percentage) |
|---|---|
| Pulmonary | 102 (58%) |
| Digestive | 38 (21%) |
| Urinary | 19 (11%) |
| Cutaneous | 5 (3%) |
| Meningeal | 3 (2%) |
| Unknown | 10 (6%) |
| Overall Population (n = 177) | Pre-hospital Lactatemia ≥ 4 mmol/L (n = 57) | Pre-hospital Lactatemia < 4 mmol/L (n = 120) | p Value | |
|---|---|---|---|---|
| Age (years) | 70 ± 14 | 69 ± 15 | 71 ± 12 | 0.483 |
| Weight (kg) | 70 ± 15 | 72 ± 14 | 69 ± 16 | 0.300 |
| Size (cm) | 171 ± 8 | 171 ± 8 | 170 ± 10 | 0.663 |
| SBP (mmHg) | 101 ± 55 | 99 ± 29 | 91 ± 31 | 0.367 |
| DBP (mmHg) | 58 ± 22 | 59 ± 21 | 57 ± 22 | 0.612 |
| MBP (mmHg) | 71 ± 23 | 70 ± 22 | 69 ± 24 | 0.793 |
| HR (beats.min−1) | 116 ± 29 | 118 ± 29 | 109 ± 29 | 0.069 |
| RR (movements.min−1) | 30 (24–40) | 32 (25–40) | 28 (20–36) | 0.038 * |
| Pulse oximetry (%) | 92 (84–96) | 92 (83–97) | 90 (85–95) | 0.824 |
| Body core temperature (°C) | 38.3 (36.0–39.2) | 38.0 (35.6–39.1) | 38.6 (38.0–39.2) | 0.022 * |
| Glycemia (mmol/L) | 8.8 (6.3–12.1) | 9.0 (6.4–12.3) | 7.5 (6.0–10.2) | 0.281 |
| Glasgow coma scale | 14 (12–15) | 14 (12–15) | 15 (12–15) | 0.594 |
| Blood lactate level (mmol/L) | 6.3 ± 3.7 | 2.3 ± 1.0 | 7.7 ± 3.2 | <0.001 * |
| Pre-hospital fluid expansion (mL) | 1039 ± 587 | 1038 ± 599 | 979 ± 547 | 0.551 |
| Norepinephrine administration | 64 (36%) | 18 (32%) | 46 (38%) | 0.921 |
| Norepinephrine dose | 1.0 (0.5–2.0) | 1.0 (0.5–2.0) | 1.0 (0.9–1.1) | 0.185 |
| Pre-hospital duration (min) | 83 ± 29 | 81 ± 30 | 85 ± 28 | 0.486 |
| In-ICU length of stay (days) | 6 (3–10) | 7 (4–11) | 5 (3–8) | 0.083 |
| In-hospital length of stay (days) | 14 (8–22) | 14 (7–23) | 15 (8–20) | 0.351 |
| SOFA score | 8 (4–11) | 8 (5–11) | 3 (5–8) | 0.026 * |
| SAPS2 score | 58 ± 22 | 63 ± 22 | 49 ± 21 | <0.001 * |
| Male gender | 124 (70%) | 31 (54%) | 93 (78%) | 0.401 |
| High blood pressure | 78 (44%) | 17 (30%) | 61 (51%) | 0.494 |
| Coronaropathy | 25 (22%) | 3 (5%) | 22 (18%) | 0.093 |
| Chronic cardiac failure | 21 (12%) | 9 (16%) | 12 (10%) | 0.272 |
| Diabetes mellitus | 46 (26%) | 11 (19%) | 35 (30%) | 0.675 |
| HIV infection | 6 (3%) | 1 (2%) | 5 (3%) | 0.473 |
| Cancer history | 53 (30%) | 15 (26%) | 38 (32%) | 0.143 |
| COPD | 17 (10%) | 4 (7%) | 13 (11%) | 0.788 |
| Chronic renal failure | 19 (11%) | 3 (5%) | 16 (13%) | 0.786 |
| Pre-hospital AB administration | 54 (31%) | 20 (35%) | 34 (28%) | 0.177 |
| Before Matching n = 171 | After Matching n = 166 | |||||
|---|---|---|---|---|---|---|
| PS covariate | IPL < 4 mM n = 126 | IPL ≥ 4 mM n = 45 | p Value | IPL < 4 mM n = 126 | IPL ≥ 4 mM n = 40 | p Value |
| Age | 71 ± 12 | 69 ± 15 | 0.395 | 71 ± 12 | 69 ± 15 | 0.481 |
| In-hospital LOS | 15 (8–20) | 14 (7–23) | 0.355 | 15 (8–20) | 14 (7–23) | 0.328 |
| Initial PO | 90 (85–94) | 92 (83–97) | 0.777 | 90 (85–94) | 92 (83–97) | 0.717 |
| Initial MBP | 69 ± 24 | 71 ± 22 | 0.631 | 69 ± 20 | 71 ± 22 | 0.657 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jouffroy, R.; Léguillier, T.; Gilbert, B.; Tourtier, J.P.; Bloch-Laine, E.; Ecollan, P.; Bounes, V.; Boularan, J.; Gueye-Ngalgou, P.; Nivet-Antoine, V.; et al. Pre-Hospital Lactatemia Predicts 30-Day Mortality in Patients with Septic Shock—Preliminary Results from the LAPHSUS Study. J. Clin. Med. 2020, 9, 3290. https://doi.org/10.3390/jcm9103290
Jouffroy R, Léguillier T, Gilbert B, Tourtier JP, Bloch-Laine E, Ecollan P, Bounes V, Boularan J, Gueye-Ngalgou P, Nivet-Antoine V, et al. Pre-Hospital Lactatemia Predicts 30-Day Mortality in Patients with Septic Shock—Preliminary Results from the LAPHSUS Study. Journal of Clinical Medicine. 2020; 9(10):3290. https://doi.org/10.3390/jcm9103290
Chicago/Turabian StyleJouffroy, Romain, Teddy Léguillier, Basile Gilbert, Jean Pierre Tourtier, Emmanuel Bloch-Laine, Patrick Ecollan, Vincent Bounes, Josiane Boularan, Papa Gueye-Ngalgou, Valérie Nivet-Antoine, and et al. 2020. "Pre-Hospital Lactatemia Predicts 30-Day Mortality in Patients with Septic Shock—Preliminary Results from the LAPHSUS Study" Journal of Clinical Medicine 9, no. 10: 3290. https://doi.org/10.3390/jcm9103290
APA StyleJouffroy, R., Léguillier, T., Gilbert, B., Tourtier, J. P., Bloch-Laine, E., Ecollan, P., Bounes, V., Boularan, J., Gueye-Ngalgou, P., Nivet-Antoine, V., Beaudeux, J.-L., & Vivien, B. (2020). Pre-Hospital Lactatemia Predicts 30-Day Mortality in Patients with Septic Shock—Preliminary Results from the LAPHSUS Study. Journal of Clinical Medicine, 9(10), 3290. https://doi.org/10.3390/jcm9103290





