Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke
Abstract
:1. Introduction
2. Materials and Methods
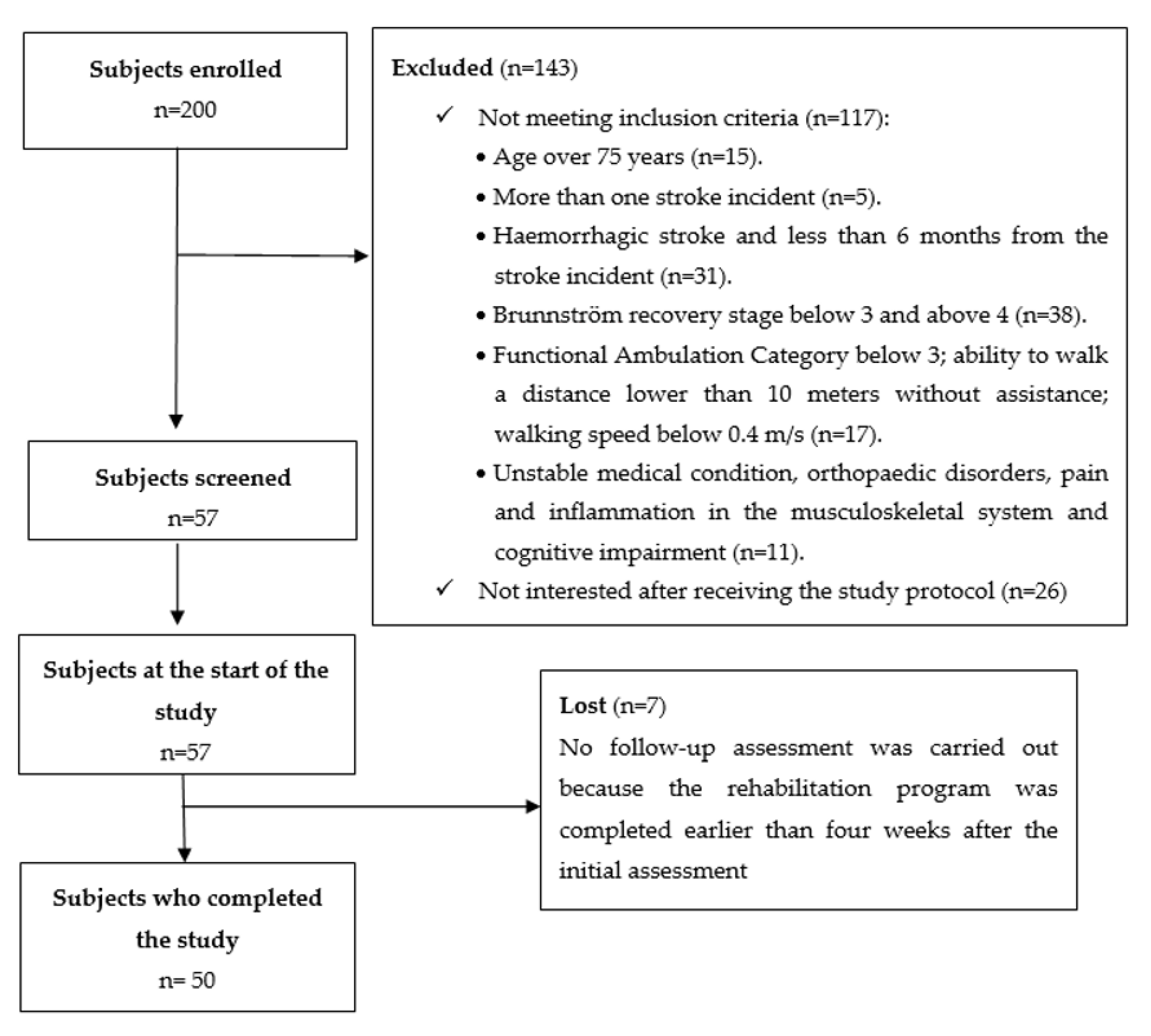
2.1. Participants
2.2. Measures
2.3. Data Analysis
2.4. Procedures
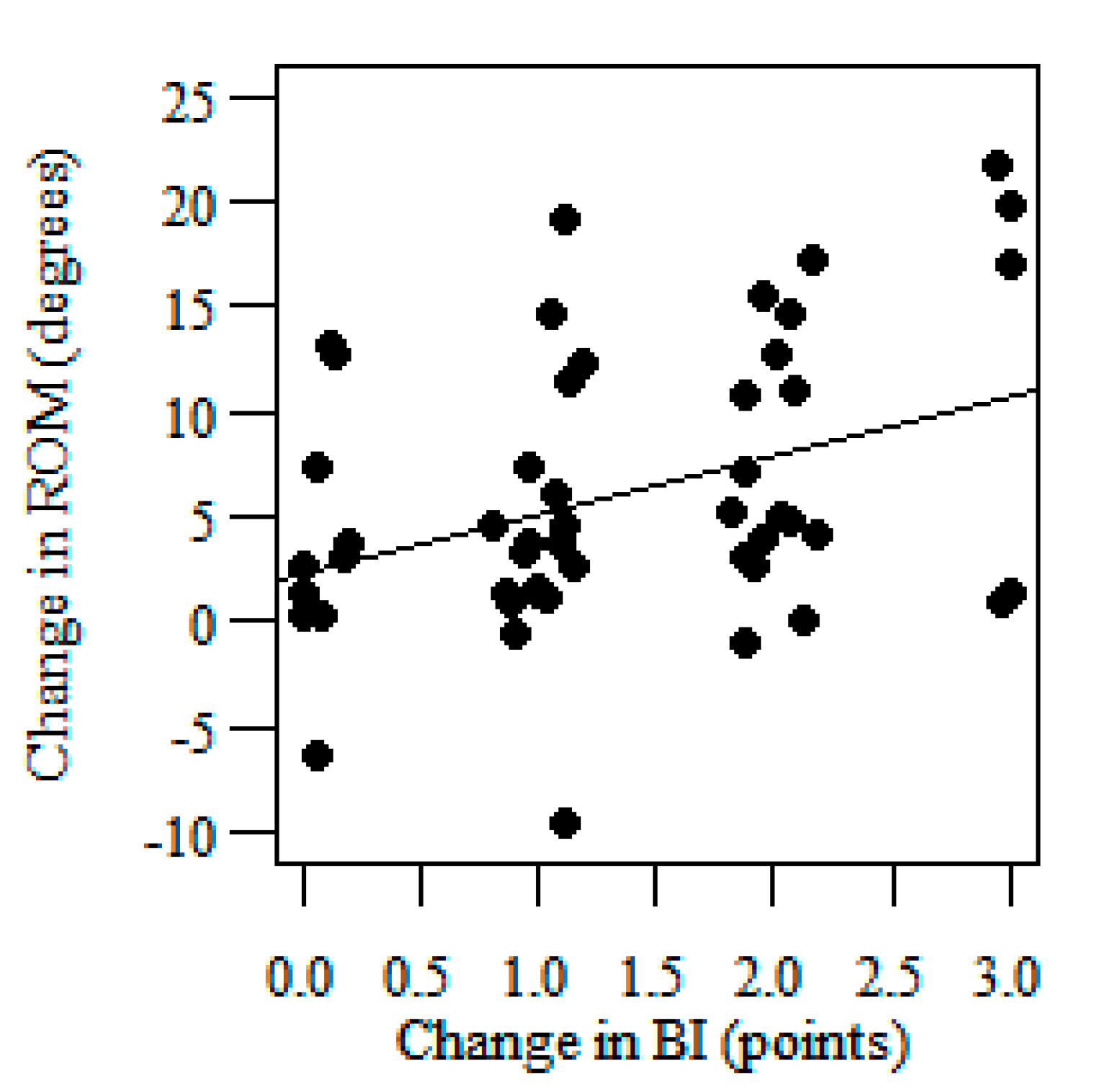
3. Results
4. Discussion
Study Limitation
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- An, S.; Lee, Y.; Shin, H.; Lee, G. Gait velocity and walking distance to predict community walking after stroke. Nurs. Health Sci. 2015, 17, 533–538. [Google Scholar] [CrossRef] [PubMed]
- van Bloemendaal, M.; van de Water, A.T.; van de Port, I.G. Walking tests for stroke survivors: A systematic review of their measurement properties. Disabil. Rehabil. 2012, 34, 2207–2221. [Google Scholar] [CrossRef] [PubMed]
- Kosak, M.; Smith, T. Comparison of the 2-, 6-, and 12-minute walk tests in patients with stroke. J. Rehabil. Res. Dev. 2005, 42, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Hafsteinsdóttir, T.B.; Rensink, M.; Schuurmans, M. Clinimetric properties of the Timed Up and Go Test for patients with stroke: A systematic review. Top. Stroke. Rehabil. 2014, 21, 197–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wonsetler, E.C.; Bowden, M.G. A systematic review of mechanisms of gait speed change post-stroke. Part 1: Spatiotemporal parameters and asymmetry ratios. Top. Stroke Rehabil. 2017, 24, 435–446. [Google Scholar] [CrossRef]
- Patterson, K.K.; Nadkarni, N.K.; Black, S.E.; McIlroy, W.E. Temporal gait symmetry and velocity differ in their relationship to age. Gait Posture 2012, 35, 590–594. [Google Scholar] [CrossRef] [Green Version]
- Barak, S.; Duncan, P.W. Issues in selecting outcome measures to assess functional recovery after stroke. NeuroRx 2006, 3, 505–524. [Google Scholar] [CrossRef] [Green Version]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Andrews, A.W.; Glenney, S.S. Minimal clinically important difference for comfortable speed as a measure of gait performance in patients undergoing inpatient rehabilitation after stroke. J. Phys. Ther. Sci. 2013, 25, 1223–1225. [Google Scholar] [CrossRef] [Green Version]
- Bushnell, C.; Bettger, J.P.; Cockroft, K.M.; Cramer, S.C.; Edelen, M.O.; Hanley, D.; Katzan, I.L.; Mattke, S.; Nilsen, D.M.; Piquado, T.; et al. Chronic Stroke Outcome Measures for Motor Function Intervention Trials: Expert Panel Recommendations. Circ. Cardiovasc. Qual. Outcomes 2015, 8, S163–S169. [Google Scholar] [CrossRef] [Green Version]
- Fulk, G.D.; He, Y. Minimal Clinically Important Difference of the 6-Minute Walk Test in People with Stroke. J. Neurol. Phys. Ther. 2018, 42, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, K.; Tirosh, O. The gait profile score and movement analysis profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, M.; Dabiri, Y.; Li, L.P. Recent Advances in Computational Mechanics of the Human Knee Joint. Comput. Math. Methods. Med. 2013, 2013, 718423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reicher, M.; Bochenek, A. Human Anathomy. General Anatomy. Bones, Joints and Ligaments; PZWL Press: Warsaw, Poland, 2008. [Google Scholar]
- Perry, J.; Garret, M.; Gronley, J.K.; Mulroy, S.J. Classification of walking handicap in the stroke population. Stroke 1995, 26, 982–989. [Google Scholar] [CrossRef] [PubMed]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Nadeau, S.; Betschart, M.; Bethoux, F. Gait analysis for poststroke rehabilitation: The relevance of biomechanical analysis and the impact of gait speed. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Boudarham, J.; Roche, N.; Pradon, D.; Bonnyaud, C.; Bensmail, D.; Zory, R. Variations in kinematics during clinical gait analysis in stroke patients. PLoS ONE 2013, 8, e66421. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.; Alghamdi, G.A.; Alghamdi, M.A.; Altowaijri, A.; Richardson, S. The relationship of lower limb muscle strength and knee joint hyperextension during the stance phase of gait in hemiparetic stroke patients. Physiother. Res. Int. 2012, 17, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarczyk, K.; Wit, A.; Krawczyk, M.; Zaborski, J. Gait classification in post-stroke patients using artificial neural networks. Gait Posture 2009, 30, 207–210. [Google Scholar] [CrossRef]
- Mun, B.M.; Lee, Y.S.; Kim, T.H.; Lee, J.H.; Sim, S.M.; Park, I.M.; Seo, D.K. Study on the usefulness of sit to stand training in self-directed treatment of stroke patients. J. Phys. Ther. Sci. 2014, 26, 483–485. [Google Scholar] [CrossRef] [Green Version]
- Beyaert, C.; Vasa, R.; Frykberg, G.E. Gait post-stroke: Pathophysiology and rehabilitation strategies. Neurophysiol. Clin. 2015, 45, 335–355. [Google Scholar] [CrossRef] [PubMed]
- De Quervain, I.A.; Simon, S.R.; Leurgans, S.; Pease, W.S.; McAllister, D. Gait pattern in the early recovery period after stroke. J. Bone Joint Surg. Am. 1996, 78, 1506–1514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.M.; Eng, J.J. Magnitude and pattern of 3D kinematic and kinetic gait profiles in persons with stroke: Relationship to walking speed. Gait Posture 2004, 20, 140–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulroy, S.; Gronley, J.; Weiss, W.; Newsam, C.; Perry, J. Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture 2003, 18, 114–125. [Google Scholar] [CrossRef]
- Olney, S.J.; Griffin, M.P.; Monga, T.N.; McBride, I.D. Work and power in gait of stroke patients. Arch. Phys. Med. Rehabil. 1991, 72, 309–314. [Google Scholar] [PubMed]
- Kinsella, S.; Moran, K. Gait pattern categorization of stroke participants with equinus deformity of the foot. Gait Posture 2008, 27, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Olney, S.J.; Griffin, M.P.; McBride, I.D. Multivariate examination of data from gait analysis of persons with stroke. Phys. Ther. 1998, 78, 814–828. [Google Scholar] [CrossRef] [Green Version]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1998, 10, 61–63. [Google Scholar] [CrossRef]
- Hsueh, I.P.; Lee, M.M.; Hsieh, C.L. Psychometric characteristics of the Barthel Activities of Daily Living Index in stroke patients. J. Formos. Med. Assoc. 2001, 100, 526–532. [Google Scholar]
- Hsieh, Y.W.; Wang, C.H.; Wu, S.C.; Chen, P.C.; Sheu, C.F.; Hsieh, C.L. Establishing the minimal clinically important difference of the Barthel Index in stroke patients. Neurorehabil. Neural. Repair. 2007, 21, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Katz, J.N.; Wright, J.G.; Wells, G.; Boers, M.; Strand, V.; Shea, B. Looking for important change/differences in studies of responsiveness. OMERACT MCID Working Group. Outcome Measures in Rheumatology. Minimal Clinically Important Difference. J. Rheumatol. 2001, 28, 400–405. [Google Scholar] [PubMed]
- Hagg, O.; Fritzell, P.; Nordwall, A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur. Spine J. 2003, 12, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Lydick, E.; Epstein, R.S. Interpretation of quality of life changes. Qual. Life Res. 1993, 2, 221–226. [Google Scholar] [CrossRef]
- Wyrwich, K.W. Minimal important difference thresholds and the standard error of measurement: Is there a connection? J. Biopharm. Stat. 2004, 14, 97–110. [Google Scholar] [CrossRef]
- Crosby, R.D.; Kolotkin, R.L.; Williams, G.R. Defining clinically meaningful change in health-related quality of life. J. Clin. Epidemiol. 2003, 56, 395–407. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction; Springer Press: New York, NY, USA, 2009. [Google Scholar]
- Hoffman, J.I.E. Variations Based on Linear Regression, in Biostatistics for Medical and Biomedical Practitioners; Academic Press: London, UK, 2015. [Google Scholar]
- Beninato, M.; Gill-Body, K.M.; Salles, S.; Stark, P.C.; Black-Schaffer, R.M.; Stein, J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch. Phys. Med. Rehabil. 2006, 87, 32–39. [Google Scholar] [CrossRef]
- Stratford, P.W.; Binkley, F.M.; Riddle, D.L. Health status measures: Strategies and analytic methods for assessing change scores. Phys. Ther. 1996, 76, 1109–1123. [Google Scholar] [CrossRef]
- Guzik, A.; Drużbicki, M. Application of the Gait Deviation Index in the analysis of post-stroke hemiparetic gait. J. Biomech. 2020, 99, 109575. [Google Scholar] [CrossRef]
- Carmo, A.A.; Kleiner, A.F.; Costa, P.H.; Barros, R.M. Three-dimensional kinematic analysis of upper and lower limb motion during gait of post-stroke patients. Braz. J. Med. Biol. Res. 2012, 45, 537–545. [Google Scholar] [CrossRef] [Green Version]
- Drużbicki, M.; Guzik, A.; Przysada, G.; Kwolek, A.; Brzozowska-Magoń, A.; Sobolewski, M. Changes in Gait Symmetry After Training on a Treadmill with Biofeedback in Chronic Stroke Patients: A 6-Month Follow-Up from a Randomized Controlled Trial. Med. Sci. Monit. 2016, 22, 4859–4868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duncan, P.W.; Lai, S.M.; Keighley, J. Defining post-stroke recovery: Implications for design and interpretation of drug trials. Neuropharmacology 2000, 39, 835–841. [Google Scholar] [CrossRef]
- Lee, K.B.; Lim, S.H.; Kim, K.H.; Kim, K.J.; Kim, Y.R.; Chang, W.N.; Yeom, J.W.; Kim, Y.D.; Hwang, B.Y. Six-month functional recovery of stroke patients: A multi-time-point study. Int. J. Rehabil. Res. 2015, 38, 173–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dąbrowski, J.; Czajka, A.; Zielińska-Turek, J.; Jaroszyński, J.; Furtak-Niczyporuk, M.; Mela, A.; Poniatowski, Ł.A.; Drop, B.; Dorobek, M.; Barcikowska-Kotowicz, M.; et al. Brain Functional Reserve in the Context of Neuroplasticity after Stroke. Neural. Plast. 2019, 2019, 9708905. [Google Scholar] [CrossRef] [Green Version]
- Kopp, B.; Kunkel, A.; Muhlnickel, W.; Villringer, K.; Taub, E.; Flor, H. Plasticity in the motor system related to therapy-induced improvement of movement after stroke. Neuroreport 1990, 10, 807–810. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |




| Group N = 50 | |
|---|---|
| Mean age, (SD) | 60.9 ± 11.2 |
| Mean time from stroke (months), range | 42 (8–120) |
| Sex (women/men) | 18/32 |
| Hemisphere lesions (right/left) | 15/35 |
| Knee Flexion/Extension Range of Motion, N = 50 | |
|---|---|
| Baseline ROM affected side (deg.), mean (SD) | 34.62 (9.71) |
| Follow-up ROM affected side (deg.), mean (SD) | 41.58 (9.52) |
| Baseline ROM unaffected side (deg.), mean (SD) | 42.33 (8.52) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.78 (8.84) |
| Baseline ROM right side (deg.), mean (SD) | 36.9 (10.24) |
| Follow-up ROM right side (deg.), mean (SD) | 44.63 (10.2) |
| Baseline ROM left side (deg.), mean (SD) | 40.08 (9.44) |
| Follow-up ROM left side (deg.), mean (SD) | 45.43 (9.67) |
| Mean Knee Sagittal ROM—MCID Group, N = 34 | |
| Baseline ROM affected side (deg.), mean (SD) | 33.6 (9.34) |
| Follow-up ROM affected side (deg.), mean (SD) | 42.1 (9.2) |
| Baseline ROM unaffected side (deg.), mean (SD) | 41.64 (8.95) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.45 (9.25) |
| Mean Knee Sagittal ROM—No-change Group, N = 16 | |
| Baseline ROM affected side (deg.), mean (SD) | 38.23 (11.0) |
| Follow-up ROM affected side (deg.), mean (SD) | 39.8 (11.26) |
| Baseline ROM unaffected side (deg.), mean (SD) | 44.88 (7.77) |
| Follow-up ROM unaffected side (deg.), mean (SD) | 48.6 (9.55) |
| MCID (deg.) | 95% Confidence Interval | ||
|---|---|---|---|
| Anchor-Based Method | 8.48 | 6.7 | 10.26 |
| Distribution-Based Method | 1.86 | 1.3 | 3.27 |
| Linear Regression Analysis | 7.71 | 5.22 | 10.2 |
| Receiver operating characteristic Curve | 3.9 | --- | --- |
| MCID (deg.) | 95% Confidence Interval | ||
|---|---|---|---|
| Anchor-Based Method | 6.81 | 4.57 | 9.05 |
| Distribution-Based Method | 5.63 | 3.93 | 9.88 |
| Linear Regression Analysis | 4.66 | 0.95 | 8.37 |
| Receiver operating characteristic Curve | 3.8 | --- | --- |
| Knee Flexion/Extension ROM (before Rehabilitation) | Age Groups (Years) | p | |||||
| Up to 50 | Over 50 | ||||||
| Mean | 95% CI | SD | Mean | 95% CI | SD | ||
| Knee flexion/extension ROM affected side (deg.) | 37.66 | 25.28–50.03 | 13.38 | 34.13 | 31.29–36.97 | 9.21 | 0.7353 |
| Knee flexion/extension ROM unaffected side (deg.) | 45.16 | 36.8–53.52 | 9.04 | 41.9 | 39.22–44.58 | 8.71 | 0.1762 |
| Knee Flexion/Extension ROM (Effects of Rehabilitation) | Age Groups (Years) | p | |||||
| Up to 50 | Over 50 | ||||||
| Mean | 95% CI | SD | Mean | 95% CI | SD | ||
| Knee flexion/extension ROM affected side (deg.) | 4.56 | 0.15–9.26 | 5.09 | 7.35 | 5.58–9.12 | 5.75 | 0.2367 |
| Knee flexion/extension ROM unaffected side (deg.) | 5.01 | 3.9–13.12 | 8.76 | 6.32 | 4.33–8.30 | 6.44 | 0.3980 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzik, A.; Drużbicki, M.; Wolan-Nieroda, A.; Turolla, A.; Kiper, P. Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. J. Clin. Med. 2020, 9, 3305. https://doi.org/10.3390/jcm9103305
Guzik A, Drużbicki M, Wolan-Nieroda A, Turolla A, Kiper P. Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. Journal of Clinical Medicine. 2020; 9(10):3305. https://doi.org/10.3390/jcm9103305
Chicago/Turabian StyleGuzik, Agnieszka, Mariusz Drużbicki, Andżelina Wolan-Nieroda, Andrea Turolla, and Pawel Kiper. 2020. "Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke" Journal of Clinical Medicine 9, no. 10: 3305. https://doi.org/10.3390/jcm9103305
APA StyleGuzik, A., Drużbicki, M., Wolan-Nieroda, A., Turolla, A., & Kiper, P. (2020). Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. Journal of Clinical Medicine, 9(10), 3305. https://doi.org/10.3390/jcm9103305







