Therapeutic Maintenance of Baricitinib and Tofacitinib in Real Life
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
- -
- RA according to the 2010 ACR/EULAR criteria [10].
- -
- Age 18 years or older.
- -
- Initiation of JAKi therapy.
- -
- No objection to the use of their data.
2.2. Data Recorded
- -
- Baseline characteristics (age, sex, body mass index, history of pulmonary, digestive and urogenital infections, neoplastic history, Charlson comorbidity index [11], and smoking).
- -
- Disease characteristics (duration of RA, positivity of rheumatoid factor (RF) and anticitrullinated protein antibodies (ACPA), presence of extra-articular manifestation, presence of erosion, prior treatments, and concomitant treatments).
- -
- Clinical data at baseline, 3 months, 6 months, and 12 months (number of nocturnal awakenings, duration of morning rusting, pain Visual Analog Scale (VAS), patient global health VAS, disease activity score in 28 joints using erythrocyte sedimentation rate (DAS-28 ESR), disease activity score in 28 joints using C-reactive protein (DAS-28 CRP), number of swollen joints (NSJ), number of tender joints (NTJ), and secondary effects (infections, neoplasia or cardiovascular events)).
- -
- Biological data at baseline, 3 months, 6 months, and 12 months (complete blood count (CBC), sedimentation rate (ESR), C-reactive protein (CRP), liver function, creatinine, modification of diet in renal disease (MDRD) clearance, and lipid profile including total cholesterol, triglycerides, low density lipoprotein cholesterol (LDLc), and high density lipoprotein cholesterol (HDLc)).
2.3. Statistical Analysis
3. Results
3.1. Patient Selection and Characteristics
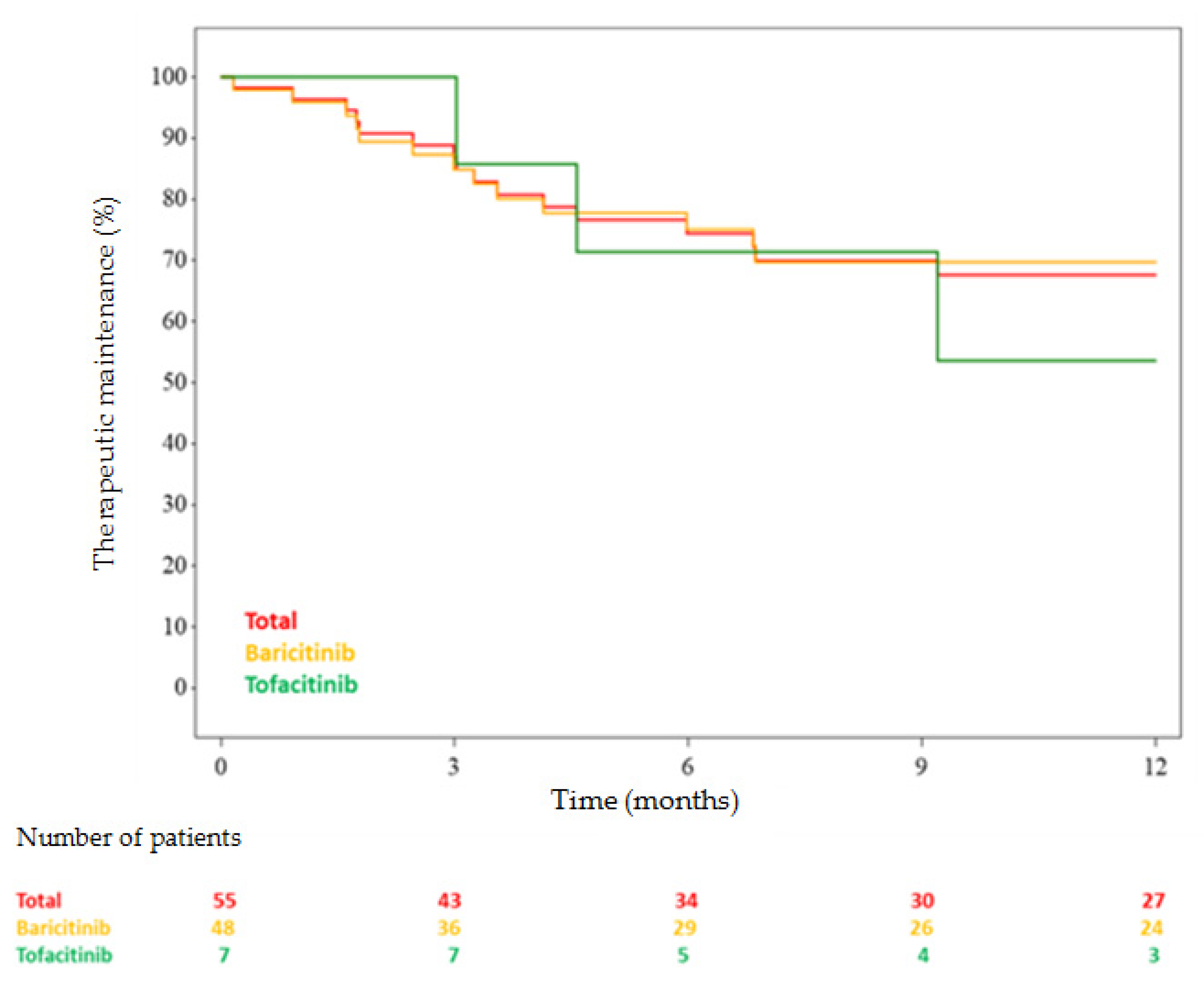
3.2. JAKi Maintenance
3.3. Factors Associated with Discontinuation of JAKis and Adverse Effects
3.4. Biological Data
3.5. Effectiveness Profile
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Smolen, J.S.; Aletaha, D.; McInnes, I.B. Rheumatoid arthritis. Lancet 2016, 388, 2023–2038. [Google Scholar] [CrossRef]
- Malemud, C.J. The role of the JAK/STAT signal pathway in rheumatoid arthritis. Ther. Adv. Musculoskelet Dis. 2018, 10, 117–127. [Google Scholar] [CrossRef]
- Dowty, M.E.; Lin, T.H.; Jesson, M.I.; Hegen, M.; Martin, D.A.; Katkade, V.; Menon, S.; Telliez, J. Janus kinase inhibitors for the treatment of rheumatoid arthritis demonstrate similar profiles of in vitro cytokine receptor inhibition. Pharmacol. Res. Perspect. 2019, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smolen, J.S.; Landewé, R.B.M.; Bijlsma, J.W.J.; Burmester, G.R.; Dougados, M.; Kerschbaumer, A.; McInnes, I.B.; Sepriano, A.; van Vollenhoven, R.F.; de Wit, M.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann. Rheum. Dis. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, J.G.; Ahern, M.J.; Coleman, M.; Weedon, H.; Papangelis, V.; Beroukas, D.; Roberts-Thomson, P.J.; Smith, M.D. Changes in synovial tissue Jak-STAT expression in rheumatoid arthritis in response to successful DMARD treatment. Ann. Rheum. Dis. 2006, 65, 1558–1564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verden, A.; Dimbil, M.; Kyle, R.; Overstreet, B.; Hoffman, K.B. Analysis of Spontaneous Postmarket Case Reports Submitted to the FDA Regarding Thromboembolic Adverse Events and JAK Inhibitors. Drug Saf. 2018, 41, 357–361. [Google Scholar] [CrossRef]
- Taylor, P.C.; Weinblatt, M.E.; Burmester, G.R.; Rooney, T.P.; Witt, S.; Walls, C.D.; Issa, M.; Salinas, C.A.; Saifan, C.; Zhang, X.; et al. Cardiovascular Safety during Treatment with Baricitinib in Rheumatoid Arthritis. Arthritis Rheumatol. 2019, 71, 1042–1055. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.B.; Tanaka, Y.; Mariette, X.; Curtis, J.R.; Lee, E.B.; Nash, P.; Winthrop, K.L.; Charles-Schoeman, C.; Thirunavukkarasu, K.; DeMasi, R.; et al. Long-term safety of tofacitinib for the treatment of rheumatoid arthritis up to 8.5 years: Integrated analysis of data from the global clinical trials. Ann. Rheum. Dis. 2017, 76, 1253–1262. [Google Scholar] [CrossRef] [Green Version]
- Daien, C.; Hua, C.; Gaujoux-Viala, C.; Cantagrel, A.; Dubremetz, M.; Dougados, M.; Fautrel, B.; Mariette, X.; Nayral, N.; Richez, C.; et al. Update of French society for rheumatology recommendations for managing rheumatoid arthritis. Jt. Bone Spine 2019, 86, 135–150. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O.; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann. Rheum. Dis. 2010, 69, 1580–1588. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Prevoo, M.L.; van’t Hof, M.A.; Kuper, H.H.; van Leeuwen, M.A.; van de Putte, L.B.; van Riel, P.L. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995, 38, 44–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salmon, J.-H.; Letarouilly, J.-G.; Goëb, V.; Kanagaratnam, L.; Coquerelle, P.; Guyot, M.-H.; Houvenagel, E.; Lecuyer, N.; Marguerie, L.; Morel, G.; et al. Actual Persistence of Abatacept in Rheumatoid Arthritis: Results of the French-Ric Network. J. Clin. Med. 2020, 9, 1528. [Google Scholar] [CrossRef] [PubMed]
- Tahiri, L.; Allali, F.; Jroundi, I.; Abouqal, R.; Hajjaj-Hassouni, N. Therapeutic maintenance level of methotrexate in rheumatoid arthritis. Sante 2006, 16, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Chopin, C.; Pauvele, L.; Jaulerry, S.; Brochot, P.; Eschard, J.-P.; Salmon, J.-H. Effectiveness, therapeutic maintenance and reasons for stopping tocilizumab (TCZ): A retrospective and monocentric study in 88 patients followed for rheumatoid arthritis (RA) at the Reims university hospital. Therapie 2018, 73, 231–236. [Google Scholar] [CrossRef]
- Figueiredo, I.T.; Morel, J.; Sany, J.; Combe, B. Maintenance and tolerability of infliximab in a cohort of 152 patients with rheumatoid arthritis. Clin. Exp. Rheumatol. 2008, 26, 18–23. [Google Scholar] [PubMed]
- Darloy, J.; Segaud, N.; Salmon, J.-H.; Eschard, J.-P.; Goëb, V.; Deprez, X.; Guyot, M.-H.; Houvenagel, E.; Lecuyer, N.; Marguerie, L.; et al. Tocilizumab Effectiveness after Switching from Intravenous to Subcutaneous Route in Patients with Rheumatoid Arthritis: The RoSwitch Study. Rheumatol. Ther. 2019, 6, 61–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, P.C.; Keystone, E.C.; van der Heijde, D.; Weinblatt, M.E.; Del Carmen Morales, L.; Reyes Gonzaga, J.; Yakushin, S.; Ishii, T.; Emoto, K.; Beattie, S.; et al. Baricitinib versus Placebo or Adalimumab in Rheumatoid Arthritis. N. Engl. J. Med. 2017, 376, 652–662. [Google Scholar] [CrossRef]
- Fleischmann, R.; Mysler, E.; Hall, S.; Kivitz, A.J.; Moots, R.J.; Luo, Z.; DeMasi, R.; Soma, K.; Zhang, R.; Takiya, L.; et al. Efficacy and safety of tofacitinib monotherapy, tofacitinib with methotrexate, and adalimumab with methotrexate in patients with rheumatoid arthritis (ORAL Strategy): A phase 3b/4, double-blind, head-to-head, randomised controlled trial. Lancet 2017, 390, 457–468. [Google Scholar] [CrossRef]
- Genovese, M.C.; Kremer, J.; Zamani, O.; Ludivico, C.; Krogulec, M.; Xie, L.; Beattie, S.D.; Koch, A.E.; Cardillo, T.E.; Rooney, T.P.; et al. Baricitinib in Patients with Refractory Rheumatoid Arthritis. N. Engl. J. Med. 2016, 374, 1243–1252. [Google Scholar] [CrossRef]
- Keystone, E.C.; Taylor, P.C.; Drescher, E.; Schlichting, D.E.; Beattie, S.D.; Berclaz, P.-Y.; Lee, C.H.; Fidelus-Gort, R.K.; Luchi, M.E.; Rooney, T.P.; et al. Safety and efficacy of baricitinib at 24 weeks in patients with rheumatoid arthritis who have had an inadequate response to methotrexate. Ann. Rheum. Dis. 2015, 74, 333–340. [Google Scholar] [CrossRef] [PubMed]
- XELJANZ (tofacitinib): Restriction d’Utilisation en cas de Risque élevé d’Embolie Pulmonaire. Available online: https://www.vidal.fr/actualites/23360/xeljanz_tofacitinib_restriction_d_utilisation_en_cas_de_risque_eleve_d_embolie_pulmonaire/ (accessed on 5 August 2020).
- Paul, S.K.; Montvida, O.; Best, J.H.; Gale, S.; Pethoe-Schramm, A.; Sarsour, K. Effectiveness of biologic and non-biologic antirheumatic drugs on anaemia markers in 153,788 patients with rheumatoid arthritis: New evidence from real-world data. Semin. Arthritis Rheum. 2018, 47, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Choy, E.H. Clinical significance of Janus Kinase inhibitor selectivity. Rheumatology 2019, 58, 953–962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smolen, J.S.; Genovese, M.C.; Takeuchi, T.; Hyslop, D.L.; Macias, W.L.; Rooney, T.; Chen, L.; Dickson, C.L.; Riddle Camp, J.; Cardillo, T.E.; et al. Safety Profile of Baricitinib in Patients with Active Rheumatoid Arthritis with over 2 Years Median Time in Treatment. J. Rheumatol. 2019, 46, 7–18. [Google Scholar] [CrossRef] [Green Version]
- Taylor, P.C.; Moore, A.; Vasilescu, R.; Alvir, J.; Tarallo, M. A structured literature review of the burden of illness and unmet needs in patients with rheumatoid arthritis: A current perspective. Rheumatol. Int. 2016, 36, 685–695. [Google Scholar] [CrossRef] [Green Version]
- Hewlett, S.; Cockshott, Z.; Byron, M.; Kitchen, K.; Tipler, S.; Pope, D.; Hehir, M. Patients’ perceptions of fatigue in rheumatoid arthritis: Overwhelming, uncontrollable, ignored. Arthritis Rheum. 2005, 53, 697–702. [Google Scholar] [CrossRef]
- Xie, F.; Yun, H.; Bernatsky, S.; Curtis, J.R. Brief Report: Risk of Gastrointestinal Perforation among Rheumatoid Arthritis Patients Receiving Tofacitinib, Tocilizumab, or Other Biologic Treatments. Arthritis Rheumatol. 2016, 68, 2612–2617. [Google Scholar] [CrossRef]
- Nakajima, A.; Inoue, E.; Shimizu, Y.; Kobayashi, A.; Shidara, K.; Sugimoto, N.; Seto, Y.; Tanaka, E.; Taniguchi, A.; Momohara, S.; et al. Presence of comorbidity affects both treatment strategies and outcomes in disease activity, physical function, and quality of life in patients with rheumatoid arthritis. Clin. Rheumatol. 2015, 34, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Neubauer, S.; Cifaldi, M.; Mittendorf, T.; Ganguli, A.; Wolff, M.; Zeidler, J. Biologic TNF inhibiting agents for treatment of rheumatoid arthritis: Persistence and dosing patterns in Germany. Health Econ. Rev. 2014, 4, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |



| Whole Population (n = 55) | |
|---|---|
| Female sex, n (%) | 45 (81.8%) |
| Age (years), med [Q1–Q3] | 58.0 [46.0–67.0] |
| Body mass index (kg/m²), med [Q1–Q3] | 25.9 [22.9–30.5] * |
| Disease duration (years), med [Q1–Q3] | 11.0 [4.0–18.0] |
| Personal medical history | |
| Infection, n (%) | 18/49 (36.7%) |
| Neoplasia, n (%) | 4 (7.3%) |
| Smoking, n (%) | 12/49 (24.5%) |
| Charlson comorbidity index, med [Q1–Q3] | 2.0 [0.0–3.0] |
| DAS-28 ESR, med [Q1–Q3] | 4.2 [3.5–4.9] |
| DAS-28 CRP, med [Q1–Q3] | 4.2 [3.3–4.8] |
| Extra-articular manifestations, n (%) | 8/53 (15.1%) |
| Treatment | |
| Methotrexate at initiation, n (%) | 30 (54.5%) |
| Methotrexate dose (mg/week), med (min–max) | 20.0 (7.5–25.0) |
| Corticosteroids at initiation | 23 (41.8%) |
| Corticosteroids dose (mg/day), med (min–max) | 7 (2–20) |
| RF positive, n (%) | 44 (80.0%) |
| ACPA positive, n (%) | 43 (78.2%) |
| Erosion presence, n (%) | 34 (61.8%) |
| Total | Baricitinib | Tofacitinib | |
|---|---|---|---|
| Stop/Censure | 16/39 | 13/35 | 3/4 |
| Kaplan–Meier (CI 95%) | |||
| 3 months | 86.89% [74.43–93.53] | 84.9% [70.88–92.51] | 100.0% [100.0–100.0] |
| 6 months | 74.45% [59.99–84.33] | 75.1% [59.41–85.43] | 71.43% [25.82–91.98] |
| 9 months | 69.93% [55.0–80.74] | 69.74% [53.4–81.29] | 71.43% [25.82–91.98] |
| 12 months | 67.6% [52.47–78.85] | 69.74% [53.4–81.29] | 53.57% [13.2–82.5] |
| Parameters | HR | Lower 95% CI | Upper 95% CI | p-Value |
|---|---|---|---|---|
| Age (for 1 year) | 1.055 | 1.015 | 1.096 | 0.0067 |
| Female vs. male sex | 1.851 | 0.420 | 8.164 | 0.4159 |
| Disease duration (for 1 year) | 1.021 | 0.964 | 1.083 | 0.4763 |
| Personal medical history | ||||
| Infections | 1.264 | 0.438 | 3.645 | 0.6647 |
| Neoplasia | 0.806 | 0.106 | 6.108 | 0.8349 |
| Smoking | 0.390 | 0.089 | 1.717 | 0.2132 |
| Charlson comorbidity index (for 1 point) | 1.358 | 1.126 | 1.638 | 0.0014 |
| DAS28-ESR at initiation (for 1 point) | 1.324 | 0.882 | 1.987 | 0.1753 |
| DAS28-CRP (at initiation (for 1 point) | 1.091 | 0.709 | 1.680 | 0.6925 |
| Prior treatment | ||||
| No prior biological treatment | 0.705 | 0.160 | 3.102 | 0.6438 |
| 1 tumor necrosis factor inhibitor versus none | 0.573 | 0.143 | 2.296 | 0.4316 |
| 2 or more tumor necrosis factor inhibitors versus none | 1.151 | 0.346 | 3.830 | 0.8190 |
| Interleukin 6 inhibitor | 1.167 | 0.434 | 3.137 | 0.7598 |
| Rituximab | 1.498 | 0.520 | 4.315 | 0.4541 |
| Abatacept | 0.955 | 0.358 | 2.551 | 0.9273 |
| Corticosteroids at initiation | 2.722 | 1.006 | 7.365 | |
| Methotrexate at initiation | 0.547 | 0.203 | 1.474 | 0.2330 |
| RF and/or ACPA positive | 1.318 | 0.299 | 5.809 | 0.7151 |
| Erosion presence | 1.116 | 0.405 | 3.072 | 0.8317 |
| Difference between Baseline and 3 Months | Difference between Baseline and 6 Months | |
|---|---|---|
| Hemoglobin (g/dL), med [Q1–Q3] | −0.4 [−1.0–0.1] ** | −0.8 [−1.1–0.1] * |
| Platelets (/mm3), med [Q1–Q3] | 56,000 [6000–82,000] * | 38,500 [−12,000–76,000] |
| Leukocytes (/mm3), med [Q1–Q3] | −300.0 [−1800–500] * | −105.0 [−1410–420] |
| Polynuclear neutrophils (/mm3), med [Q1–Q3] | −488.5 [−1229.5–516.5] * | 85.5 [−1040–655] |
| Eosinophilic cells (/mm3), med [Q1–Q3] | −40.5 [−91–145] * | −24.0 [−91–−1.0] |
| Lymphocytes (/mm3), med [Q1–Q3] | 41.0 [−400–792] * | −181.5 [–501–430] |
| ESR, med [Q1–Q3] | 0.0 [−4.0–4.0] * | −0.5 [−5.0–3.0] |
| CRP, med [Q1–Q3] | −1.1 [−5.9–0.0] * | −3.1 [−7.2–0.0] |
| Aspartate transaminase (UI/L), med [Q1–Q3] | 3.0 [−3.0–7.0] ** | 4.0 [−2.0–6.0] |
| Alanine transaminase (UI/L), med [Q1–Q3] | 1.0 [−31.0–24.0] ** | 0.0 [−6.0–7.0] |
| Creatinine (µmol/L), med [Q1–Q3] | 2.6 [−2.5–7.0] ** | 0.0 [−4.5–7.9] |
| Creatinine clearance (mL/min), med [Q1–Q3] | −2.3 [−7.8–7.3] ** | 0.0 [−11.0–7.7] |
| Total cholesterol (g/L), med [Q1–Q3] | 0.1 [−0.2–0.2] † | 0.1 [−0.1–0.2] † |
| Triglycerides (g/L), med [Q1–Q3] | 0.0 [−0.6–0.2] † | −0.3 [−0.6–0.2] † |
| LDL cholesterol (g/L), med [Q1–Q3] | 0.0 [−0.2–0.2] † | 0.0 [−0.1–0.1] † |
| HDL cholesterol (g/L), med [Q1–Q3] | 0.0 [−0.4–0.4] † | 0.0 [0.0–0.1] † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deprez, V.; Le Monnier, L.; Sobhy-Danial, J.-M.; Grados, F.; Henry-Desailly, I.; Salomon-Goëb, S.; Rabin, T.; Ristic, S.; Fumery, M.; Fardellone, P.; et al. Therapeutic Maintenance of Baricitinib and Tofacitinib in Real Life. J. Clin. Med. 2020, 9, 3319. https://doi.org/10.3390/jcm9103319
Deprez V, Le Monnier L, Sobhy-Danial J-M, Grados F, Henry-Desailly I, Salomon-Goëb S, Rabin T, Ristic S, Fumery M, Fardellone P, et al. Therapeutic Maintenance of Baricitinib and Tofacitinib in Real Life. Journal of Clinical Medicine. 2020; 9(10):3319. https://doi.org/10.3390/jcm9103319
Chicago/Turabian StyleDeprez, Valentine, Laure Le Monnier, Jean-Marc Sobhy-Danial, Franck Grados, Isabelle Henry-Desailly, Sarah Salomon-Goëb, Thibault Rabin, Sanja Ristic, Mathurin Fumery, Patrice Fardellone, and et al. 2020. "Therapeutic Maintenance of Baricitinib and Tofacitinib in Real Life" Journal of Clinical Medicine 9, no. 10: 3319. https://doi.org/10.3390/jcm9103319
APA StyleDeprez, V., Le Monnier, L., Sobhy-Danial, J.-M., Grados, F., Henry-Desailly, I., Salomon-Goëb, S., Rabin, T., Ristic, S., Fumery, M., Fardellone, P., & Goëb, V. (2020). Therapeutic Maintenance of Baricitinib and Tofacitinib in Real Life. Journal of Clinical Medicine, 9(10), 3319. https://doi.org/10.3390/jcm9103319






