Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
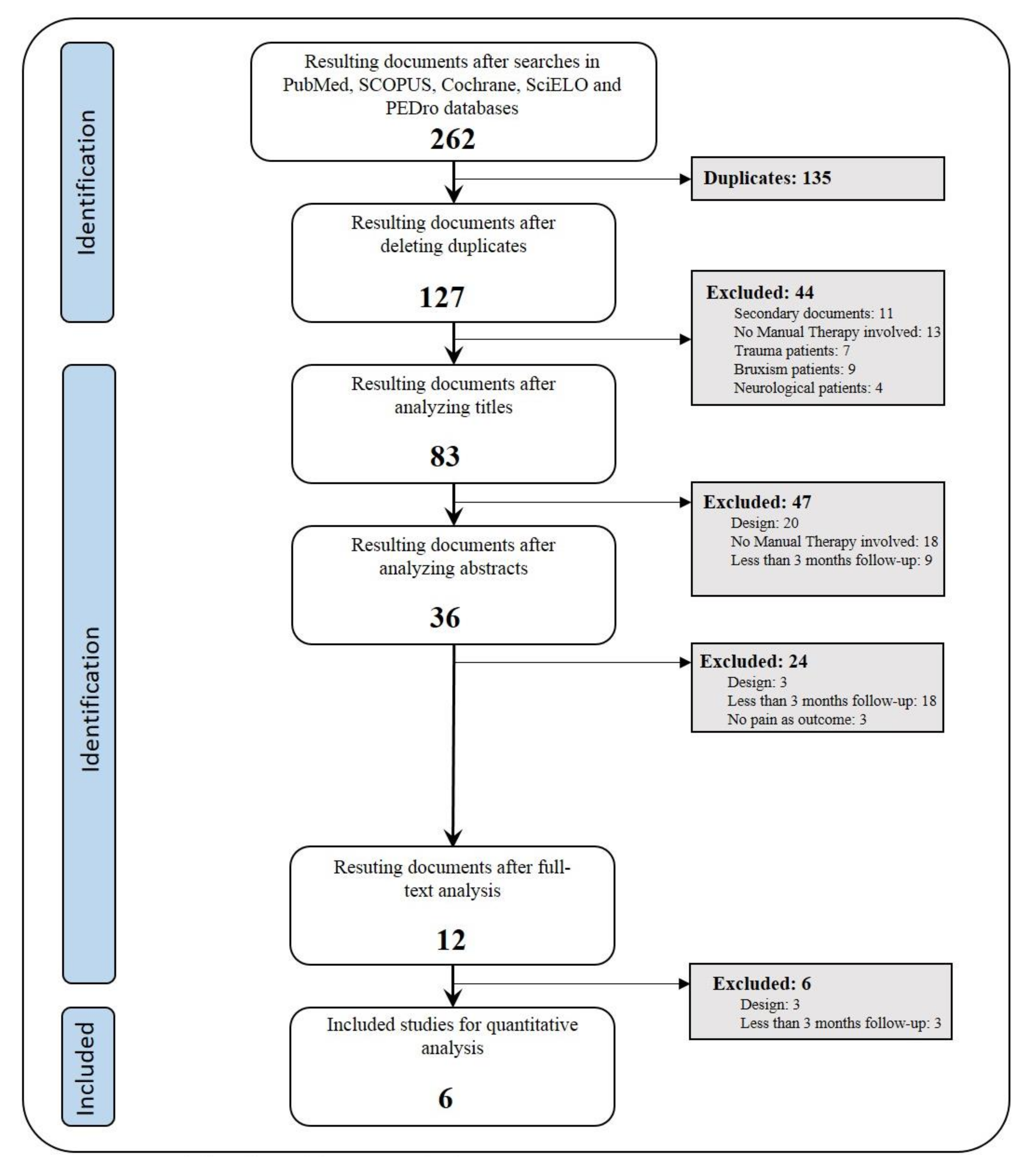
2.2. Study Selection
2.3. Inclusion and Exclusion Criteria
2.4. Outcomes
3. Results
3.1. Study Selection
3.2. Methodological Quality
4. Discussion
4.1. Pain
4.2. Mouth Opening
4.3. Study Characteristics
4.4. Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Isberg, A. Temporomandibular Joint Dysfunction: A Practitioner’s Guide; CRC Press: Boca Raton, FL, USA, 2001; ISBN 978-1-901865-44-8. [Google Scholar]
- Akheel, D.M. Temporomandibular Joint Disorders; Lulu: Morisville, NC, USA, 2014; ISBN 978-1-312-31610-2. [Google Scholar]
- Perez, C.V.; de Leeuw, R.; Okeson, J.P.; Carlson, C.R.; Li, H.-F.; Bush, H.M.; Falace, D.A. The incidence and prevalence of temporomandibular disorders and posterior open bite in patients receiving mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath. Schlaf. Atm. 2013, 17, 323–332. [Google Scholar] [CrossRef]
- Machado, L.P.e.S.; de Nery, C.G.; Leles, C.R.; de Nery, M.B.M.; Okeson, J.P. The prevalence of clinical diagnostic groups in patients with temporomandibular disorders. Cranio J. Craniomandib. Pract. 2009, 27, 194–199. [Google Scholar] [CrossRef]
- Peck, C.C.; Goulet, J.-P.; Lobbezoo, F.; Schiffman, E.L.; Alstergren, P.; Anderson, G.C.; de Leeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R.; et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2–23. [Google Scholar] [CrossRef] [Green Version]
- Isberg, A.; Stenstrom, B.; Isacsson, G. Frequency of bilateral temporomandibular joint disc displacement in patients with unilateral symptoms: A 5-year follow-up of the asymptomatic joint. A clinical and arthrotomographic study. Dento Maxillo Facial Radiol. 1991, 20, 73–76. [Google Scholar] [CrossRef]
- Okeson, J.P.; de Leeuw, R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent. Clin. North Am. 2011, 55, 105–120. [Google Scholar] [CrossRef]
- Pesquera Velasco, J.; Casares García, G.; Jiménez Pasamontes, N.; García Gómez, F.A. Método de ayuda para el diagnóstico de los trastornos de la articulación temporomandibular: Análisis discriminante aplicado a los Trastornos Temporomandibulares. Med. Oral Patol. Oral Cir. Bucal Ed. Impresa 2005, 10, 294–300. [Google Scholar]
- Tjakkes, G.-H.E.; Reinders, J.-J.; Tenvergert, E.M.; Stegenga, B. TMD pain: The effect on health related quality of life and the influence of pain duration. Health Qual. Life Outcomes 2010, 8, 46. [Google Scholar] [CrossRef] [Green Version]
- Roldán-Barraza, C.; Janko, S.; Villanueva, J.; Araya, I.; Lauer, H.-C. A systematic review and meta-analysis of usual treatment versus psychosocial interventions in the treatment of myofascial temporomandibular disorder pain. J. Oral Facial Pain Headache 2014, 28, 205–222. [Google Scholar] [CrossRef]
- Fricton, J. Current evidence providing clarity in management of temporomandibular disorders: Summary of a systematic review of randomized clinical trials for intra-oral appliances and occlusal therapies. J. Evid.-Based Dent. Pract. 2006, 6, 48–52. [Google Scholar] [CrossRef]
- Butts, R.; Dunning, J.; Pavkovich, R.; Mettille, J.; Mourad, F. Conservative management of temporomandibular dysfunction: A literature review with implications for clinical practice guidelines (Narrative review part 2). J. Bodyw. Mov. Ther. 2017, 21, 541–548. [Google Scholar] [CrossRef]
- De Gomes, C.A.F.P.; Politti, F.; Andrade, D.V.; de Sousa, D.F.M.; Herpich, C.M.; Dibai-Filho, A.V.; de Gonzalez, T.O.; Biasotto-Gonzalez, D.A. Effects of massage therapy and occlusal splint therapy on mandibular range of motion in individuals with temporomandibular disorder: A randomized clinical trial. J. Manip. Physiol. Ther. 2014, 37, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Garrigós-Pedrón, M.; La Touche, R.; Navarro-Desentre, P.; Gracia-Naya, M.; Segura-Ortí, E. Effects of a Physical Therapy Protocol in Patients with Chronic Migraine and Temporomandibular Disorders: A Randomized, Single-Blinded, Clinical Trial. J. Oral Facial Pain Headache 2018, 32, 137–150. [Google Scholar] [CrossRef] [Green Version]
- Wewege, M.A.; Booth, J.; Parmenter, B.J. Aerobic vs. resistance exercise for chronic non-specific low back pain: A systematic review and meta-analysis. J. Back Musculoskelet. Rehabil. 2018, 31, 889–899. [Google Scholar] [CrossRef] [PubMed]
- Martins, W.R.; Blasczyk, J.C.; de Aparecida Furlan Oliveira, M.; Lagôa Gonçalves, K.F.; Bonini-Rocha, A.C.; Dugailly, P.-M.; de Oliveira, R.J. Efficacy of musculoskeletal manual approach in the treatment of temporomandibular joint disorder: A systematic review with meta-analysis. Man. Ther. 2016, 21, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Pitance, L.; Singh, V.; Neto, F.; Thie, N.; Michelotti, A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys. Ther. 2016, 96, 9–25. [Google Scholar] [CrossRef] [Green Version]
- Guarda-Nardini, L.; Stecco, A.; Stecco, C.; Masiero, S.; Manfredini, D. Myofascial pain of the jaw muscles: Comparison of short-term effectiveness of botulinum toxin injections and fascial manipulation technique. Cranio J. Craniomandib. Pract. 2012, 30, 95–102. [Google Scholar] [CrossRef]
- Nagata, K.; Hori, S.; Mizuhashi, R.; Yokoe, T.; Atsumi, Y.; Nagai, W.; Goto, M. Efficacy of mandibular manipulation technique for temporomandibular disorders patients with mouth opening limitation: A randomized controlled trial for comparison with improved multimodal therapy. J. Prosthodont. Res. 2019, 63, 202–209. [Google Scholar] [CrossRef]
- Craane, B.; Dijkstra, P.U.; Stappaerts, K.; De Laat, A. Randomized controlled trial on physical therapy for TMJ closed lock. J. Dent. Res. 2012, 91, 364–369. [Google Scholar] [CrossRef]
- Kalamir, A.; Bonello, R.; Graham, P.; Vitiello, A.L.; Pollard, H. Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: A randomized controlled trial. J. Manip. Physiol. Ther. 2012, 35, 26–37. [Google Scholar] [CrossRef]
- Ismail, F.; Demling, A.; Hessling, K.; Fink, M.; Stiesch-Scholz, M. Short-term efficacy of physical therapy compared to splint therapy in treatment of arthrogenous TMD. J. Oral Rehabil. 2007, 34, 807–813. [Google Scholar] [CrossRef]
- Huang, H.; Grant, J.A.; Miller, B.S.; Mirza, F.M.; Gagnier, J.J. A Systematic Review of the Psychometric Properties of Patient-Reported Outcome Instruments for Use in Patients with Rotator Cuff Disease. Am. J. Sports Med. 2015, 43, 2572–2582. [Google Scholar] [CrossRef] [PubMed]
- Delitto, A.; George, S.Z.; Van Dillen, L.; Whitman, J.M.; Sowa, G.A.; Shekelle, P.; Denninger, T.R.; Godges, J.J. Low back pain: Clinical linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2012, 42, A1–A57. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Calderon, J.; Flores-Cortes, M.; Morales-Asencio, J.M.; Luque-Suarez, A. Conservative Interventions Reduce Fear in Individuals with Chronic Low Back Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2020, 101, 329–358. [Google Scholar] [CrossRef]
- Ulger, O.; Demirel, A.; Oz, M.; Tamer, S. The effect of manual therapy and exercise in patients with chronic low back pain: Double blind randomized controlled trial. J. Back Musculoskelet. Rehabil. 2017, 30, 1303–1309. [Google Scholar] [CrossRef]


| Garrigós-Pedrón M. (2018) [14] | Nagata K. et al. (2018) [19] | Craane B. et al. (2012) [20] | Guarda-Nardini L. et al. (2011) [18] | Kalamir A. et al. (2011) [21] | Ismail F. et al. (2007) [22] | |
|---|---|---|---|---|---|---|
| Item 1 | ● | ● | ● | ● | ● | ● |
| Item 2 | - | ● | ● | - | ● | - |
| Item 3 | ● | ● | ● | ● | ● | ● |
| Item 4 | - | ● | - | - | - | - |
| Item 5 | - | - | - | - | - | - |
| Item 6 | ● | - | ● | - | ● | - |
| Item 7 | ● | ● | ● | - | ● | ● |
| Item 8 | - | ● | ● | - | ● | - |
| Item 9 | ● | ● | ● | ● | ● | ● |
| Item 10 | ● | ● | ● | ● | ● | ● |
| TOTAL | 6/10 | 8/10 | 8/10 | 4/10 | 8/10 | 5/10 |
| Author | Sample Size (Women) | Age | Pathology | Interventions | Session Frequency |
|---|---|---|---|---|---|
| Garrigós-Pedrón M. et al. (2018) | 45(39) CG:22(19) COG:23(20) | CG: 48.2 (±11.3) COG: 46.0 (±9.1) | Chronic migraine, myofascial TMD | CG = TE (cervical muscle isometric exercises, neurodynamics) + MT (suboccipital muscle inhibition technique, passive mobilization) COG = CG + caudal longitudinal technique, NMT, TMJ TE, neurodynamics | 6 sessions 30 min/session 3–6 weeks |
| Nagata K. et al. (2018) | 61(50) TE+MT: 31 TE: 30 | 49.6 (±25) TE+MT: 48.2 (±21.1) TE: 50.7 (±18.3) | TMD, myalgia and/or arthralgia during mouth opening or palpation, limited opening (<35mm): “non-reducing disc displacement with opening limitation” | TE+MT = “boost”-type manipulation + ET TE = self-exercises, CBT, education | MT: 1 session/2 weeks (until >40mm MMO) TE: opening exercises 10 rep. 3–5/day, SMFT every hour |
| Craane B. et al. (2012) | 49(49) Physio: 23(23) Control: 26(24) | Physio: 34.7 (±14) Control: 38.5 (±15.1) | Non-reducing disc displacement with opening limitation | Physio= Education, temporal muscle stretching, intraoral treatment of masseter, opening exercises, traction and opening mobilization, self-treatment Control = Education | Physio: 2 sessions/week during first 3 weeks; 1 session/week during last 3 weeks |
| Guarda-Nardini L. et al. (2011) | 30(22) BT:15(11) FMT: 15(11) | BT: 47.7(±14.3) FMT: 43.2(±13.9) | Myofascial TMD with or without pain during mouth opening, for at least 6 months | BT = Several BT injections in masseter and temporal muscles FMT = Manual pressure at craniocervical coordination centers | BT: 1 session FMT: 3 (±1) sessions 50 min 2–4 weeks |
| Kalamir A. et al. (2011) | 93(50) IMT: 31(17) IMTES: 31(16) Control: 31(17) | IMT: 35(±6.7) IMTES: 34(±6.1) Control: 35(±5.0) | Daily periarticular pain with or without noises, for at least 3 months | IMT = Intraoral pressure in temporal muscle, lateral and medial pterygoid muscles, intraoral sphenopalatine ganglion IMT+E+S = IMT + education + self-care (cross-pressure chewing technique, post-isometric) Control = No treatment (waiting list) | IMT: 2 sessions/week 10–15 min/session 5 weeks IMTES: 4 sessions Educative talk for 2 min Exercises 2 times/day |
| Ismail F. et al. (2007) | 26(23) G1: 13(10) G2: 13(13) | G1: 44.5(±14.1) G2: 41.7(±16.5) | Arthrogenicacute TMD with less than 6 months evolution, <38 mm MMO with pain | Group 1 = Michigan splint 24 h/day except during meals Group 2 = Michigan splint + TMJ traction mobilization, massage therapy | 2 sessions/week 45 min/session 12 weeks |
| Author | Outcomes (Main; Secondary) | Follow-Up | Outcome Evolution | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain (VAS) | MMO (mm) | |||||||||||
| Base | Post | 3 M | 6 M | 1 Y | Base | Post | 3 M | 6 M | 1 Y | |||
| Garrigós-Pedrón M. (2018) | CF-PDI, HIT-6; TSK-11, VAS, temporal; masseter muscle and wrist PPT; pain-free active MMO | 6 weeks 3 months | 7.63 (1.16) | 5.965 (1.426) ** d = 1.31 | 4.126 (2.150) ** d = 2.75 | − | − | 32.87 (7.16) | 37.22 (5.98) ** d = −0.61 | 41.13 (6.49) ** d = −1.15 | − | − |
| Nagata K. (2018) | Active MMO, pain and noises from TMJ using NRS 0–10 | Every 2 weeks, for 18 weeks | 5.76 (2.26) | GRAF | GRAF | − | − | 28.32 (4.55) | GRAF | GRAF | − | − |
| Craane B. (2012) | MPQ, VAS, MFIQ, active and passive MMO (mm), masseter and temporal muscle PPT | 3, 6, 12, 26, 52 weeks | 5.0 (3.8–6.0) | − | 2.3 (0.65–3.35) | 1.75 (0.05–3) | 0.2 (0–1.6) | 35.8 (7.4) | − | 39.4 (6.3) | 41.6 (6) | 42.7 (5.7) |
| Guarda-Nardini L. (2011) | VAS, ROM | 3 months | 6.0 (2.0) | 2.1 (1.4) * | 2.5 (2.2) * | − | − | 52.0 (9.5) | − | 52.4 (N.S.) | − | − |
| Kalamir A. (2011) | 0–11 scale for pain at rest, MMO, plus both of them while clenching their jaws; MMO (mm), GRC 0–7 | 6 weeks 6 months 1 year | 4.46 (6.41) = 4.05(5.82) 4.26 (7.49) = 3.87(6.81) | − | − (N.S.) | GRAF | −3.1 = −2.82 −4.0 = −3.6 | 37.42 39.89 | − | − | GRAF | GRAF |
| Ismail F. (2007) | Active and passive MMO (mm), protrusion movement (mm), VAS (total, during movement, at rest, after mandibular loading) | 1 week 1 month 6 weeks 3 months | 4.5 (2) | − | −2.8 (2.1) | − | − | 30.1 (5.4) | − | 40.8 (4.1) | − | − |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Valencia, A.; Ruiz-Muñoz, M.; Martin-Martin, J.; Cuesta-Vargas, A.; González-Sánchez, M. Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3404. https://doi.org/10.3390/jcm9113404
Herrera-Valencia A, Ruiz-Muñoz M, Martin-Martin J, Cuesta-Vargas A, González-Sánchez M. Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(11):3404. https://doi.org/10.3390/jcm9113404
Chicago/Turabian StyleHerrera-Valencia, Andres, Maria Ruiz-Muñoz, Jaime Martin-Martin, Antonio Cuesta-Vargas, and Manuel González-Sánchez. 2020. "Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 11: 3404. https://doi.org/10.3390/jcm9113404
APA StyleHerrera-Valencia, A., Ruiz-Muñoz, M., Martin-Martin, J., Cuesta-Vargas, A., & González-Sánchez, M. (2020). Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(11), 3404. https://doi.org/10.3390/jcm9113404





