Short Term Presence of Subretinal Fluid in Central Serous Chorioretinopathy Affects Retinal Thickness and Function
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
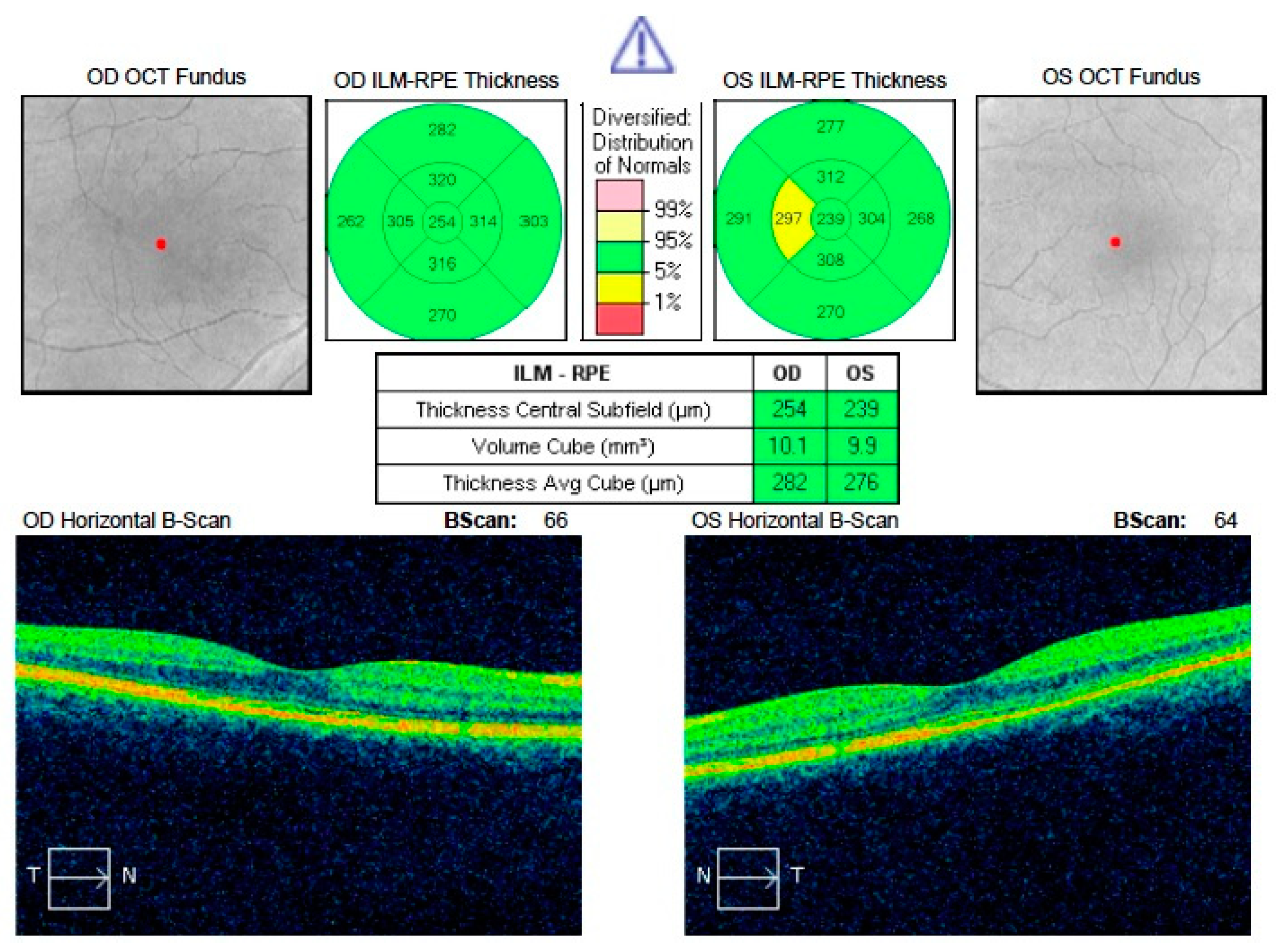
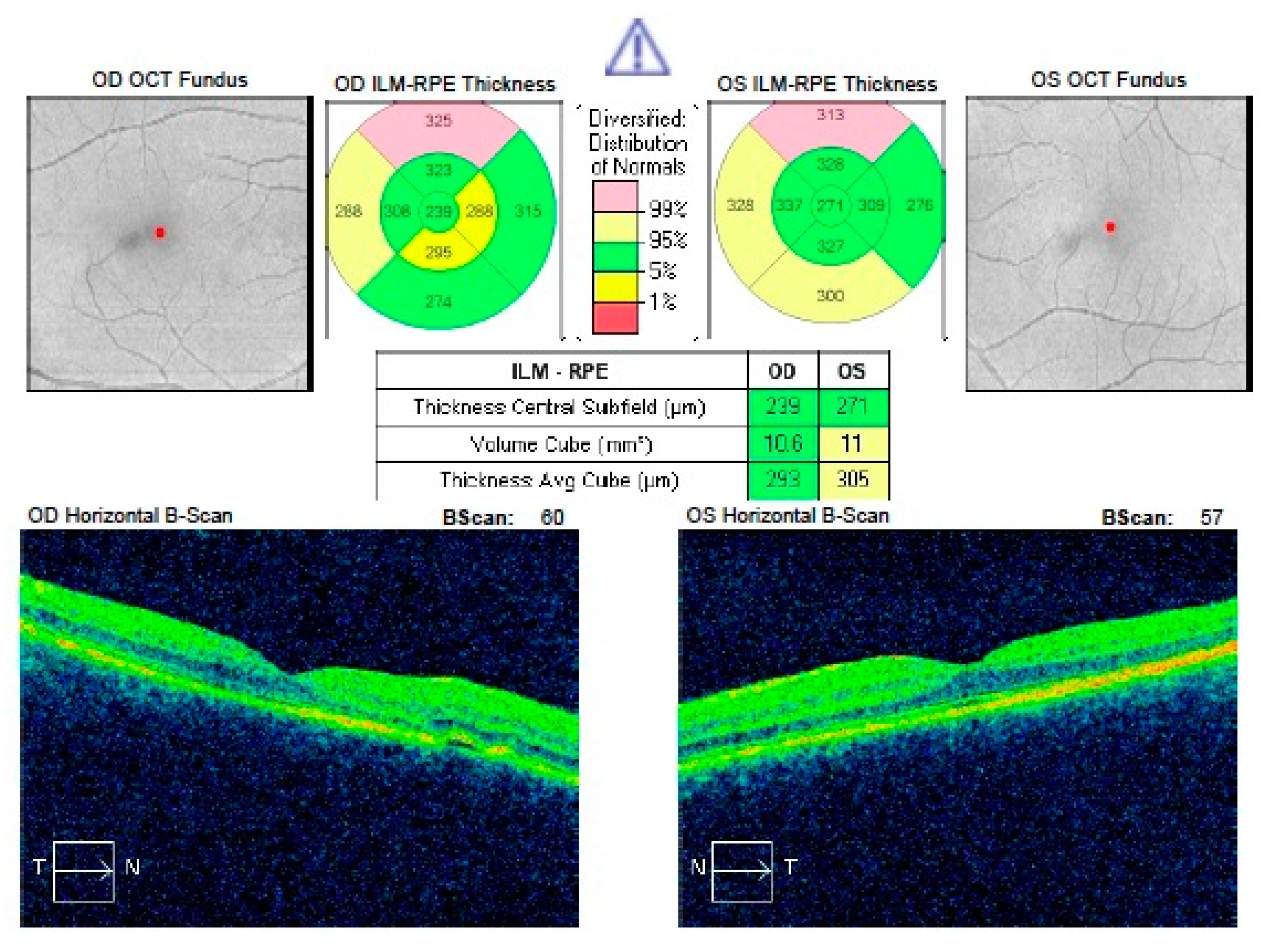
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Data Availability
Ethical Statement
References
- Daruich, A.; Matet, A.; Dirani, A.; Bousquet, E.; Zhao, M.; Farman, N.; Jaisser, F.; Behar-Cohen, F. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog. Retin. Eye Res. 2015, 48, 82–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, M.L.; Van Buskirk, E.M.; Friedman, E.; Gragoudas, E.; Chandra, S. Experience with nontreatment of central serous choroidopathy. Arch. Ophthalmol. 1974, 91, 247–503. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.; Noble, J.; Forooghian, F.; Meyerle, C. Central serous chorioretinopathy: Update on pathophysiology and treatment. Surv. Ophthalmol. 2013, 58, 103–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yannuzzi, L.A. Central serous chorioretinopathy: A personal perspective. Am. J. Ophthalmol. 2010, 149, 361–363. [Google Scholar] [CrossRef] [PubMed]
- Gass, J.D.M. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, 3rd ed.; BMJ Publishing Group: London, UK, 1987; pp. 46–59. [Google Scholar]
- Mrejen, S.; Balaratnasingam, C.; Kaden, T.R.; Bottini, A.; Dansingani, K.; Bhavsar, K.V.; Yannuzzi, N.A.; Patel, S.; Chen, K.C.; Yu, S.; et al. Long-term Visual Outcomes and Causes of Vision Loss in Chronic Central Serous Chorioretinopathy. Ophthalmology 2019, 126, 576–588. [Google Scholar] [CrossRef] [PubMed]
- Breukink, M.B.; Dingemans, A.J.; Hollander, A.I.D.; Keunen, J.E.; MacLaren, R.E.; Fauser, S.; Querques, G.; Hoyng, C.B.; Downes, S.M.; Boon, C.J. Chronic central serous chorioretinopathy: Long-term follow-up and vision-related quality of life. Clin. Ophthalmol. 2016, 11, 39–46. [Google Scholar] [CrossRef] [Green Version]
- Gawęcki, M.; Jaszczuk-Maciejewska, A.; Jurska-Jaśko, A.; Kneba, M.; Grzybowski, A. Impairment of visual acuity and retinal morphology following resolved chronic central serous chorioretinopathy. BMC Ophthalmol. 2019, 19, 160. [Google Scholar] [CrossRef] [Green Version]
- Gawęcki, M.; Jaszczuk-Maciejewska, A.; Jurska-Jaśko, A.; Grzybowski, A. Functional and morphological outcome in patients with chronic central serouschorioretinopathy treated by subthreshold micropulse laser. Graefes. Arch. Clin. Exp. Ophthalmol. 2017, 255, 2299–2306. [Google Scholar] [CrossRef]
- Luttrull, J.K.; Sinclair, S.H. Safety of transfoveal subthreshold diode micropulse laser for fovea-involving diabetic macular edema in eyes with good visual acuity. Retina 2014, 34, 2010–2020. [Google Scholar] [CrossRef] [Green Version]
- Luttrull, J.K.; Dorin, G. Subthreshold diode micropulse laser photocoagulation (SDM) as invisible retinal phototherapy for diabetic macular edema: A review. Curr. Diabetes Rev. 2012, 8, 274–284. [Google Scholar] [CrossRef] [Green Version]
- Vujosevic, S.; Martini, F.; Convento, E.; Longhin, E.; Kotsafti, O.; Parrozzani, R.; Midena, E. Subthreshold laser therapy for diabetic macular edema: Metabolic and safety issues. Curr. Med. Chem. 2013, 20, 3267–3271. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Martini, F.; Longhin, E.; Convento, E.; Cavarzeran, F.; Midena, E. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: Morphologic and functional safety. Retina 2015, 35, 1594–1603. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.K.; Jayadev, C.; Mohan, A.; Vijayan, P.; Battu, R.; Dabir, S.; Shetty, B.; Shetty, R. Subthreshold micropulse yellow laser (577 nm) in chronic central serous chorioretinopathy: Safety profile and treatment outcome. Eye 2015, 29, 258–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desmettre, T.J.; Mordon, S.R.; Buzawa, D.M.; Mainster, M.A. Micropulse and continuous wave diode retinal photocoagulation: Visible and subvisible lesion parameters. Br. J. Ophthalmol. 2016, 90, 709–712. [Google Scholar] [CrossRef] [Green Version]
- Chang, D.B.; Luttrull, J.K. Comparison of Subthreshold 577 and 810 nm Micropulse Laser Effects on Heat-Shock Protein Activation Kinetics: Implications for Treatment Efficacy and Safety. Transl. Vis. Sci. Technol. 2020, 9, 23. [Google Scholar] [CrossRef]
- Gawęcki, M. Laser treatment in retinitis pigmentosa-a review. Lasers Med. Sci. 2020, 35, 1663–1670. [Google Scholar] [CrossRef]
- Ojima, Y.; Tsujikawa, A.; Yamashiro, K.; Ooto, S.; Tamura, H.; Yoshimura, N. Restoration of outer segments of foveal photoreceptors after resolution of central serous chorioretinopathy. Jpn. J. Ophthalmol. 2010, 54, 55–60. [Google Scholar] [CrossRef] [Green Version]
- Van Rijssen, T.J.; Van Dijk, E.H.; Yzer, S.; Ohno-Matsui, K.; Keunen, J.E.; Schlingemann, R.O.; Sivaprasad, S.; Querques, G.; Downes, S.M.; Fauser, S.; et al. Central serous chorioretinopathy: Towards an evidence-based treatment guideline. Prog. Retin. Eye Res. 2019, 15, 100770. [Google Scholar] [CrossRef]
- Hata, M.; Oishi, A.; Shimozono, M.; Mandai, M.; Nishida, A.; Kurimoto, Y. Early changes in foveal thickness in eyes with central serous chorioretinopathy. Retina 2013, 33, 296–301. [Google Scholar] [CrossRef]
- Baran, N.V.; Gürlü, V.P.; Esgin, H. Long-term macular function in eyes with central serous chorioretinopathy. Clin. Exp. Ophthalmol. 2005, 33, 369–372. [Google Scholar] [CrossRef]
- Lourthai, P.; Bhurayanontachai, P. Pattern of Contrast Sensitivity Changes in Acute Central Serous Chorioretinopathy. J. Ophthalmol. 2017, 2017, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gawęcki, M.; Jaszczuk-Maciejewska, A.; Jurska-Jaśko, A.; Kneba, M.; Grzybowski, A. Transfoveal Micropulse Laser Treatment of Central Serous Chorioretinopathy within Six Months of Disease Onset. J. Clin. Med. 2019, 8, 1398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luttrull, J.K. Low-Intensity/High-Density Subthreshold Diode Micropulse Laser for Central Serous Chorioretinopathy. Retina 2016, 36, 1658–1663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, S.; Sridharan, P.; Arora, T.; Chhabra, M.; Ghosh, B. Subthreshold diode micropulse laser versus observation in acute central serous chorioretinopathy. Clin. Exp. Optom. 2019, 102, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Behnia, M.; Khabazkhoob, M.; Aliakbari, S.; Abadi, A.E.; Hashemi, H.; Pourvahidi, P. Improvement in visual acuity and contrast sensitivity in patients with central serous chorioretinopathy after macular subthreshold laser therapy. Retina 2013, 33, 324–328. [Google Scholar] [CrossRef]
- Keunen, J.E.E.; Battaglia-Parodi, M.; Vujosevic, S.; Luttrull, J.K. International Retinal Laser Society Guidelines For Subthreshold Laser Treatment. Trans. Vis. Sci. Tech. 2020, 9, 15. [Google Scholar] [CrossRef]
- Robertson, D.M.; Ilstrup, D. Direct, indirect, and sham laser photocoagulation in the management of central serous chorioretinopathy. Am. J. Ophthalmol. 1983, 95, 457–466. [Google Scholar] [CrossRef]
- Leaver, P.; Williams, C. Argon laser photocoagulation in the treatment of central serous retinopathy. Br. J. Ophthalmol. 1979, 63, 674–677. [Google Scholar] [CrossRef] [Green Version]
- Ficker, L.; Vafidis, G.; While, A.; Leaver, P. Long-term follow-up of a prospective trial of argon laser photocoagulation in the treatment of central serous retinopathy. Br. J. Ophthalmol. 1988, 72, 829–834. [Google Scholar] [CrossRef] [Green Version]
- Ambiya, V.; Khodani, M.; Goud, A.; Narayanan, R.; Tyagi, M.; Rani, P.K.; Chhablani, J. Early Focal Laser Photocoagulation in Acute Central Serous Chorioretinopathy: A Prospective, Randomized Study. Ophthalmic Surg. Lasers Imaging Retina 2017, 48, 564–571. [Google Scholar] [CrossRef]
- Liu, H.Y.; Yang, C.H.; Yang, C.M.; Ho, T.C.; Lin, C.P.; Hsieh, Y.T. Half-dose Versus Half-time Photodynamic Therapy for Central Serous Chorioretinopathy. Am. J. Ophthalmol. 2016, 167, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Zhang, F.; Chen, Y.; Dai, H.; Qu, J.; Dong, C.; Kang, X.; Liu, Y.; Yang, L.; Li, Y.; et al. A 50% vs. 30% dose of verteporfin (photodynamic therapy) for acute central serous chorioretinopathy: One-year results of a randomized clinical trial. JAMA Ophthalmol. 2015, 133, 333–340. [Google Scholar] [PubMed]
- Tsai, M.J.; Hsieh, Y.T. Half-time photodynamic therapy for central serous chorioretinopathy. Optom. Vis. Sci. 2014, 91, 1140–1145. [Google Scholar] [CrossRef]
- Hagen, S.; Ansari-Shahrezaei, S.; Smretschnig, E.; Glittenberg, C.; Krebs, I.; Graf, A.; Binder, S. The effect of photodynamic therapy on macular sensitivity in eyes with acute central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 1081–1089. [Google Scholar] [CrossRef]
- Smretschnig, E.; Ansari-Shahrezaei, S.; Moussa, S.; Glittenberg, C.; Krebs, I.; Binder, S. Half-fluence photodynamic therapy in acute central serous chorioretinopathy. Retina 2012, 32, 2014–2019. [Google Scholar] [CrossRef]
- Wu, Z.H.; Lai, R.Y.; Yip, Y.W.; Chan, W.M.; Lam, D.S.; Lai, T.Y. Improvement in multifocal electroretinography after half-dose verteporfin photodynamic therapy for central serous chorioretinopathy: A randomized placebo-controlled trial. Retina 2011, 31, 1378–1386. [Google Scholar] [CrossRef]
- Chan, W.M.; Lai, T.Y.; Lai, R.Y.; Liu, D.T.; Lam, D.S. Half-dose verteporfin photodynamic therapy for acute central serous chorioretinopathy: One-year results of a randomized controlled trial. Ophthalmology 2008, 115, 1756–1765. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.W.; Zhou, P.; Xiao, H.X.; Lv, Y.S.; Li, C.A.; Liu, G.D.; Li, X.X. Photodynamic therapy for acute central serous chorioretinopathy: The safe effective lowest dose of verteporfin. Retina 2009, 29, 1155–1161. [Google Scholar] [CrossRef]
- Kim, K.S.; Lee, W.K.; Lee, S.B. Half-dose photodynamic therapy targeting the leakage point on the fluorescein angiography in acute central serous chorioretinopathy: A pilot study. Am. J. Ophthalmol. 2014, 157, 366–373. [Google Scholar] [CrossRef]
| Parameter | Mean | Median | Minimum | Maximum | SD |
|---|---|---|---|---|---|
| Age | 42.07 | 42.00 | 30.00 | 61.00 | 9.33 |
| Duration of CSCR at presentation (weeks) | 4.73 | 4.00 | 3.00 | 8.00 | 1.33 |
| Maximum time to resolution of SRF (weeks) | 14.07 | 14.00 | 12.00 | 18.00 | 2.15 |
| Parameter | Before Treatment | After Treatment | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Mean Value | Median Value | SD | Mean Value | Median Value | SD | ||
| CRT (µm) | 406.40 | 403.00 | 96.62 | 238.80 | 240.00 | 23.39 | <0.0001 |
| MFT (µm) | 341.08 | 281.00 | 123.46 | 178.93 | 174.00 | 16.88 | <0.0001 |
| BCVA (logMAR) | 0.34 | 0.30 | 0.22 | 0.11 | 0.1 | 0.13 | <0.0001 |
| Parameter | Affected Eye after Treatment | Collateral Eye | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Mean Value | Median Value | SD | Mean Value | Median Value | SD | ||
| CRT (µm) | 238.80 | 240.00 | 23.39 | 264.87 | 266.00 | 21.22 | 0.000023 |
| MFT (µm) | 178.93 | 174.00 | 16.88 | 199.47 | 194.00 | 17.87 | 0.001 |
| BCVA (logMAR) | 0.11 | 0.10 | 0.13 | 0.01 | 0.00 | 0.04 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gawęcki, M.; Jaszczuk, A.; Grzybowski, A. Short Term Presence of Subretinal Fluid in Central Serous Chorioretinopathy Affects Retinal Thickness and Function. J. Clin. Med. 2020, 9, 3429. https://doi.org/10.3390/jcm9113429
Gawęcki M, Jaszczuk A, Grzybowski A. Short Term Presence of Subretinal Fluid in Central Serous Chorioretinopathy Affects Retinal Thickness and Function. Journal of Clinical Medicine. 2020; 9(11):3429. https://doi.org/10.3390/jcm9113429
Chicago/Turabian StyleGawęcki, Maciej, Agnieszka Jaszczuk, and Andrzej Grzybowski. 2020. "Short Term Presence of Subretinal Fluid in Central Serous Chorioretinopathy Affects Retinal Thickness and Function" Journal of Clinical Medicine 9, no. 11: 3429. https://doi.org/10.3390/jcm9113429
APA StyleGawęcki, M., Jaszczuk, A., & Grzybowski, A. (2020). Short Term Presence of Subretinal Fluid in Central Serous Chorioretinopathy Affects Retinal Thickness and Function. Journal of Clinical Medicine, 9(11), 3429. https://doi.org/10.3390/jcm9113429







