A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies
Abstract
1. Introduction
2. Experimental Section
2.1. Materials and Methods
2.2. Simple Pre-Operative Nuclear Classification Score (SPONCS)
2.3. Validation Study
2.4. Statistical Analysis
3. Results
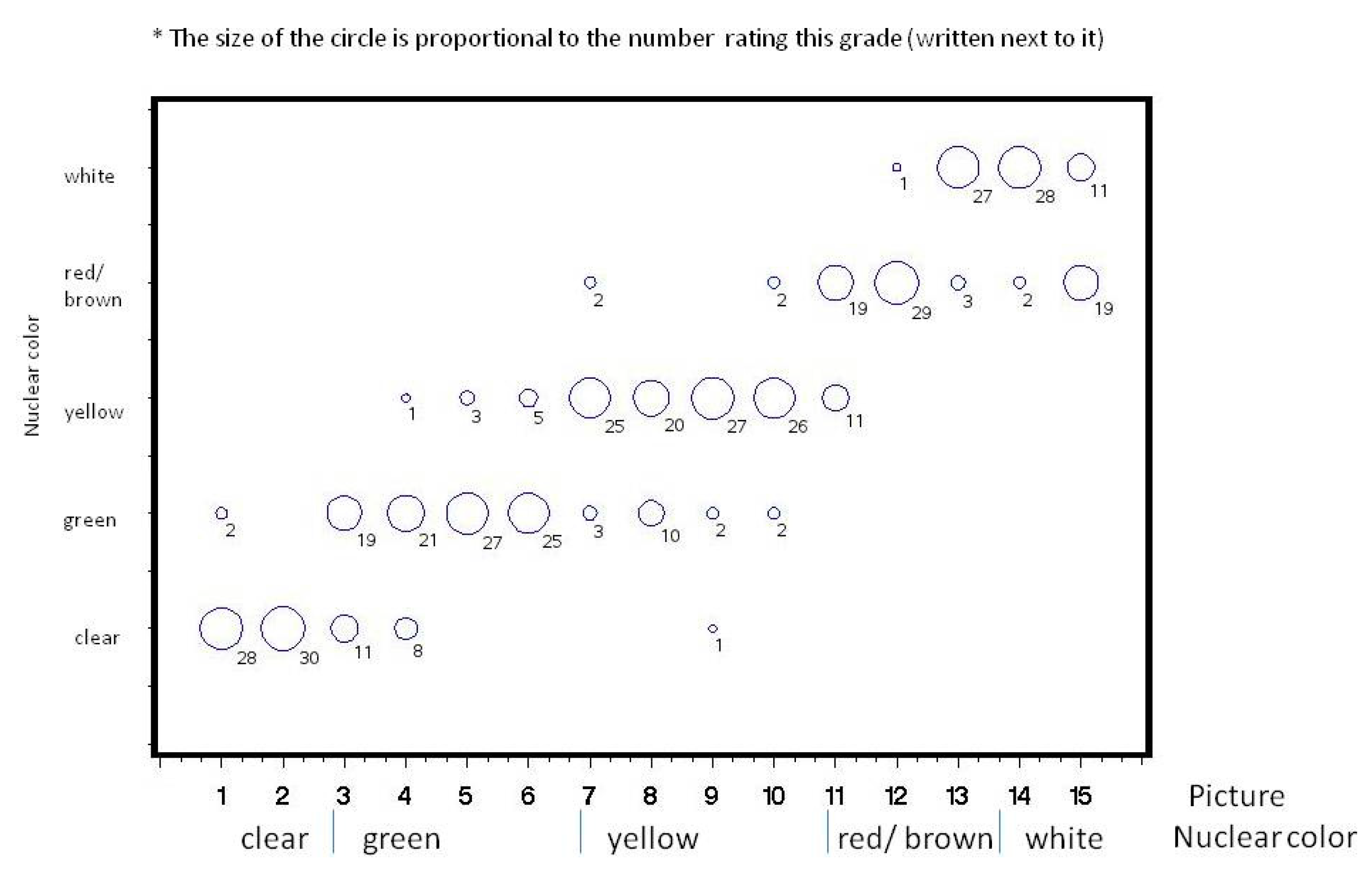
3.1. Inter-Observer Reliably
3.2. SPONCS Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Usmani, B.; Iftikhar, M.; Latif, A.; Shah, S.M. Epidemiology of primary ophthalmic procedures performed in the United States. Can. J. Ophthalmol. 2019, 54, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Chylack, L.T.J.; Leske, M.C.; Sperduto, R.; Khu, P.; McCarthy, D. Lens Opacities Classification System. Arch. Ophthalmol. 1988, 106, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Chylack, L.T.; Wolfe, J.K.; Singer, D.M.; Leske, M.C.; Bullimore, M.A.; Bailey, I.L.; Friend, J.; McCarthy, D.; Wu, S.-Y. The Lens Opacities Classification System III. Arch. Ophthalmol. 1993, 111, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Davison, J.A.; Chylack, L.T. Clinical application of the lens Opacities Classification System III in the performance of phacoemulsification. J. Cataract. Refract. Surg. 2003, 29, 138–145. [Google Scholar] [CrossRef]
- Sparrow, J.M.; Bron, A.J.; Brown, N.A.P.; Ayliffe, W.; Hill, A.R. The Oxford Clinical Cataract Classification and Grading System. Int. Ophthalmol. 1986, 9, 207–225. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Shibata, T.; Obazawa, H.; Fujiwara, T.; Kogure, F.; Obara, Y.; Itoi, M.; Katou, K.; Akiyama, K.; Okuyama, S. Classification System for Cataracts. Ophthalmic Res. 1990, 22, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Thylefors, B.; Chylack, L.T.; Konyama, K.; Sasaki, K.; Sperduto, R.; Taylor, H.R.; West, S. WHO Cataract Grading Group. A simplified cataract grading system. Ophthalmic Epidemiol. 2002, 9, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Barraquer, R.I.; Cortés, L.P.; Allende, M.J.; Montenegro, G.A.; Ivankovic, B.; D’Antin, J.C.; Osorio, H.M.; Michael, R. Validation of the Nuclear Cataract Grading System BCN 10. Ophthalmic Res. 2017, 57, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Gali, H.E.; Sella, R.; Afshari, N.A. Cataract grading systems. Curr. Opin. Ophthalmol. 2019, 30, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Du, X.-L.; Li, W.-B.; Hu, B.-J. Application of artificial intelligence in ophthalmology. Int. J. Ophthalmol. 2018, 11, 1555–1561. [Google Scholar] [PubMed]
- Liu, X.; Jiang, J.; Zhang, K.; Long, E.; Cui, J.; Zhu, M.; An, Y.; Zhang, J.; Liu, Z.; Lin, Z.; et al. Localization and diagnosis framework for pediatric cataracts based on slit-lamp images using deep features of a convolutional neural network. PLoS ONE 2017, 12, e0168606. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Lin, S.; Wong, T.Y. Automatic Feature Learning to Grade Nuclear Cataracts Based on Deep Learning. IEEE Trans. Biomed. Eng. 2015, 62, 2693–2701. [Google Scholar] [CrossRef] [PubMed]
- Rosado-Adames, N.; Afshari, N.A. The changing fate of the corneal endothelium in cataract surgery. Curr. Opin. Ophthalmol. 2012, 23, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Al-Khateeb, G.; Shajari, M.; Vunnava, K.; Petermann, K.; Kohnen, T. Impact of lens densitometry on phacoemulsification parameters and usage of ultrasound energy in femtosecond laser-assisted lens surgery. Can. J. Ophthalmol. 2017, 52, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Garcin, T.; Grivet, D.; Thuret, G.; Gain, P. Using Optical Quality Analysis System for predicting surgical parameters in age-related cataract patients. PLoS ONE 2020, 15, e0240350. [Google Scholar] [CrossRef] [PubMed]





| Classification System | Classification Method | Year | Advantages | Limitations |
|---|---|---|---|---|
| Oxford Clinical Cataract Classification and Grading System [5] | Composite Slit-Lamp-Based System. Cataract Features Are Classified Morphologically, and Individual Features Are Graded by Comparison with Standard Diagrams Mounted Adjacent to The Slit-Lamp. | 1986 | Very Detailed | Requires a Large Number of Cataract Characteristics. Complex. |
| Japanese Cooperative Cataract Epidemiology Study Group [6] | Clinical Photos of Nuclear, Cortical, and Subcapsular Opacities | 1990 | Based on Standardized Images | Designed for Epidemiological Studies. Need to Use Standardized Photograph Reference and Analyze Multiple Lens Characteristics |
| Lens Opacities Classification System (LOCS) III [2] | Six Slit-Lamp Images of Nuclear Color and Opalescence, Five Retro-Illumination Images of Cortical, and Five Retro-Illumination Images of Posterior Subcapsular Cataract | Current Gold Standard 1993 | Comprehensive and Detailed. Simplified in Comparison with Previous Classifications | Requires Reference Photographs. Difficult to Apply in Clinical Settings |
| World Health Organization (WHO) Simplified Cataract Classification [7] | Comparison to Standardized Photographs | 2002 | Separate Grading for Nuclear, Cortical, and Posterior Subcapsular Cataracts | Designed for Epidemiological Studies. Need for Reference Photographs |
| BCN 10 [8] | Reference Photograph Color Images | 2017 | Designed to Predict Lens Hardness Before Surgery. Ten Grades of Nuclear Opacity | Need for Reference Photographs |
| Artificial Intelligence (AI) [9,10,11,12] | Imaging Technology and Deep Learning | Based on Automated Optical Imaging Devices | Need for High Technology Measures. Many Algorithms. No Current Gold Standard |
| Grade | Description | Nucleus Color | Posterior Cortex Color |
|---|---|---|---|
| 0 | Clear Lens | Clear | Clear |
| 1 | Subcapsular Cataract with Clear Nucleus | Clear | Clear |
| 2 | Mild Hardness | Green | Green |
| 2+ | Green | Yellow | |
| 3 | Moderate Hardness | Yellow | Yellow |
| 3+ | Yellow | Red/Brown | |
| 4 | Advanced Hardness | Red/Brown | Red/Brown |
| 4+ | Red/Brown | White | |
| 5 | Hypermature/Morgagnian (Liquefaction of the Cortex and Sinking of The Nucleus to the Bottom of the Capsular Bag) | Black/White | Black/White |
| Variable | Category | Summary |
|---|---|---|
| Total, n (%) | 596 (100) | |
| Age (years) | Mean ± SD | 74.2 ± 10.1 |
| Median (IQR) | 76 (68–81) | |
| Gender, n (%) | ||
| Male | 258 (43.3) | |
| Female | 338 (56.7) | |
| SPONCS ○ Score, n (%) | ||
| 0 | 2 (3) | |
| 1 | 42 (7) | |
| 2 | 247 (41.4) | |
| 3 | 236 (39.6) | |
| 4 | 62 (10.4) | |
| 5 | 7 (1.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mandelblum, J.; Fischer, N.; Achiron, A.; Goldberg, M.; Tuuminen, R.; Zunz, E.; Spierer, O. A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies. J. Clin. Med. 2020, 9, 3503. https://doi.org/10.3390/jcm9113503
Mandelblum J, Fischer N, Achiron A, Goldberg M, Tuuminen R, Zunz E, Spierer O. A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies. Journal of Clinical Medicine. 2020; 9(11):3503. https://doi.org/10.3390/jcm9113503
Chicago/Turabian StyleMandelblum, Jorge, Naomi Fischer, Asaf Achiron, Mordechai Goldberg, Raimo Tuuminen, Eran Zunz, and Oriel Spierer. 2020. "A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies" Journal of Clinical Medicine 9, no. 11: 3503. https://doi.org/10.3390/jcm9113503
APA StyleMandelblum, J., Fischer, N., Achiron, A., Goldberg, M., Tuuminen, R., Zunz, E., & Spierer, O. (2020). A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies. Journal of Clinical Medicine, 9(11), 3503. https://doi.org/10.3390/jcm9113503






