Characteristics and Outcomes in Patients with Ventilator-Associated Pneumonia Who Do or Do Not Develop Acute Respiratory Distress Syndrome. An Observational Study
Abstract
:1. Introduction
2. Methods
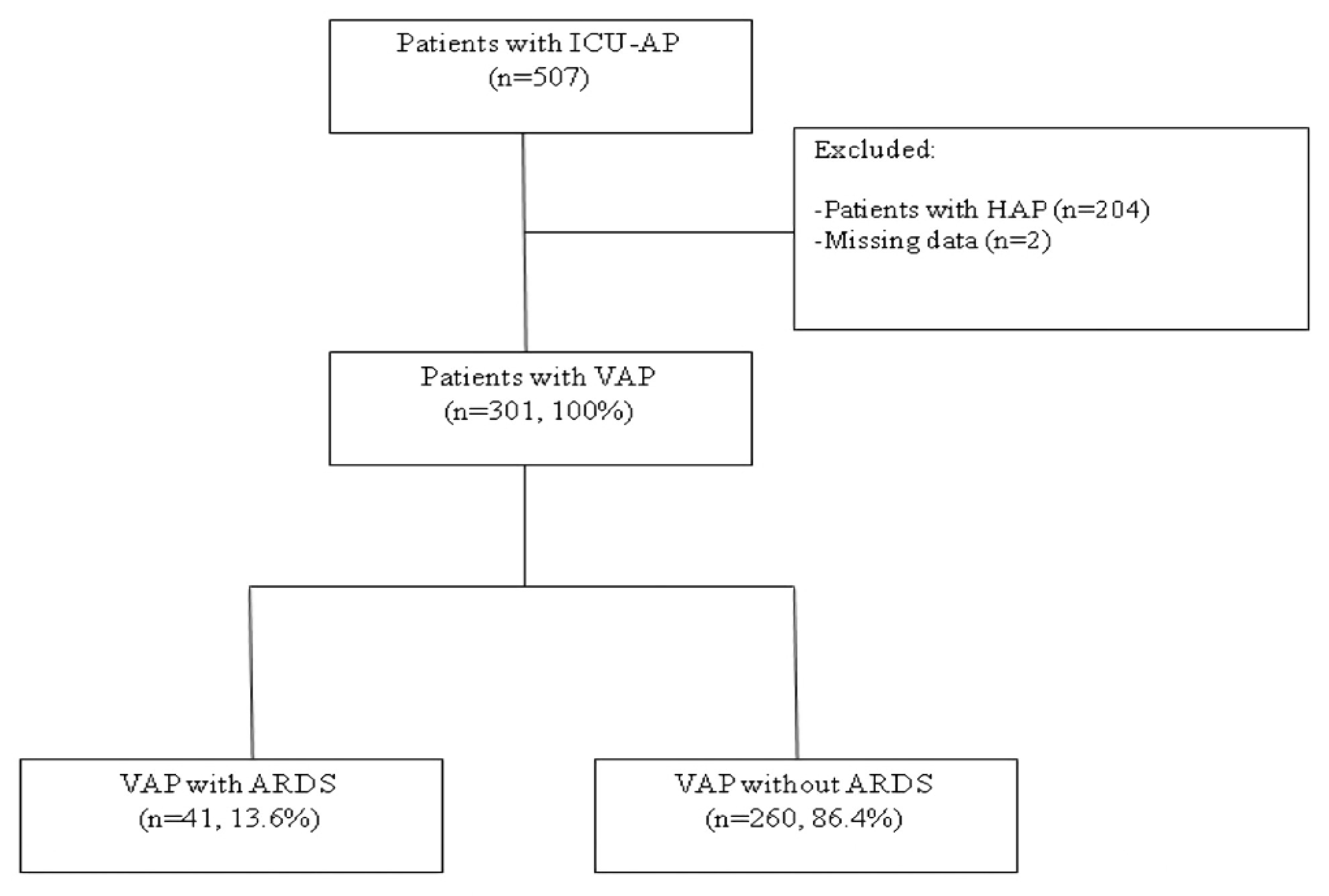
2.1. Design and Patients
2.2. Definition of Pneumonia and ARDS
2.3. Microbiological Evaluation and Diagnosis Criteria
2.4. Data Collection
2.5. Antimicrobial Treatment
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Microbiological Diagnosis
3.3. Mortality, Length of Stay, and Ventilator-Free Days
4. Discussion
5. Conclusions
List of Abbreviations
| ARDS | Acute respiratory distress syndrome |
| ATS | American thoracic society |
| CAP | Community acquired pneumonia |
| CI | Confidence interval |
| COPD | Chronic obstructive pulmonary disease |
| CPAP | Continuous positive airway pressure |
| CT | Computed tomography |
| ETI | Endotracheal intubation |
| HR | Hazard ratios |
| ICU | Intensive care unit |
| IDSA | Infectious Diseases Society of America |
| MDR | Multidrug-resistant pathogens |
| PEEP | Positive end-expiratory pressure |
| Q1 | First quartile |
| Q3 | Third quartile |
| SAPS | Simplified acute physiology score |
| SOFA | Sequential organ failure assessment |
| VAP | Ventilator associated pneumonia |
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rello, J. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest 2002, 122, 2115–2121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres, A.; Niederman, M.S.; Chastre, J.; Ewig, S.; Fernandez-Vandellos, P.; Hanberger, H.; Kollef, M.H.; Bassi, G.L.; Luna, C.M.; Martin-Loeches, I.; et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia. Eur. Respir. J. 2017, 50, 1700582. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lerma, F.; Palomar-Martínez, M.; Sanchez-García, M.; Martínez-Alonso, M.; Álvarez-Rodríguez, J.; Lorente, L.; Arias-Rivera, S.; García, R.; Gordo, F.; Añón, J.; et al. Prevention of Ventilator-Associated Pneumonia: The Multimodal Approach of the Spanish ICU “Pneumonia Zero” Program. Crit. Care Med. 2018, 46, 181–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, R.N. Microbial Etiologies of Hospital-Acquired Bacterial Pneumonia and Ventilator-Associated Bacterial Pneumonia. Clin. Infect. Dis. 2010, 51, S81–S87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melsen, W.G. Attributable mortality of ventilator-associated pneumonia: A meta-analysis of individual patient data from randomised prevention studies. Lancet Infect. Dis. 2013, 13, 665–671. [Google Scholar] [CrossRef]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Bonten, M.J. The systemic inflammatory response in the development of ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 1997, 156, 1105–1113. [Google Scholar] [CrossRef] [Green Version]
- Millo, J.L. Compartmentalisation of cytokines and cytokine inhibitors in ventilator-associated pneumonia. Intensive Care Med. 2004, 30, 68–74. [Google Scholar] [CrossRef]
- Wang, Y. Lung fluid biomarkers for acute respiratory distress syndrome: A systematic review and meta-analysis. Crit. Care 2019, 23, 43. [Google Scholar] [CrossRef] [Green Version]
- Meduri, G.U. Clinical review: A paradigm shift: The bidirectional effect of inflammation on bacterial growth. Clinical implications for patients with acute respiratory distress syndrome. Crit. Care 2002, 6, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Forel, J.M. Ventilator-associated pneumonia and ICU mortality in severe ARDS patients ventilated according to a lung-protective strategy. Crit. Care 2012, 16, R65. [Google Scholar] [CrossRef] [Green Version]
- Di Pasquale, M.; Ferrer, M.; Esperatti, M.; Crisafulli, E.; Giunta, V.; Bassi, G.L.; Rinaudo, M.; Blasi, F.; Niederman, M.; Torres, A. Assessment of severity of ICU-acquired pneumonia and association with etiology. Crit. Care Med. 2014, 42, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S. Simplified Acute Physiology Score (SAPS II) Based on a European/North American Multicenter Study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [CrossRef] [PubMed]
- Collett, D. Modelling Survival Data in Medical Research, 2nd ed.; Chapman & Hall/Crc: Boca Raton, FL, USA, 1994. [Google Scholar]
- Johnson, N.; Kotz, S.; Efron, B.; Tibshirani, R.J. lnspection Errors for Attributes in Quality Control An Introduction to the Bootstrap; J MillerJ Hand Inference Asymptot O Barndorff-Nielsen DR Cox; Chapman & Hall/CRC: Boca Raton, FL, USA, 1989; p. 153. [Google Scholar]
- Sterne, J.A.C.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ Online 2009, 339, 157–160. [Google Scholar] [CrossRef]
- Cilloniz, C.; Ferrer, M.; Liapikou, A.; García-Vidal, C.; Gabarrús, A.; Ceccato, A.; De La Bellacasa, J.P.; Blasi, F.; Torres, A. Acute respiratory distress syndrome in mechanically ventilated patients with community-acquired pneumonia. Eur. Respir. J. 2018, 51, 1702215. [Google Scholar] [CrossRef]
- Vidaur, L.; Gualis, B.; Rodriguez, A.; Ramírez, R.; Sandiumenge, A.; Sirgo, G.; Diaz, E.; Rello, J. Clinical resolution in patients with suspicion of ventilator-associated pneumonia: A cohort study comparing patients with and without acute respiratory distress syndrome. Crit. Care Med. 2005, 33, 1248–1253. [Google Scholar] [CrossRef]
- Ahmed, A.H.; Litell, J.M.; Malinchoc, M.; Kashyap, R.; Schiller, H.J.; Pannu, S.R.; Singh, B.; Li, G.; Gajic, O. The role of potentially preventable hospital exposures in the development of acute respiratory distress syndrome: A population-based study. Crit. Care Med. 2014, 42, 31–39. [Google Scholar] [CrossRef] [Green Version]
- TenHoor, T.; Mannino, D.M.; Moss, M. Risk factors for ARDS in the United States: Analysis of the 1993 National Mortality Followback Study. Chest 2001, 119, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Wip, C.; Napolitano, L. Bundles to prevent ventilator-associated pneumonia: How valuable are they? Curr. Opin. Infect. Dis. 2009, 22, 159–166. [Google Scholar] [CrossRef]
- Papazian, L. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. N. Eng. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guerin, C. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef] [PubMed]
- Briel, M. Higher vs Lower Positive End-Expiratory Pressure in Patients with Acute Lung Injury and Acute Respiratory Distress Syndrome. Systematic Review and Meta-analysis. JAMA 2010, 303, 865–873. [Google Scholar] [CrossRef] [PubMed]

| Variables | Patients with Ventilator-Associated Pneumonia Who Developed Acute Respiratory Distress Syndrome n = 41 | Patients with Ventilator-Associated Pneumonia Who Did not Develop Acute Respiratory Distress Syndrome n = 260 | p-Value |
|---|---|---|---|
| Age, years, median (Q1; Q3) | 56 (47; 69) | 66 (53; 74) | 0.020 |
| Sex, male/female, n | 23/18 | 184/76 | 0.060 |
| Alcohol abuse (current or former), n (%) | 8 (20) | 63 (24.2) | 0.55 |
| Prior corticosteroid use, n (%) | 4 (10) | 25 (10.6) | >0.99 |
| SAPS II score at ICU admission, median (Q1; Q3) | 35.5 (27; 44) | 42 (32; 53) | 0.025 |
| SOFA score at ICU admission, median (Q1; Q3) | 7 (6; 9) | 8(5; 10) | 0.95 |
| Comorbidities, n (%) a | |||
| Diabetes Mellitus | 7 (17.1) | 63 (24.2) | 0.31 |
| Chronic renal failure | 2 (4.9) | 23 (8.8) | 0.54 |
| Chronic heart disease | 8 (19.5) | 90 (34.6) | 0.055 |
| Chronic lung disease | 11 (26.8) | 81 (31.2) | 0.57 |
| COPD | 3 (7.3) | 56 (21.5) | 0.033 |
| Solid neoplasm | 6 (14.6) | 28 (10.8) | 0.43 |
| Chronic liver disease | 11 (26.8) | 32 (12.3) | 0.014 |
| Main causes of ICU admission and Severity, n (%) | |||
| Post-operative | 7 (17.1) | 55 (21.2) | 0.54 |
| Decreased consciousness | 5 (12.2) | 45 (17.3) | 0.41 |
| Hypoxemic respiratory failure | 5 (12.2) | 23 (8.8) | 0.56 |
| Multiple traumas | 3 (7.3) | 25 (9.6) | 0.77 |
| Hypercapnic respiratory failure | 7 (17.1) | 23 (8.8) | 0.15 |
| Septic shock | 4 (9.8) | 21 (8.1) | 0.76 |
| Cardiogenic shock | - | 4 (1.5) | 0.23 |
| Hypovolemic shock | 3 (7.3) | 3 (1.2) | 0.23 |
| Abdominal disorders | 2 (4.9) | 9 (3.5) | 0.65 |
| Cardiac arrest | 2 (4.9) | 24 (9.2) | 0.55 |
| Acute coronary syndrome | - | 14 (5.4) | 0.23 |
| Other | 3 (7.3) | 14 (5.4) | 0.23 |
| Days from ETI to VAP, median (Q1; Q3) | 5 (3; 9) | 6 (3; 10) | 0.79 |
| SOFA at VAP onset, median (Q1; Q3) | 9 (8; 11) | 7 (5; 10) | 0.001 |
| Shock at VAP onset, n (%) | 24 (58.5) | 123 (47.7) | 0.20 |
| PaO2/FiO2, median (Q1; Q3) | 145 (126.2; 182) | 212 (152; 272.5) | <0.001 |
| Prior ARDS diagnosis, n (%) | 8 (19) | 17 (7) | 0.005 |
| Mechanical ventilation parameters and respiratory mechanics, median (Q1; Q3) | |||
| Tidal volume (mL) | 490 (428; 527) | 500 (450; 565) | 0.18 |
| Respiratory rate (respirations per minute) | 18 (15; 20) | 16 (14; 19) | 0.012 |
| Positive end-expiratory pressure (cmH2O) | 6 (5; 10) | 7.5 (5; 9) | 0.90 |
| End-inspiratory pressure (plateau pressure) (cmH2O) | 20 (16; 26) | 21 (17; 25) | 0.96 |
| Respiratory system compliance (mL×cmH2O−1) | 38.5 (30.7; 68.5) | 40 (29.6; 54) | 0.91 |
| Driving pressure (cmH2O) | 13 (8; 16) | 14 (10; 17) | 0.51 |
| Microbiology, n (%) | Patients with Ventilator-Associated Pneumonia Who Developed Acute Respiratory Distress Syndrome n = 41 | Patients with Ventilator-Associated Pneumonia Who Did not Develop Acute Respiratory Distress Syndrome n = 260 | p-Value |
|---|---|---|---|
| Microbiological diagnosis | 25 (61) | 190 (73.1) | 0.11 |
| Pseudomonas aeruginosa | 14 (34.1) | 62 (23.8) | 0.16 |
| Pseudomonas aeruginosa MDR | 7 (17.1) | 17 (6.5) | 0.089 |
| Polymicrobial a | 7 (18.9) | 47 (18.8) | 0.99 |
| Staphylococcus aureus MSSA | 5 (13.5) | 56 (22.4) | 0.22 |
| Staphylococcus aureus MRSA | 2 (4.9) | 16 (6.2) | 0.58 |
| Klebsiella spp | 2 (5.4) | 23 (9.2) | 0.75 |
| Escherichia coli | 3 (8.1) | 10 (4) | 0.23 |
| Aspergillus spp | 2 (5.4) | 5 (2) | 0.22 |
| Proteus spp | 1 (2.7) | 5 (2) | 0.57 |
| Enterobacteriaceae spp | 1 (2.7) | 12 (4.8) | >0.99 |
| Serratia spp | 1 (2.7) | 9 (3.6) | >0.99 |
| Pneumoccocus spp | 1 (2.7) | 9 (3.6) | >0.99 |
| Stenotrophomona maltophilia | 1 (2.7) | 12 (4.8) | >0.99 |
| Virus | 2 (5.4) | 3 (1.2) | 0.13 |
| Appropriate empirical treatment | 19 (76) | 163 (85.8) | 0.20 |
| Variables | Patients with Ventilator-Associated Pneumonia Who Developed Acute Respiratory Distress Syndrome n = 41 | Patients with Ventilator-Associated Pneumonia Who Did not Develop Acute Respiratory Distress Syndrome n = 260 | p-Value |
|---|---|---|---|
| Outcomes | |||
| 28-day mortality, n (%) | 12 (29.3) | 58 (22.3) | 0.32 |
| 90-day mortality, n (%) | 18 (45) | 89 (35) | 0.22 |
| ICU mortality, n (%) | 15 (36.6) | 66 (25.4) | 0.13 |
| ICU length of stay (days), median (Q1; Q3) | 21 (13; 41) | 19 (13; 31) | 0.26 |
| Hospital length of stay (days), median (Q1; Q3) | 37 (21; 63) | 37.5 (21; 61.5) | 0.59 |
| 28-day ventilator-free days, median (Q1; Q3) | 0 (0; 17.5) | 12 (0; 22) | 0.10 |
| Duration of mechanical ventilation (days), median (Q1; Q3) | 18 (11; 33) | 14 (9; 24) | 0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbeta, E.; Ceccato, A.; Artigas, A.; Ferrer, M.; Fernández, L.; López, R.; Bueno, L.; Motos, A.; Li Bassi, G.; Mellado, R.; et al. Characteristics and Outcomes in Patients with Ventilator-Associated Pneumonia Who Do or Do Not Develop Acute Respiratory Distress Syndrome. An Observational Study. J. Clin. Med. 2020, 9, 3508. https://doi.org/10.3390/jcm9113508
Barbeta E, Ceccato A, Artigas A, Ferrer M, Fernández L, López R, Bueno L, Motos A, Li Bassi G, Mellado R, et al. Characteristics and Outcomes in Patients with Ventilator-Associated Pneumonia Who Do or Do Not Develop Acute Respiratory Distress Syndrome. An Observational Study. Journal of Clinical Medicine. 2020; 9(11):3508. https://doi.org/10.3390/jcm9113508
Chicago/Turabian StyleBarbeta, Enric, Adrian Ceccato, Antoni Artigas, Miquel Ferrer, Laia Fernández, Rubén López, Leticia Bueno, Anna Motos, Gianluigi Li Bassi, Ricard Mellado, and et al. 2020. "Characteristics and Outcomes in Patients with Ventilator-Associated Pneumonia Who Do or Do Not Develop Acute Respiratory Distress Syndrome. An Observational Study" Journal of Clinical Medicine 9, no. 11: 3508. https://doi.org/10.3390/jcm9113508
APA StyleBarbeta, E., Ceccato, A., Artigas, A., Ferrer, M., Fernández, L., López, R., Bueno, L., Motos, A., Li Bassi, G., Mellado, R., Ferrando, C., Palomeque, A. C., Panigada, M., Gabarrús, A., de Mendoza, D., & Torres, A. (2020). Characteristics and Outcomes in Patients with Ventilator-Associated Pneumonia Who Do or Do Not Develop Acute Respiratory Distress Syndrome. An Observational Study. Journal of Clinical Medicine, 9(11), 3508. https://doi.org/10.3390/jcm9113508








