Lycium barbarum Polysaccharide Suppresses Expression of Fibrotic Proteins in Primary Human Corneal Fibroblasts
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Cell Characterization
2.3. LBP Preparation and Treatment
2.4. Treatment of Cells
2.5. Immunofluorescence
2.6. Western Blot
2.7. Cell Viability Assay
2.8. Statistical Analysis
3. Results
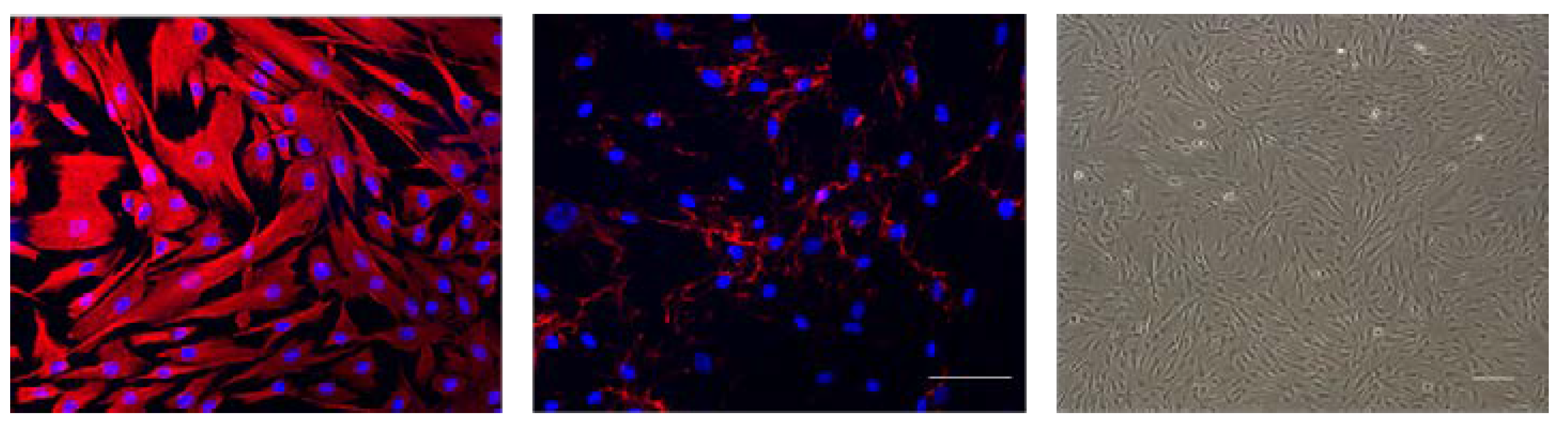
3.1. Corneal Fibroblasts Express Vimentin and Fibronectin
3.2. LBP Selectively Affects Myofibroblast Cell Viability
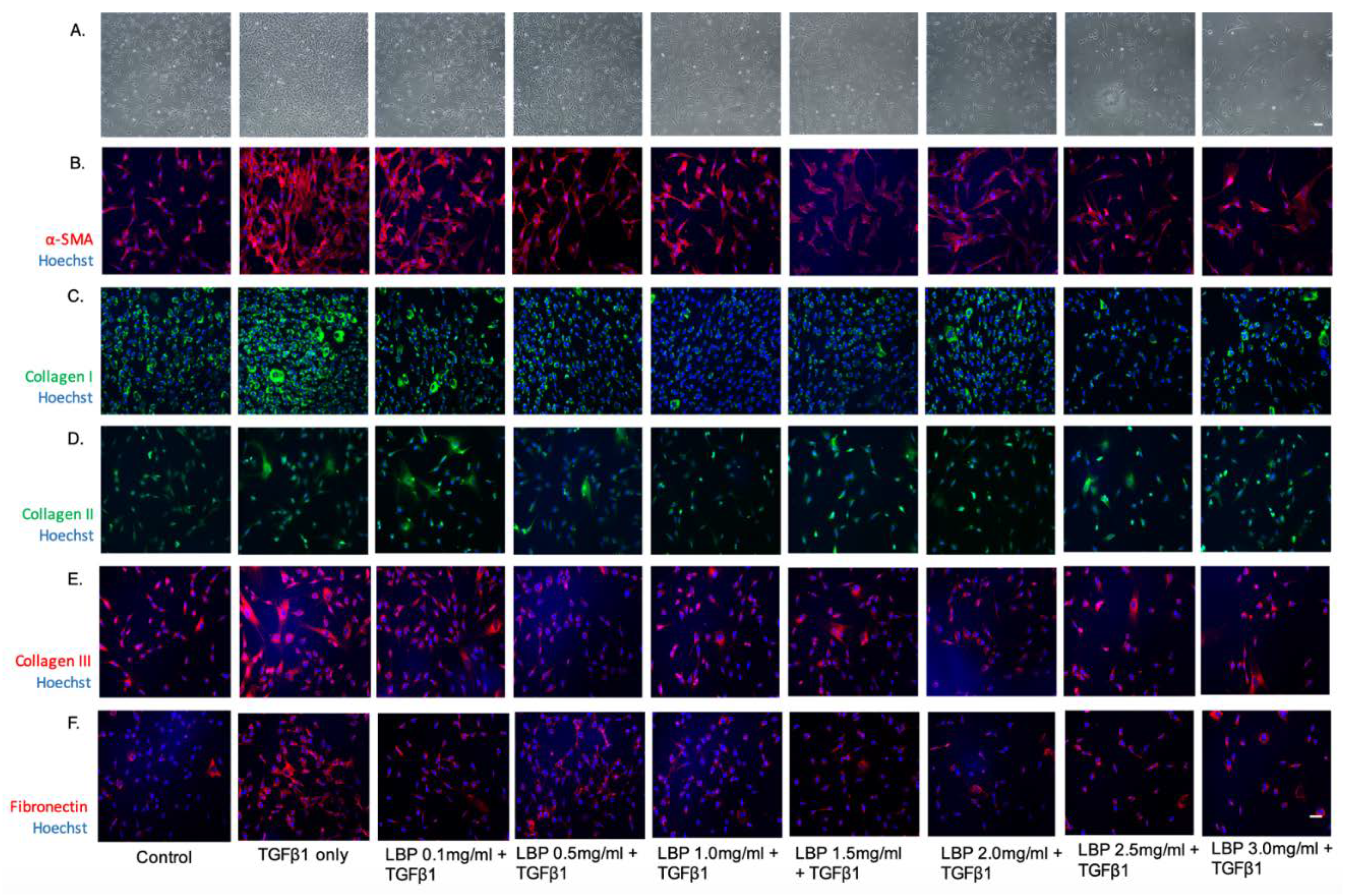
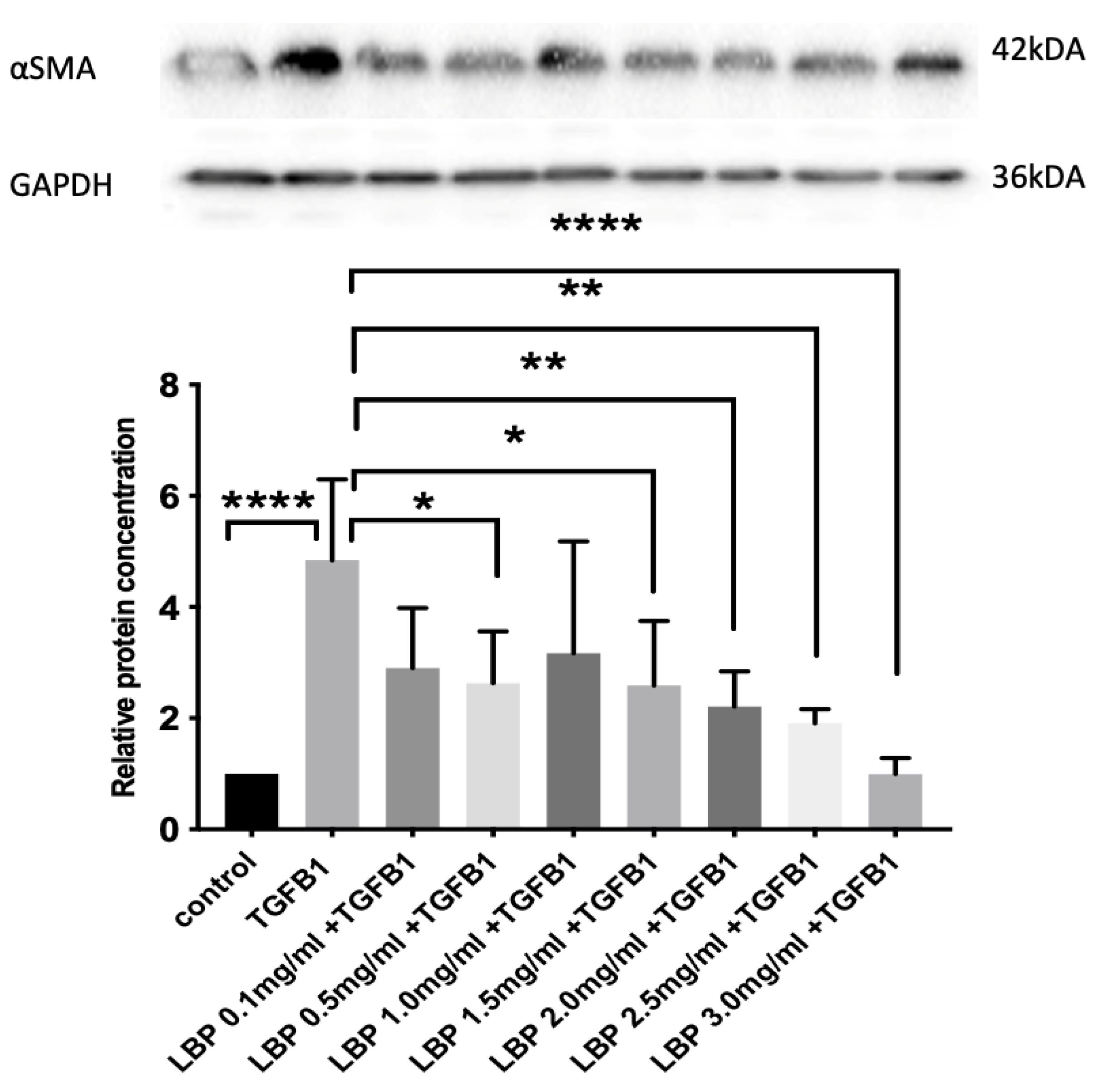
3.3. LBP Attenuates TGFβ1-Induced Fibrosis
3.4. LBP Has No Significant Effect on Fibroblasts
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability Statement
References
- Whitcher, J.P.; Srinivasan, M.; Upadhyay, M.P. Corneal blindness: A global perspective. Bull. World Health Organ. 2001, 79, 214–221. [Google Scholar] [PubMed]
- Kwok, S.S.; Shih, K.C.; Bu, Y.; Lo, A.C.; Chan, T.C.; Lai, J.S.; Jhanji, V.; Tong, L. Systematic Review on Therapeutic Strategies to Minimize Corneal Stromal Scarring After Injury. Eye Contact Lens 2019, 45, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.C.; Kwon, J.W.; Han, Y.K.; Wee, W.R.; Lee, J.H. The epidemiology of cosmetic treatments for corneal opacities in a Korean population. Korean J. Ophthalmol. 2010, 24, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Hirst, L.W.; Farmer, E.R.; Green, W.R.; Silver, A.; Walsh, F.B. Familial corneal scarring: A new dystrophy? Ophthalmology 1984, 91, 174–178. [Google Scholar] [CrossRef]
- Al Arfaj, K.; Al Zamil, W. Spontaneous corneal perforation in ocular rosacea. Middle East Afr. J. Ophthalmol. 2010, 17, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Sriram, S.; Gibson, D.J.; Robinson, P.; Pi, L.; Tuli, S.; Lewin, A.S.; Schultz, G. Assessment of anti-scarring therapies in ex vivo organ cultured rabbit corneas. Exp. Eye Res. 2014, 125, 173–182. [Google Scholar] [CrossRef]
- Tandon, A.; Tovey, J.C.K.; Sharma, A.; Gupta, R.; Mohan, R.R. Role of transforming growth factor Beta in corneal function, biology and pathology. Curr. Mol. Med. 2010, 10, 565–578. [Google Scholar]
- Strissel, K.J.; Rinehart, W.B.; Fini, M.E. A corneal epithelial inhibitor of stromal cell collagenase synthesis identified as TGF-beta 2. Investig. Ophthalmol. Vis. Sci. 1995, 36, 151–162. [Google Scholar]
- Khong, J.J.; Muecke, J. Complications of mitomycin C therapy in 100 eyes with ocular surface neoplasia. Br. J. Ophthalmol. 2006, 90, 819–822. [Google Scholar] [CrossRef]
- Rubinfeld, R.S.; Pfister, R.R.; Stein, R.M.; Foster, C.S.; Martin, N.F.; Stoleru, S.; Talley, A.R.; Speaker, M.G. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology 1992, 99, 1647–1654. [Google Scholar] [CrossRef]
- Huxlin, K.R.; Hindman, H.B.; Jeon, K.-I.; Bühren, J.; MacRae, S.; DeMagistris, M.; Ciufo, D.; Sime, P.J.; Phipps, R.P. Topical rosiglitazone is an effective anti-scarring agent in the cornea. PLoS ONE 2013, 8, e70785. [Google Scholar] [CrossRef]
- Cho, Y.W.; Yoo, W.S.; Kim, S.J.; Chung, I.Y.; Seo, S.W.; Yoo, J.M. Efficacy of systemic vitamin C supplementation in reducing corneal opacity resulting from infectious keratitis. Medicine (Baltimore) 2014, 93, e125. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Rodier, J.T.; Sharma, A.; Giuliano, E.A.; Sinha, P.R.; Hesemann, N.P.; Mohan, R.R. Targeted AAV5-Smad7 gene therapy inhibits corneal scarring in vivo. PLoS ONE 2017, 12, e0172928. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Jiang, X.; Wang, T.; Zhang, B.; Zhao, H. Lyciumbarbarum Polysaccharide (LBP): A Novel Prebiotics Candidate for Bifidobacterium and Lactobacillus. Front. Microbiol. 2018, 9, 1034. [Google Scholar] [CrossRef]
- Xiao, J.; Xing, F.; Huo, J.; Fung, M.L.; Liong, E.C.; Ching, Y.P.; Xu, A.; Chang, R.C.C.; So, K.F.; Tipoe, G.L. Lycium barbarum polysaccharides therapeutically improve hepatic functions in non-alcoholic steatohepatitis rats and cellular steatosis model. Sci. Rep. 2014, 4, 5587. [Google Scholar] [CrossRef]
- Gan, F.; Liu, Q.; Liu, Y.; Huang, D.; Pan, C.; Song, S.; Huang, K. Lycium barbarum polysaccharides improve CCl4-induced liver fibrosis, inflammatory response and TLRs/NF-κB signaling pathway expression in wistar rats. Life Sci. 2018, 192, 205–212. [Google Scholar] [CrossRef]
- Du, S.; Han, B.; Li, K.; Zhang, X.; Sha, X.; Gao, L. Lycium barbarum Polysaccharides Protect Rat Corneal Epithelial Cells against Ultraviolet B-Induced Apoptosis by Attenuating the Mitochondrial Pathway and Inhibiting JNK Phosphorylation. Biomed. Res. Int. 2017, 2017, 5806832. [Google Scholar] [CrossRef] [PubMed]
- Jester, J.V. An Eye on Repair; Springer: Boston, MA, USA, 2006; pp. 118–138. [Google Scholar] [CrossRef]
- Myrna, K.E.; Pot, S.A.; Murphy, C.J. Meet the corneal myofibroblast: The role of myofibroblast transformation in corneal wound healing and pathology. Vet. Ophthalmol. 2009, 12 (Suppl. 1), 25–27. [Google Scholar] [CrossRef]
- Guo, X.; Sriram, S.; Tran, J.A.; Hutcheon, A.E.K.; Zieske, J.D. Inhibition of Human Corneal Myofibroblast Formation. Investig. Ophthalmol. Vis. Sci. 2018, 59, 3511–3520. [Google Scholar] [CrossRef]
- Zhang, K.; Rekhter, M.D.; Gordon, D.; Phan, S.H. Myofibroblasts and their role in lung collagen gene expression during pulmonary fibrosis. A combined immunohistochemical and in situ hybridization study. Am. J. Pathol. 1994, 145, 114–125. [Google Scholar]
- Ihanamaki, T.; Pelliniemi, L.J.; Vuorio, E. Collagens and collagen-related matrix components in the human and mouse eye. Prog. Retin. Eye Res. 2004, 23, 403–434. [Google Scholar] [CrossRef] [PubMed]
- Hassell, J.R.; Birk, D.E. The molecular basis of corneal transparency. Exp. Eye Res. 2010, 91, 326–335. [Google Scholar] [CrossRef]
- Hinz, B.; Gabbiani, G. Mechanisms of force generation and transmission by myofibroblasts. Curr. Opin. Biotechnol. 2003, 14, 538–546. [Google Scholar] [CrossRef]
- Greene, C.A.; Green, C.R.; Dickinson, M.E.; Johnson, V.; Sherwin, T. Keratocytes are induced to produce collagen type II: A new strategy for in vivo corneal matrix regeneration. Exp. Cell Res. 2016, 347, 241–249. [Google Scholar] [CrossRef]
- Yam, G.H.F.; Riau, A.K.; Funderburgh, M.L.; Mehta, J.S.; Jhanji, V. Keratocyte biology. Exp. Eye Res. 2020, 196, 108062. [Google Scholar] [CrossRef]
- Kwok, S.S.; Bu, Y.; Lo, A.C.; Chan, T.C.; So, K.F.; Lai, J.S.; Shih, K.C. A Systematic Review of Potential Therapeutic Use of Lycium Barbarum Polysaccharides in Disease. Biomed. Res. Int. 2019, 2019, 4615745. [Google Scholar] [CrossRef]
- Chien, K.J.; Horng, C.T.; Huang, Y.S.; Hsieh, Y.H.; Wang, C.J.; Yang, J.S.; Lu, C.C.; Chen, F.A. Effects of Lycium barbarum (goji berry) on dry eye disease in rats. Mol. Med. Rep. 2018, 17, 809–818. [Google Scholar] [CrossRef]



| Primary Antibodies | Company | Catalogue Number | Dilution | Host Species |
|---|---|---|---|---|
| Anti-vimentin | Abcam | Ab92547 | 1:500 | Rabbit |
| Anti-fibronectin | Abcam | Ab2413 | 1:1000 | Rabbit |
| Anti-α-smooth muscle actin | Abcam | ab124964 | 1:250 | Rabbit |
| Anti-collagen type I | Abcam | ab34710 | 1:500 | Rabbit |
| Anti-collagen type II | Abcam | ab34712 | 1:150 | Rabbit |
| Anti-collagen Type III | Abcam | ab6310 | 1:200 | Mouse |
| Secondary antibodies | ||||
| Anti-Rabbit IgG H&L (Alexa Fluor® 594) | Abcam | ab150080 | 1:500 | Goat |
| Anti-Rabbit IgG H&L (Alexa Fluor® 488) | Abcam | ab150073 | 1:500 | Donkey |
| Anti-Mouse IgG H&L (Alexa Fluor® 594) | Abcam | ab150108 | 1:500 | Donkey |
| Primary Antibodies | Company | Model Number | Dilution | Host Species |
|---|---|---|---|---|
| Anti-α-smooth muscle actin | Abcam | ab124964 | 1:10,000 | Rabbit |
| Anti-GAPDH | Santa Cruz | sc-32233 | 1:200 | Mouse |
| Secondary antibodies | ||||
| Anti-Rabbit IgG H&L (HRP) | Abcam | ab205718 | 1:2000 | Goat |
| Anti-Mouse IgG H&L (HRP) | Abcam | ab6728 | 1:5000 | Rabbit |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwok, S.S.; Wong, F.S.-Y.; Shih, K.C.; Chan, Y.-K.; Bu, Y.; Chan, T.C.-Y.; Ng, A.L.-K.; Lo, A.C.-Y.; Tong, L.; Yam, G.H.-F.; et al. Lycium barbarum Polysaccharide Suppresses Expression of Fibrotic Proteins in Primary Human Corneal Fibroblasts. J. Clin. Med. 2020, 9, 3572. https://doi.org/10.3390/jcm9113572
Kwok SS, Wong FS-Y, Shih KC, Chan Y-K, Bu Y, Chan TC-Y, Ng AL-K, Lo AC-Y, Tong L, Yam GH-F, et al. Lycium barbarum Polysaccharide Suppresses Expression of Fibrotic Proteins in Primary Human Corneal Fibroblasts. Journal of Clinical Medicine. 2020; 9(11):3572. https://doi.org/10.3390/jcm9113572
Chicago/Turabian StyleKwok, Sum Sum, Francisca Siu-Yin Wong, Kendrick Co Shih, Yau-Kei Chan, Yashan Bu, Tommy Chung-Yan Chan, Alex Lap-Ki Ng, Amy Cheuk-Yin Lo, Louis Tong, Gary Hin-Fai Yam, and et al. 2020. "Lycium barbarum Polysaccharide Suppresses Expression of Fibrotic Proteins in Primary Human Corneal Fibroblasts" Journal of Clinical Medicine 9, no. 11: 3572. https://doi.org/10.3390/jcm9113572
APA StyleKwok, S. S., Wong, F. S.-Y., Shih, K. C., Chan, Y.-K., Bu, Y., Chan, T. C.-Y., Ng, A. L.-K., Lo, A. C.-Y., Tong, L., Yam, G. H.-F., & Jhanji, V. (2020). Lycium barbarum Polysaccharide Suppresses Expression of Fibrotic Proteins in Primary Human Corneal Fibroblasts. Journal of Clinical Medicine, 9(11), 3572. https://doi.org/10.3390/jcm9113572





