Classical McIndoe Technique Versus the McIndoe Technique with a Neovaginal PACIENA Prosthesis® and No Skin Graft
Abstract
:1. Introduction
2. Experimental Section
2.1. Inclusion Criteria
- Women diagnosed with vaginal agenesis due to Rokitansky syndrome or Morris syndrome wishing to undergo neovaginal surgery using the McIndoe technique.
- Adults of legal age and minors with parental authorization.
- A signed informed consent form.
- Women diagnosed with vaginal agenesis who were operated on at San Juan University Hospital between 1992 and 2015 using the classical McIndoe technique.
2.2. Exclusion Criteria
- Women suffering from any medical pathology (metabolic disease, coagulopathy, cardiovascular disease, respiratory disease, Crohn’s disease, rectal disease) that contraindicates surgery or that may worsen the results of neovaginal surgery.
- Minors with no parental authorization.
- The existence of any previous reconstructive neovaginal surgery.
- Any other kind of neovaginal surgery undergone other than the McIndoe technique.
2.3. Research Plan and Procedures
2.4. Outcomes
- The age of the patient at the time of surgery.
- The age of the patient at the time of diagnosis.
- Occurrence of hemorrhage during surgery.
- Occurrence of other incidents during surgery.
- The length of time spent at the hospital.
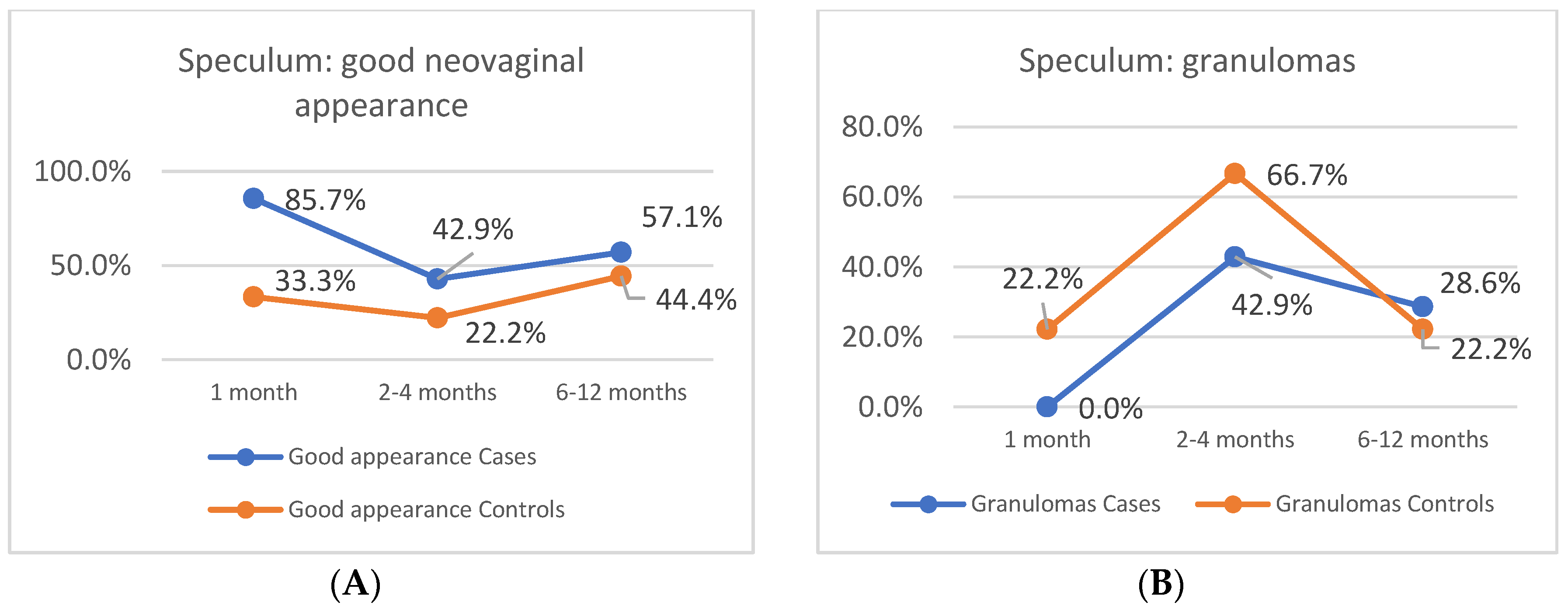
- The appearance of the neovagina in the speculum assessment (month 1, months 2–4, months 6–12).
- The patient’s symptoms in two periods (months 1–4, months 6–12).
- o
- Pain from the placement of the prosthesis.
- o
- Continuous pelvic pain.
- o
- Foul-smelling discharge.
- o
- Fever.
- Length of the neovagina at months 1–2.
- The need to change to a smaller maintenance dilator.
- Adequate epithelialization of the vagina.
- The time elapsed until beginning sexual relations.
- Satisfactory sexual relations (at month 4 and month 6).
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Relevance
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- ACOG Committee Opinion No. 728 Summary. Obstet. Gynecol. 2018, 131, 196–197. [CrossRef]
- McIndoe, A. The treatment of congenital absence and obliterative conditions of the vagina. Br. J. Plast. Surg. 1950, 2, 254–267. [Google Scholar] [PubMed]
- Acién, P.; Nohales-Alfonso, F.J.; Sánchez-Ferrer, M.-L.; Sánchez-Lozano, M.; Navarro-Lillo, V.; Acién, M. Clinical Pilot Study to Evaluate the Neovaginal PACIENA Prosthesis® for Vaginoplasty without Skin Grafts in Women with Vaginal Agenesis. BMC Women’s Health 2019, 19, 144. [Google Scholar] [CrossRef] [PubMed]
- Acién, P.; Acién, M.; Oliva-Meyer, M.-A.; Sánchez-Lozano, M.; Martínez-Garcia, J. McIndoe Operation without Skin Graft: A New Neovaginal Prosthesis of Polylactic Acid (PLA). BJMMR 2016, 18, 1–7. [Google Scholar] [CrossRef]
- Lin, W.C.; Chang, C.Y.; Shen, Y.Y.; Tsai, H.D. Use of Autologous Buccal Mucosa for Vaginoplasty: A Study of Eight Cases. Hum. Reprod. 2003, 18, 604–607. [Google Scholar] [CrossRef] [Green Version]
- van Leeuwen, K.; Baker, L.; Grimsby, G. Autologous Buccal Mucosa Graft for Primary and Secondary Reconstruction of Vaginal Anomalies. Semin. Pediatr. Surg. 2019, 28, 150843. [Google Scholar] [CrossRef]
- Hage, J.J.; Karim, R.B. Abdominoplastic Secondary Full-Thickness Skin Graft Vaginoplasty for Male-to-Female Transsexuals. Plast. Reconstr. Surg. 1998, 101, 1512–1515. [Google Scholar] [CrossRef]
- Motta, G.L.; Tavares, P.M.; da Silva, G.V.M.; Berger, M.; Silva Neto, B.; Rosito, T.E. Full-Thickness Skin Mesh Graft Vaginoplasty: A Skin Sparing Technique. Int. Braz. J. Urol. 2017, 43, 1193. [Google Scholar] [CrossRef] [Green Version]
- Gentileschi, S.; Pino, V.; Albanese, R.; Salgarello, M.; Scambia, G.; Ercoli, A. Simultaneous Correction of Breast Hypertrophy and Vaginal Agenesis: Aesthetic Surgery to the Aid of Reconstructive Surgery. J. Obstet. Gynaecol. Res. 2019, 45, 1398–1403. [Google Scholar] [CrossRef]
- Panici, P.B.; Bellati, F.; Boni, T.; Francescangeli, F.; Frati, L.; Marchese, C. Vaginoplasty Using Autologous in Vitro Cultured Vaginal Tissue in a Patient with Mayer-von-Rokitansky-Kuster-Hauser Syndrome. Hum. Reprod. 2007, 22, 2025–2028. [Google Scholar] [CrossRef] [Green Version]
- Panici, P.B.; Maffucci, D.; Ceccarelli, S.; Vescarelli, E.; Perniola, G.; Muzii, L.; Marchese, C. Autologous In Vitro Cultured Vaginal Tissue for Vaginoplasty in Women With Mayer-Rokitansky-Küster-Hauser Syndrome: Anatomic and Functional Results. J. Minim. Invasive Gynecol. 2015, 22, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Sabatucci, I.; Palaia, I.; Marchese, C.; Muzii, L.; Morte, C.D.; Giorgini, M.; Musella, A.; Ceccarelli, S.; Vescarelli, E.; Panici, P. Treatment of the Mayer–Rokitansky–Küster–Hauser Syndrome with Autologous in Vitro Cultured Vaginal Tissue: Descriptive Study of Long-term Results and Patient Outcomes. BJOG Int. J. Obstet. Gynaecol. 2018, 126, 123–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Qiu, J.; Ding, J.; Hua, K. Comparison of Neovaginoplasty Using Acellular Porcine Small Intestinal Submucosa Graft or Interceed in Patients with Mayer–Rokitansky–Küster–Hauser Syndrome. Arch. Gynecol. Obstet. 2019, 300, 1633–1636. [Google Scholar] [CrossRef] [PubMed]
- Jackson, N.D.; Rosenblatt, P.L. Use of Interceed Absorbable Adhesión Barrier for Vaginoplasty. Obstet. Gynecol. 1994, 84, 1048–1050. [Google Scholar] [PubMed]
- Motoyama, S.; Laoag-Fernandez, J.B.; Mochizuki, S.; Yamabe, S.; Maruo, T. Vaginoplasty with Interceed Absorbable Adhesion Barrier for Complete Squamous Epithelialization in Vaginal Agenesis. Am. J. Obstet. Gynecol. 2003, 188, 1260–1264. [Google Scholar] [CrossRef]
- Inagaki, M.; Motoyama, S.; Laoag-Fernandez, J.B.; Yasuda, R.; Maruo, T. Two Cases Reports of Less Invasive Surgery Using Interceed (Oxidized Regenerated Cellulose) Absorbable Adhesion Barrier for Vaginoplasty in Mayer-Rokitansky-Kuster-Hauser Syndrome. Int. Surg. 2009, 94, 48–53. [Google Scholar]
- Zhang, X.; Liu, Z.; Yang, Y.; Yao, Y.; Tao, Y. The Clinical Outcomes of Vaginoplasty Using Tissue-Engineered Biomaterial Mesh in Patients with Mayer-Rokitansky-Küster-Hauser Syndrome. Int. J. Surg. 2017, 44, 9–14. [Google Scholar] [CrossRef]
- Kamalakannan, J.; Murthy, V.; Kularashmi, B.S.; Jajoo, K. Customized Silicone Vaginal Stent. J. Obstet. Gynecol. India 2015, 65, 281–283. [Google Scholar] [CrossRef] [Green Version]
- Rathee, M.; Boora, P.; Kundu, R. Custom Fabricated Acrylic Vaginal Stent as an Adjunct to Surgical Creation of Neovagina for a Young Female with Isolated Vaginal Agenesis. J. Hum. Reprod. Sci. 2014, 7, 272. [Google Scholar] [CrossRef]
- Anagani, M.; Agrawal, P.; Meka, K.; Narayana, R.T.; Bandameedipally, R. Novel Minimally Invasive Technique of Neovaginoplasty Using an Absorbable Adhesion Barrier. J. Minim. Invasive Gynecol. 2020, 27, 206–211. [Google Scholar] [CrossRef]
- Farah, S.F.; Anderson, D.G.; Langer, R. Physical and Mechanical Properties of PLA, and Their Functions in Widespread Applications—A Comprehensive Review. Adv. Drug Deliv. Rev. 2016, 107, 367–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Callens, N.; De Cuypere, G.; Wolffenbuttel, K.P.; Beerendonk, C.C.M.; van der Zwan, Y.G.; van den Berg, M.; Monstrey, S.; Van Kuyk, M.E.; De Sutter, P.; Dessens, A.B.; et al. Long-Term Psychosexual and Anatomical Outcome after Vaginal Dilation or Vaginoplasty: A Comparative Study. J. Sex. Med. 2012, 9, 1842–1851. [Google Scholar] [CrossRef] [PubMed]
- ACOG Committee Opinion Number 274, July 2002. Nonsurgical Diagnosis and Management of Vaginal Agenesis. Obstet. Gynecol. 2002, 100, 213–216. [Google Scholar] [CrossRef]
- Bracaglia, R.; D’Ettorre, M.; Gentileschi, S.; Tambasco, D. Was the Surgeon a Satisfactory Informant? How to Minimize Room for Claims. Aesthet. Surg. J. 2014, 34, 632–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herlin, M.; Bay Bjørn, A.-M.; Jørgensen, L.K.; Trolle, B.; Petersen, M.B. Treatment of Vaginal Agenesis in Mayer-Rokitansky-Küster-Hauser Syndrome in Denmark: A Nationwide Comparative Study of Anatomical Outcome and Complications. Fertil. Steril. 2018, 110, 746–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Patient | Age at Diagnosis (Year) | Age at Surgery (Year) | Diagnosis | Duration (Minutes) | Time Spent in Hospital (Days) | Neovaginal Length (cm) |
|---|---|---|---|---|---|---|
| CASE 1 | 13 | 17 | Rokitansky | 85 | 5 | 9.0 |
| CASE 2 | 14 | 19 | Rokitansky | 90 | 14 | 8.0 |
| CASE 3 | 18 | 25 | Rokitansky | 80 | 2 | 10.0 |
| CASE 4 | 18 | 26 | Rokitansky | 80 | 2 | 11.0 |
| CASE 5 | 13 | 19 | Rokitansky | 90 | 3 | 9.0 |
| CASE 6 | 16 | 20 | Morris | 90 | 19 | 6.5 |
| CASE 7 | 16 | 21 | Rokitansky | 90 | 7 | 9.0 |
| CONTROL 1 | 15 | 16 | Rokitansky | 150 | 24 | 7.0 |
| CONTROL 2 | 17 | 18 | Rokitansky | 110 | 10 | 7.0 |
| CONTROL 3 | 16 | 20 | Rokitansky | 130 | 18 | 7.0 |
| CONTROL 4 | 16 | 25 | Rokitansky | 150 | 9 | 8.0 |
| CONTROL 5 | 16 | 19 | Rokitansky | 165 | 11 | 6.0 |
| CONTROL 6 | 16 | 21 | Rokitansky | 180 | 10 | 6.0 |
| CONTROL 7 | 16 | 18 | Rokitansky | 135 | 10 | 4.0 |
| CONTROL 8 | 17 | 17 | Rokitansky | 180 | 12 | 7.0 |
| CONTROL 9 | 14 | 14 | Rokitansky | 200 | 17 | 7.0 |
| Cases (n = 7) | Controls (n = 9) | |||
|---|---|---|---|---|
| Symptoms | 3–4 Months | 6–12 Months | 3–4 Months | 6–12 Months |
| None | 3 (42.9%) | 5 (71.4%) | 5 (55.5%) | 6 (66.7%) |
| Pain placement prothesis | 3 (42.9%) | 1 (14.3%) | 0 | 0 |
| Bleeding | 0 | 0 | 3 (33.3%) | 0 |
| Abdominal pain | 0 | 0 | 1 (11.1%) | 2 (22.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro, V.; Acién, M.I.; Acién, P. Classical McIndoe Technique Versus the McIndoe Technique with a Neovaginal PACIENA Prosthesis® and No Skin Graft. J. Clin. Med. 2020, 9, 3648. https://doi.org/10.3390/jcm9113648
Navarro V, Acién MI, Acién P. Classical McIndoe Technique Versus the McIndoe Technique with a Neovaginal PACIENA Prosthesis® and No Skin Graft. Journal of Clinical Medicine. 2020; 9(11):3648. https://doi.org/10.3390/jcm9113648
Chicago/Turabian StyleNavarro, Victoria, Maria Isabel Acién, and Pedro Acién. 2020. "Classical McIndoe Technique Versus the McIndoe Technique with a Neovaginal PACIENA Prosthesis® and No Skin Graft" Journal of Clinical Medicine 9, no. 11: 3648. https://doi.org/10.3390/jcm9113648
APA StyleNavarro, V., Acién, M. I., & Acién, P. (2020). Classical McIndoe Technique Versus the McIndoe Technique with a Neovaginal PACIENA Prosthesis® and No Skin Graft. Journal of Clinical Medicine, 9(11), 3648. https://doi.org/10.3390/jcm9113648





