The Impact of Overnight Orthokeratology on Accommodative Response in Myopic Subjects
Abstract
1. Introduction
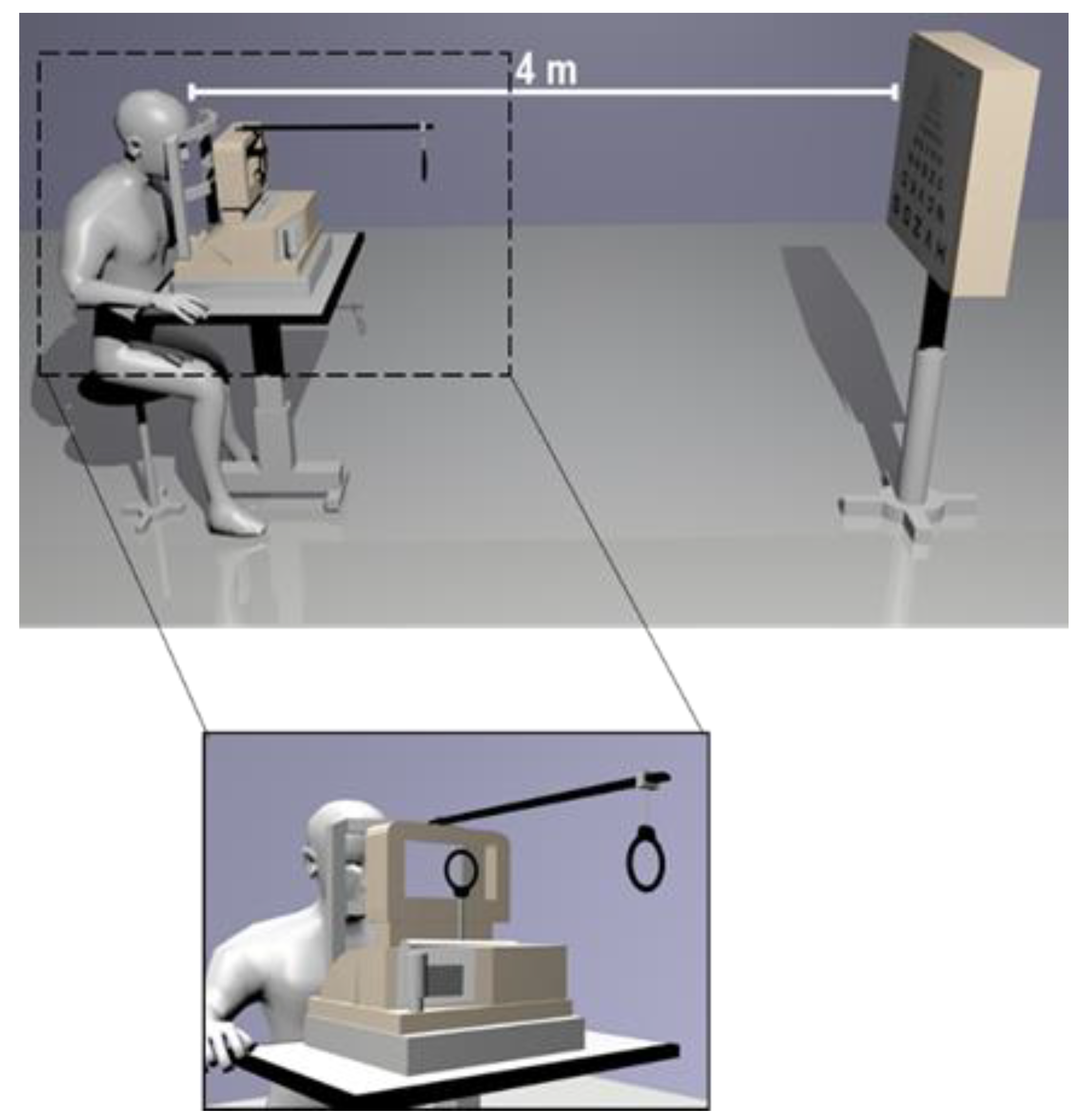
2. Material and Methods
2.1. Study Design
2.2. Subjects and Inclusion Criteria
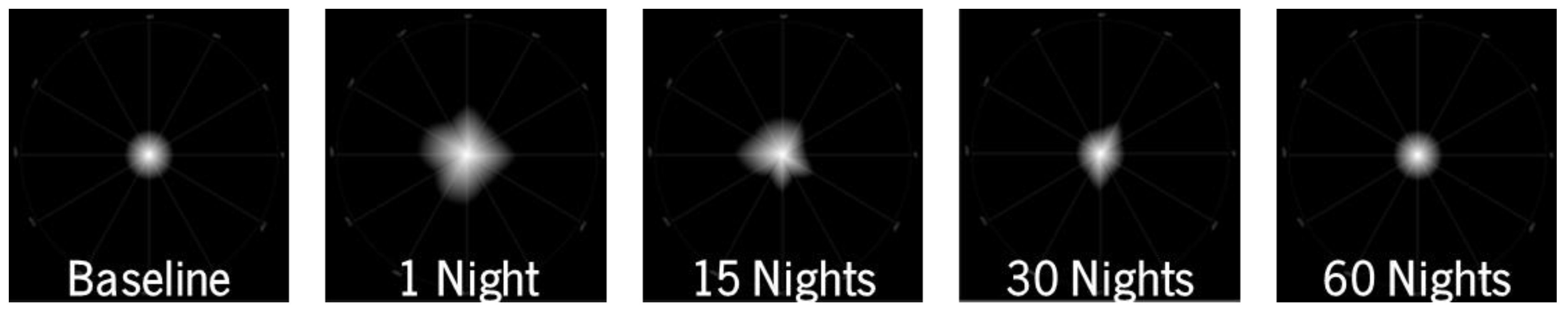
2.3. Measurements and Protocol
2.4. Contact Lens
2.5. Statistical Analysis
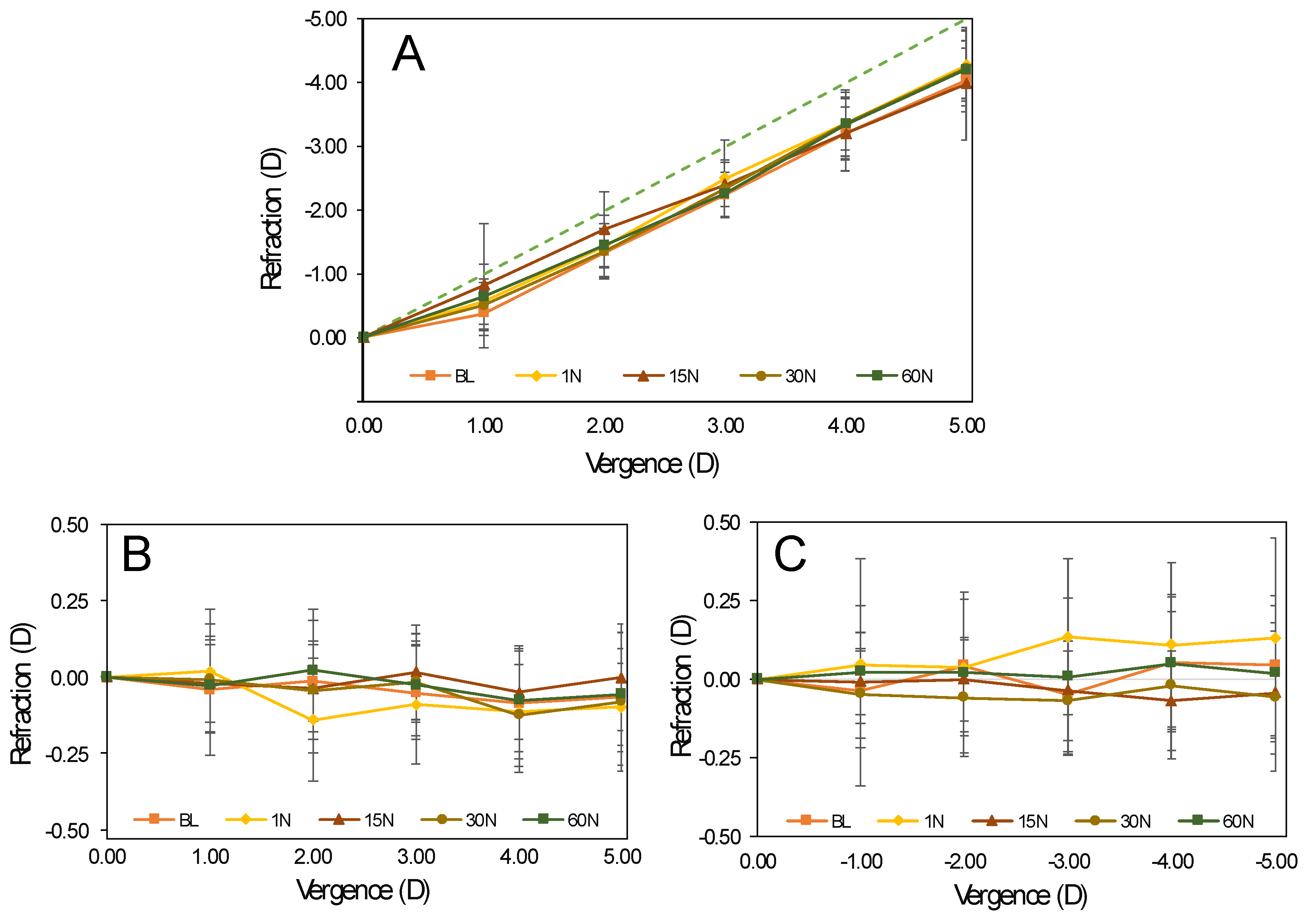
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Swarbrick, H.A. Orthokeratology review and update. Clin. Exp. Optom. 2006, 89, 124–143. [Google Scholar] [CrossRef] [PubMed]
- Mountford, J.; David, R.; Trusit, D. Orthokeratology: Principles and Practice, 1st ed.; Butterworth-Heinemann: Edinburgh, UK, 2004. [Google Scholar]
- Grzybowski, A.; Kanclerz, P.; Tsubota, K.; Lanca, C.; Saw, S.-M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020, 20, 27. [Google Scholar] [CrossRef] [PubMed]
- Vagge, A.; Desideri, L.F.; Nucci, P.; Serafino, M.; Giannaccare, G.; Traverso, C.E. Prevention of progression in myopia: A systematic review. Diseases 2018, 6, 92. [Google Scholar] [CrossRef] [PubMed]
- Si, J.-K.; Tang, K.; Bi, H.-S.; Bi, H.; Guo, J.-G.; Wang, X.-R. Orthokeratology for Myopia Control. Optom. Vis. Sci. 2015, 92, 252–257. [Google Scholar] [CrossRef] [PubMed]
- González-Méijome, J.M.; Peixoto-De-Matos, S.C.; Faria-Ribeiro, M.; Lopes-Ferreira, D.P.; Jorge, J.; Legerton, J.; Queiros, A. Strategies to regulate myopia progression with contact lenses. Eye Contact Lens. 2016, 42, 24–34. [Google Scholar] [CrossRef]
- Alharbi, A.; Swarbrick, H.A. The effects of overnight orthokeratology lens wear on corneal thickness. Investig. Opthalmol. Vis. Sci. 2003, 44, 2518–2523. [Google Scholar] [CrossRef]
- Queirós, A.; González-Méijome, J.M.; Villa-Collar, C.; Gutiérrez, A.R.; Jorge, J. Local steepening in peripheral corneal curvature after corneal refractive therapy and LASIK. Optom. Vis. Sci. 2010, 87, 432–439. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, J.-E. Influence of orthokeratology lens on axial length elongation and myopic progression in childhood myopia. Kosin Med. J. 2017, 32, 204–211. [Google Scholar] [CrossRef][Green Version]
- Sun, Y.; Xu, F.; Zhang, T.; Liu, M.; Wang, D.; Chen, Y.; Liu, Q. Orthokeratology to control myopia progression: A meta-analysis. PLoS ONE 2015, 10, e0124535. [Google Scholar] [CrossRef]
- Gwiazda, J.E.; Thorn, F.; Bauer, J.; Held, R. Myopic children show insufficient accommodative response to blur. Investig. Ophthalmol. Vis. Sci. 1993, 34, 690–694. [Google Scholar]
- Gwiazda, J.; Bauer, J.; Thorn, F.; Held, R. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vis. Res. 1995, 35, 1299–1304. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Hayes, J.R.; Jones, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K. Accommodative lag before and after the onset of myopia. Investig. Opthalmol. Vis. Sci. 2006, 47, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A.; Rosen, R. The possible role of peripheral refraction in development of myopia. Optom. Vis. Sci. 2016, 93, 1042–1044. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; Lopes-Ferreira, D.; González-Méijome, J.M. Astigmatic peripheral defocus with different contact lenses: Review and meta-analysis. Curr. Eye Res. 2016, 41, 1005–1015. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.M.; Radhakrishnan, H.; Price, H.; Rae, S.; Theagarayan, B.; Calver, R.I.; Sailoganathan, A.; Latham, K.; O’Leary, D.J. A randomized clinical trial to assess the effect of a dual treatment on myopia progression: The Cambridge Anti-Myopia Study. Ophthalmic Physiol. Opt. 2013, 33, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Faria-Ribeiro, M.; Navarro, R.; González-Méijome, J.M. Effect of pupil size on wavefront refraction during orthokeratology. Optom. Vis. Sci. 2016, 93, 1399–1408. [Google Scholar] [CrossRef]
- Faria-Ribeiro, M.; Belsue, R.N.; López-Gil, N.; González-Méijome, J.M. Morphology, topography, and optics of the orthokeratology cornea. J. Biomed. Opt. 2016, 21, 075011. [Google Scholar] [CrossRef]
- McLeod, A.D.L. Effects of Overnight Orthokeratology on Phoria, Vergence, and Accommodation in Children; New England College of Optometry: Boston, MA, USA, 2006. [Google Scholar]
- Brand, P. The effect of orthokeratology on accommodative and convergence function: A clinic-based pilot study. Optom. Vis. Perform. 2013, 1, 162–167. [Google Scholar]
- Felipe-Márquez, G.; Nombela-Palomo, M.; Cacho, I.; Nieto-Bona, A. Accommodative changes produced in response to overnight orthokeratology. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 253, 619–626. [Google Scholar] [CrossRef]
- Johnson, K.L.; Gifford, P.; Hendicott, P.L.; Schmid, K.L. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Contact Lens Anterior Eye 2017, 40, 184–189. [Google Scholar] [CrossRef]
- Queirós, A.; Fernandes, P.R.B.; Jorge, J.; Almeida, J.B.; Parafita, M.A.; González-Méijome, J.M. Non-contact tonometry synchronized with cardiac rhythm and its relationship with blood pressure. Ophthalmic Physiol. Opt. 2006, 26, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Neves, H.I.F.; Araújo, R.J.F.M.; Rico-Del-Viejo, L.; Silva, A.C.; Queirós, A.; González-Méijome, J.M. Validation of a method to measure light distortion surrounding a source of glare. J. Biomed. Opt. 2015, 20, 075002. [Google Scholar] [CrossRef] [PubMed]
- Brito, P.; Salgado-Borges, J.; Neves, H.; Gonzalez-Meijome, J.; Monteiro, M. Light-distortion analysis as a possible indicator of visual quality after refractive lens exchange with diffractive multifocal intraocular lenses. J. Cataract. Refract. Surg. 2015, 41, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Altoaimi, B.H.; Almutairi, M.S.; Kollbaum, P.S.; Bradley, A. Accommodative behavior of young eyes wearing multifocal contact lenses. Optom. Vis. Sci. 2018, 95, 416–427. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef]
- Queirós, A.; Amorim-De-Sousa, A.; Lopes-Ferreira, D.; Villa-Collar, C.; Gutiérrez Ángel, R.; González-Méijome, J.M. Relative peripheral refraction across 4 meridians after orthokeratology and LASIK surgery. Eye Vis. 2018, 5, 12. [Google Scholar] [CrossRef]
- Smith, E.L.; Hung, L.-F.; Huang, J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vis. Res. 2009, 49, 2386–2392. [Google Scholar] [CrossRef]
- Queirós, A.; González-Méijome, J.M.; Jorge, J.; Villa-Collar, C.; Gutiérrez Ángel, R. Peripheral refraction in myopic patients after orthokeratology. Optom. Vis. Sci. 2010, 87, 323–329. [Google Scholar] [CrossRef]
- Kang, P.; Swarbrick, H. Peripheral refraction in myopic children wearing orthokeratology and gas-permeable lenses. Optom. Vis. Sci. 2011, 88, 476–482. [Google Scholar] [CrossRef]
- Kang, P.; Gifford, P.; Swarbrick, H. Can manipulation of orthokeratology lens parameters modify peripheral refraction? Optom. Vis. Sci. 2013, 90, 1237–1248. [Google Scholar] [CrossRef]
- Kang, P.; Swarbrick, H.A. Time course of the effects of orthokeratology on peripheral refraction and corneal topography. Ophthalmic Physiol. Opt. 2013, 33, 277–282. [Google Scholar] [CrossRef] [PubMed]
- González-Méijome, J.M.; Faria-Ribeiro, M.; Lopes-Ferreira, D.; Fernandes, P.R.B.; Carracedo, G.; Queirós, A. Changes in peripheral refractive profile after orthokeratology for different degrees of myopia. Curr. Eye Res. 2015, 41, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kang, P.; Swarbrick, H. New perspective on myopia control with orthokeratology. Optom. Vis. Sci. 2016, 93, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Nichols, J.J.; Marsich, M.M.; Nguyen, M.; Barr, J.T.; Bullimore, M.A. Overnight orthokeratology. Optom. Vis. Sci. 2000, 77, 628–629. [Google Scholar] [CrossRef]
- Soni, P.S.; Nguyen, T.T.; Bonanno, J.A. Overnight orthokeratology: Visual and corneal changes. Eye Contact Lens 2003, 29, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Soni, P.S.; Nguyen, T.T.; Bonanno, J.A. Overnight orthokeratology: Refractive and corneal recovery after discontinuation of reverse-geometry lenses. Eye Contact Lens 2004, 30, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Walline, J.J.; Rah, M.J.; Jones, L.A. The Children’s Overnight Orthokeratology Investigation (COOKI) Pilot Study. Optom. Vis. Sci. 2004, 81, 407–413. [Google Scholar] [CrossRef][Green Version]
- Cheung, S.W.; Cho, P.; Chan, B. Astigmatic changes in orthokeratology. Optom. Vis. Sci. 2009, 86, 1352–1358. [Google Scholar] [CrossRef]
- Li, F.; Jiang, Z.-X.; Hao, P.; Li, X. A Meta-analysis of central corneal thickness changes with overnight orthokeratology. Eye Contact Lens 2016, 42, 141–146. [Google Scholar] [CrossRef]
- Berntsen, D.A.; Barr, J.T.; Mitchell, G.L. The effect of overnight contact lens corneal reshaping on higher-order aberrations and best-corrected visual acuity. Optom. Vis. Sci. 2005, 82, 490–497. [Google Scholar] [CrossRef]
- Johnson, K.L.; Carney, L.G.; Mountford, J.A.; Collins, M.J.; Cluff, S.; Collins, P.K. Visual performance after overnight orthokeratology. Contact Lens Anterior Eye 2007, 30, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, T.; Okamoto, C.; Ishii, Y.; Takahira, T.; Kakita, T.; Oshika, T. Mesopic contrast sensitivity and ocular higher-order aberrations after overnight orthokeratology. Am. J. Ophthalmol. 2008, 145, 645–655.e1. [Google Scholar] [CrossRef] [PubMed]
- Santolaria, E.; Cerviño, A.; Queirós, A.; Brautaset, R.; González-Méijome, J.M. Subjective satisfaction in long-term orthokeratology patients. Eye Contact Lens 2013, 39, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Santolaria-Sanz, E.; Cervino, A.; González-Méijome, J.M. Corneal aberrations, contrast sensitivity, and light distortion in orthokeratology patients: 1-year results. J. Ophthalmol. 2016, 2016, 8453462. [Google Scholar] [CrossRef] [PubMed]
- Kang, P.; Watt, K.; Chau, T.; Zhu, J.; Evans, B.J.; Swarbrick, H.A. The impact of orthokeratology lens wear on binocular vision and accommodation: A short-term prospective study. Contact Lens Anterior Eye 2018, 41, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Gifford, K.L.; Gifford, P.; Hendicott, P.L.; Schmid, K.L. Zone of clear single binocular vision in myopic orthokeratology. Eye Contact Lens 2020, 46, 82–90. [Google Scholar] [CrossRef]
- Han, X.; Xu, D.; Ge, W.; Wang, Z.; Li, X.; Liu, W. A comparison of the effects of orthokeratology lens, medical lens, and ordinary frame glasses on the accommodative response in myopic children. Eye Contact Lens 2018, 44, 268–271. [Google Scholar] [CrossRef]
- Gifford, P.; Li, M.; Lu, H.; Miu, J.; Panjaya, M.; Swarbrick, H.A. Corneal versus ocular aberrations after overnight orthokeratology. Optom. Vis. Sci. 2013, 90, 439–447. [Google Scholar] [CrossRef]
- Felipe-Márquez, G.; Nombela-Palomo, M.; Palomo-Álvarez, C.; Cacho, I.; Nieto-Bona, A. Binocular function changes produced in response to overnight orthokeratology. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 255, 179–188. [Google Scholar] [CrossRef]
- Batres, L.; Peruzzo, S.; Serramito, M.; Carracedo, G. Accommodation response and spherical aberration during orthokeratology. Graefes Arch. Clin. Exp. Ophthalmol. 2019, 258, 117–127. [Google Scholar] [CrossRef]
| M (D) | J0 (D) | J45 (D) | HCDVA | LCDVA | |
|---|---|---|---|---|---|
| BL | −0.33 ± 0.68 | 0.05 ± 0.22 | −0.02 ± 0.21 | −0.09 ± 0.08 | 0.08 ± 0.08 |
| 1 N | −0.52 ± 0.38 | 0.07 ± 0.18 | −0.03 ± 0.23 | 0.02 ± 0.11 | 0.25 ± 0.13 |
| 15 N | 0.02 ± 0.40 | 0.01 ± 0.15 | −0.06 ± 0.26 | −0.09 ± 0.10 | 0.11 ± 0.12 |
| 30 N | 0.00 ± 0.42 | −0.01 ± 0.19 | −0.07 ± 0.21 | −0.12 ± 0.08 | 0.09 ± 0.11 |
| 60 N | −0.05 ± 0.36 | −0.03 ± 0.15 | 0.01 ± 0.24 | −0.11 ± 0.11 | 0.15 ± 0.13 |
| p-values | <0.001+ | 0.390+ | 0.359+ | <0.001+ | 0.004+ |
| Post hoc test | 1 N–BL;1 N–15 N; 1 N–30 N; 1 N–60 N | x | x | 1 N–15 N; 1 N–30 N; 1 N–60 N | BL-1 N; 1 N–30 N |
| LDI (%) | BFCIrreg (mm) | BFCIrregSD (mm) | |
|---|---|---|---|
| BL | 10.50 ± 5.59 | 0.35 ± 0.25 | 3.24 ± 1.16 |
| 1 N | 11.31 ± 5.96 | 0.46 ± 0.33 | 3.27 ± 1.16 |
| 15 N | 9.57 ± 5.90 | 0.60 ± 0.82 | 3.52 ± 1.87 |
| 30 N | 9.79 ± 8.18 | 0.71 ± 1.37 | 2.86 ± 2.14 |
| 60 N | 10.51 ± 7.98 | 0.50 ± 0.68 | 3.23 ± 2.28 |
| p-values | 0.007+ | 0.821+ | 0.321+ |
| Post hoc test | 1 N–15 N; 1 N–30 N | x | x |
| BL | 1 N | 15 N | 30 N | 60 N | p-values | Post hoc test | ||
|---|---|---|---|---|---|---|---|---|
| 1.00 D | −0.39 ± 0.36 | −0.57 ± 0.37 | −0.82 ± 1.00 | −0.50 ± 0.37 | −0.64 ± 0.53 | 0.184+ | x | |
| 2.00 D | −1.34 ± 0.39 | −1.44 ± 0.51 | −1.70 ± 0.61 | −1.36 ± 0.44 | −1.46 ± 0.35 | 0.047+ | x | |
| M | 3.00 D | −2.24 ± 0.36 | −2.50 ± 0.62 | −2.41 ± 0.36 | −2.34 ± 0.47 | −2.26 ± 0.36 | 0.351+ | x |
| 4.00 D | −3.21 ± 0.43 | −3.35 ± 0.51 | −3.20 ± 0.59 | −3.35 ± 0.55 | −3.35 ± 0.42 | 0.721+ | x | |
| 5.00 D | −4.04 ± 0.51 | −4.28 ± 0.58 | −3.98 ± 0.91 | −4.23 ± 0.61 | −4.21 ±0.46 | 0.380+ | x | |
| 1.00 D | −0.04 ± 0.22 | 0.02 ± 0.21 | −0.02 ± 0.13 | −0.01 ± 0.15 | −0.03 ± 0.15 | 0.965+ | x | |
| 2.00 D | −0.01 ± 0.24 | −0.14 ± 0.21 | −0.04 ± 0.14 | −0.04 ± 0.17 | 0.02 ± 0.17 | 0.115+ | x | |
| J0 | 3.00D | −0.05 ± 0.16 | −0.09 ± 0.20 | 0.02 ± 0.16 | −0.02 ± 0.14 | −0.03 ± 0.17 | 0.278+ | x |
| 4.00 D | −0.09 ± 0.18 | −0.11 ± 0.20 | −0.05 ± 0.16 | −0.12 ± 0.17 | −0.08 ± 0.17 | 0.688+ | x | |
| 5.00 D | −0.07 ± 0.16 | −0.10 ± 0.15 | 0.00 ± 0.18 | −0.08 ± 0.23 | −0.06 ± 0.24 | 0.631+ | x | |
| 1.00 D | −0.06 ± 0.24 | 0.05 ± 0.19 | -0.01 ± 0.11 | −0.05 ± 0.14 | 0.02 ± 0.37 | 0.103+ | x | |
| 2.00 D | 0.04 ± 0.22 | 0.04 ± 0.22 | 0.00 ± 0.14 | −0.06 ± 0.19 | 0.02 ± 0.26 | 0.366+ | x | |
| J45 | 3.00 D | −0.05 ± 0.19 | 0.14 ± 0.26 | −0.04 ± 0.16 | −0.07 ± 0.16 | 0.01 ± 0.26 | 0.001+ | BL-1 N; 1 N–30 N |
| 4.00 D | 0.05 ± 0.22 | 0.11 ± 0.27 | −0.07 ± 0.16 | −0.02 ± 0.24 | 0.05 ± 0.22 | 0.021+ | 1 N–15 N | |
| 5.00 D | 0.04 ± 0.23 | 0.13 ± 0.33 | −0.07 ± 0.16 | −0.06 ± 0.24 | 0.02 ± 0.22 | 0.272+ | x |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira-da-Mota, A.F.; Costa, J.; Amorim-de-Sousa, A.; González-Méijome, J.M.; Queirós, A. The Impact of Overnight Orthokeratology on Accommodative Response in Myopic Subjects. J. Clin. Med. 2020, 9, 3687. https://doi.org/10.3390/jcm9113687
Pereira-da-Mota AF, Costa J, Amorim-de-Sousa A, González-Méijome JM, Queirós A. The Impact of Overnight Orthokeratology on Accommodative Response in Myopic Subjects. Journal of Clinical Medicine. 2020; 9(11):3687. https://doi.org/10.3390/jcm9113687
Chicago/Turabian StylePereira-da-Mota, Ana F., Jéssica Costa, Ana Amorim-de-Sousa, José M. González-Méijome, and António Queirós. 2020. "The Impact of Overnight Orthokeratology on Accommodative Response in Myopic Subjects" Journal of Clinical Medicine 9, no. 11: 3687. https://doi.org/10.3390/jcm9113687
APA StylePereira-da-Mota, A. F., Costa, J., Amorim-de-Sousa, A., González-Méijome, J. M., & Queirós, A. (2020). The Impact of Overnight Orthokeratology on Accommodative Response in Myopic Subjects. Journal of Clinical Medicine, 9(11), 3687. https://doi.org/10.3390/jcm9113687







