Transport of L-Arginine Related Cardiovascular Risk Markers
Abstract
:1. Introduction
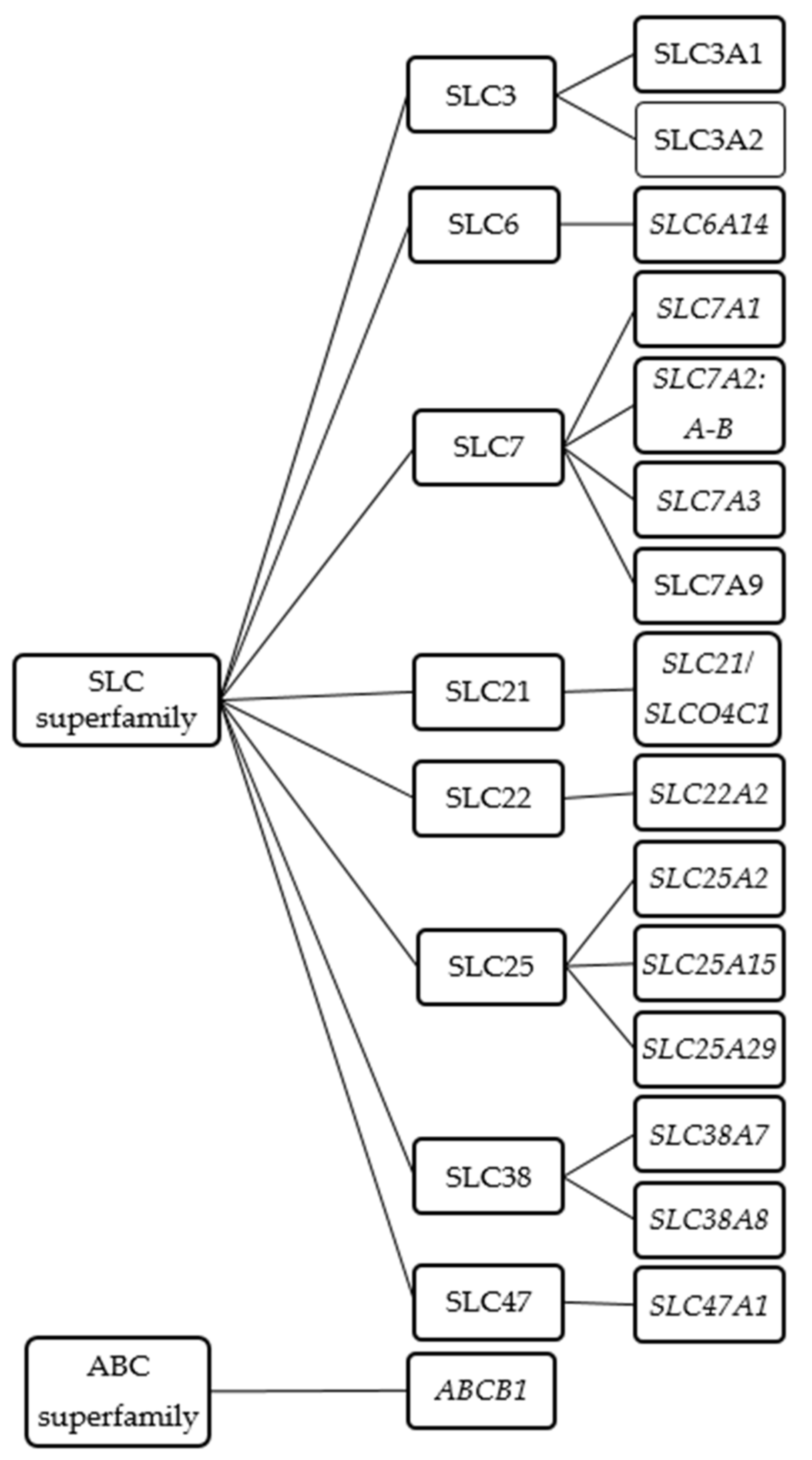
2. Transporter Families Shown to Transport L-Arginine and/or Its Derivatives
2.1. The Solute Carrier (SLC) Superfamily
2.1.1. SLC6 Family
SLC6A14 (ATB0,+)
2.1.2. SLC7 Family
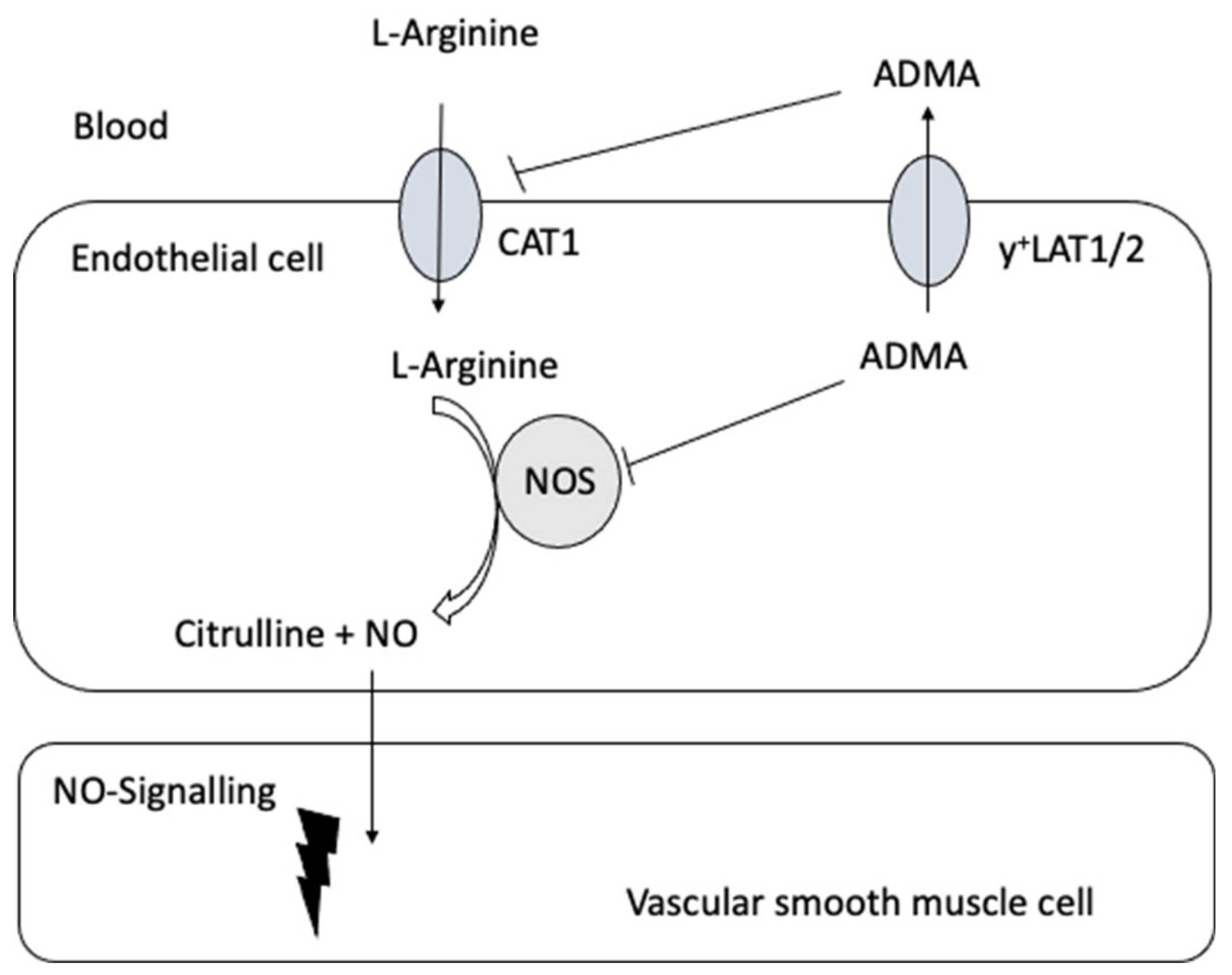
SLC7A1 (CAT1)
SLC7A2 (CAT2A and CAT2B)
SLC7A3 (CAT3)
SLC7A6 (y+LAT2) and SLC7A7 (y+LAT1)
SLC7A9-SLC3A1 (b0,+AT-rBAT)
2.1.3. SLCO/SLC21 Family
SLCO4C1 (OATP4C1)
2.1.4. SLC22 Family
SLC22A2 (OCT2)
2.1.5. SLC25 Family
SLC25A2 (ORNT2), SLC25A15 (ORNT1), and SLC25A29 (ORNT3)
2.1.6. SLC38 Family
SLC38A4 (SNAT4), SLC38A7 (SNAT7), and SLC38A8 (SNAT8)
2.1.7. The SLC47 Family
SLC47A1 (MATE1)
2.2. The Adenosine Triphosphate (ATP)-Binding Cassette (ABC) Superfamily
ABCB1/MDR1 (P-glycoprotein)
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases/ (accessed on 10 June 2020).
- Palmer, R.M.J.; Ashton, D.S.; Moncada, S. Vascular endothelial cells synthesize nitric oxide from L-arginine. Nat. Cell Biol. 1988, 333, 664–666. [Google Scholar] [CrossRef] [PubMed]
- Cooke, J.P. Does ADMA Cause Endothelial Dysfunction? Arter. Thromb. Vasc. Biol. 2000, 20, 2032–2037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gornik, H.L.; Creager, M.A. Arginine and Endothelial and Vascular Health. J. Nutr. 2004, 134, 2880S–2887S. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, N.W.; Mattson, D.L. Role of l-arginine in nitric oxide production in health and hypertension. Clin. Exp. Pharmacol. Physiol. 2009, 36, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Drexler, H.; Zeiher, A.; Meinzer, K.; Just, H. Correction of endothelial dysfunction in coronary microcirculation of hypercholesterolaemic patients by L-arginine. Lancet 1991, 338, 1546–1550. [Google Scholar] [CrossRef]
- Dong, J.-Y.; Qin, L.-Q.; Zhang, Z.; Zhao, Y.; Wang, J.; Arigoni, F.; Zhang, W. Effect of oral l-arginine supplementation on blood pressure: A meta-analysis of randomized, double-blind, placebo-controlled trials. Am. Heart J. 2011, 162, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.W.; Fernstrom, J.D.; Thompson, J.; Morris, S.M.; Kuller, L.H. Biochemical responses of healthy subjects during dietary supplementation with L-arginine. J. Nutr. Biochem. 2004, 15, 534–539. [Google Scholar] [CrossRef]
- Drover, J.W.; Dhaliwal, R.; Weitzel, L.; Wischmeyer, M.P.E.; Ochoa, J.B.; Heyland, D.K. Perioperative Use of Arginine-Supplemented Diets: A Systematic Review of the Evidence. J. Am. Coll. Surg. 2011, 212, 385–399. [Google Scholar] [CrossRef]
- Piatti, P.; Monti, L.D.; Valsecchi, G.; Magni, F.; Setola, E.; Marchesi, F.; Galli-Kienle, M.; Pozza, G.; Alberti, K.G.M. Long-Term Oral L-Arginine Administration Improves Peripheral and Hepatic Insulin Sensitivity in Type 2 Diabetic Patients. Diabetes Care 2001, 24, 875–880. [Google Scholar] [CrossRef] [Green Version]
- Bode-Böger, S.M.; Scalera, F.; Ignarro, L. The l-arginine paradox: Importance of the l-arginine/asymmetrical dimethylarginine ratio. Pharmacol. Ther. 2007, 114, 295–306. [Google Scholar] [CrossRef]
- Closs, E.I.; Scheld, J.S.; Sharafi, M.; Förstermann, U. Substrate supply for nitric-oxide synthase in macrophages and endothelial cells: Role of cationic amino acid transporters. Mol. Pharmacol. 2000, 57, 68–74. [Google Scholar] [PubMed]
- Simon, A.; Plies, L.; Habermeier, A.; Martiné, U.; Reining, M.; Closs, E.I. Role of Neutral Amino Acid Transport and Protein Breakdown for Substrate Supply of Nitric Oxide Synthase in Human Endothelial Cells. Circ. Res. 2003, 93, 813–820. [Google Scholar] [CrossRef] [Green Version]
- Shin, S.; Mohan, S.; Fung, H.-L. Intracellular l-arginine concentration does not determine NO production in endothelial cells: Implications on the “l-arginine paradox”. Biochem. Biophys. Res. Commun. 2011, 414, 660–663. [Google Scholar] [CrossRef] [Green Version]
- Atzler, D.; Schwedhelm, E.; Choe, C. L-Homoarginine and cardiovascular disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Böger, M.R.H. The emerging role of asymmetric dimethylarginine as a novel cardiovascular risk factor. Cardiovasc. Res. 2003, 59, 824–833. [Google Scholar] [CrossRef] [Green Version]
- Vallance, P.; Leone, A.; Calver, A.; Collier, J.; Moncada, S. Endogenous Dimethylarginine as an Inhibitor of Nitric Oxide Synthesis. J. Cardiovasc. Pharmacol. 1992, 20, S60–S62. [Google Scholar] [CrossRef]
- Goonasekera, C.D.; Rees, D.D.; Woolard, P.; Frend, A.; Shah, V.; Dillon, M.J. Nitric oxide synthase inhibitors and hypertension in children and adolescents. J. Hypertens. 1997, 15, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, H.; Itoh, S.; Kimoto, M.; Kohno, K.; Tamai, O.; Wada, Y.; Yasukawa, H.; Iwami, G.; Okuda, S.; Imaizumi, T. Asymmetrical Dimethylarginine, an Endogenous Nitric Oxide Synthase Inhibitor, in Experimental Hypertension. Hypertension 1997, 29, 242–247. [Google Scholar] [CrossRef] [Green Version]
- Fliser, D.; Kielstein, J.T.; Haller, H.; Bode-Böger, S.M. Asymmetric dimethylarginine: A cardiovascular risk factor in renal disease? Kidney Int. 2003, 63, S37–S40. [Google Scholar] [CrossRef] [Green Version]
- Ronden, R.A.; Houben, A.J.H.M.; Teerlink, T.; Bakker, J.A.; Bierau, J.; Stehouwer, C.D.A.; De Leeuw, P.W.; Kroon, A.A. Reduced renal plasma clearance does not explain increased plasma asymmetric dimethylarginine in hypertensive subjects with mild to moderate renal insufficiency. Am. J. Physiol. Physiol. 2012, 303, F149–F156. [Google Scholar] [CrossRef] [Green Version]
- Colonna, V.D.G.; Bianchi, M.; Pascale, V.; Ferrario, P.; Morelli, F.; Pascale, W.; Tomasoni, L.; Turiel, M. Asymmetric dimethylarginine (ADMA): An endogenous inhibitor of nitric oxide synthase and a novel cardiovascular risk molecule. Med Sci. Monit. 2009, 15, 91–101. [Google Scholar]
- Leiper, J.; Nandi, M.; Torondel, B.; Murray-Rust, J.; Malaki, M.; O’Hara, B.; Rossiter, S.; Anthony, S.; Madhani, M.; Selwood, D.; et al. Disruption of methylarginine metabolism impairs vascular homeostasis. Nat. Med. 2007, 13, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Kielstein, J.; Impraim, B.; Simmel, S.; Bode-Böger, S.M.; Tsikas, D.; Frölich, J.C.; Hoeper, M.M.; Haller, H.; Fliser, D. Cardiovascular Effects of Systemic Nitric Oxide Synthase Inhibition With Asymmetrical Dimethylarginine in Humans. Circulation 2004, 109, 172–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achan, V.; Broadhead, M.; Malaki, M.; Whitley, G.; Leiper, J.; MacAllister, R.; Vallance, P. Asymmetric Dimethylarginine Causes Hypertension and Cardiac Dysfunction in Humans and Is Actively Metabolized by Dimethylarginine Dimethylaminohydrolase. Arter. Thromb. Vasc. Biol. 2003, 23, 1455–1459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodionov, R.N.; Murry, D.J.; Vaulman, S.F.; Stevens, J.W.; Lentz, S.R. Human Alanine-Glyoxylate Aminotransferase 2 Lowers Asymmetric Dimethylarginine and Protects from Inhibition of Nitric Oxide Production. J. Biol. Chem. 2009, 285, 5385–5391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodionov, R.N.; Martens-Lobenhoffer, J.; Brilloff, S.; Burdin, D.V.; Jarzebska, N.; Demyanov, A.V.; Hohenstein, B.; Weiss, N.; Bode-Böger, S.M. Acetylation of asymmetric and symmetric dimethylarginine: An undercharacterized pathway of metabolism of endogenous methylarginines. Nephrol. Dial. Transplant. 2015, 31, 57–63. [Google Scholar] [CrossRef] [Green Version]
- Kielstein, J.T.; Fliser, D.; Veldink, H. Asymmetric Dimethylarginine and Symmetric Dimethylarginine: Axis of Evil or Useful Alliance? Semin. Dial. 2009, 22, 346–350. [Google Scholar] [CrossRef]
- Nijveldt, R.J.; Teerlink, T.; Siroen, M.P.; van Lambalgen, A.A.; Rauwerda, J.A.; van Leeuwen, P.A. The liver is an important organ in the metabolism of asymmetrical dimethylarginine (ADMA). Clin. Nutr. 2003, 22, 17–22. [Google Scholar] [CrossRef]
- Schlesinger, S.; Sonntag, S.R.; Lieb, W.; Maas, R. Asymmetric and Symmetric Dimethylarginine as Risk Markers for Total Mortality and Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Studies. PLoS ONE 2016, 11, e0165811. [Google Scholar] [CrossRef]
- Choe, C.; Atzler, D.; Wild, P.S.; Carter, A.M.; Böger, R.H.; Ojeda, F.; Simova, O.; Stockebrand, M.; Lackner, K.; Nabuurs, C.; et al. Homoarginine Levels Are Regulated by l -Arginine:Glycine Amidinotransferase and Affect Stroke Outcome. Circulation 2013, 128, 1451–1461. [Google Scholar] [CrossRef] [Green Version]
- Pilz, S.; Meinitzer, A.; Gaksch, M.; Grübler, M.; Verheyen, N.; Drechsler, C.; Hartaigh, B.Ó.; Lang, F.; Alesutan, I.; Voelkl, J.; et al. Homoarginine in the renal and cardiovascular systems. Amino Acids 2015, 47, 1703–1713. [Google Scholar] [CrossRef] [PubMed]
- März, W.; Meinitzer, A.; Drechsler, C.; Pilz, S.; Krane, V.; Kleber, M.E.; Fischer, J.; Winkelmann, B.R.; Böhm, B.O.; Ritz, E.; et al. Homoarginine, Cardiovascular Risk, and Mortality. Circulation 2010, 122, 967–975. [Google Scholar] [CrossRef]
- Moali, C.; Boucher, J.-L.; Sari, M.-A.; Stuehr, A.D.J.; Mansuy, D. Substrate Specificity of NO Synthases: Detailed Comparison ofl-Arginine, Homo-l-arginine, TheirNω-Hydroxy Derivatives, andNω-Hydroxynor-l-arginine. Biochemistry 1998, 37, 10453–10460. [Google Scholar] [CrossRef] [PubMed]
- Hrabák, A.; Bajor, T.; Temesi, A. Comparison of Substrate and Inhibitor Specificity of Arginase and Nitricm Oxide (NO) Synthase for Arginine Analogs and Related Compounds in Murine and Rat Macrophages. Biochem. Biophys. Res. Commun. 1994, 198, 206–212. [Google Scholar] [CrossRef]
- Brӧer, S. The SLC6 orphans are forming a family of amino acid transporters. Neurochem. Int. 2006, 48, 559–567. [Google Scholar] [CrossRef]
- Nelson, N. The Family of Na+/Cl− Neurotransmitter Transporters. J. Neurochem. 2002, 71, 1785–1803. [Google Scholar] [CrossRef] [Green Version]
- Kekuda, R.; Torres-Zamorano, V.; Fei, Y.-J.; Prasad, P.D.; Li, H.W.; Mader, L.D.; Leibach, F.H.; Ganapathy, V. Molecular and functional characterization of intestinal Na(+)-dependent neutral amino acid transporter B0. Am. J. Physiol. Content 1997, 272, G1463–G1472. [Google Scholar] [CrossRef]
- Sloan, J.L.; Mager, S. Cloning and Functional Expression of a Human Na+and Cl−-dependent Neutral and Cationic Amino Acid Transporter B0+. J. Biol. Chem. 1999, 274, 23740–23745. [Google Scholar] [CrossRef] [Green Version]
- Kekuda, R.; Prasad, P.D.; Fei, Y.-J.; Torres-Zamorano, V.; Sinha, S.; Yang-Feng, T.L.; Leibach, F.H.; Ganapathy, V. Cloning of the Sodium-dependent, Broad-scope, Neutral Amino Acid Transporter Bofrom a Human Placental Choriocarcinoma Cell Line. J. Biol. Chem. 1996, 271, 18657–18661. [Google Scholar] [CrossRef] [Green Version]
- Sun, L.; Rommens, J.M.; Corvol, H.; Li, W.; Li, X.; A Chiang, T.; Lin, F.; Dorfman, R.; Busson, P.-F.; Parekh, R.V.; et al. Multiple apical plasma membrane constituents are associated with susceptibility to meconium ileus in individuals with cystic fibrosis. Nat. Genet. 2012, 44, 562–569. [Google Scholar] [CrossRef]
- Doyle, F.A.; McGivan, J.D. The bovine renal epithelial cell line NBL-1 expresses a broad specificity Na+-dependent neutral amino acid transport system (System B°) similar to that in bovine renal brush border membrane vesicles. Biochim. Biophys. Acta Biomembr. 1992, 1104, 55–62. [Google Scholar] [CrossRef]
- Uchiyama, T.; Fujita, T.; Gukasyan, H.J.; Kim, K.-J.; Borok, Z.; Crandall, E.D.; Lee, V.H.L. Functional characterization and cloning of amino acid transporter B0,+ (ATB0,+) in primary cultured rat pneumocytes. J. Cell. Physiol. 2007, 214, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Palacín, M.; Estévez, R.; Bertran, J.; Zorzano, A. Molecular Biology of Mammalian Plasma Membrane Amino Acid Transporters. Physiol. Rev. 1998, 78, 969–1054. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, V.; Ganapathy, M.E.; Leibach, F.H. Intestinal transport of peptides and amino acids. In Current Topics in Membranes; Elsevier: Amsterdam, The Netherlands, 2000; Volume 50, pp. 379–412. [Google Scholar]
- Suviolahti, E.; Oksanen, L.J.; Öhman, M.; Cantor, R.M.; Ridderstråle, M.; Tuomi, T.; Kaprio, J.; Rissanen, A.; Mustajoki, P.; Jousilahti, P.; et al. The SLC6A14 gene shows evidence of association with obesity. J. Clin. Investig. 2003, 112, 1762–1772. [Google Scholar] [CrossRef]
- Gupta, N.; Miyauchi, S.; Martindale, R.G.; Herdman, A.V.; Podolsky, R.; Miyake, K.; Mager, S.; Prasad, P.D.; Ganapathy, M.E.; Ganapathy, V. Upregulation of the amino acid transporter ATB0,+ (SLC6A14) in colorectal cancer and metastasis in humans. Biochim. Biophys. Acta Mol. Basis Dis. 2005, 1741, 215–223. [Google Scholar] [CrossRef] [Green Version]
- Gupta, N.; Prasad, P.D.; Ghamande, S.; Moore-Martin, P.; Herdman, A.V.; Martindale, R.G.; Podolsky, R.; Mager, S.; Ganapathy, M.E.; Ganapathy, V. Up-regulation of the amino acid transporter ATB0,+ (SLC6A14) in carcinoma of the cervix. Gynecol. Oncol. 2006, 100, 8–13. [Google Scholar] [CrossRef]
- Yanai, H.; Ben-Shachar, S.; Baram, L.; Elad, H.; Gitstein, G.; Brazowski, E.; Tulchinsky, H.; Pasmanik-Chor, M.; Dotan, I. Gene expression alterations in ulcerative colitis patients after restorative proctocolectomy extend to the small bowel proximal to the pouch. Gut 2015, 64, 756–764. [Google Scholar] [CrossRef]
- Karunakaran, S.; Umapathy, N.S.; Thangaraju, M.; Hatanaka, T.; Itagaki, S.; Munn, D.H.; Prasad, P.D.; Ganapathy, V. Interaction of tryptophan derivatives with SLC6A14 (ATB0,+) reveals the potential of the transporter as a drug target for cancer chemotherapy. Biochem. J. 2008, 414, 343–355. [Google Scholar] [CrossRef]
- Corvol, H.; Blackman, S.M.; Boëlle, P.-Y.; Gallins, P.J.; Pace, R.G.; Stonebraker, J.R.; Accurso, F.J.; Clement, A.; Collaco, J.M.; Dang, H.; et al. Genome-wide association meta-analysis identifies five modifier loci of lung disease severity in cystic fibrosis. Nat. Commun. 2015, 6, 8382. [Google Scholar] [CrossRef] [Green Version]
- Di Paola, M.; Park, A.J.; Ahmadi, S.; Roach, E.J.; Wu, Y.-S.; Struder-Kypke, M.; Lam, J.S.; Bear, C.E.; Khursigara, C.M. SLC6A14Is a Genetic Modifier of Cystic Fibrosis That RegulatesPseudomonas aeruginosaAttachment to Human Bronchial Epithelial Cells. mBio 2017, 8, e02073-17. [Google Scholar] [CrossRef] [Green Version]
- Gutiérrez, M.L.; Corchete-Sánchez, L.; Teodósio, C.; Sarasquete, M.-E.; Abad, M.D.M.; Iglesias, M.; Esteban, C.; Sayagués, J.M.; Orfao, A.; Muñoz-Bellvís, L. Identification and characterization of the gene expression profiles for protein coding and non-coding RNAs of pancreatic ductal adenocarcinomas. Oncotarget 2015, 6, 19070–19086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babu, E.; Bhutia, Y.D.; Ramachandran, S.; Gnanaprakasam, J.P.; Prasad, P.D.; Thangaraju, M.; Ganapathy, V. Deletion of the amino acid transporter Slc6a14 suppresses tumour growth in spontaneous mouse models of breast cancer. Biochem. J. 2015, 469, 17–23. [Google Scholar] [CrossRef]
- Closs, E.I.; Wagner, C.A.; Palacin, M.; Endou, H.; Kanai, Y. CATs and HATs: The SLC7 family of amino acid transporters. Pflügers Archiv. Eur. J. Physiol. 2004, 447, 532–542. [Google Scholar] [CrossRef] [Green Version]
- Fotiadis, D.; Kanai, Y.; Palacín, M. The SLC3 and SLC7 families of amino acid transporters. Mol. Asp. Med. 2013, 34, 139–158. [Google Scholar] [CrossRef] [PubMed]
- White, M.F.; Christensen, H.N. Cationic amino acid transport into cultured animal cells. II. Transport system barely perceptible in ordinary hepatocytes, but active in hepatoma cell lines. J. Biol. Chem. 1982, 257, 4450–4457. [Google Scholar] [PubMed]
- I Closs, E.; Gräf, P. Cationic amino acid transporters (CATs). Targets for the manipulation of NO-synthase activity? Pharm. Biotechnol. 1999, 12, 229–249. [Google Scholar]
- Kavanaugh, M.P. Voltage dependence of facilitated arginine flux mediated by the system y+ basic amino acid transporter. Biochemistry 1993, 32, 5781–5785. [Google Scholar] [CrossRef]
- Albritton, L.M.; Kim, J.W.; Tseng, L.; Cunningham, J.M. Envelope-binding domain in the cationic amino acid transporter determines the host range of ecotropic murine retroviruses. J. Virol. 1993, 67, 2091–2096. [Google Scholar] [CrossRef] [Green Version]
- Closs, E.I.; Boissel, J.-P.; Habermeier, A.; Rotmann, A. Structure and Function of Cationic Amino Acid Transporters (CATs). J. Membr. Biol. 2006, 213, 67–77. [Google Scholar] [CrossRef]
- Devés, R.; Boyd, C.A.R. Transporters for Cationic Amino Acids in Animal Cells: Discovery, Structure, and Function. Physiol. Rev. 1998, 78, 487–545. [Google Scholar] [CrossRef]
- Hatzoglou, M.; Fernandez, J.; Yaman, I.; Closs, E. Regulation of catonic amino acid transport: The story of the CAT-1 transporter. Annu. Rev. Nutr. 2004, 24, 377–399. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Closs, E.I.; Albritton, L.M.; Cunningham, J.M. Transport of cationic amino acids by the mouse ecotropic retrovirus receptor. Nat. Cell Biol. 1991, 352, 725–728. [Google Scholar] [CrossRef] [PubMed]
- Vanoaica, L.; Behera, A.; Camargo, S.M.; Forster, I.C.; Verrey, F. Real-time functional characterization of cationic amino acid transporters using a new FRET sensor. Pflügers Archiv Eur. J. Physiol. 2015, 468, 563–572. [Google Scholar] [CrossRef]
- Closs, E.I. CATs, a family of three distinct mammalian cationic amino acid transporters. Amino Acids 1996, 11, 193–208. [Google Scholar] [PubMed]
- Closs, E.I.; Simon, A.; Vékony, N.; Rotmann, A. Plasma Membrane Transporters for Arginine. J. Nutr. 2004, 134, 2752S–2759S. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.; Pacitti, A.J.; Souba, W.W. Characterization of L-arginine transport by pulmonary artery endothelial cells. Am. J. Physiol. Cell. Mol. Physiol. 1993, 264, L351–L356. [Google Scholar] [CrossRef] [PubMed]
- McDonald, K.K.; I Zharikov, S.; Block, E.R.; Kilberg, M.S. A Caveolar Complex between the Cationic Amino Acid Transporter 1 and Endothelial Nitric-oxide Synthase May Explain the “Arginine Paradox”. J. Biol. Chem. 1997, 272, 31213–31216. [Google Scholar] [CrossRef] [Green Version]
- Closs, E.I.; Basha, F.Z.; Habermeier, A.; Förstermann, U. Interference ofL-Arginine Analogues withL-Arginine Transport Mediated by the y+Carrier hCAT-2B. Nitric Oxide 1997, 1, 65–73. [Google Scholar] [CrossRef]
- Strobel, J.; Mieth, M.; Endreß, B.; Auge, D.; König, J.; Fromm, M.F.; Maas, R. Interaction of the cardiovascular risk marker asymmetric dimethylarginine (ADMA) with the human cationic amino acid transporter 1 (CAT1). J. Mol. Cell. Cardiol. 2012, 53, 392–400. [Google Scholar] [CrossRef]
- Closs, E.I.; Gräf, P.; Habermeier, A.; Cunningham, J.M.; Förstermann, U. Human Cationic Amino Acid Transporters hCAT-1, hCAT-2A, and hCAT-2B: Three Related Carriers with Distinct Transport Properties. Biochemistry 1997, 36, 6462–6468. [Google Scholar] [CrossRef]
- Chafai, A.; Fromm, M.F.; König, J.; Maas, R. The prognostic biomarker L-homoarginine is a substrate of the cationic amino acid transporters CAT1, CAT2A and CAT2B. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lüneburg, N.; Xanthakis, V.; Schwedhelm, E.; Sullivan, L.M.; Maas, R.; Anderssohn, M.; Riederer, U.; Glazer, N.L.; Vasan, R.S.; Böger, R.H. Reference Intervals for Plasma L-Arginine and the L-Arginine:Asymmetric Dimethylarginine Ratio in the Framingham Offspring Cohort. J. Nutr. 2011, 141, 2186–2190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Möller, P.; Alvestrand, A.; Bergström, J.; Fürst, P.; Hellström, K. Electrolytes and Free Amino Acids in Leg Skeletal Muscle of Young and Elderly Women. Gerontology 1983, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Moller, P.; Bergström, J.; Eriksson, S.; Fürst, P.; Hellström, K. Effect of Aging on Free Amino Acids and Electrolytes in Leg Skeletal Muscle. Clin. Sci. 1979, 56, 427–432. [Google Scholar] [CrossRef] [Green Version]
- Atzler, D.; Schwedhelm, E.; Nauck, M.; Ittermann, T.; Böger, R.H.; Friedrich, N. Serum reference intervals of homoarginine, ADMA, and SDMA in the Study of Health in Pomerania. Clin. Chem. Lab. Med. 2014, 52, 1835–1842. [Google Scholar] [CrossRef]
- Atzler, D.; Mieth, M.; Maas, R.; Böger, R.H.; Schwedhelm, E. Stable isotope dilution assay for liquid chromatography-tandem mass spectrometric determination of l-homoarginine in human plasma. J. Chromatogr. B 2011, 879, 2294–2298. [Google Scholar] [CrossRef]
- Jaźwińska-Kozuba, A.; Martens-Lobenhoffer, J.; Kruszelnicka, O.; Rycaj, J.; Chyrchel, B.; Surdacki, A.; Bode-Böger, S.M. Opposite Associations of Plasma Homoarginine and Ornithine with Arginine in Healthy Children and Adolescents. Int. J. Mol. Sci. 2013, 14, 21819–21832. [Google Scholar] [CrossRef] [Green Version]
- Kayacelebi, A.A.; Beckmann, B.; Gutzki, F.-M.; Jordan, J.; Tsikas, D. GC–MS and GC–MS/MS measurement of the cardiovascular risk factor homoarginine in biological samples. Amino Acids 2014, 46, 2205–2217. [Google Scholar] [CrossRef]
- May, M.; Kayacelebi, A.A.; Batkai, S.; Jordan, J.; Tsikas, D.; Engeli, S. Plasma and tissue homoarginine concentrations in healthy and obese humans. Amino Acids 2015, 47, 1847–1852. [Google Scholar] [CrossRef]
- Böger, R.H. The pharmacodynamics of L-arginine. Altern. Ther. Heal. Med. 2014, 20, 48–54. [Google Scholar] [CrossRef]
- Wu, G.; Morris, J.S.M. Arginine metabolism: Nitric oxide and beyond. Biochem. J. 1998, 336, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Castillo, L.; Ajami, A.; Branch, S.; Chapman, T.; Yu, Y.-M.; Burke, J.; Young, V. Plasma arginine kinetics in adult man: Response to an arginine-free diet. Metabolism 1994, 43, 114–122. [Google Scholar] [CrossRef]
- Anthony, S.; Leiper, J.; Vallance, P. Endogenous production of nitric oxide synthase inhibitors. Vasc. Med. 2005, 10, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Päivä, H.; Lehtimäki, T.; Laakso, J.; Ruokonen, I.; Tervonen, R.; Metso, S.; Nikkilä, M.; Wuolijoki, E.; Laaksonen, R. Dietary composition as a determinant of plasma asymmetric dimethylarginine in subjects with mild hypercholesterolemia. Metabolism 2004, 53, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.; Che, D.; Qin, G.; Farouk, M.H.; Hailong, J.; Rui, H. Novel Biosynthesis, Metabolism and Physiological Functions of L-Homoarginine. Curr. Protein Pept. Sci. 2018, 20, 184–193. [Google Scholar] [CrossRef]
- Kayacelebi, A.A.; Langen, J.; Weigt-Usinger, K.; Chobanyan-Jürgens, K.; Mariotti, F.; Schneider, J.Y.; Rothmann, S.; Frölich, J.C.; Atzler, R.; Choe, C.; et al. Biosynthesis of homoarginine (hArg) and asymmetric dimethylarginine (ADMA) from acutely and chronically administered free l-arginine in humans. Amino Acids 2015, 47, 1893–1908. [Google Scholar] [CrossRef]
- Morris, S.M. Arginine Metabolism Revisited. J. Nutr. 2016, 146, 2579S–2586S. [Google Scholar] [CrossRef]
- Xuan, C.; Xu, L.-Q.; Tian, Q.-W.; Li, H.; Wang, Q.; He, G.-W.; Lun, L.-M. Dimethylarginine Dimethylaminohydrolase 2 (DDAH 2) Gene Polymorphism, Asymmetric Dimethylarginine (ADMA) Concentrations, and Risk of Coronary Artery Disease: A Case-Control Study. Sci. Rep. 2016, 6, 33934. [Google Scholar] [CrossRef]
- Kakimoto, Y.; Akazawa, S. Isolation and identification of N-G,N-G- and N-G,N’-G-dimethyl-arginine, N-epsilon-mono-, di-, and trimethyllysine, and glucosylgalactosyl- and galactosyl-delta-hydroxylysine from human urine. J. Biol. Chem. 1970, 245, 5751–5758. [Google Scholar]
- Seppälä, I.; Kleber, M.E.; Lyytikäinen, L.-P.; Hernesniemi, J.; Mäkelä, K.-M.; Oksala, N.; Laaksonen, R.; Pilz, S.; Tomaschitz, A.; Silbernagel, G.; et al. Genome-wide association study on dimethylarginines reveals novel AGXT2 variants associated with heart rate variability but not with overall mortality. Eur. Heart J. 2013, 35, 524–531. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, T.; Kimoto, M.; Watanabe, H.; Sasaoka, K. Metabolism of NG,NG- and NG,NG-dimethylarginine in rats. Arch. Biochem. Biophys. 1987, 252, 526–537. [Google Scholar] [CrossRef]
- Rodionov, R.N.; Oppici, E.; Martens-Lobenhoffer, J.; Jarzebska, N.; Brilloff, S.; Burdin, D.; Demyanov, A.; Kolouschek, A.; Leiper, J.; Maas, R.; et al. A Novel Pathway for Metabolism of the Cardiovascular Risk Factor Homoarginine by alanine:glyoxylate aminotransferase 2. Sci. Rep. 2016, 6, 35277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bollenbach, A.; Cordts, K.; Hanff, E.; Atzler, R.; Choe, C.-U.; Schwedhelm, E.; Tsikas, D. Evidence by GC-MS that lysine is an arginase-catalyzed metabolite of homoarginine in vitro and in vivo in humans. Anal. Biochem. 2019, 577, 59–66. [Google Scholar] [CrossRef]
- Brosnan, M.E.; Brosnan, J.T. Renal Arginine Metabolism. J. Nutr. 2004, 134, 2791S–2795S. [Google Scholar] [CrossRef] [Green Version]
- Tizianello, A.; De Ferrari, G.; Garibotto, G.; Gurreri, G.; Robaudo, C. Renal metabolism of amino acids and ammonia in subjects with normal renal function and in patients with chronic renal insufficiency. J. Clin. Investig. 1980, 65, 1162–1173. [Google Scholar] [CrossRef]
- Van De Poll, M.C.G.; Soeters, P.B.; Deutz, N.E.P.; Fearon, K.C.H.; DeJong, C.H.C. Renal metabolism of amino acids: Its role in interorgan amino acid exchange. Am. J. Clin. Nutr. 2004, 79, 185–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doolan, P.D.; Harper, H.A.; Hutchin, M.E.; Shreeve, W.W. Renal Clearance of Eighteen Individual Amino Acids in Human Subjects 1. J. Clin. Investig. 1955, 34, 1247–1255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, B.D.; Cameron, J.S. Homoarginine in Cystinuria. Clin. Sci. Mol. Med. 1974, 46, 173–182. [Google Scholar] [CrossRef]
- Torremans, A.; Marescau, B.; Vanholder, R.; De Smet, R.; Billiouw, J.-M.; De Deyn, P.P. The low nanomolar levels of N G -monomethylarginine in serum and urine of patients with chronic renal insufficiency are not significantly different from control levels. Amino Acids 2003, 24, 375–381. [Google Scholar] [CrossRef]
- Frenay, A.-R.S.; Kayacelebi, A.A.; Beckmann, B.; Soedamah-Muhtu, S.S.; De Borst, M.H.; Berg, E.V.D.; Van Goor, H.; Bakker, S.J.L.; Tsikas, D. High urinary homoarginine excretion is associated with low rates of all-cause mortality and graft failure in renal transplant recipients. Amino Acids 2015, 47, 1827–1836. [Google Scholar] [CrossRef]
- Jacobi, J.; Tsao, P.S. Asymmetrical dimethylarginine in renal disease: Limits of variation or variation limits? A systematic review. Am. J. Nephrol. 2007, 28, 224–237. [Google Scholar] [CrossRef] [Green Version]
- Drechsler, C.; Kollerits, B.; Meinitzer, A.; März, W.; Ritz, E.; König, P.; Neyer, U.; Pilz, S.; Wanner, C.; Kronenberg, F.; et al. Homoarginine and Progression of Chronic Kidney Disease: Results from the Mild to Moderate Kidney Disease Study. PLoS ONE 2013, 8, e63560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, W.H.W.; Wang, Z.; Cho, L.; Brennan, D.M.; Hazen, S.L. Diminished Global Arginine Bioavailability and Increased Arginine Catabolism as Metabolic Profile of Increased Cardiovascular Risk. J. Am. Coll. Cardiol. 2009, 53, 2061–2067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamada, Y.; Nagaretani, H.; Tamura, S.; Ohama, T.; Maruyama, T.; Hiraoka, H.; Yamashita, S.; Yamada, A.; Kiso, S.; Inui, Y.; et al. Vascular endothelial dysfunction resulting from l-arginine deficiency in a patient with lysinuric protein intolerance. J. Clin. Investig. 2001, 108, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Atzler, D.; Gore, M.O.; Ayers, C.R.; Choe, C.-U.; Böger, R.H.; De Lemos, J.A.; McGuire, D.K.; Schwedhelm, E. Homoarginine and Cardiovascular Outcome in the Population-Based Dallas Heart Study. Arter. Thromb. Vasc. Biol. 2014, 34, 2501–2507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pilz, S.; Teerlink, T.; Scheffer, P.G.; Meinitzer, A.; Rutters, F.; Tomaschitz, A.; Drechsler, C.; Kienreich, K.; Nijpels, G.; Stehouwer, C.D.A.; et al. Homoarginine and mortality in an older population: The Hoorn study. Eur. J. Clin. Investig. 2014, 44, 200–208. [Google Scholar] [CrossRef]
- Perkins, C.P.; Mar, V.; Shutter, J.R.; Del Castillo, J.; Danilenko, D.M.; Medlock, E.S.; Ponting, I.L.; Graham, M.; Stark, K.L.; Zuo, Y.; et al. Anemia and perinatal death result from loss of the murine ecotropic retrovirus receptor mCAT-1. Genes Dev. 1997, 11, 914–925. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Frank, J.W.; Little, D.R.; Dunlap, K.A.; Satterfield, M.C.; Burghardt, R.C.; Hansen, T.R.; Wu, G.; Bazer, F.W. Functional role of arginine during the peri-implantation period of pregnancy. I. Consequences of loss of function of arginine transporter SLC7A1 mRNA in ovine conceptus trophectoderm. FASEB J. 2014, 28, 2852–2863. [Google Scholar] [CrossRef]
- Kakoki, M.; Wang, W.; Mattson, D.L. Cationic Amino Acid Transport in the Renal Medulla and Blood Pressure Regulation. Hypertension 2002, 39, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Venardos, K.; Jones, E.; Morris, B.J.; Chin-Dusting, J.; Kaye, D.M. Identification of a Novel Polymorphism in the 3′UTR of thel-Arginine Transporter GeneSLC7A1. Circulation 2007, 115, 1269–1274. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Kaye, D.M. Mechanistic insights into the link between a polymorphism of the 3′UTR of theSLC7A1gene and hypertension. Hum. Mutat. 2008, 30, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Määttä, K.; Kunnas, T.; Nikkari, S.T. Contribution of SLC7A1 genetic variant to hypertension, the TAMRISK study. BMC Med Genet. 2013, 14, 1–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, H.; Yin, X.; Lunetta, K.L.; Dupuis, J.; McManus, D.D.; Lubitz, S.A.; Magnani, J.W.; Joehanes, R.; Munson, P.J.; Larson, M.G.; et al. Whole Blood Gene Expression and Atrial Fibrillation: The Framingham Heart Study. PLoS ONE 2014, 9, e96794. [Google Scholar] [CrossRef] [PubMed]
- Thériault, S.; Whitlock, R.; Raman, K.; Vincent, J.; Yusuf, S.; Paré, G. Gene Expression Profiles for the Identification of Prevalent Atrial Fibrillation. J. Am. Heart Assoc. 2017, 6, 006057. [Google Scholar] [CrossRef] [PubMed]
- Grupper, A.; Shashar, M.; Bahry, D.; Pri-Paz, Y.; Ben Tur, O.; Levi, S.; Chernichovski, T.; Chernin, G.; Schwartz, I.F. Cyclosporine Attenuates Arginine Transport, in Human Endothelial Cells, through Modulation of Cationic Amino Acid Transporter-1. Am. J. Nephrol. 2013, 37, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Bentur, O.S.; Schwartz, D.; Chernichovski, T.; Ingbir, M.; Weinstein, T.; Chernin, G.; Schwartz, I.F. Estradiol augments while progesterone inhibits arginine transport in human endothelial cells through modulation of cationic amino acid transporter-1. Am. J. Physiol. Integr. Comp. Physiol. 2015, 309, R421–R427. [Google Scholar] [CrossRef]
- Toral, M.; Jimenez, R.; Montoro-Molina, S.; Romero, M.; Wangensteen, R.; Duarte, J.; Vargas, F. Thyroid hormones stimulate L-arginine transport in human endothelial cells. J. Endocrinol. 2018, 239, 49–62. [Google Scholar] [CrossRef] [Green Version]
- Sala, R.; Rotoli, B.M.; Colla, E.; Visigalli, R.; Parolari, A.; Bussolati, O.; Gazzola, G.C.; Dall’Asta, V. Two-way arginine transport in human endothelial cells: TNF-α stimulation is restricted to system y+. Am. J. Physiol. Physiol. 2002, 282, C134–C143. [Google Scholar] [CrossRef]
- Hoshide, R.; Ikeda, Y.; Karashima, S.; Matsuura, T.; Komaki, S.; Kishino, T.; Niikawa, N.; Endo, F.; Matsuda, I. Molecular Cloning, Tissue Distribution, and Chromosomal Localization of Human Cationic Amino Acid Transporter 2 (HCAT2). Genomics 1996, 38, 174–178. [Google Scholar] [CrossRef]
- I Closs, E.; Albritton, L.M.; Kim, J.W.; Cunningham, J.M. Identification of a low affinity, high capacity transporter of cationic amino acids in mouse liver. J. Biol. Chem. 1993, 268, 7538–7544. [Google Scholar]
- Strobel, J.; Müller, F.; Zolk, O.; Endreß, B.; König, J.; Fromm, M.F.; Maas, R. Transport of asymmetric dimethylarginine (ADMA) by cationic amino acid transporter 2 (CAT2), organic cation transporter 2 (OCT2) and multidrug and toxin extrusion protein 1 (MATE1). Amino Acids 2013, 45, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Palacín, M.; Errasti-Murugarren, E.; Rosell, A. Heteromeric amino acid transporters. In search of the molecular bases of transport cycle mechanisms1. Biochem. Soc. Trans. 2016, 44, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Brӧer, S. The SLC38 family of sodium–amino acid co-transporters. Pflügers Archiv Eur. J. Physiol. 2013, 466, 155–172. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Sun, K.; Meng, Z.; Chen, L. The SLC transporter in nutrient and metabolic sensing, regulation, and drug development. J. Mol. Cell Biol. 2019, 11, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Carnegie, P.; Fellows, F.; Symington, G. Urinary excretion of methylarginine in human disease. Metabolism 1977, 26, 531–537. [Google Scholar] [CrossRef]
- Siroen, M.P.C.; Van Der Sijp, J.R.M.; Teerlink, T.; Van Schaik, C.; Nijveldt, R.J.; Van Leeuwen, P.A.M. The human liver clears both asymmetric and symmetric dimethylarginine. Hepatology 2005, 41, 559–565. [Google Scholar] [CrossRef]
- Inoue, Y.; Bode, B.P.; Beck, D.J.; Li, A.P.; Bland, K.I.; Souba, W.W. Arginine Transport in Human Liver. Ann. Surg. 1993, 218, 350–363. [Google Scholar] [CrossRef]
- Burdin, D.V.; Kolobov, A.A.; Brocker, C.; Soshnev, A.A.; Samusik, N.; Demyanov, A.V.; Brilloff, S.; Jarzebska, N.; Martens-Lobenhoffer, J.; Mieth, M.; et al. Diabetes-linked transcription factor HNF4α regulates metabolism of endogenous methylarginines and β-aminoisobutyric acid by controlling expression of alanine-glyoxylate aminotransferase 2. Sci. Rep. 2016, 6, 35503. [Google Scholar] [CrossRef]
- Nijveldt, R.J.; Siroen, M.P.C.; Van Der Hoven, B.; Teerlink, T.; A Prins, H.; Girbes, A.R.J.; Van Leeuwen, P.A.M. High plasma arginine concentrations in critically ill patients suffering from hepatic failure. Eur. J. Clin. Nutr. 2004, 58, 587–593. [Google Scholar] [CrossRef] [Green Version]
- Mookerjee, R.; Dalton, R.N.; Davies, N.; Hodges, S.J.; Turner, C.; Williams, R.; Jalan, R. Inflammation is an important determinant of levels of the endogenous nitric oxide synthase inhibitor asymmetric dimethylarginine (ADMA) in acute liver failure. Liver Transplant. 2007, 13, 400–405. [Google Scholar] [CrossRef]
- Lluch, P.; Torondel, B.; Medina, P.; Segarra, G.; Del Olmo, J.A.; Serra, M.A.; Rodrigo, J.M. Plasma concentrations of nitric oxide and asymmetric dimethylarginine in human alcoholic cirrhosis. J. Hepatol. 2004, 41, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Mookerjee, R.P.; Malaki, M.; Davies, N.; Hodges, S.J.; Dalton, R.N.; Turner, C.; Sen, S.; Williams, R.; Leiper, J.; Vallance, P.; et al. Increasing dimethylarginine levels are associated with adverse clinical outcome in severe alcoholic hepatitis. Hepatology 2007, 45, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.; Manner, C.K.; Kleeman, J.; MacLeod, C.L. Sustained Nitric Oxide Production in Macrophages Requires the Arginine Transporter CAT2. J. Biol. Chem. 2001, 276, 15881–15885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeramian, A.; Martin, L.; Serrat, N.; Arpa, L.; Soler, C.; Bertran, J.; McLeod, C.; Palacín, M.; Modolell, M.; Lloberas, J.; et al. Arginine Transport via Cationic Amino Acid Transporter 2 Plays a Critical Regulatory Role in Classical or Alternative Activation of Macrophages. J. Immunol. 2006, 176, 5918–5924. [Google Scholar] [CrossRef] [Green Version]
- King, N.E.; Rothenberg, M.E.; Zimmermann, N. Arginine in Asthma and Lung Inflammation. J. Nutr. 2004, 134, 2830S–2836S. [Google Scholar] [CrossRef] [Green Version]
- Thompson, R.W.; Pesce, J.T.; Ramalingam, T.; Wilson, M.S.; White, S.; Cheever, A.W.; Ricklefs, S.M.; Porcella, S.F.; Li, L.; Ellies, L.G.; et al. Cationic Amino Acid Transporter-2 Regulates Immunity by Modulating Arginase Activity. PLoS Pathog. 2008, 4, e1000023. [Google Scholar] [CrossRef] [Green Version]
- Visigalli, R.; Barilli, A.; Bussolati, O.; Sala, R.; Gazzola, G.C.; Parolari, A.; Tremoli, E.; Simon, A.; Closs, E.I.; Dall’Asta, V. Rapamycin stimulates arginine influx through CAT2 transporters in human endothelial cells. Biochim. Biophys. Acta Biomembr. 2007, 1768, 1479–1487. [Google Scholar] [CrossRef] [Green Version]
- Yeramian, A.; Martin, L.; Arpa, L.; Bertran, J.; Soler, C.; McLeod, C.; Modolell, M.; Palacín, M.; Lloberas, J.; Celada, A. Macrophages require distinct arginine catabolism and transport systems for proliferation and for activation. Eur. J. Immunol. 2006, 36, 1516–1526. [Google Scholar] [CrossRef]
- Jäger, K.; Bönisch, U.; Risch, M.; Worlitzsch, D.; Paulsen, F.P. Detection and Regulation of Cationic Amino Acid Transporters in Healthy and Diseased Ocular Surface. Investig. Opthalmology Vis. Sci. 2009, 50, 1112–1121. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, B.; Wang, Y.; Bai, B.; Yu, T.; Chu, X.-M. The biomarkers of key miRNAs and target genes associated with acute myocardial infarction. PeerJ 2020, 8, e9129. [Google Scholar] [CrossRef]
- Closs, E.I.; Ostad, M.A.; Simon, A.; Warnholtz, A.; Jabs, A.; Habermeier, A.; Daiber, A.; Förstermann, U.; Münzel, T. Impairment of the extrusion transporter for asymmetric dimethyl-l-arginine: A novel mechanism underlying vasospastic angina. Biochem. Biophys. Res. Commun. 2012, 423, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Prot-Bertoye, C.; Lebbah, S.; Daudon, M.; Tostivint, I.; Bataille, P.; Bridoux, F.; Brignon, P.; Choquenet, C.; Cochat, P.; Combe, C.; et al. CKD and Its Risk Factors among Patients with Cystinuria. Clin. J. Am. Soc. Nephrol. 2015, 10, 842–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kum, F.; Wong, K.; Game, D.; Bultitude, M.; Thomas, K. Hypertension and renal impairment in patients with cystinuria: Findings from a specialist cystinuria centre. Urolithiasis 2019, 47, 357–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toyohara, T.; Suzuki, T.; Morimoto, R.; Akiyama, Y.; Souma, T.; Shiwaku, H.O.; Takeuchi, Y.; Mishima, E.; Abe, M.; Tanemoto, M.; et al. SLCO4C1 Transporter Eliminates Uremic Toxins and Attenuates Hypertension and Renal Inflammation. J. Am. Soc. Nephrol. 2009, 20, 2546–2555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, F.Z.; Campain, A.; Yang, J.Y.H.; Morris, B.J. Meta-Analysis of Genome-Wide Gene Expression Differences in Onset and Maintenance Phases of Genetic Hypertension. Hypertension 2010, 56, 319–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bozkus, C.C.; Elzey, B.D.; Crist, S.A.; Ellies, L.G.; Ratliff, T.L. Expression of Cationic Amino Acid Transporter 2 Is Required for Myeloid-Derived Suppressor Cell-Mediated Control of T Cell Immunity. J. Immunol. 2015, 195, 5237–5250. [Google Scholar] [CrossRef]
- Jin, Y.; Liu, Y.; Nelin, L.D. Deficiency of cationic amino acid transporter-2 protects mice from hyperoxia-induced lung injury. Am. J. Physiol. Cell. Mol. Physiol. 2019, 316, L598–L607. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Iyer, D.; Rodgers, L.E.; Vanthenapalli, S.; Panguluri, S.K. Impact of hyperoxia on cardiac pathophysiology. J. Cell. Physiol. 2019, 234, 12595–12603. [Google Scholar] [CrossRef]
- Imaizumi, A.; Adachi, Y.; Kawaguchi, T.; Higasa, K.; Tabara, Y.; Sonomura, K.; Sato, T.-A.; Takahashi, M.; Mizukoshi, T.; Yoshida, H.-O.; et al. Genetic basis for plasma amino acid concentrations based on absolute quantification: A genome-wide association study in the Japanese population. Eur. J. Hum. Genet. 2019, 27, 621–630. [Google Scholar] [CrossRef]
- Yahyaoui, R.; Blasco-Alonso, J.; Benito, C.; Rodríguez-García, E.; Andrade, F.; Aldámiz-Echevarría, L.; Muñoz-Hernández, M.C.; Vega, A.I.; Pérez-Cerdá, C.; García-Martín, M.L.; et al. A new metabolic disorder in human cationic amino acid transporter-2 that mimics arginase 1 deficiency in newborn screening. J. Inherit. Metab. Dis. 2019, 42, 407–413. [Google Scholar] [CrossRef]
- Vékony, N.; Wolf, S.; Boissel, J.-P.; Gnauert, K.; Closs, E.I. Human Cationic Amino Acid Transporter hCAT-3 Is Preferentially Expressed in Peripheral Tissues. Biochemistry 2001, 40, 12387–12394. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.; Sawamura, T.; Masaki, T.; MacLeod, C.L. Increased Cat3-mediated Cationic Amino Acid Transport Functionally Compensates inCat1Knockout Cell Lines. J. Biol. Chem. 1998, 273, 14663–14666. [Google Scholar] [CrossRef] [Green Version]
- Ito, K.; Groudine, M. A New Member of the Cationic Amino Acid Transporter Family Is Preferentially Expressed in Adult Mouse Brain. J. Biol. Chem. 1997, 272, 26780–26786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nava, C.; Rupp, J.; Boissel, J.-P.; Mignot, C.; Rastetter, A.; Amiet, C.; Jacquette, A.; Dupuits, C.; Bouteiller, D.; Keren, B.; et al. Hypomorphic variants of cationic amino acid transporter 3 in males with autism spectrum disorders. Amino Acids 2015, 47, 2647–2658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verrey, F.; Meier, C.; Rossier, G.; Kühn, L.C. Glycoprotein-associated amino acid exchangers: Broadening the range of transport specificity. Pflügers Archiv Eur. J. Physiol. 2000, 440, 503–512. [Google Scholar] [CrossRef]
- Brӧer, S. Amino Acid Transport Across Mammalian Intestinal and Renal Epithelia. Physiol. Rev. 2008, 88, 249–286. [Google Scholar] [CrossRef]
- Bröer, A.; Wagner, C.A.; Lang, F.; Brӧer, S. The heterodimeric amino acid transporter 4F2hc/y+LAT2 mediates arginine efflux in exchange with glutamine. Biochem. J. 2000, 349, 787–795. [Google Scholar] [CrossRef]
- Torrents, D.; Estévez, R.; Pineda, M.; Fernández, E.; Lloberas, J.; Shi, Y.-B.; Zorzano, A.; Palacín, M. Identification and Characterization of a Membrane Protein (y+L Amino Acid Transporter-1) That Associates with 4F2hc to Encode the Amino Acid Transport Activity y+L. J. Biol. Chem. 1998, 273, 32437–32445. [Google Scholar] [CrossRef] [Green Version]
- Boyd, C.; Deves, R.; Laynes, R.; Kudo, Y.; Sebastio, G. Cationic amino acid transport through system y+L in erythrocytes of patients with lysinuric protein intolerance. Pflügers Archiv Eur. J. Physiol. 2000, 439, 513–516. [Google Scholar] [CrossRef]
- Pfeiffer, R.; Rossier, G.; Spindler, B.; Meier, C.; Kühn, L.; Verrey, F. Amino acid transport of y+L-type by heterodimers of 4F2hc/CD98 and members of the glycoprotein-associated amino acid transporter family. EMBO J. 1999, 18, 49–57. [Google Scholar] [CrossRef] [Green Version]
- Rotoli, B.M.; Bussolati, O.; Sala, R.; Barilli, A.; Talarico, E.; Gazzola, G.C.; Dall’Asta, V. INFγ stimulates arginine transport through system y+L in human monocytes. FEBS Lett. 2004, 571, 177–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milewski, K.; Bogacińska-Karaś, M.; Fręśko, I.; Hilgier, W.; Jazwiec, R.; Albrecht, J.; Zielińska, M. Ammonia Reduces Intracellular Asymmetric Dimethylarginine in Cultured Astrocytes Stimulating Its y+LAT2 Carrier-Mediated Loss. Int. J. Mol. Sci. 2017, 18, 2308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kayanoki, Y.; Kawata, S.; Yamasaki, E.; Kiso, S.; Inoue, S.; Tamura, S.; Taniguchi, N.; Matsuzawa, Y. Reduced nitric oxide production by L-arginine deficiency in lysinuric protein intolerance exacerbates intravascular coagulation. Metabolism 1999, 48, 1136–1140. [Google Scholar] [CrossRef]
- Mauhin, W.; Habarou, F.; Gobin, S.; Servais, A.; Brassier, A.; Grisel, C.; Roda, C.; Pinto, G.; Moshous, D.; Ghalim, F.; et al. Update on Lysinuric Protein Intolerance, a Multi-faceted Disease Retrospective cohort analysis from birth to adulthood. Orphanet J. Rare Dis. 2017, 12, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanner, L.; Näntö-Salonen, K.; Niinikoski, H.; Jahnukainen, T.; Keskinen, P.; Saha, H.; Kananen, K.; Helanterä, A.; Metso, M.; Linnanvuo, M.; et al. Nephropathy Advancing to End-Stage Renal Disease: A Novel Complication of Lysinuric Protein Intolerance. J. Pediatr. 2007, 150, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Fernández, E.; Carrascal, M.; Rousaud, F.; Abián, J.; Zorzano, A.; Palacín, M.; Chillarón, J. rBAT-b0,+AT heterodimer is the main apical reabsorption system for cystine in the kidney. Am. J. Physiol. Physiol. 2002, 283, F540–F548. [Google Scholar] [CrossRef] [Green Version]
- Bertran, J.; Werner, A.; Chillarón, J.; Nunes, V.; Biber, J.; Testar, X.; Zorzano, A.; Estivill, X.; Murer, H.; Palacín, M. Expression cloning of a human renal cDNA that induces high affinity transport of L-cystine shared with dibasic amino acids in Xenopus oocytes. J. Biol. Chem. 1993, 268, 14842–14849. [Google Scholar]
- Tate, S.S.; Yan, N.; Udenfriend, S. Expression cloning of a Na(+)-independent neutral amino acid transporter from rat kidney. Proc. Natl. Acad. Sci. USA 1992, 89, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Wells, R.G.; Hediger, M.A. Cloning of a rat kidney cDNA that stimulates dibasic and neutral amino acid transport and has sequence similarity to glucosidases. Proc. Natl. Acad. Sci. USA 1992, 89, 5596–5600. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.-X.; Rozen, R.; Hediger, M.A.; Goodyer, P.; Eydoux, P. Assignment of the Gene for Cystinuria (SLC3A1) to Human Chromosome 2p21 by Fluorescence in Situ Hybridization. Genomics 1994, 24, 413–414. [Google Scholar] [CrossRef]
- Bisceglia, L.; Calonge, M.J.; Totaro, A.; Feliubadaló, L.; Melchionda, S.; García, J.; Testar, X.; Gallucci, M.; Ponzone, A.; Zelante, L.; et al. Localization, by linkage analysis, of the cystinuria type III gene to chromosome 19q13.1. Am. J. Hum. Genet. 1997, 60, 611–616. [Google Scholar] [PubMed]
- Wagner, C.A.; Lang, F.; Bröer, S. Function and structure of heterodimeric amino acid transporters. Am. J. Physiol. Physiol. 2001, 281, C1077–C1093. [Google Scholar] [CrossRef] [PubMed]
- Feliubadaló, L.; Font, M.; Purroy, J.; Rousaud, F.; Estivill, X.; Nunes, V.; Golomb, E.; Centola, M.; Aksentijevich, I.; Kreiss, Y.; et al. Non-type I cystinuria caused by mutations in SLC7A9, encoding a subunit (bo,+AT) of rBAT. Nat. Genet. 1999, 23, 52–57. [Google Scholar] [CrossRef]
- Busch, A.; Herzer, T.; Waldegger, S.; Schmidt, F.; Palacin, M.; Biber, J.; Markovich, D.; Murer, H.; Lang, F. Opposite directed currents induced by the transport of dibasic and neutral amino acids in Xenopus oocytes expressing the protein rBAT. J. Biol. Chem. 1994, 269, 25581–25586. [Google Scholar] [PubMed]
- Reig, N.; Chillarón, J.; Bartoccioni, P.; Fernández, E.; Bendahan, A.; Zorzano, A.; Kanner, B.; Palacín, M.; Bertran, J. The light subunit of system bo,+ is fully functional in the absence of the heavy subunit. EMBO J. 2002, 21, 4906–4914. [Google Scholar] [CrossRef] [Green Version]
- Chillarón, J.; Estévez, R.; Mora, C.; A Wagner, C.; Suessbrich, H.; Lang, F.; Gelpí, J.L.; Testar, X.; E Busch, A.; Zorzano, A.; et al. Obligatory Amino Acid Exchange via Systems bo,+-like and y+L-like. J. Biol. Chem. 1996, 271, 17761–17770. [Google Scholar] [CrossRef] [Green Version]
- Mizoguchi, K.; Cha, S.H.; Chairoungdua, A.; Kim, D.K.; Shigeta, Y.; Matsuo, H.; Fukushima, J.-I.; Awa, Y.; Akakura, K.; Goya, T.; et al. Human cystinuria-related transporter: Localization and functional characterization. Kidney Int. 2001, 59, 1821–1833. [Google Scholar] [CrossRef] [Green Version]
- Bauch, C.; Verrey, F. Apical heterodimeric cystine and cationic amino acid transporter expressed in MDCK cells. Am. J. Physiol. Physiol. 2002, 283, F181–F189. [Google Scholar] [CrossRef] [Green Version]
- Crawhall, J.C.; Scowen, E.F.; Thompson, C.J.; Watts, R.W.E. The Renal Clearance of Amino Acids in Cystinuria. J. Clin. Investig. 1967, 46, 1162–1171. [Google Scholar] [CrossRef]
- Andreassen, K.H.; Pedersen, K.V.; Osther, S.S.; Jung, H.U.; Lildal, S.K.; Osther, P.J.S. How should patients with cystine stone disease be evaluated and treated in the twenty-first century? Urolithiasis 2015, 44, 65–76. [Google Scholar] [CrossRef]
- Martell, H.J.; Wong, K.A.; Martin, J.F.; Kassam, Z.; Thomas, K.; Wass, M.N. Associating mutations causing cystinuria with disease severity with the aim of providing precision medicine. BMC Genom. 2017, 18, 47–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmadi, S.; Xia, S.; Wu, Y.-S.; Di Paola, M.; Kissoon, R.; Luk, C.; Lin, F.; Du, K.; Rommens, J.M.; Bear, C.E. SLC6A14, an amino acid transporter, modifies the primary CF defect in fluid secretion. eLife 2018, 7, e37963. [Google Scholar] [CrossRef] [PubMed]
- Ruffin, M.; Mercier, J.; Calmel, C.; Mésinèle, J.; Bigot, J.; Sutanto, E.N.; Kicic, A.; Corvol, H.; Guillot, L. Update on SLC6A14 in lung and gastrointestinal physiology and physiopathology: Focus on cystic fibrosis. Cell. Mol. Life Sci. 2020, 77, 3311–3323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galietta, L.J.V.; Musante, L.; Romio, L.; Caruso, U.; Fantasia, A.; Gazzolo, A.; Romano, L.; Sacco, O.; Rossi, G.A.; Varesio, L.; et al. An electrogenic amino acid transporter in the apical membrane of cultured human bronchial epithelial cells. Am. J. Physiol. Cell. Mol. Physiol. 1998, 275, L917–L923. [Google Scholar] [CrossRef] [PubMed]
- Jain-Vakkalagadda, B.; Pal, D.; Gunda, S.; Nashed, Y.; Ganapathy, V.; Mitra, A.K. Identification of a Na+-Dependent Cationic and Neutral Amino Acid Transporter, B0,+, in Human and Rabbit Cornea. Mol. Pharm. 2004, 1, 338–346. [Google Scholar] [CrossRef]
- Dai, R.; Peng, F.; Xiao, X.; Gong, X.; Jiang, Y.; Zhang, M.; Tian, Y.; Xu, Y.; Ma, J.; Li, M.; et al. Hepatitis B virus X protein-induced upregulation of CAT-1 stimulates proliferation and inhibits apoptosis in hepatocellular carcinoma cells. Oncotarget 2017, 8, 60962–60974. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Wang, W.; Wang, J.; Yang, C.; Mao, H.; Fu, X.; Wu, Y.; Cai, J.; Han, J.; Xu, Z.; et al. Overexpression of Arginine Transporter CAT-1 Is Associated with Accumulation of L-Arginine and Cell Growth in Human Colorectal Cancer Tissue. PLoS ONE 2013, 8, e73866. [Google Scholar] [CrossRef]
- Abdelmagid, S.A.; Rickard, J.A.; McDonald, W.J.; Thomas, L.N.; Too, C.K. CAT-1-mediated arginine uptake and regulation of nitric oxide synthases for the survival of human breast cancer cell lines. J. Cell. Biochem. 2011, 112, 1084–1092. [Google Scholar] [CrossRef]
- Deves, R.; Angelo, S.; Chávez, P. N-ethylmaleimide discriminates between two lysine transport systems in human erythrocytes. J. Physiol. 1993, 468, 753–766. [Google Scholar] [CrossRef]
- White, M.F. The transport of cationic amino acids across the plasma membrane of mammalian cells. Biochim. Biophys. Acta Rev. Biomembr. 1985, 822, 355–374. [Google Scholar] [CrossRef]
- White, M.F.; Gazzola, G.C.; Christensen, H.N. Cationic amino acid transport into cultured animal cells. I. Influx into cultured human fibroblasts. J. Biol. Chem. 1982, 257, 4443–4449. [Google Scholar] [PubMed]
- Wang, H.; Kavanaugh, M.P.; North, R.A.; Kabat, D. Cell-surface receptor for ecotropic murine retroviruses is a basic amino-acid transporter. Nat. Cell Biol. 1991, 352, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Beyer, S.R.; Mallmann, R.T.; Jaenecke, I.; Habermeier, A.; Boissel, J.-P.; Closs, E.I. Identification of Cysteine Residues in Human Cationic Amino Acid Transporter hCAT-2A That Are Targets for Inhibition byN-Ethylmaleimide. J. Biol. Chem. 2013, 288, 30411–30419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacLeod, C.L.; Finley, K.D.; Kakuda, D.K. y(+)-type cationic amino acid transport: Expression and regulation of the mCAT genes. J. Exp. Biol. 1994, 196, 109–121. [Google Scholar]
- Shen, L.; Qian, C.; Cao, H.; Wang, Z.; Luo, T.; Liang, C. Upregulation of the solute carrier family 7 genes is indicative of poor prognosis in papillary thyroid carcinoma. World J. Surg. Oncol. 2018, 16, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Hosokawa, H.; Sawamura, T.; Kobayashi, S.; Ninomiya, H.; Miwa, S.; Masaki, T. Cloning and Characterization of a Brain-specific Cationic Amino Acid Transporter. J. Biol. Chem. 1997, 272, 8717–8722. [Google Scholar] [CrossRef] [Green Version]
- Palacín, M.; Mora, C.; Chillarón, J.; Calonge, M.J.; Estévez, R.; Torrents, D.; Testar, X.; Zorzano, A.; Nunes, V.; Purroy, J.; et al. The molecular basis of cystinuria: The role of the rBAT gene. Amino Acids 1996, 11, 225–246. [Google Scholar]
- Jiang, Y.; Cao, Y.; Wang, Y.; Li, W.; Liu, X.; Lv, Y.; Li, X.; Mi, J. Cysteine transporter SLC3A1 promotes breast cancer tumorigenesis. Theranostics 2017, 7, 1036–1046. [Google Scholar] [CrossRef] [Green Version]
- Waldegger, S.; Schmidt, F.; Herzer, T.; Gulbins, E.; Schuster, A.; Biber, J.; Markovich, D.; Murer, H.; Busch, A.E.; Lang, F. Heavy metal mediated inhibition of rBAT-induced amino acid transport. Kidney Int. 1995, 47, 1677–1681. [Google Scholar] [CrossRef] [Green Version]
- Pfeiffer, R.; Loffing, J.; Rossier, G.; Bauch, C.; Meier, C.; Eggermann, T.; Loffing-Cueni, M.; Kühn, L.C.; Verrey, F. Luminal Heterodimeric Amino Acid Transporter Defective in Cystinuria. Mol. Biol. Cell 1999, 10, 4135–4147. [Google Scholar] [CrossRef] [Green Version]
- Chairoungdua, A.; Segawa, H.; Kim, J.Y.; Miyamoto, K.-I.; Haga, H.; Fukui, Y.; Mizoguchi, K.; Ito, H.; Takeda, E.; Endou, H.; et al. Identification of an Amino Acid Transporter Associated with the Cystinuria-related Type II Membrane Glycoprotein. J. Biol. Chem. 1999, 274, 28845–28848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertran, J.; Werner, A.; Moore, M.L.; Stange, G.; Markovich, D.; Biber, J.; Testar, X.; Zorzano, A.; Palacín, M.; Murer, H. Expression cloning of a cDNA from rabbit kidney cortex that induces a single transport system for cystine and dibasic and neutral amino acids. Proc. Natl. Acad. Sci. USA 1992, 89, 5601–5605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rotoli, B.M.; Barilli, A.; Visigalli, R.; Ferrari, F.; Dall’Asta, V. y+LAT1 and y+LAT2 contribution to arginine uptake in different human cell models: Implications in the pathophysiology of Lysinuric Protein Intolerance. J. Cell. Mol. Med. 2020, 24, 921–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torrents, D.; Mykkänen, J.; Pineda, M.; Feliubadaló, L.; Estévez, R.; De Cid, R.; Sanjurjo, P.; Zorzano, A.; Nunes, V.; Huoponen, K.; et al. Identification of SLC7A7, encoding y+LAT-1, as the lysinuric protein intolerance gene. Nat. Genet. 1999, 21, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Sperandeo, M.P.; Annunziata, P.; Bozzato, A.; Piccolo, P.; Maiuri, L.; D’Armiento, M.; Ballabio, A.; Corso, G.; Andria, G.; Borsani, G.; et al. Slc7a7 disruption causes fetal growth retardation by downregulating Igf1 in the mouse model of lysinuric protein intolerance. Am. J. Physiol. Physiol. 2007, 293, C191–C198. [Google Scholar] [CrossRef] [Green Version]
- Gunturiz, M.L.; Forrero, A.Y.; Chaparro, P.E. Genes Implicated in Obesity and Overweight: Potential Biomarkers of Early Diagnosis. Curr. Res. Clin. Diab. Obes. 2018. [Google Scholar] [CrossRef]
- Hu, X.; Han, T.; Bian, Y.; Tong, H.; Wen, X.; Li, Y.; Wan, X. Knockdown of SLCO4C1 inhibits cell proliferation and metastasis in endometrial cancer through inactivating the PI3K/Akt signaling pathway. Oncol. Rep. 2020, 43, 919–929. [Google Scholar] [CrossRef]
- Du, P.; Wang, A.; Ma, Y.; Jia, A.; Li, Y.; Li, X. Impact of SLCO4C1 Genotypes, Creatinine, and Spironolactone on Digoxin Population Pharmacokinetic Variables in Patients With Cardiac Insufficiency. Clin. Ther. 2020. [Google Scholar] [CrossRef]
- Sato, T.; Mishima, E.; Mano, N.; Abe, T.; Yamaguchi, H. Potential Drug Interactions Mediated by Renal Organic Anion Transporter OATP4C1. J. Pharmacol. Exp. Ther. 2017, 362, 271–277. [Google Scholar] [CrossRef] [Green Version]
- Taghikhani, E.; Maas, R.; Fromm, M.F.; König, J. The renal transport protein OATP4C1 mediates uptake of the uremic toxin asymmetric dimethylarginine (ADMA) and efflux of cardioprotective L-homoarginine. PLoS ONE 2019, 14, e0213747. [Google Scholar] [CrossRef]
- Taghikhani, E.; Maas, R.; Taudte, R.V.; Gessner, A.; Fromm, M.F.; König, J. Vectorial transport of the arginine derivatives asymmetric dimethylarginine (ADMA) and l-homoarginine by OATP4C1 and P-glycoprotein studied in double-transfected MDCK cells. Amino Acids 2020, 52, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.J.; Hu, T.; Wang, J. Polyspecific organic cation transporters and their impact on drug intracellular levels and pharmacodynamics. Pharmacol. Res. 2016, 111, 237–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schömig, E.; Lazar, A.; Gründemann, D. Extraneuronal Monoamine Transporter and Organic Cation Transporters 1 and 2: A Review of Transport Efficiency. Bone Regulators Osteop. Ther. 2006, 151–180. [Google Scholar] [CrossRef]
- Hacker, K.; Maas, R.; Kornhuber, J.; Fromm, M.F.; Zolk, O. Substrate-Dependent Inhibition of the Human Organic Cation Transporter OCT2: A Comparison of Metformin with Experimental Substrates. PLoS ONE 2015, 10, e0136451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nies, A.T.; Koepsell, H.; Damme, K.; Schwab, M. Organic Cation Transporters (OCTs, MATEs), In Vitro and In Vivo Evidence for the Importance in Drug Therapy. Bone Regulators Osteoporos. Ther. 2010, 105–167. [Google Scholar] [CrossRef]
- Cohen, R.; Basel-Vanagaite, L.; Goldberg-Stern, H.; Halevy, A.; Shuper, A.; Feingold-Zadok, M.; Behar, D.M.; Straussberg, R.; Basel-Salmon, L. Two siblings with early infantile myoclonic encephalopathy due to mutation in the gene encoding mitochondrial glutamate/H+ symporter SLC25A22. Eur. J. Paediatr. Neurol. 2014, 18, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.C.; Qian, Y.; Li, X.; Xu, J.; Kang, W.; Tong, J.H.; To, K.-F.; Jin, Y.; Li, W.; Chen, H.; et al. SLC25A22 Promotes Proliferation and Survival of Colorectal Cancer Cells With KRAS Mutations and Xenograft Tumor Progression in Mice via Intracellular Synthesis of Aspartate. Gastroenterology 2016, 151, 945–960. [Google Scholar] [CrossRef] [Green Version]
- Fiermonte, G.; Dolce, V.; David, L.; Santorelli, F.M.; Dionisi-Vici, C.; Palmieri, F.; Walker, J.E. The Mitochondrial Ornithine Transporter: Bacterial Expression, Reconstitution, Functional Characterization, and Tissue Distribution of Two Human Isoforms. J. Biol. Chem. 2003, 278, 32778–32783. [Google Scholar] [CrossRef] [Green Version]
- Porcelli, V.; Longo, A.; Palmieri, F.; Closs, E.I.; Palmieri, F. Asymmetric dimethylarginine is transported by the mitochondrial carrier SLC25A2. Amino Acids 2015, 48, 427–436. [Google Scholar] [CrossRef]
- Martinelli, D.; Diodato, N.; Ponzi, E.; Monné, M.; Boenzi, S.; Bertini, E.S.; Fiermonte, G.; Dionisi-Vici, C.C. The hyperornithinemia-hyperammonemia-homocitrullinuria syndrome. Orphanet J. Rare Dis. 2015, 10, 29. [Google Scholar] [CrossRef] [Green Version]
- Camacho, J.; Rioseco-Camacho, N. The Human and Mouse SLC25A29 Mitochondrial Transporters Rescue the Deficient Ornithine Metabolism in Fibroblasts of Patients with the Hyperornithinemia-Hyperammonemia-Homocitrullinuria (HHH) Syndrome. Pediatr. Res. 2009, 66, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmieri, F. Diseases caused by defects of mitochondrial carriers: A review. Biochim. Biophys. Acta Gen. Subj. 2008, 1777, 564–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porcelli, V.; Fiermonte, G.; Longo, A.; Palmieri, F. The Human GeneSLC25A29, of Solute Carrier Family 25, Encodes a Mitochondrial Transporter of Basic Amino Acids. J. Biol. Chem. 2014, 289, 13374–13384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matoba, S.; Nakamuta, S.; Miura, K.; Hirose, M.; Shiura, H.; Kohda, T.; Nakamuta, N.; Ogura, A. Paternal knockout of Slc38a4/SNAT4 causes placental hypoplasia associated with intrauterine growth restriction in mice. Proc. Natl. Acad. Sci. USA 2019, 116, 21047–21053. [Google Scholar] [CrossRef] [Green Version]
- Hu, C.; Tao, L.; Cao, X.; Chen, L. The solute carrier transporters and the brain: Physiological and pharmacological implications. Asian J. Pharm. Sci. 2020, 15, 131–144. [Google Scholar] [CrossRef]
- Christensen, H.N. Role of amino acid transport and countertransport in nutrition and metabolism. Physiol. Rev. 1990, 70, 43–77. [Google Scholar] [CrossRef]
- Hatanaka, T.; Huang, W.; Ling, R.; Prasad, P.D.; Sugawara, M.; Leibach, F.H.; Ganapathy, V. Evidence for the transport of neutral as well as cationic amino acids by ATA3, a novel and liver-specific subtype of amino acid transport system A. Biochim. Biophys. Acta Biomembr. 2001, 1510, 10–17. [Google Scholar] [CrossRef] [Green Version]
- Hägglund, M.G.A.; Sreedharan, S.; Nilsson, V.C.O.; Shaik, J.H.A.; Almkvist, I.M.; Bäcklin, S.; Wrange, O.; Fredriksson, R. Identification of SLC38A7 (SNAT7) Protein as a Glutamine Transporter Expressed in Neurons. J. Biol. Chem. 2011, 286, 20500–20511. [Google Scholar] [CrossRef] [Green Version]
- Poulter, J.A.; Al-Araimi, M.; Conte, I.; Van Genderen, M.M.; Sheridan, E.; Carr, I.M.; Parry, D.A.; Shires, M.; Carrella, S.; Bradbury, J.; et al. Recessive Mutations in SLC38A8 Cause Foveal Hypoplasia and Optic Nerve Misrouting without Albinism. Am. J. Hum. Genet. 2013, 93, 1143–1150. [Google Scholar] [CrossRef] [Green Version]
- Hägglund, M.G.; Hellsten, S.V.; Bagchi, S.; Philippot, G.; Löfqvist, E.; Nilsson, V.C.; Almkvist, I.; Karlsson, E.; Sreedharan, S.; Tafreshiha, A.; et al. Transport of l-Glutamine, l-Alanine, l-Arginine and l-Histidine by the Neuron-Specific Slc38a8 (SNAT8) in CNS. J. Mol. Biol. 2015, 427, 1495–1512. [Google Scholar] [CrossRef]
- Nies, A.T.; Damme, K.; Kruck, S.; Schaeffeler, E.; Schwab, M. Structure and function of multidrug and toxin extrusion proteins (MATEs) and their relevance to drug therapy and personalized medicine. Arch. Toxicol. 2016, 90, 1555–1584. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, A.; Inui, K.-I. Importance of the multidrug and toxin extrusion MATE/SLC47A family to pharmacokinetics, pharmacodynamics/toxicodynamics and pharmacogenomics. Br. J. Pharmacol. 2011, 164, 1817–1825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glaeser, H. Importance of P-glycoprotein for Drug–Drug Interactions. Bone Regulators Osteoporos. Ther. 2010, 201, 285–297. [Google Scholar] [CrossRef]
- Sharom, F.J. Complex Interplay between the P-Glycoprotein Multidrug Efflux Pump and the Membrane: Its Role in Modulating Protein Function. Front. Oncol. 2014, 4, 41. [Google Scholar] [CrossRef] [Green Version]
- Kim, R.B. Drugs as P-glycoprotein substrates, inhibitors, and inducers. Drug Metab. Rev. 2002, 34, 47–54. [Google Scholar] [CrossRef]
- Yasui-Furukori, N.; Uno, T. Drug-Drug Interactions of P-gp Substrates Unrelated to CYP Metabolism. Curr. Drug Metab. 2019, 20, 124–129. [Google Scholar] [CrossRef]
- Roth, M.; Obaidat, A.; Hagenbuch, B. OATPs, OATs and OCTs: The organic anion and cation transporters of the SLCO and SLC22A gene superfamilies. Br. J. Pharmacol. 2012, 165, 1260–1287. [Google Scholar] [CrossRef] [Green Version]
- Mikkaichi, T.; Suzuki, T.; Onogawa, T.; Tanemoto, M.; Mizutamari, H.; Okada, M.; Chaki, T.; Masuda, S.; Tokui, T.; Eto, N.; et al. Isolation and characterization of a digoxin transporter and its rat homologue expressed in the kidney. Proc. Natl. Acad. Sci. USA 2004, 101, 3569–3574. [Google Scholar] [CrossRef] [Green Version]
- Hagenbuch, B.; Meier, P.J. Organic anion transporting polypeptides of the OATP/ SLC21 family: Phylogenetic classification as OATP/ SLCO superfamily, new nomenclature and molecular/functional properties. Pflügers Archiv Eur. J. Physiol. 2004, 447, 653–665. [Google Scholar] [CrossRef] [Green Version]
- Chu, X.-Y.; Bleasby, K.; Yabut, J.; Cai, X.; Chan, G.H.; Hafey, M.J.; Xu, S.; Bergman, A.J.; Braun, M.P.; Dean, D.C.; et al. Transport of the Dipeptidyl Peptidase-4 Inhibitor Sitagliptin by Human Organic Anion Transporter 3, Organic Anion Transporting Polypeptide 4C1, and Multidrug Resistance P-glycoprotein. J. Pharmacol. Exp. Ther. 2007, 321, 673–683. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, T.; Toyohara, T.; Akiyama, Y.; Takeuchi, Y.; Mishima, E.; Suzuki, C.; Ito, S.; Soga, T.; Abe, T. Transcriptional Regulation of Organic Anion Transporting Polypeptide SLCO4C1 as a New Therapeutic Modality to Prevent Chronic Kidney Disease. J. Pharm. Sci. 2011, 100, 3696–3707. [Google Scholar] [CrossRef] [PubMed]
- AlbarracÌn, M.G.; Forero, A.Y.; Chaparro, P. Genes implicated in obesity and overweight potential biomarkers of early diagnosis. Curr. Res. Clin. Diab. Obes. 2018, 2018. [Google Scholar] [CrossRef]
- Nigam, S.K. The SLC22 Transporter Family: A Paradigm for the Impact of Drug Transporters on Metabolic Pathways, Signaling, and Disease. Annu. Rev. Pharmacol. Toxicol. 2018, 58, 663–687. [Google Scholar] [CrossRef] [PubMed]
- Volk, C. OCTs, OATs, and OCTNs: Structure and function of the polyspecific organic ion transporters of the SLC22 family. Wiley Interdiscip. Rev. Membr. Transp. Signal. 2013, 3, 1–13. [Google Scholar] [CrossRef]
- Taubert, D.; Grimberg, G.; Stenzel, W.; Schömig, E. Identification of the Endogenous Key Substrates of the Human Organic Cation Transporter OCT2 and Their Implication in Function of Dopaminergic Neurons. PLoS ONE 2007, 2, e385. [Google Scholar] [CrossRef] [Green Version]
- Gorboulev, V.; Ulzheimer, J.C.; Akhoundova, A.; Ulzheimer-Teuber, I.; Karbach, U.; Quester, S.; Baumann, C.; Lang, F.; Busch, A.E.; Koepsell, H. Cloning and Characterization of Two Human Polyspecific Organic Cation Transporters. DNA Cell Biol. 1997, 16, 871–881. [Google Scholar] [CrossRef]
- Ciarimboli, G.; Deuster, D.; Knief, A.; Sperling, M.; Holtkamp, M.; Edemir, B.; Pavenstädt, H.; Lanvers-Kaminsky, C.; Zehnhoff-Dinnesen, A.A.; Schinkel, A.H.; et al. Organic Cation Transporter 2 Mediates Cisplatin-Induced Oto- and Nephrotoxicity and Is a Target for Protective Interventions. Am. J. Pathol. 2010, 176, 1169–1180. [Google Scholar] [CrossRef]
- Busch, A.E.; Karbach, U.; Miska, D.; Gorboulev, V.; Akhoundova, A.; Volk, C.; Arndt, P.; Ulzheimer, J.C.; Sonders, M.S.; Baumann, C.; et al. Human Neurons Express the Polyspecific Cation Transporter hOCT2, Which Translocates Monoamine Neurotransmitters, Amantadine, and Memantine. Mol. Pharmacol. 1998, 54, 342–352. [Google Scholar] [CrossRef] [Green Version]
- Harper, J.N.; Wright, S.H. Multiple mechanisms of ligand interaction with the human organic cation transporter, OCT2. Am. J. Physiol. Physiol. 2013, 304, F56–F67. [Google Scholar] [CrossRef] [Green Version]
- Gründemann, D.; Köster, S.; Kiefer, N.; Breidert, T.; Engelhardt, M.; Spitzenberger, F.; Obermüller, N.; Schömig, E. Transport of Monoamine Transmitters by the Organic Cation Transporter Type 2, OCT2. J. Biol. Chem. 1998, 273, 30915–30920. [Google Scholar] [CrossRef] [Green Version]
- Leone, A.; Moncada, S.; Vallance, P.; Calver, A.; Collier, J. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet 1992, 339, 572–575. [Google Scholar] [CrossRef]
- Lai, Y.; Varma, M.; Feng, B.; Stephens, J.C.; Kimoto, E.; El-Kattan, A.; Ichikawa, K.; Kikkawa, H.; Ono, C.; Suzuki, A.; et al. Impact of drug transporter pharmacogenomics on pharmacokinetic and pharmacodynamic variability—Considerations for drug development. Expert Opin. Drug Metab. Toxicol. 2012, 8, 723–743. [Google Scholar] [CrossRef] [PubMed]
- Ruprecht, J.J.; Kunji, E.R.S. The SLC25 Mitochondrial Carrier Family: Structure and Mechanism. Trends Biochem. Sci. 2020, 45, 244–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camacho, J.A.; Obie, C.; Biery, B.; Goodman, B.K.; Hu, C.-A.; Almashanu, S.; Steel, G.; Casey, R.; Lambert, M.; Mitchell, G.A.; et al. Hyperornithinaemia- hyperammonaemia- homocitrullinuria syndrome is caused by mutations in a gene encoding a mitochondrial ornithine transporter. Nat. Genet. 1999, 22, 151–158. [Google Scholar] [CrossRef]
- A Camacho, J.; Rioseco-Camacho, N.; Andrade, D.; Porter, J.; Kong, J. Cloning and characterization of human ORNT2: A second mitochondrial ornithine transporter that can rescue a defective ORNT1 in patients with the hyperornithinemia–hyperammonemia–homocitrullinuria syndrome, a urea cycle disorder. Mol. Genet. Metab. 2003, 79, 257–271. [Google Scholar] [CrossRef]
- Sekoguchi, E.; Sato, N.; Yasui, A.; Fukada, S.; Nimura, Y.; Aburatani, H.; Ikeda, K.; Matsuura, A. A Novel Mitochondrial Carnitine-acylcarnitine Translocase Induced by Partial Hepatectomy and Fasting. J. Biol. Chem. 2003, 278, 38796–38802. [Google Scholar] [CrossRef] [Green Version]
- Palmieri, F. The mitochondrial transporter family SLC25: Identification, properties and physiopathology. Mol. Asp. Med. 2013, 34, 465–484. [Google Scholar] [CrossRef]
- Palmieri, L.; De Marco, V.; Iacobazzi, V.; Palmieri, F.; Runswick, M.J.; Walker, J.E. Identification of the yeast ARG-11 gene as a mitochondrial ornithine carrier involved in arginine biosynthesis. FEBS Lett. 1997, 410, 447–451. [Google Scholar] [CrossRef]
- MacKenzie, B.; Erickson, J.D. Sodium-coupled neutral amino acid (System N/A) transporters of the SLC38 gene family. Pflügers Archiv Eur. J. Physiol. 2004, 447, 784–795. [Google Scholar] [CrossRef]
- Desforges, M.; Lacey, H.A.; Glazier, J.D.; Greenwood, S.L.; Mynett, K.J.; Speake, P.F.; Sibley, C.P. SNAT4 isoform of system A amino acid transporter is expressed in human placenta. Am. J. Physiol. Physiol. 2006, 290, C305–C312. [Google Scholar] [CrossRef] [Green Version]
- Jackson, M.J.; Beaudet, A.L.; E O’Brien, W. Mammalian Urea Cycle Enzymes. Annu. Rev. Genet. 1986, 20, 431–464. [Google Scholar] [CrossRef] [PubMed]
- Damme, K.; Nies, A.T.; Schaeffeler, E.; Schwab, M. Mammalian MATE (SLC47A) transport proteins: Impact on efflux of endogenous substrates and xenobiotics. Drug Metab. Rev. 2011, 43, 499–523. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, M.; Yasuda, M.; Morita, Y.; Otsuka, C.; Tsuchiya, T.; Omote, H.; Moriyama, Y. Identification of Essential Amino Acid Residues of the NorM Na+/Multidrug Antiporter in Vibrio parahaemolyticus. J. Bacteriol. 2005, 187, 1552–1558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanihara, Y.; Masuda, S.; Sato, T.; Katsura, T.; Ogawa, O.; Inui, K.-I. Substrate specificity of MATE1 and MATE2-K, human multidrug and toxin extrusions/H+-organic cation antiporters. Biochem. Pharmacol. 2007, 74, 359–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otsuka, M.; Matsumoto, T.; Morimoto, R.; Arioka, S.; Omote, H.; Moriyama, Y. A human transporter protein that mediates the final excretion step for toxic organic cations. Proc. Natl. Acad. Sci. USA 2005, 102, 17923–17928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuda, M.; Terada, T.; Asaka, J.-I.; Ueba, M.; Katsura, T.; Inui, K.-I. Oppositely directed H+ gradient functions as a driving force of rat H+/organic cation antiporter MATE1. Am. J. Physiol. Physiol. 2007, 292, F593–F598. [Google Scholar] [CrossRef] [Green Version]
- König, J.; Zolk, O.; Singer, K.; Hoffmann, C.; Fromm, M.F. Double-transfected MDCK cells expressing human OCT1/MATE1 or OCT2/MATE1: Determinants of uptake and transcellular translocation of organic cations. Br. J. Pharmacol. 2011, 163, 546–555. [Google Scholar] [CrossRef] [Green Version]
- Vallance, P.; Leiper, J. Cardiovascular Biology of the Asymmetric Dimethylarginine:Dimethylarginine Dimethylaminohydrolase Pathway. Arter. Thromb. Vasc. Biol. 2004, 24, 1023–1030. [Google Scholar] [CrossRef]
- Juliano, R.; Ling, V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim. Biophys. Acta Biomembr. 1976, 455, 152–162. [Google Scholar] [CrossRef]
- Thiebaut, F.; Tsuruo, T.; Hamada, H.; Gottesman, M.M.; Pastan, I.; Willingham, M.C. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc. Natl. Acad. Sci. USA 1987, 84, 7735–7738. [Google Scholar] [CrossRef] [Green Version]
- Meissner, K.; Sperker, B.; Karsten, C.; Zu Schwabedissen, H.E.M.; Seeland, U.; Böhm, M.; Bien, S.; Dazert, P.; Kunert-Keil, C.; Vogelgesang, S.; et al. Expression and Localization of P-glycoprotein in Human Heart. J. Histochem. Cytochem. 2002, 50, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Schinkel, A.H.; Jonker, J.W. Mammalian drug efflux transporters of the ATP binding cassette (ABC) family: An overview. Adv. Drug Deliv. Rev. 2003, 55, 3–29. [Google Scholar] [CrossRef]
- Schinkel, A.H. P-Glycoprotein, a gatekeeper in the blood–brain barrier. Adv. Drug Deliv. Rev. 1999, 36, 179–194. [Google Scholar] [CrossRef]
- Hunter, J.; Hirst, B.H. Intestinal secretion of drugs. The role of P-glycoprotein and related drug efflux systems in limiting oral drug absorption. Adv. Drug Deliv. Rev. 1997, 25, 129–157. [Google Scholar] [CrossRef]
- Fromm, M.F. Importance of P-glycoprotein at blood–tissue barriers. Trends Pharmacol. Sci. 2004, 25, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Staud, F.; Ceckova, M.; Micuda, S.; Pavek, P. Expression and Function of P-Glycoprotein in Normal Tissues: Effect on Pharmacokinetics. In Advanced Structural Safety Studies; Springer Science and Business Media LLC: Berlin, Germany, 2009; Volume 596, pp. 199–222. [Google Scholar]
- Parker, R.B.; Yates, C.R.; Laizure, S.C.; Weber, K.T. P-Glycoprotein Modulates Aldosterone Plasma Disposition and Tissue Uptake. J. Cardiovasc. Pharmacol. 2006, 47, 55–59. [Google Scholar] [CrossRef]
- Eap, C.B.; Bochud, M.; Elston, R.C.; Bovet, P.; Maillard, M.P.; Nussberger, J.; Schild, L.; Shamlaye, C.; Burnier, M. CYP3A5 and ABCB1 Genes Influence Blood Pressure and Response to Treatment, and Their Effect Is Modified by Salt. Hypertension 2007, 49, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Bochud, M.; Eap, C.B.; Maillard, M.P.; Johnson, T.; Vollenweider, P.; Bovet, P.; Elston, R.C.; Bergmann, S.; Beckmann, J.S.; Waterworth, D.; et al. Association of ABCB1 genetic variants with renal function in Africans and in Caucasians. BMC Med. Genom. 2008, 1, 21. [Google Scholar] [CrossRef] [Green Version]
| L-Arginine | Asymmetric Dimethylarginine (ADMA) | Symmetric Dimethylarginine (SDMA) | L-Homoarginine | |
|---|---|---|---|---|
| Plasma concentration Reference values in healthy populations (2.5th–97.5th centile) | 41–114 µM [74]; 72.4–113.7 µM [75,76] | 0.41–0.96 µM [77] | 0.27–0.67 µM [77] | 1.6–2.6 µM [77]; 1.4–2.5 µM [78,79,80,81] |
| Source/synthesis | Diet (85–90%; ca. 5 g/day) [82] and 10–15% endogenous synthesis in the kidney (16 μM/kg/hr) [83,84] | Endogenous hydrolysis of proteins containing asymmetrically methylated L-arginine residues [85]; possible contribution of diet [86] | Endogenous hydrolysis of proteins containing symmetrically methylated L-arginine residues [85]; possible contribution of diet [86] | Endogenous synthesis by glycine amidino transferase (AGAT) [87]; possible contribution of diet [88] |
| Metabolism | Major enzymes: L-arginine: glycine amidino transferase (AGAT), NO synthases (NOS; 3 isozymes), arginases (2 isozymes), and L-arginine decarboxylase [89] | Dimethylarginine dimethylaminohydrolase 1 (DDAH1) accounts for > 80% of the metabolic elimination [25]; Dimethylarginine dimethylaminohydrolase 1 (DDAH2) [90]; AGXT2 [26] | Primarily by renal excretion [91]; AGXT2 [92,93] | Metabolized by alanine—glyoxylate aminotransferase 2 (AGXT2) [94]; arginase and NO-Synthases [95] (relative contribution are uncertain) |
| Renal clearance | ~0.14 mL/min [96,97,98,99,100] | ~69 mL/min [101] | ~71 mL/min [101] | ~0.7 mL/min [78,79,80,81,102] |
| Association of plasma concentration and renal clearance | Positive correlation with estimated glomerular filtration rate (eGFR) [74] | Weak inverse correlation with eGFR [103] | Strong inverse correlation with eGFR, like creatinine [103] | Positive correlation with eGFR [104] |
| Association with mortality and cardiovascular disease | In most studies no independent biomarker for cardiovascular events or total mortality [105]; In short term supplementation studies associated with functional improvements of endothelial function [106] | Elevated plasma concentration independently predicts total and cardiovascular mortality [30] | Elevated plasma concentration independently predicts total and cardiovascular mortality [30] | Low plasma concentration independently predicts total and cardiovascular mortality [33,107,108] |
| Gene Human/Rodent. | Protein | Alternative Protein Name, (Assoc. with) | Transport Type |
|---|---|---|---|
| SLC3A1/SLc3a1 | rBAT | NBAT | Chaperone (not transporting) |
| SLC3A2/SLc3a2 | 4F2hc | CD98hc, FRP | Chaperone (not transporting) |
| SLC6A14/SLc6a14 | ATB0,+ | β-alanine carrier | F |
| SLC7A1/SLc7a1 | CAT1 | System y+, ATRC1 | F (non-obligatory E) |
| SLC7A2/Slc7a2 | CAT2A & CAT2B | System y+, ATRC2 | F (non-obligatory E) |
| SLC7A3/SLc7a3 | CAT3 | System y+, ATRC3 | F (non-obligatory E) |
| SLC7A6/SLc7a6 | y+LAT2 | System y+L [4F2hc] | E (intracellular cationic amino acids/Na+-independent against extracellular large neutral amino acids/Na+-dependent) |
| SLC7A7 | y+LAT1 | System y+L [4F2hc] | E (intracellular cationic amino acids/Na+-independent against extracellular large neutral amino acids/Na+-dependent) |
| SLC7A9/SLc7a9 | b0,+AT | System b0,+ [rBAT] | E (preferentially extracellular cationic amino acid and cystine against intracellular neutral amino acid) |
| SLCO4C1/Slco4c1 | OATP4C1 | SLC21A2, OATP4C1, OATPX, OATP-H | F |
| SLC22A2/SLc22a2 | OCT2 | None | F |
| SLC25A2/SLc25a2 | ORNT2 | ORCT2 | F (non-obligatory E: homoexchange, heteroexchange, unidirectional) |
| SLC25A15/SLc25a15 | ORNT1 | ORC1 | F (non-obligatory E: homoexchange, heteroexchange, unidirectional) |
| SLC25A29 | ORNT3 | ORC3 | F (non-obligatory E: homoexchange, heteroexchange, unidirectional) |
| SLC38A4/SLc38a4 | SNAT4 | ATA3 | F |
| SLC38A7 | SNAT7 | None | F |
| SLC38A8 | SNAT8 | None | F |
| SLC47A1 | MATE1 | None | E |
| ABCB1 | P-gp | None | F |
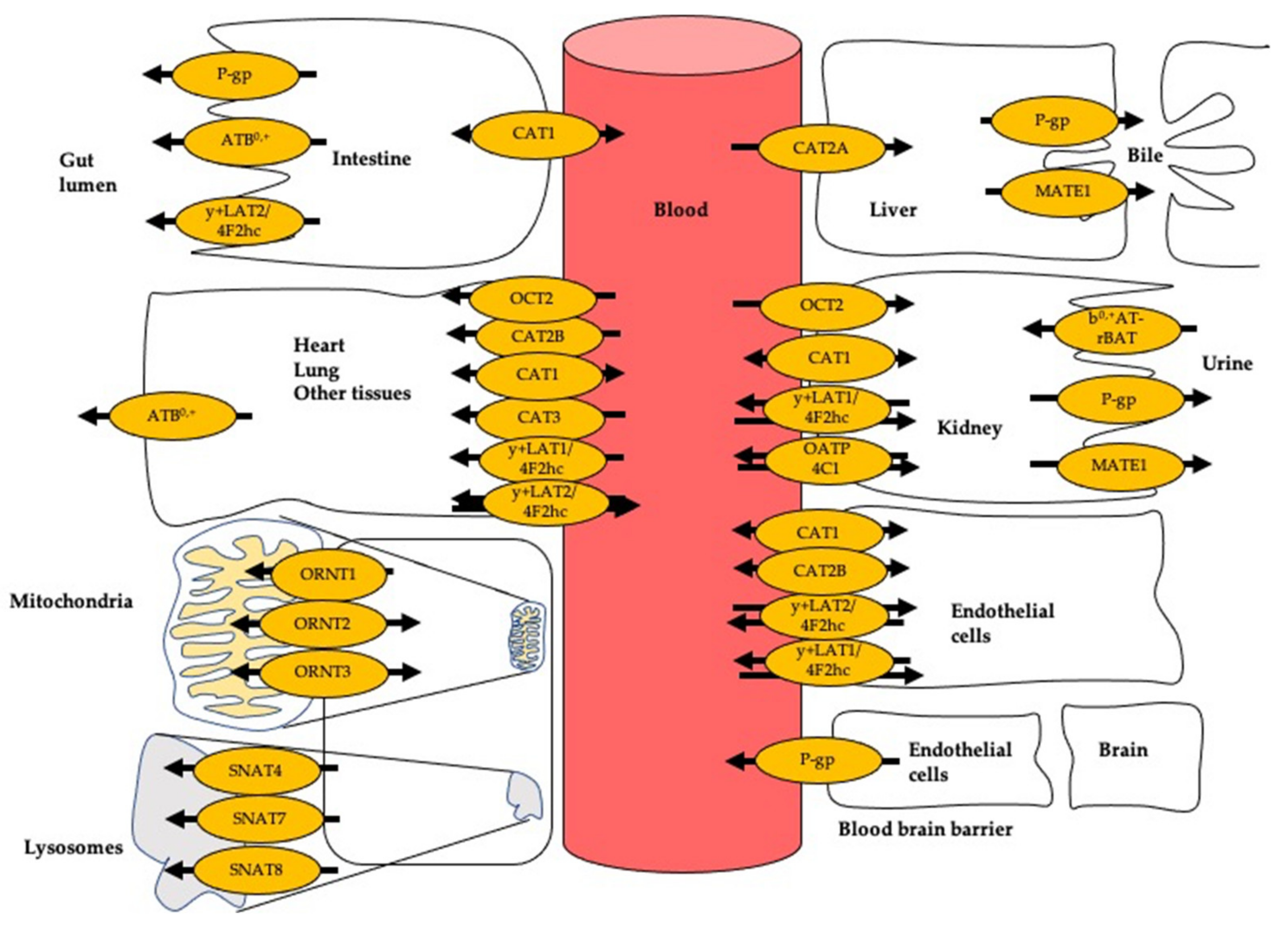
| Organ/Tissue | Transporter | |
|---|---|---|
| Kidney | Tubular cells (luminal side) | b0,+AT-rBAT, MATE1, and P-gp |
| Tubular cells (blood side) | CAT1, OCT2, OATP4C1, and y+LAT1-4F2hc | |
| Unspecified | CAT1 | |
| Intestines | ATB0,+, OCT2, CAT1, and P-gp | |
| Liver | CAT2A, SNAT4, P-gp, and MATE1 | |
| Blood vessel | Endothelial cells | CAT1, CAT2B, y+LAT1, and y+LAT2 |
| Heart | CAT1 | |
| Brain | CAT1, CAT3, y+LAT1-4F2hc, ATB0,+, OCT2, SNAT7, and SNAT8 | |
| Others | Monocytes | y+LAT1-4F2hc |
| Lymphocytes | CAT2B | |
| Erythrocytes | y+LAT1-4F2hc, y+LAT2-4F2hc, | |
| Placenta | y+LAT1-4F2hc, y+LAT2-4F2hc, CAT1, CAT2B, CAT3, OCT2, and SNAT4 | |
| Platelets | y+LAT1-4F2hc | |
| Macrophages | CAT2B | |
| Skin | CAT1 | |
| Intracellular | Lysosomes | SNAT7, and SNAT8 |
| Mitochondria | ORNT1, ORNT2, and ORNT3 | |
| Transporter (Gene/Protein) | Function | Relevance to Pathophysiology of Cardiovascular System |
|---|---|---|
| SLC7A1/CAT1 | Selective supplier of L-arginine to endothelial NOS; involved in interorgan transport of ADMA | NO-mediated endothelial function [12]; reduced activity increases risk for endothelial dysfunction and hypertension [111,112] |
| SLC7A2/CAT2 | CAT2A Hepatic uptake of ADMA and SDMA from the circulation. CAT2B uptake of L-arginine by Immune cells. | Downregulation of CAT2 expression by miRNA associated with increased risk for myocardial infarction [142] |
| SLC7A-SLC3A2/y+LAT2-4F2hc | High affinity uptake of L-arginine | Loss or a very low activity leads to increase predisposition for CVD [106] |
| SLC7A7-SLC3A2/y+LAT1-4F2hc | Mediating cellular ADMA efflux | Decreased expression associated with endothelial dysfunction [143] |
| SLC7A9-SLC3A1/b0,+AT-rBAT | Renal tubular reabsorption of L-arginine back into the circulation | Involved in L-arginine homeostasis; loss of function or reduced activity leads to increase risk of hypertension [144,145] |
| SLCO4C1/OATP4C1 | Possibly related to renal tubular efflux of ADMA into the urine | Altered expression associated with increased risk of hypertension [146] |
| SLC22A2/OCT2 | Mode of action still unknown | Impaired expression associated with essential hypertension [147] |
| Gene | Protein | Pathophysiological and Clinical Associations | Prototypic Substrate(s) | Prototypic Inhibitor(s) | Species (Expression System) | Evidence for Transport (Direct = D or Indirect = I) | |||
|---|---|---|---|---|---|---|---|---|---|
| L-Arginine | L-Homoarginine | ADMA | SDMA | ||||||
| SLC6A14; SLc6a14 | ATB0,+ | Susceptibility to secondary diseases in cystic fibrosis [184,185] | Cationic amino acids and neutral amino acids, excluding aspartate and glutamate [43] | Alpha-methyl-DL-tryptophan (α-MT) [50] | Human (human bronchial epithelial cells) [186] | (I) KM: 80 ± 8.9 µM | - | - | - |
| Human (Xenopus oocytes) [39] | (D) KM: 104 ± 35 µM | - | - | - | |||||
| Rat (human pneumocytes) [43] | (D) KM: 500 ± 110 µM; VMax: 33.3 ± 2.1 nmol × mg protein−1 × min−1 | - | - | - | |||||
| Rabbit (human cornea) [187] | (D) KM: 306 ± 72 µM; VMax: 0.12 ± 0.01 nmol × mg protein−1 × min−1 | - | - | - | |||||
| SLC7A1; SLc7a1 | CAT1 | Knockout mice: lethal [109]; knockdown mice: impaired fetal growth [110]; liver cancer [188]; colorectal cancer [189], breast cancer [190]; hypertension [112,113] | Cationic amino acids (L-arginine, L-ornithine, L-lysine, L-homoarginine, ADMA, SDMA) | N-Ethylmaleimide (NEM) [191] | Human (Xenopus oocytes) [72] | (D) KM: 110–160 µM; VMax: 1.6–1.8 nmol L-Arg/oocyte/h | - | - | - |
| Human (human embryonic kidney/HEK cells) [71] | (D) KM: 519 ± 36 µM; VMax: 11 ± 0.2 nmol × mg protein−1 × min−1; IC50: 227 µM (inhibitor ADMA) | - | (D) KM: 183 ± 21 µM; VMax: 26.9 ± 0.8 nmol × mg protein−1 × min−1; IC50: 758 µM (inhibitor L-arginine) | (I) IC50: 789 µM (inhibitor L-arginine); 273 µM (inhibitor ADMA) | |||||
| Human (HEK cells) [73] | (D) IC50: 1320 µM (inhibitor L-homoarginine) | (D) KM: 175 ± 7 µM; VMax: 12 ± 0.1 nmol × mg protein−1 × min−1; IC50: 1320 µM (inhibitor L-arginine) | (D) IC50: 642 µM (inhibitor L-homoarginine) | - | |||||
| Human (human fibroblast) [192] | (I) KM: 30–200 µM | ||||||||
| Human (human fibroblast) [193] | - | (I) KM: 40 µM | - | - | |||||
| Human (human hepatocytes) [57] | - | (I) KM: 300 µM | - | - | |||||
| Mouse (Xenopus oocytes) [64] | (D) KM: 70 µM; VMax: 190 nmol L-Arg/oocyte/h | - | - | - | |||||
| Mouse (Xenopus oocytes) [194] | (D) KM: 77 µM; VMax: 0.98 nmol L-Arg/oocyte/h | - | - | - | |||||
| Mouse (Xenopus oocytes) [72] | (D) KM: 140–250 µM; VMax: 1.1–1.6 nmol L-Arg/oocyte/h | - | - | - | |||||
| Mouse (human embryonic fibroblast) [154] | (D) KM: 107.1 ± 4.1 µM; VMax: 0.42 ± 0.01 nmol × mg protein−1 × min−1 | - | - | - | |||||
| SLC7A2A; SLc7a2A | CAT2A | L-argininemia [152] | Cationic amino acids (L-arginine, L-ornithine, L-lysine, L-homoarginine, ADMA, SDMA) | NEM [191,195] | Human (Xenopus oocytes) [72] | (D) KM: 3360–3,900 µM; VMax: 2.2–8.4 nmol L-Arg/oocyte/h | - | - | - |
| Human (HEK cells) [123] | (D) KM: 3510 ± 419 µM; VMax: 19.5 ± 0.7 nmol × mg protein−1 × min−1 | - | (D) KM: ~ 3033 ± 675 µM; VMax: ~ 11.8 ± 1.2 nmol × mg protein−1 × min−1 | - | |||||
| Human (HEK cells) [73] | (D) IC50: 3265 µM (inhibitor L-homoarginine) | (D) Saturation not reached | (D) IC50: 9244 µM (inhibitor L-homoarginine) | - | |||||
| Mouse (xenopus oocytes) [72] | (D) KM: 2100–5,200 µM; VMax: 3.9–7.1 nmol L-Arg/oocyte/h | - | - | - | |||||
| SLC7A2B; SLc7a2B | CAT2B | L-argininemia [152] | Cationic amino acids (L-arginine, L-ornithine, L-lysine, L-homoarginine, ADMA, SDMA) | NEM [191] | Human (Xenopus oocytes) [72] | (D) KM: 320–730 µM; VMax: 1.2–4.0 nmol L-Arg/oocyte/h | - | - | - |
| Human (Xenopus oocytes) [70] | - | (D) Transported | |||||||
| Human (HEK cells) [123] | (D) KM: 952 ± 92 µM; VMax: 15.3 ± 0.4 nmol × mg protein−1 × min−1 | - | (D) KM: ~ 4021 ± 532 µM; VMax: 14.3 ± 1.0 nmol × mg protein−1 × min−1 | - | |||||
| Human (HEK cells) [73] | - | (D) KM: 523 ± 35 µM; VMax: 11 ± 0.2 nmol × mg protein−1 × min−1 | - | - | |||||
| Mouse (Xenopus oocytes) [72] | (D) KM: 250–380 µM; VMax: 1.1–3.4 nmol L-Arg/oocyte/h | - | - | - | |||||
| Mouse (Xenopus oocytes) [196] | (D) KM: 187 ± 28 µM | - | - | - | |||||
| SLC7A3; SLc7a3 | CAT3 | Autism spectrum disorder [156]; papillary thyroid carcinoma [197] | Cationic amino acids (L-arginine, L-ornithine, L-lysine) | NEM [191] | Human (Xenopus oocytes) [153] | (D) KM: 450 ± 130 µM; VMax: 1.4 ± 0.3 nmol L-Arg/oocyte/h | - | - | - |
| Mouse (Xenopus oocytes) [155] | (D) KM: 40–60 µM; VMax: 16 to 60 nmol L-Arg/oocyte/h | - | - | - | |||||
| Rat (COS7) [198] | (D) KM: 103 ± 12 µM | - | - | - | |||||
| SLC7A9/SLC3A1; SLc7a9/SLc3a1 | b0,+AT/rBAT | Cystinuria [199]; breast cancer [200] Increased prevalence of hypertension [144,145] | Cystine, Cationic amino acids (L-arginine, L-ornithine, L-lysine), large neutral amino acids (leucine, glutamine) | Heavy metal (lead and mercury) [201] | Human (COS-1 cells) [175] | (I) Transported | - | - | - |
| Human (COS-7 cells) [179] | (D) KM: 108 µM; VMax: 0.65 nmol × mg protein−1 × min−1 | - | - | - | |||||
| Human (MDCK cells) [180] | (D) KM: 179 µM | - | - | - | |||||
| Human (cystinuric patients) [100] | (I) Argininuria | (I) Homoarginiuria | - | - | |||||
| Human (Xenopus oocytes) [179] | (D) Influx (KM: 85 ± 7 µM; VMax: 211 ± 11 nmol L-Arg/oocyte/h); efflux (KM: 65 ± 5 µM; VMax: 6.1 ± 0.2 nmol L-Arg/oocyte/h) | - | - | - | |||||
| Mouse (Xenopus oocytes)[202] | (D) KM: 72 ± 35 µM | - | - | - | |||||
| Mouse (COS-7) [203] | (D) KM: 203 µM; VMax: 2570 nmol × mg protein−1 × min−1 | - | - | - | |||||
| Rabbit (Xenopus oocytes) [204] | (D) KM: 105 µM; VMax: 29 nmol L-Arg/oocyte/h | - | - | - | |||||
| SLC7A6/ SLC3A2 | y+LAT2-4F2hc | Lysinuric protein intolerance [205] | Neutral amino acids (L-glutamine, L-leucine, L-glycine) and cationic amino acids (L-arginine, L-ornithine, L-lysine) | - | Human (human fibroblast) [205] | (D) KM: 145 ± 28 µM; VMax: 1479 ± 0.09 μmol × mg protein−1 × min−1 | - | - | - |
| Human (Xenopus oocytes) [159] | (D) KM: 0.12–0.14 µM | - | - | - | |||||
| SLC7A7/SLC3A2; SLc7a7/SLc3a2 | y+LAT1-4F2hc | Lysinuric protein intolerance [206]; intrauterine growth retardation [207]; endothelial dysfunction [106] | Neutral amino acids (L-leucine, L-valine) and cationic amino acids (L-arginine, L-lysine, L-ornithine) | - | Human 4F2hc and mouse y+LAT1 (oocytes) [162] | (I) Transported | - | - | - |
| Human (MDM) [205] | (D) KM: 182 ± 35 µM; VMax: 3822 ± 0.24 μmol × mg protein−1 × min−1 | - | - | - | |||||
| SLC214C1 | OATP4C1 | Obesity [208]; endometrial cancer [209]; digoxin disposition in cardiac insufficiency [210] | Amphipathic organic compounds, bromsulphthalein (BSP), bile salts, bilirubin, estrogen conjugates, thyroid hormones, neutral steroid, digoxin, methotrexate | Nicardipine, spironolactone, fluvastatin, crizotinib, levofloxacin, clarithromycin, ritonavir, saquinavir, quinidine, and verapamil [211] | Human (HEK cells) [212] | - | (D) KM: 49.9 µM | (D) KM: 232.1 µM | - |
| Human (madin-darby canine kidney/MDCK cells) [213] | (D) KM: 48.1 ± 5.7 μM | (D) KM: 49.9 ± 9.6 μM | (D) KM: 232.1 ± 78.9 μM | - | |||||
| SLC22A2 | OCT2 | Potential drug-drug interactions (metformin and cimetidine) [214] | 1- methyl-4-phenylpyridinium (MPP+), 4–4-dimethylaminostyryl-N-methylpyridinium (ASP+), histamine, tyramine, metformin [215] | Amitriptyline, doxepin, lansoprazole, pantoprazole, trimipramine [216,217] | Human (HEK cells) [123] | (D) KM: > 10,000 µM; VMax: > 50 nmol × mg protein−1 × min−1 | - | (D) KM: 967 ± 143 µM; VMax: 6.3 ± 0.3 nmol × mg protein−1 × min−1 | - |
| SLC25A2 | ORC2/ORNT2 | Early epileptic encephalopathy [218]; colorectal cancer [219] | Ornithine [220] | Spermine and spermidine [220] | Human (human proteoliposomes) [220] Human (human liposomes) [221] | (D) KM: 710 ± 90 µM; VMax: 1.2 ± 0.2 μmol × mg protein−1× min−1 | (D) Transported | (D) KM: 370 ± 40 µM; VMax: 0.31 ± 0.05 nmol × mg protein−1 × min−1 | - |
| SLC25A15 | ORC1/ORNT1 | Hyperornithinemia hyperammonemia-homocitrullinuria (HHH) syndrome [222] | L-ornithine, L-arginine, carnitine, and citrulline [220] | Citrulline, lysine, spermine, and spermidine [220] | Human (human proteoliposomes) [220] | (D) KM: 1580 ± 180 µM; VMax: 3 ± 0.4 μmol × mg protein−1× min−1 | (D) Transported | - | - |
| SLC25A29 | ORC3/ORNT3 | Hyperornithinemia hyperammonemia-homocitrullinuria (HHH) syndrome [223] | L-ornithine, L-arginine, carnitine, and citrulline [224] | Pyridoxal 5’-phosphate, tannic acid, HgCl2, mersalyl, and p-hydroxymercuribenzoate, NEM, and α-cyano-4-hydroxycinnamate [225] | Human (human proteoliposomes) [225] | (D) KM: 420 ± 40 µM; VMax: 0.237 ± 0.048 μmol × mg protein−1× min−1 | (D) Transported; Ki: 450 ± 70 µM (inhibitor L-arginine) | - | - |
| SLC38A4 | NAT3/ATA3 | Placental hypoplasia [226] | Neutral amino acids (L-glutamine, L-leucine, L-glycine) [227] | Alpha-(methylamino) isobutyric acid (MeAIB) [228] | Human (HRPE cells) [229] | (D) KM: 300 ± 40 µM; L-arginine inhibited glycine uptake 31% | - | - | - |
| SLC38A7 | SNAT7 | - | Neutral amino acids (L-glutamine, L-leucine, L-glycine) [227] | (MeAIB) [228] | Human (Xenopus oocytes) [230] | (I) Transported (uptake 4-fold) | - | - | - |
| SLC38A8 | SNAT8 | Foveal hypoplasia [231] | Neutral amino acids (Lglutamine, L-leucine, L-glycine) [227] | (MeAIB) [228] | Human (Xenopus oocytes) [232] | (I) Transported (uptake 1.4-fold) | - | - | - |
| SLC47A1 | MATE1 | Potential drug-drug interactions (metformin) [233] | Tetraethylammonium, metformin, salicylic acid, quinine, tenofir, cisplatin [217,233,234] | Cimetidine, imatinib, clonidine, diltiazem, imipramine, ranitidine, chlorhexidine [233,234] | Human (HEK cells) [123] | (D) Transported (uptake ratio 1.3) | - | (D) Transported (uptake ratio 1.1) | |
| MDR1/ ABCB1 | P-gp | Potential drug-drug interactions (digoxin, rifampin, quinidine, St. John’s wort, talinolol, fexofenadine) [235] | Cholesterols, steroid hormones, bilirubin, and numerous drugs (e.g., digoxin, quinidine, ritonavir, etoposide, and dexamethasone) [236,237] | Verapamil, atorvastatin, cyclosporine, progesterone, quinidine, carvedilol, bromocriptine, erythromycin [235,237,238] | Human (MDCK cells) [213] | - | (D) Transported (uptake ratio 1.4 at 50 μM) | (D) Transported (uptake ratio 1.2 at 50 μM) | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banjarnahor, S.; Rodionov, R.N.; König, J.; Maas, R. Transport of L-Arginine Related Cardiovascular Risk Markers. J. Clin. Med. 2020, 9, 3975. https://doi.org/10.3390/jcm9123975
Banjarnahor S, Rodionov RN, König J, Maas R. Transport of L-Arginine Related Cardiovascular Risk Markers. Journal of Clinical Medicine. 2020; 9(12):3975. https://doi.org/10.3390/jcm9123975
Chicago/Turabian StyleBanjarnahor, Sofna, Roman N. Rodionov, Jörg König, and Renke Maas. 2020. "Transport of L-Arginine Related Cardiovascular Risk Markers" Journal of Clinical Medicine 9, no. 12: 3975. https://doi.org/10.3390/jcm9123975
APA StyleBanjarnahor, S., Rodionov, R. N., König, J., & Maas, R. (2020). Transport of L-Arginine Related Cardiovascular Risk Markers. Journal of Clinical Medicine, 9(12), 3975. https://doi.org/10.3390/jcm9123975






