Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis
Abstract
:1. Introduction
2. Methods
2.1. Aim
2.2. Methodological Approach
2.3. Research Question
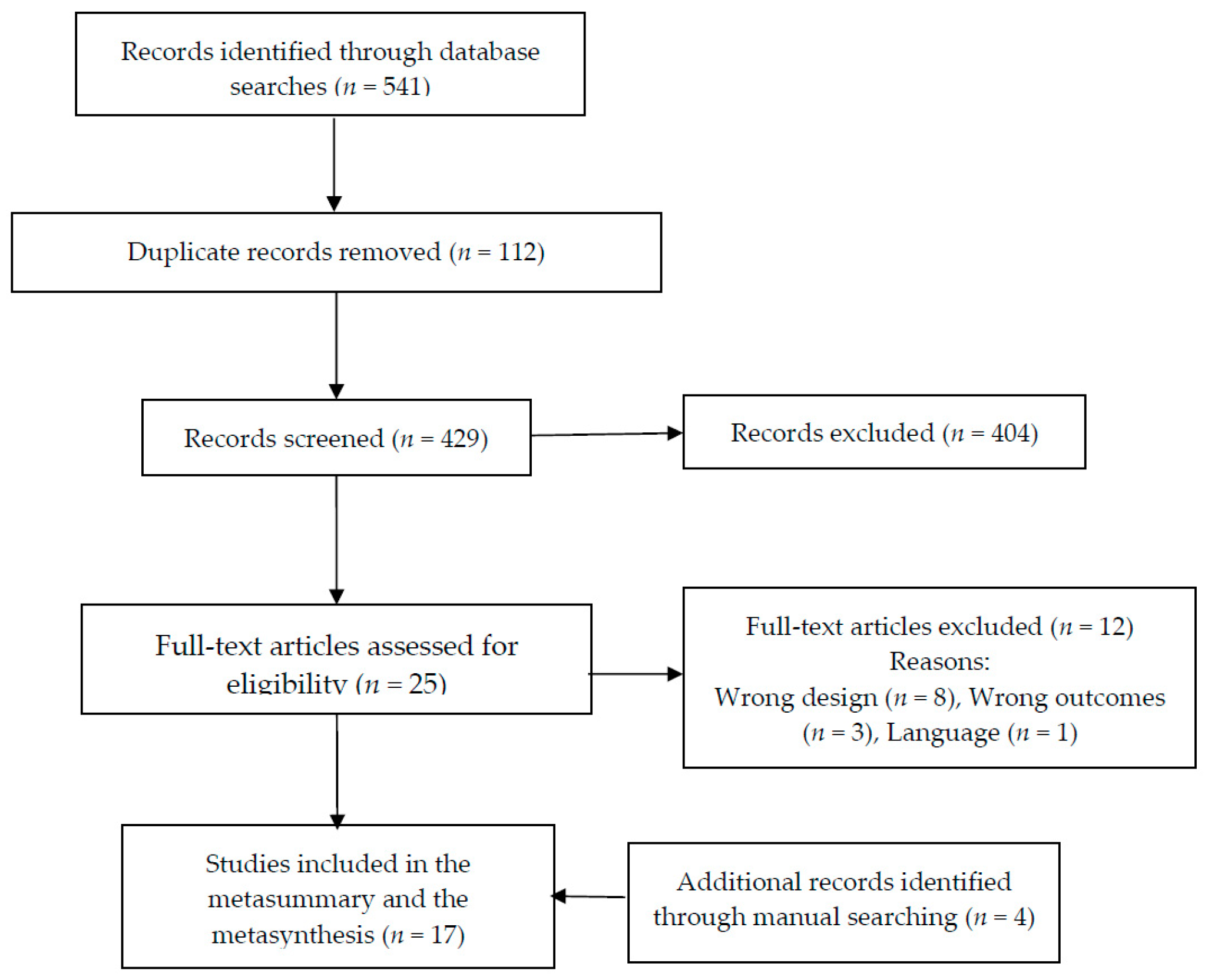
2.4. Approach to Searching
2.5. Inclusion Criteria
2.6. Data Sources
2.7. Electronic Search Strategy
2.8. Study Screening Methods and Appraisal of the Methodological Quality
2.9. Analyzing and Synthesizing Qualitative Findings
3. Results
3.1. Metasummary
3.2. Metasynthesis
3.2.1. Experience of Poor Sleep Quality in FM
- (1)
- Evaluation of Poor Sleep Quality
“Sleep, or lack of it, is the worst thing about this condition for me […] It’s just another way my body has betrayed me.”
“I can, initially, go to sleep, but it’s staying asleep that’s very hard. And then, I got to sleep tired and I wake up exhausted, and it’s frustrating.”
“Sleeplessness nights ... can you see the black circles under my eyes, because I wake up at 2 o’clock in the morning, then I wake up and feel right awake...and the next day I feel tired, I just want to sleep on but I have to get up and go to work ... I am extremely physically tired ... I am so tired I just can’t function as a normal person.”
“The fatigue, it’s number one, because I can deal with the pain, at least up to a certain point, but the fatigue there’s nothing you can do besides sleep. There is no way to help that. There’s no pill you can take, there’s no medicine.”
“I could sleep 20 hours and still be tired. That is terrible.”
“I feel constantly in pain, which obviously when I don’t get enough sleep will aggravate that, and then because I’ve aggravated pain I don’t get enough sleep. So I am on a vicious cycle, I can’t sleep properly because of the pain, and I can’t, because I am not sleeping, I then get in more pain.”
“I don’t hardly ever sleep with my husband anymore, because I disturb his sleep so much of the time with my tossing and turning, trying to get comfortable, getting in and out of bed, because I can’t get comfortable.”
“It’s not just the pain and the fatigue...it’s the nonrestorative sleep...it’s a vicious circle because if you don’t get enough sleep you feel pain more acutely...you’re more tired and unable to sleep well.”
“I will be thinking and, and trying to explain stuff to you, but my mind will just go completely blank. That gets worse on certain days, obviously with less sleep, but on other days I can sort of string together.”
“[After a night shift] I slept maybe an hour or hour and a half a day … you know how it is when you don’t sleep practically at all for weeks and months … In fact, I was practically sleepless for years …”
"It’s that sensation of really I have switched off, I am not aware of anything. That you know, those three hours where maybe the following day my husband said to me, “Oh did you hear the thunderstorm last night?” “No,” because it happened on those three hours and I didn’t hear anything. I didn’t hear the thunderstorm, I didn’t notice the light, nothing, and that is for me a proper sleep. When I’m aware of everything else I’m not, and I get up noticing that I have not slept properly.”
- (2)
- Response to Poor Sleep Quality
“The not sleeping and then not being able to function the next day when you need to perform at work …—when you’re being paid and you’re meant to work and you can’t function, it’s horrible, it’s really horrible because you feel like a failure.”
“I don’t feel like I can sleep. ... This is aging me, I can feel it. Sometimes I just hate life.”
“Sleep, or lack of it, is the worst thing about this condition for me. I have christened my bedroom “the torture chamber.”
“If there’s something on my mind, that makes me a bit worried about sleeping, I don’t know what it is but I sort of need to try and get to the bottom of it, but I sort of have this fear of going to bed.”
3.2.2. Poor Sleep Quality Management Strategies in FM
- (1)
- Management Strategies to Favor Sleep
“I am on Amytriptiline to help with my sleep and other tablets … I only take them when it is right for my body. I don’t like to be taken as a guinea pig. I don’t trust staff to deal with me in that way. I am the only person who knows what it feels like to be ill, and what is good for my body, I don’t like other people to tell me and to control me.”
“I know that it’s an absolute crucial thing to get a good night’s sleep; to go to bed at the same time; eating on time... so everything has to be regular. And the more regular it is, the better I feel.”
“I put earplugs in and I find when I put earplugs in I seem to sleep different … although I don’t like things in my ears, if it means I’m going to sleep a bit better, so whether that’s about noise, although it’s very quiet where I live, so I don’t know, I think I’m just looking for answers.”
“Sometimes I think I can get back to sleep, so I wait to see if I can and I think come on and I just lie there and hopefully I can get back to sleep easily again, um, but more often than not, I can’t so after I try for about 15 to 20 minutes and if I can’t get back to sleep after that time then as I say I put the television on and it’ll refocus me and if I fall back to sleep, good.”
3.2.3. Managing the Consequences of a Sleepless Night
“I try to get out of bed every day regardless of how I feel. I’m trying to function, so I take the various medications … in the hopes that while it causes other problems it will at least allow me to continue to have a life.”
“I might have to go to bed for a couple of hours and then I’ll be alright for the evening, because I know they advise you not to go to bed don’t they, but I can’t physically not and I find it makes me feel better actually if I do, so for me it works better, so you I’ve learnt to do what suits me rather than what I’m told to do you know they say you muck up your body clock up if you sleep in the day but for me it doesn’t work that way.”
4. Discussion
4.1. Rigour
4.2. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strategy for PubMed
References
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar]
- Cabo-Meseguer, A.; Cerdá-Olmedo, G.; Trillo-Mata, J.L. Fibromialgia: Prevalencia, perfiles epidemiológicos y costes económicos. Med. Clin. (Barc.) 2017, 149, 441–448. [Google Scholar] [PubMed]
- Wolfe, F.; Walitt, B.; Perrot, S.; Rasker, J.J.; Häuser, W. Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias. PLoS ONE 2018, 13, e0203755. [Google Scholar]
- Marques, A.P.; Santo, A.D.S.D.E.; Berssaneti, A.A.; Matsutani, L.A.; Yuan, S.L.K. Prevalence of fibromyalgia: Literature review update. Rev. Bras. Reumatol. (Engl. Ed.) 2017, 57, 356–363. [Google Scholar]
- Joshi, V.L.; Chopra, A. Is there an urban-rural divide? Population surveys of rheumatic musculoskeletal disorders in the Pune Region of India using the COPCORD Bhigwan model. J. Rheumatol. 2009, 36, 614–622. [Google Scholar]
- Haq, S.A.; Darmawan, J.; Islam, M.N.; Uddin, M.Z.; Das, B.B.; Rahman, F.; Chowdhury, M.A.J.; Alam, M.N.; Mahmud, T.A.K.; Chowdhury, M.R.; et al. Prevalence of rheumatic diseases and associated outcomes in rural and urban communities in Bangladesh: A COPCORD study. J. Rheumatol. 2005, 32, 348–353. [Google Scholar]
- Rodriguez-Amado, J.; Peláez-Ballestas, I.; Sanin, L.H.; Esquivel-Valerio, A.J.; Burgos-Vargas, R.; Pérez-Barbosa, L.; Riega-Torres, J.; Garza-Elizondo, M.A. Epidemiology of rheumatic diseases. A community-based study in urban and rural populations in the state of Nuevo Leon, Mexico. J. Rheumatol. 2011, 38, 9–14. [Google Scholar]
- Turhanoğlu, A.D.; Yilmaz, Ş.; Kaya, S.; Dursun, M.; Kararmaz, A.; Saka, G. The Epidemiological Aspects of Fibromyalgia Syndrome in Adults Living in Turkey: A Population Based Study. J. Musculoskelet. Pain 2008, 16, 141–147. [Google Scholar]
- Carmona, L.; Gabriel, R.; Ballina, J.; Laffon, A.; Grupo de Estudio EPISER. Proyecto EPISER 2000: Prevalencia de enfermedades reumáticas en la población española. Rev. Esp. Reumatol. 2001, 28, 18–25. [Google Scholar]
- Boomershine, C. Fibromyalgia: The Prototypical Central Sensitivity Syndrome. Curr. Rheumatol. Rev. 2015, 11, 131–145. [Google Scholar]
- Arnold, L.M.; Choy, E.; Clauw, D.J.; Goldenberg, D.L.; Harris, R.E.; Helfenstein, M.; Jensen, T.S.; Noguchi, K.; Silverman, S.L.; Ushida, T.; et al. Fibromyalgia and Chronic Pain Syndromes. Clin. J. Pain 2016, 32, 737–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sluka, K.A.; Clauw, D.J. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience 2016, 338, 114–129. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Solà, J. Central Sensitization: A Pathogenic Mechanism in Complex Undefined Diseases. Neurophychiatry J. 2019, 9, 2485–2490. [Google Scholar]
- Fleming, K.; Volcheck, M. Central Sensitization Syndrome and the Initial Evaluation of a Patient with Fibromyalgia: A Review. Rambam Maimonides Med. J. 2015, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnold, L.M.; Bennett, R.M.; Crofford, L.J.; Dean, L.E.; Clauw, D.J.; Goldenberg, D.L.; Fitzcharles, M.-A.; Paiva, E.S.; Staud, R.; Sarzi-Puttini, P.; et al. AAPT Diagnostic Criteria for Fibromyalgia. J. Pain 2019, 20, 611–628. [Google Scholar] [CrossRef] [Green Version]
- Rudin, N.J. Fibromyalgia. In Pain; Abd-Elsayed, A., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 693–697. [Google Scholar]
- Theadom, A.; Cropley, M. ‘This constant being woken up is the worst thing’—Experiences of sleep in fibromyalgia syndrome. Disabil. Rehabil. 2010, 32, 1939–1947. [Google Scholar] [CrossRef] [Green Version]
- Wagner, J.-S.; DiBonaventura, M.D.; Chandran, A.B.; Cappelleri, J.C. The association of sleep difficulties with health-related quality of life among patients with fibromyalgia. BMC Musculoskelet. Disord. 2012, 13, 199. [Google Scholar] [CrossRef] [Green Version]
- Andrade, A.; Vilarino, G.T.; Sieczkowska, S.M.; Coimbra, D.R.; Bevilacqua, G.G.; Steffens, R.D.A.K. The relationship between sleep quality and fibromyalgia symptoms. J. Health Psychol. 2020, 25, 1176–1186. [Google Scholar] [CrossRef]
- Theadom, A.; Cropley, M.; Humphrey, K.L. Exploring the role of sleep and coping in quality of life in fibromyalgia. J. Psychosom. Res. 2007, 62, 145–151. [Google Scholar] [CrossRef]
- Keskindag, B.; Karaaziz, M. The association between pain and sleep in fibromyalgia. Saudi Med. J. 2017, 38, 465–475. [Google Scholar] [CrossRef]
- Mun, C.J.; Davis, M.C.; Campbell, C.M.; Finan, P.H.; Tennen, H. Linking Nonrestorative Sleep and Activity Interference Through Pain Catastrophizing and Pain Severity: An Intraday Process Model Among Individuals With Fibromyalgia. J. Pain 2020, 21, 546–556. [Google Scholar] [CrossRef] [PubMed]
- Choy, E.H.S. The role of sleep in pain and fibromyalgia. Nat. Rev. Rheumatol. 2015, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Börsbo, B.; Liedberg, G.M.; Björk, M. Self-reported nonrestorative sleep in fibromyalgia—relationship to impairments of body functions, personal function factors, and quality of life. J. Pain Res. 2015, 8, 499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mannerkorpi, K.; Gard, G. Hinders for continued work among persons with fibromyalgia. BMC Musculoskelet. Disord. 2012, 13, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turk, D.C. Treatment of Patients with Fibromyalgia. In Psychological Approaches to Pain Management. A Practitioner’s Handbook; Turk, D.C., Gatchel, R.J., Eds.; The Guilford Press: New York, NY, USA, 2018; ISBN 0898622921. [Google Scholar]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Flub, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef]
- Tang, N.K.Y.; Goodchild, C.E.; Webster, L.R. Sleep and Chronic Pain. In Treatment of Chronic Pain by Integrative Approaches; Deer, T.R., Leong, M.S., Ray, A.L., Eds.; Springer: New York, NY, USA, 2015; pp. 203–217. ISBN 978-1-4939-1820-1. [Google Scholar]
- Lawson, K. Sleep Dysfunction in Fibromyalgia and Therapeutic Approach Options. OBM Neurobiol. 2020, 4, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Finfgeld-Connett, D. Generalizability and transferability of meta-synthesis research findings. J. Adv. Nurs. 2010, 66, 246–254. [Google Scholar] [CrossRef]
- Mohammed, M.A.; Moles, R.J.; Chen, T.F. Meta-synthesis of qualitative research: The challenges and opportunities. Int. J. Clin. Pharm. 2016, 38, 695–704. [Google Scholar]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. [Google Scholar] [CrossRef] [Green Version]
- Sandelowski, M.; Barroso, J. Synthesizing Qualitative Research Findings. In Handbook for Synthesizing Qualitative Research; Springer Publishing Company, LLC: New York, NY, USA, 2007; pp. 151–226. ISBN 0826156940. [Google Scholar]
- Haussler, S.C. Handbook for Synthesizing Qualitative Research. J. Contin. Educ. Nurs. 2008, 39, 47. [Google Scholar] [CrossRef]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CASP. CASP Qualitative Checklist: Critical Appraisal Skills Program. Available online: http://www.media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf (accessed on 18 March 2019).
- Humphreys, J.; Janson, S.; Donesky, D.A.; Dracup, K.; Lee, K.A.; Puntillo, K.; Faucett, J.A.; Aouizerat, B.; Miaskowski, C.; Baggott, C.; et al. Theory of Symptom Management. In Middle Range Theory for Nursing; Smith, M.J., Liehr, P.R., Eds.; Springer Publishing Company, LLC: New York, NY, USA, 2014; pp. 141–164. ISBN 978-0-8261-9551-7. [Google Scholar]
- Larson, J.P.; Crrieri-Kohlman, V.; Dodd, M.J.; Douglas, M.; Faucett, J.; Froelicher, E.; Gortner, S.; Halliburton, P.; Janson, S.; Lee, K.A.; et al. A Model for Symptom Management. Image J. Nurs. Scholarsh. 1994, 26, 272–276. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramlee, F.; Afolalu, E.F.; Tang, N.K.Y. Do People with Chronic Pain Judge Their Sleep Differently? A Qualitative Study. Behav. Sleep Med. 2016, 2002, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, D.; Álvarez Gallardo, I.C.; Wilson, I.; Hughes, C.M.; Davison, G.W.; Sañudo, B.; McVeigh, J.G. ‘Exercise to me is a scary word’: Perceptions of fatigue, sleep dysfunction, and exercise in people with fibromyalgia syndrome—A focus group study. Rheumatol. Int. 2018, 38, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.; Whipple, M.O.; Rhudy, L.M. Fibromyalgia Flares: A Qualitative Analysis. Pain Med. 2015, 17, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, L.; Mannix, S.; Arnold, L.M.; Burbridge, C.; Howard, K.; McQuarrie, K.; Pitman, V.; Resnick, M.; Roth, T.; Symonds, T. Assessment of sleep in patients with fibromyalgia: Qualitative development of the fibromyalgia sleep diary. Health Qual. Life Outcomes 2014, 12, 111. [Google Scholar] [CrossRef] [Green Version]
- Kengen Traska, T.; Rutledge, D.N.; Mouttapa, M.; Weiss, J.; Aquino, J. Strategies used for managing symptoms by women with fibromyalgia. J. Clin. Nurs. 2012, 21, 626–635. [Google Scholar] [CrossRef]
- Sallinen, M.; Kukkurainen, M.L.; Peltokallio, L.; Mikkelsson, M. “I’m tired of being tired”—Fatigue as experienced by women with fibromyalgia. Adv. Physiother. 2011, 13, 11–17. [Google Scholar] [CrossRef]
- Humphrey, L.; Arbuckle, R.; Mease, P.; Williams, D.A.; Samsoe, B.D.; Gilbert, C. Fatigue in fibromyalgia: A conceptual model informed by patient interviews. BMC Musculoskelet. Disord. 2010, 11, 216. [Google Scholar] [CrossRef] [Green Version]
- Martin, S.; Chandran, A.; Zografos, L.; Zlateva, G. Evaluation of the impact of fibromyalgia on patients’ sleep and the content validity of two sleep scales. Health Qual. Life Outcomes 2009, 7, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lempp, H.K.; Hatch, S.L.; Carville, S.F.; Choy, E.H. Patients’ experiences of living with and receiving treatment for fibromyalgia syndrome: A qualitative study. BMC Musculoskelet. Disord. 2009, 10, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnold, L.M.; Crofford, L.J.; Mease, P.J.; Burgess, S.M.; Palmer, S.C.; Abetz, L.; Martin, S.A. Patient perspectives on the impact of fibromyalgia. Patient Educ. Couns. 2008, 73, 114–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crooks, V.A. Exploring the altered daily geographies and lifeworlds of women living with fibromyalgia syndrome: A mixed-method approach. Soc. Sci. Med. 2007, 64, 577–588. [Google Scholar] [CrossRef]
- Cunningham, M.M.; Jillings, C. Individuals’ descriptions of living with fibromyalgia. Clin. Nurs. Res. 2006, 15, 258–273. [Google Scholar] [CrossRef]
- Söderberg, S.; Lundman, B.; Norberg, A. The meaning of fatigue and tiredness as narrated by women with fibromyalgia and healthywomen. J. Clin. Nurs. 2002, 11, 247–255. [Google Scholar] [CrossRef]
- Cudney, S.A.; Butler, M.R.; Weinert, C.; Sullivan, T. Ten Rural Women Living with Fibromyalgia Tell It Like It Is. Holist. Nurs. Pract. 2002, 16, 35–45. [Google Scholar] [CrossRef]
- Sturge-Jacobs, M. The experience of living with fibromyalgia: Confronting an invisible disability. Res. Theory Nurs. Pract. 2002, 16, 19–31. [Google Scholar] [CrossRef]
- Raymond, M.; Brown, J. Experience of fibromyalgia: Qualitative study. Can. Fam. Physician 2000, 46, 1100–1106. [Google Scholar]
- Dodd, M.; Janson, S.; Facione, N.; Faucett, J.; Froelicher, E.S.; Humphreys, J.; Lee, K.; Miaskowski, C.; Puntillo, K.; Rankin, S.; et al. Advancing the science of symptom management. J. Adv. Nurs. 2001, 33, 668–676. [Google Scholar] [CrossRef]
- Whibley, D.; AlKandari, N.; Kristensen, K.; Barnish, M.; Rzewuska, M.; Druce, K.L.; Tang, N.K. Sleep and Pain. Clin. J. Pain 2019, 35, 544–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kline, C. Sleep Quality. In Encyclopedia of Behavioral Medicine; Springer: New York, NY, USA, 2013; pp. 1811–1813. [Google Scholar]
- Moldofsky, H. The significance of the sleeping-waking brain for the understanding of widespread musculoskeletal pain and fatigue in fibromyalgia syndrome and allied syndromes. Jt. Bone Spine 2008, 75, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Litwiller, B.; Snyder, L.A.; Taylor, W.D.; Steele, L.M. The relationship between sleep and work: A meta-analysis. J. Appl. Psychol. 2017, 102, 682–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The Association of Sleep and Pain: An Update and a Path Forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herrero Babiloni, A.; De Koninck, B.P.; Beetz, G.; De Beaumont, L.; Martel, M.O.; Lavigne, G.J. Sleep and pain: Recent insights, mechanisms, and future directions in the investigation of this relationship. J. Neural Transm. 2020, 127, 647–660. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Mairesse, O.; Neu, D.; Leysen, L.; Danneels, L.; Cagnie, B.; Meeus, M.; Moens, M.; Ickmans, K.; Goubert, D. Sleep Disturbances in Chronic Pain: Neurobiology, Assessment, and Treatment in Physical Therapist Practice. Phys. Ther. 2018, 98, 325–335. [Google Scholar] [CrossRef]
- Haack, M.; Simpson, N.; Sethna, N.; Kaur, S.; Mullington, J. Sleep deficiency and chronic pain: Potential underlying mechanisms and clinical implications. Neuropsychopharmacology 2020, 45, 205–216. [Google Scholar] [CrossRef]
- Chinn, S.; Caldwell, W.; Gritsenko, K. Fibromyalgia Pathogenesis and Treatment Options Update. Curr. Pain Headache Rep. 2016, 20, 25. [Google Scholar] [CrossRef]
- Finan, P.H.; Smith, M.T. The comorbidity of insomnia, chronic pain, and depression: Dopamine as a putative mechanism. Sleep Med. Rev. 2013, 17, 173–183. [Google Scholar] [CrossRef] [Green Version]
- Buenaver, L.F.; Quartana, P.J.; Grace, E.G.; Sarlani, E.; Simango, M.; Edwards, R.R.; Haythornthwaite, J.A.; Smith, M.T. Evidence for indirect effects of pain catastrophizing on clinical pain among myofascial temporomandibular disorder participants: The mediating role of sleep disturbance. Pain 2012, 153, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.T.; Perlis, M.L.; Carmody, T.P.; Smith, M.S.; Giles, D.E. Presleep Cognitions in Patients with Insomnia Secondary to Chronic Pain. J. Behav. Med. 2001, 24, 93–114. [Google Scholar] [CrossRef] [PubMed]
- Galbiati, A.; Giora, E.; Sarasso, S.; Zucconi, M.; Ferini-Strambi, L. Repetitive thought is associated with both subjectively and objectively recorded polysomnographic indices of disrupted sleep in insomnia disorder. Sleep Med. 2018, 45, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Theadom, A.; Cropley, M. Dysfunctional beliefs, stress and sleep disturbance in fibromyalgia. Sleep Med. 2008, 9, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, N.; Phillips, L.A.; Pigeon, W.R.; Quigley, K.S.; Graff, F.; Litke, D.R.; Helmer, D.A.; Rath, J.F.; McAndrew, L.M. Coping with Medically Unexplained Physical Symptoms: The Role of Illness Beliefs and Behaviors. Int. J. Behav. Med. 2019, 26, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Estévez-López, F.; Maestre-Cascales, C.; Russell, D.; Álvarez-Gallardo, I.C.; Rodriguez-Ayllon, M.; Hughes, C.M.; Davison, G.W.; Sañudo, B.; McVeigh, J.G. Effectiveness of Exercise on Fatigue and Sleep Quality in Fibromyalgia: A Systematic Review and Meta-analysis of Randomized Trials. Arch. Phys. Med. Rehabil. 2020. [Google Scholar] [CrossRef]
| Authors and Year of Publication | Country | Sample Characteristics | Method of Approach | CASP Checklist n. of Items Fulfilled/n. of Items |
|---|---|---|---|---|
| Ramlee et al. [40] | England | n = 6 (3♀/3♂) Mean age = 49 years | Personal semi-structured interviews | 10/10 |
| Russell et al. [41] | North Ireland | n = 14 (12♀/2♂) | Focus groups | 10/10 |
| Vincent et al. [42] | USA | n = 44 (34♀/10♂) Mean age: 45 years | Open-ended interview administered electronically | 10/10 |
| Kleinman et al. [43] | n = 34 (30♀/4♂) Mean age = 47.8 years | Focus groups | 9/10 | |
| Traska et al. [44] | USA | n = 8♀ Mean age = 61 years | Interview group | 9/10 |
| Sallinen et al. [45] | Finland | n = 20♀ Mean age = 54 years | Narrative interview | 9/10 |
| Humphrey et al. [46] | USA Germany France | n = 40 Mean age = 48.7 years | Open-ended interviews | 10/10 |
| Theadom et al. [17] | England | n = 16 (14♀/2♂) Mean age (50.95 years) | Semi-structured interviews | 9/10 |
| Martin et al. [47] | USA | n = 20 (16♀/4♂) Mean age = 50.3 years | Personal structured interviews | 9/10 |
| Lempp et al. [48] | England | n = 12 (11♀/1♂) Mean age = 49 years | Personal semi-structured interviews | 9/10 |
| Arnold et al. [49] | USA | n = 48♀ Mean age = 51 years | Focus groups | 9/10 |
| Crooks [50] | Canada | n = 55♀ | Personal semi-structured interviews | 9/10 |
| Cunningham et al. [51] | Canada | n = 8 (7♀/1♂) Age range 30-70 | Personal in-depth interviews | 9/10 |
| Söderberg et al. [52] | Sweden | n = 25♀ Mean age = 46.8 years | Personal narrative interviews | 9/10 |
| Cudney et al. [53] | USA | n = 10♀ | Unstructured, online support group | 9/10 |
| Sturge-Jacobs [54] | Canada | n = 9♀ Age range 20-57 years | Personal unstructured interviews | 10/10 |
| Raymond and Brown [55] | Canada | n = 7 (6♀/1♂) | Personal in-depth semi-structured interviews | 9/10 |
| Overarching Theme | Experience of Poor Sleep Quality in FM | Poor Sleep Quality Management Strategies in FM | Intrastudy Intensity Effect Sizes | ||
|---|---|---|---|---|---|
| Sub-Themes | Evaluation of Poor Sleep Quality | Response to Poor Sleep Quality | Management Strategies to Favor Sleep | Managing the Consequences of a Sleepless Night | Individual Studies’ Contributions to Sub-Themes |
| Ramlee et al. [40] | ● | 0.7% | |||
| Russell et al. [41] | ● | 0.1% | |||
| Vincent et al. [42] | ● | 0.1% | |||
| Kleinman et al. [43] | ● | ● | 10.5% | ||
| Traska et al. [44] | ● | 0.1% | |||
| Sallinen et al. [45] | ● | ● | 0.2% | ||
| Humphrey et al. [46] | ● | 0.3% | |||
| Theadom et al. [17] | ● | ● | ● | ● | 29% |
| Martin et al. [47]) | ● | 0.1% | |||
| Lempp et al. [48] | ● | ● | 0.2% | ||
| Arnold et al. [49] | ● | ● | 0.2% | ||
| Crooks [50] | ● | ● | 0.2% | ||
| Cunningham et al. [51] | ● | ● | 0.3% | ||
| Söderberg et al. [52] | ● | ● | 0.3% | ||
| Cudney et al. [53] | ● | ● | ● | ● | 16.3% |
| Sturge-Jacobs [54] | ● | ● | ● | 0.3% | |
| Raymond and Brown [55] | ● | 0.1% | |||
| Interstudy Frequency Effect Sizes | |||||
| Representation of sub-themes in individual studies | 76% | 29% | 41.6% | 41% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Climent-Sanz, C.; Morera-Amenós, G.; Bellon, F.; Pastells-Peiró, R.; Blanco-Blanco, J.; Valenzuela-Pascual, F.; Gea-Sánchez, M. Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis. J. Clin. Med. 2020, 9, 4000. https://doi.org/10.3390/jcm9124000
Climent-Sanz C, Morera-Amenós G, Bellon F, Pastells-Peiró R, Blanco-Blanco J, Valenzuela-Pascual F, Gea-Sánchez M. Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis. Journal of Clinical Medicine. 2020; 9(12):4000. https://doi.org/10.3390/jcm9124000
Chicago/Turabian StyleCliment-Sanz, Carolina, Genís Morera-Amenós, Filip Bellon, Roland Pastells-Peiró, Joan Blanco-Blanco, Fran Valenzuela-Pascual, and Montserrat Gea-Sánchez. 2020. "Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis" Journal of Clinical Medicine 9, no. 12: 4000. https://doi.org/10.3390/jcm9124000
APA StyleCliment-Sanz, C., Morera-Amenós, G., Bellon, F., Pastells-Peiró, R., Blanco-Blanco, J., Valenzuela-Pascual, F., & Gea-Sánchez, M. (2020). Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis. Journal of Clinical Medicine, 9(12), 4000. https://doi.org/10.3390/jcm9124000






