Consensus-Based Recommendations for Advance Directives of People with Parkinson’s Disease in Regard to Typical Complications by German Movement Disorder Specialists
Abstract
1. Introduction
2. Experimental Section
2.1. Ethics Approval
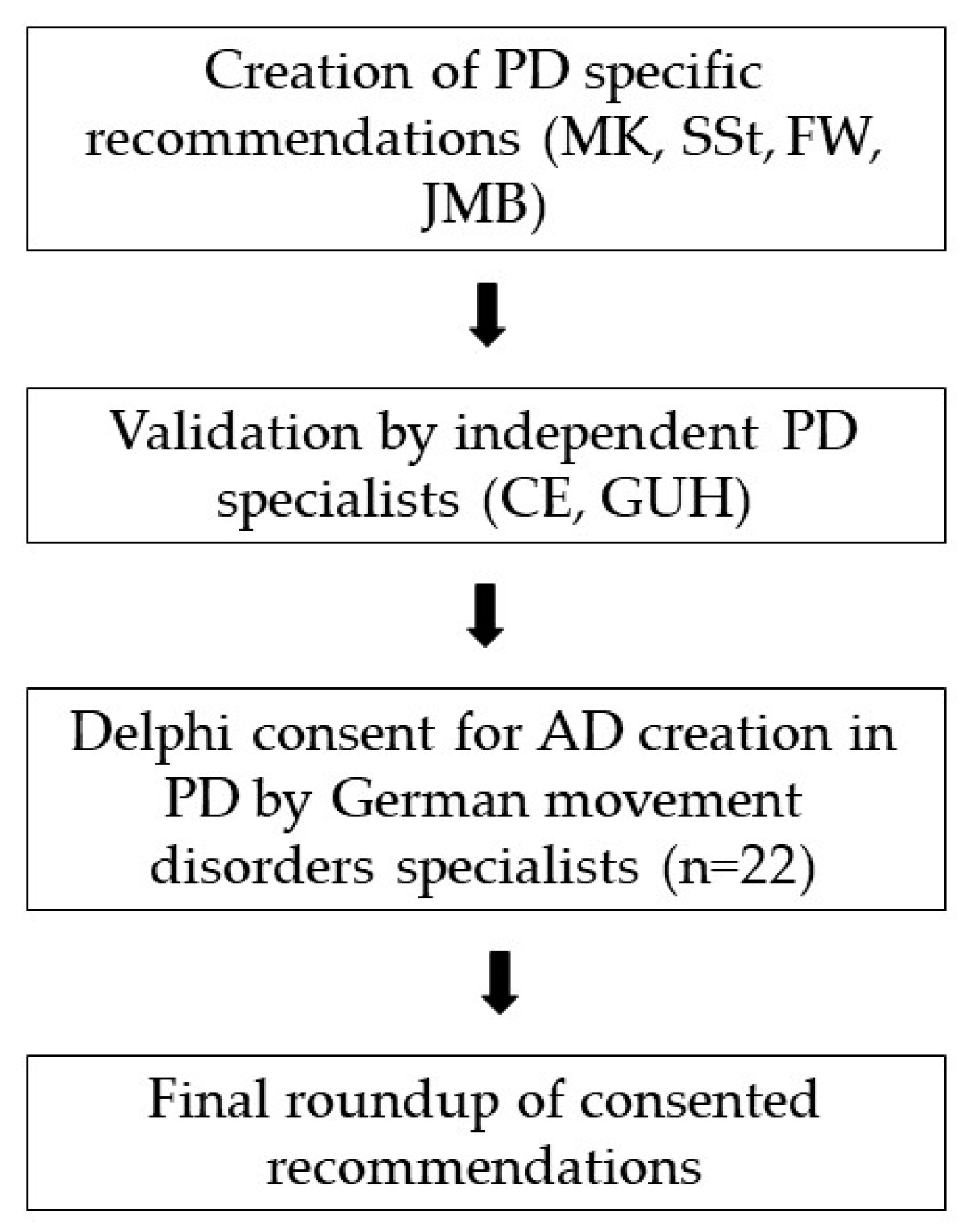
2.2. Study Design
2.3. Study Population
3. Results
3.1. Study Participants
3.2. Pre-Test
3.3. Consensus on Recommendations
3.3.1. Delphi Round 1
3.3.2. Delphi Round 2
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| 1st Domain: Timing of integrating recommendations in ADs | ||
| 1.1. | PwP sollten so früh wie möglich und proaktiv auf die Integrierung spezifischer Aspekte ihrer Erkrankung in eine vorliegende PV oder eine geplante PV aufmerksam gemacht werden. | Patients suffering from Parkinson’s disease should as early as possible and proactively be made aware of the integration of disease-specific aspects into an existing or planned living will. |
| 1.2. | Spezifische Handlungsanweisungen sollten dann beraten und gemeinsam gefunden werden, wenn der Patient noch in der Lage ist komplexe Entscheidungen und deren Konsequenzen zu überblicken. | Specific instructions should be discussed and defined when the patient is still able to understand the complexity of the decisions, including the consequences. |
| 1.3. | Spezifische Szenarien können dabei helfen, dem Patienten die allgemeinen krankheitsspezifischen Entscheidungen zu verdeutlichen. | Specific scenarios can help to clarify the general disease-specific decisions for the patient. |
| 1.4. | Bereits bei der Aufklärung über nicht-orale Folgetherapien sollte auch über palliativmedizinische Aspekte dieser Therapie aufmerksam gemacht werden. | During the education about non-oral therapies, attention should also already be drawn to palliative medical aspects of this therapy. |
| 1.5. | Spätestens in einem fortgeschrittenen Stadium der Erkrankung sollte über Schluckstörungen und invasive Behandlung vegetativer Symptome wie Blasen- und Mastdarmstörungen gesprochen werden. | Swallowing disorders and invasive treatment of vegetative symptoms, such as bladder and rectal disorders, should be discussed in an advanced stage of the disease at the latest. |
| 1.6. | Bereits früh im Verlauf der Erkrankung, aber spätestens nach dem ersten Auftreten dieser Symptome, sollte über neuropsychiatrische Symptome und deren Behandlung im Rahmen palliativer Versorgungssituationen gesprochen werden. | Neuropsychiatric symptoms and their treatment in palliative care situations should be discussed early in the course of the disease, but at the latest after the first appearance of these symptoms. |
| 2nd Domain: Levodopa carbidopa intestinal gel | ||
| 2.1. | Im Falle schwerer Schluckstörungen, die es mir unmöglich machen Medikamente/Parkinsonmedikamente zu schlucken, möchte ich (nicht) über alternative Applikationswege behandelt werden. | In case of severe swallowing disorders that make it impossible for me to swallow medications/Parkinson’s medications, I would (not) like to be treated via alternative routes of application. |
| 2.2. | Im Falle einer schweren Demenz wünsche ich (nicht), sofern medizinisch indiziert, die Fortführung der LCIG Therapie. | In the case of the occurrence of severe dementia, I (do not) wish the continuation of medically indicated LCIG therapy. |
| 2.3. | Sollte eine LCIG Therapie eingeleitet werden, möchte ich über diese (nicht) ernährt/mit Flüssigkeit versorgt werden. | If a LCIG therapy should be initiated, I would (not) like to be nourished/supplied with liquid via this therapy. |
| 2.4. | Ich wünsche/verweigere die Gabe von Flüssigkeiten und Ernährung über den PEG Schenkel des LCIG Systems im fortgeschrittenen Stadium der Parkinsonerkrankung. | I wish/deny the administration of fluids and nutrition via the PEG leg of the LCIG system in advanced stages of Parkinson’s disease. |
| 3rd Domain: Deep brain stimulation | ||
| 3.1. | Im Falle einer ausbleibenden Wirkung der Stimulation mit optimalen Parametern, wünsche ich bei Batterieerschöpfung keinen/einen Stimulatorwechsel oder eine Aufladung. | If the stimulation with optimal parameters is not effective, I do not wish to change or recharge the stimulator when the battery is exhausted. |
| 3.2. | Sollte ich selber oder Dritte Zeichen von Suizidalität unter THS bei mir bemerken, bitte ich um sofortige Anpassung meiner Therapie. | Should I or third parties notice signs of suicidal tendencies under THS, my therapy should be adjusted immediately. |
| 4th Domain: Swallowing disorder | ||
| 4.1. | Sollten im Verlauf meiner Erkrankung schwere Schluckstörungen auftreten, die mit konservativen Therapien nicht behandelbar sind, stimme ich einer PEG-Anlage zur Sicherung der Atemwege zu/nicht zu. | If severe swallowing disorders occur in the course of my illness, which cannot be treated with conservative therapies, I agree/disagree with a PEG-plant for securing the airways. |
| 4.2. | Sollten im Verlauf meiner Erkrankung schwere Schluckstörungen auftreten, die mit konservativen Therapien nicht behandelbar sind, wünsche ich eine/keine symptomatische Therapie einer möglichen Atemnot notfalls auch mit einer Tracheostoma-Anlage. | If severe swallowing disorders occur in the course of my illness, which cannot be treated with conservative therapies, I would (not) like to have a symptomatic therapy for possible respiratory distress, if necessary, also with a tracheostoma system. |
| 5th Domain: Changes in personality and neuropsychological symptoms | ||
| 5.1. | Sollten meine Parkinsontherapie meine Verhaltensweisen und Kommunikations-fähigkeit einschränken bzw. verändern, wünsche ich eine/keine umgehende Anpassung bzw. Beendigung dieser Therapien. | If my Parkinson’s therapy limits or changes my behaviour and communication skills, I (do not) wish immediate adaption or termination of these therapies. |
| 5.2. | Für die Identifikation von Veränderungen bzw. Einschränkungen meiner Verhaltensweisen und Kommunikations-fähigkeit soll bitte Rücksprache mit XXX als Person meines Vertrauens gehalten werden. | For the identification of changes or limitations in my behaviour and communication skills, please consult XXX as a person of my trust. |
| 5.3. | Sollten eingesetzte Medikamente einen negativen Einfluss auf meine kognitiven Fähigkeiten haben, bitte ich um eine/keine sofortige Anpassung meiner Therapie. Eine Anpassung der Therapie kann zu einer Einschränkung der motorischen Funktionen führen. | If any of the medications used have a negative influence on my cognitive abilities, I (do not) request immediate adjustment of my therapy. An adjustment of the therapy can lead to a restriction of motor functions. |
| 5.4. | Sollte bei meinen behandelnden Ärzten Unsicherheit über das Vorliegen von neuropsychologischen Störungen im Rahmen der Parkinsonerkrankung bestehen, dann wünsche ich eine/keine Konsultation eines spezialisierten Neurologen zur Diagnostik und Anpassung meiner Therapie. | If my treating physicians are uncertain about the presence of neuropsychological disorders in the context of Parkinson’s disease, I would (not) like to have a consultation with a specialized neurologist for diagnosis and adjustment of my therapy. |
| 6th Domain: Bladder and rectal problems | ||
| 6.1. | Sollte ich im Verlauf meiner Erkrankung eine schwerwiegende Dranginkontinenz entwickeln, welche unter konservativer Therapie für mich subjektiv nicht ausreichend gelindert werden kann, dann wünsche ich (nicht) eine Katheterversorgung. | Should I develop severe urge incontinence during the course of my illness which cannot be sufficiently relieved under conservative therapy according to my subjective assessment, I (do not) want a catheter supply. |
| 6.2. | Sollten sich meine kognitiven Fähigkeiten durch die medikamentöse Therapie meiner Dranginkontinenz verschlechtern, wünsche ich (nicht) das zeitnahe Absetzen dieser Medikamente. | Should my cognitive abilities deteriorate as a result of the drug therapy of my urge incontinence, I do (not) wish to discontinue these drugs in the near future. |
References
- Heinzel, S.; Berg, D.; Binder, S.; Ebersbach, G.; Hickstein, L.; Herbst, H.; Schmedt, N. Do We Need to Rethink the Epidemiology and Healthcare Utilization of Parkinson’s Disease in Germany? Front. Neurol. 2018, 9, 500. [Google Scholar] [CrossRef]
- Tuck, K.K.; Zive, D.M.; Schmidt, T.A.; Carter, J.; Nutt, J.; Fromme, E.K. Life-sustaining treatment orders, location of death and co-morbid conditions in decedents with Parkinson’s disease. Parkinsonism Relat. Disord. 2015, 21, 1205–1209. [Google Scholar] [CrossRef]
- Klietz, M.; Tulke, A.; Muschen, L.H.; Paracka, L.; Schrader, C.; Dressler, D.W.; Wegner, F. Impaired Quality of Life and Need for Palliative Care in a German Cohort of Advanced Parkinson’s Disease Patients. Front. Neurol. 2018, 9, 120. [Google Scholar] [CrossRef]
- Fall, P.A.; Saleh, A.; Fredrickson, M.; Olsson, J.E.; Granerus, A.K. Survival time, mortality, and cause of death in elderly patients with Parkinson’s disease: A 9-year follow-up. Mov. Disord. 2003, 18, 1312–1316. [Google Scholar] [CrossRef]
- Macleod, A.D.; Taylor, K.S.; Counsell, C.E. Mortality in Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1615–1622. [Google Scholar] [CrossRef]
- Bugalho, P.; Ladeira, F.; Barbosa, R.; Marto, J.P.; Borbinha, C.; Salavisa, M.; Conceição Ld Saraiva, M.; Fernandes, M.; Meira, B. Motor and non-motor function predictors of mortality in Parkinson’s disease. J. Neural Transm. 2019, 126, 1409–1415. [Google Scholar] [CrossRef]
- Miyasaki, J.; Kluger, B. Palliative care for Parkinson’s disease: Has the time come? Curr. Neurol. Neurosci. Rep. 2015, 15, 26. [Google Scholar] [CrossRef]
- Lum, H.D.; Sudore, R.L.; Bekelman, D.B. Advance care planning in the elderly. Med. Clin. N. Am. 2015, 99, 391–403. [Google Scholar] [CrossRef]
- Sudore, R.L.; Lum, H.D.; You, J.J.; Hanson, L.C.; Meier, D.E.; Pantilat, S.Z.; Matlock, D.D.; Rietjens, J.A.C.; Korfage, I.J.; Ritchie, C.S.; et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J. Pain Symptom Manag. 2017, 53, 821–832. [Google Scholar] [CrossRef]
- Brinkman-Stoppelenburg, A.; Rietjens, J.A.; van der Heide, A. The effects of advance care planning on end-of-life care: A systematic review. Palliat. Med. 2014, 28, 1000–1025. [Google Scholar] [CrossRef]
- Houben, C.H.M.; Spruit, M.A.; Groenen, M.T.J.; Wouters, E.F.M.; Janssen, D.J.A. Efficacy of advance care planning: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2014, 15, 477–489. [Google Scholar] [CrossRef]
- Abu Snineh, M.; Camicioli, R.; Miyasaki, J.M. Decisional capacity for advanced care directives in Parkinson’s disease with cognitive concerns. Parkinsonism Relat. Disord. 2017, 39, 77–79. [Google Scholar] [CrossRef]
- Klietz, M.; Öcalan, Ö.; Schneider, N.; Dressler, D.; Stiel, S.; Wegner, F. Advance Directives of German People with Parkinson’s Disease Are Unspecific in regard to Typical Complications. Parkinson’s Dis. 2019, 2019. [Google Scholar] [CrossRef]
- Connolly, S.; Galvin, M.; Hardiman, O. End-of-life management in patients with amyotrophic lateral sclerosis. Lancet Neurol. 2015, 14, 435–442. [Google Scholar] [CrossRef]
- Lum, H.D.; Jordan, S.R.; Brungardt, A.; Ayele, R.; Katz, M.; Miyasaki, J.M.; Hall, A.; Jones, J.; Kluger, B. Framing advance care planning in Parkinson disease: Patient and care partner perspectives. Neurology 2019, 92, e2571–e2579. [Google Scholar] [CrossRef]
- Hsu, C.-C.S.; Brian, A. The Delphi Technique: Making Sense of Consensus. Pract. Assess. Res. Eval. 2007, 12, 10. [Google Scholar]
- von der Gracht, H.A. Consensus measurement in Delphi studies. Review and implications for future quality assurance. Technol. Forecast. Soc. Chang. 2012, 79, 1525–1536. [Google Scholar] [CrossRef]
- Nijhuis, F.A.P.; van den Heuvel, L.; Bloem, B.R.; Post, B.; Meinders, M.J. The Patient’s Perspective on Shared Decision-Making in Advanced Parkinson’s Disease: A Cross-Sectional Survey Study. Front. Neurol. 2019, 10, 896. [Google Scholar] [CrossRef]
- Robinson, M.T.; Holloway, R.G. Palliative Care in Neurology. Mayo Clin. Proc. 2017, 92, 1592–1601. [Google Scholar] [CrossRef]
- Eva Weck, C.; Lorenzl, S. Neuropalliative care aspects in patients with Parkinson’s disease. Fortschr. Neurol. Psychiatr. 2018, 86 (Suppl. 1), S30–S33. [Google Scholar]
- Martinez-Martin, P.; Schapira, A.H.; Stocchi, F.; Sethi, K.; Odin, P.; MacPhee, G.; Brown, R.G.; Naidu, Y.; Clayton, L.; Abe, K.; et al. Prevalence of nonmotor symptoms in Parkinson’s disease in an international setting; study using nonmotor symptoms questionnaire in 545 patients. Mov. Disord. 2007, 22, 1623–1629. [Google Scholar] [CrossRef] [PubMed]
- Kluger, B.M.; Shattuck, J.; Berk, J.; Sebring, K.; Jones, W.; Brunetti, F.; Bekelman, D.B. Defining Palliative Care Needs in Parkinson’s Disease. Mov. Disord. Clin. Pract. 2019, 6, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Klietz, M.; Greten, S.; Wegner, F.; Hoglinger, G.U. Safety and Tolerability of Pharmacotherapies for Parkinson’s Disease in Geriatric Patients. Drugs Aging 2019, 36, 511–530. [Google Scholar] [CrossRef]
- Lex, K.; Kundt, F.; Lorenzl, S. Using tube feeding and levodopa-carbidopa intestinal gel application in advanced Parkinson’s disease. Br. J. Nurs. 2018, 27, 259–262. [Google Scholar] [CrossRef]
- Buter, T.C.; van den Hout, A.; Matthews, F.E.; Larsen, J.P.; Brayne, C.; Aarsland, D. Dementia and survival in Parkinson disease: A 12-year population study. Neurology 2008, 70, 1017–1022. [Google Scholar] [CrossRef]
- Balestrino, R.; Martinez-Martin, P. Neuropsychiatric symptoms, behavioural disorders, and quality of life in Parkinson’s disease. J. Neurol. Sci. 2017, 373, 173–178. [Google Scholar] [CrossRef]
- Umemoto, G.; Furuya, H. Management of Dysphagia in Patients with Parkinson’s Disease and Related Disorders. Intern. Med. 2019, 59, 7–14. [Google Scholar] [CrossRef]
- Buhmann, C.; Bihler, M.; Emich, K.; Hidding, U.; Potter-Nerger, M.; Gerloff, C.; Niessen, A.; Flugel, T.; Koseki, J.C.; Nienstedt, J.C.; et al. Pill swallowing in Parkinson’s disease: A prospective study based on flexible endoscopic evaluation of swallowing. Parkinsonism Relat. Disord. 2019, 62, 51–56. [Google Scholar] [CrossRef]
- Lingor, P.; Csoti, I.; Koschel, J.; Schrader, C.; Winkler, C.; Wolz, M.; Reichmann, H. The Geriatric Patient with Parkinson’s Disease-A Neurological Challenge. Fortschr. Neurol. Psychiatr. 2016, 84 (Suppl. 1), S41–S47. [Google Scholar]
- Müller-Rebstein, S.; Trenkwalder, C.; Ebentheuer, J.; Oertel, W.; Culmsee, C.; Höglinger, G. Drug Safety Analysis in a Real-Life Cohort of Parkinson’s Disease Patients with Polypharmacy. CNS Drugs 2017, 31, 1093–1102. [Google Scholar] [CrossRef]
- Ebersbach, G.; Ip, C.W.; Klebe, S.; Koschel, J.; Lorenzl, S.; Schrader, C.; Winkler, C.; Franke, C. Management of delirium in Parkinson’s disease. J. Neural. Transm. 2019, 126, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Klietz, M.; Rippena, L.; Lange, F.; Tulke, A.; Paracka, L.; Dressler, D.; Wegner, F. Validating the Parkinson’s disease caregiver burden questionnaire (PDCB) in German caregivers of advanced Parkinson’s disease patients. Int. Psychogeriatr. 2019, 31, 1791–1800. [Google Scholar] [CrossRef] [PubMed]
- Schmotz, C.; Richinger, C.; Lorenzl, S. High Burden and Depression Among Late-Stage Idiopathic Parkinson Disease and Progressive Supranuclear Palsy Caregivers. J. Geriatr. Psychiatry Neurol. 2017, 30, 267–272. [Google Scholar] [CrossRef]
- Mosley, P.E.; Moodie, R.; Dissanayaka, N. Caregiver Burden in Parkinson Disease: A Critical Review of Recent Literature. J. Geriatr. Psychiatry Neurol. 2017, 30, 235–252. [Google Scholar] [CrossRef]
| Item | Answer Option | n = 30 |
|---|---|---|
| Age (years) | Mean ± SD | 40.2 ± 10.4 |
| Sex | Female | 11 (36.7%) |
| Male | 19 (63.3%) | |
| Level of professional education | Resident | 8 (26.7%) |
| Consultant | 22 (73.3%) | |
| Work experience (years) | Mean ± SD | 13.2 ± 9.5 |
| Special training in palliative care | Yes | 6 (20%) |
| No | 24 (80%) |
| Domain | Initial Number of Items | Pre-Test | Delphi Round 1 | Delphi Round 2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adapted | Dropped Out | Consented | Unconsented | Consented | Unconsented | |||||
| Adapted | Dropped Out | Adapted | Dropped Out | |||||||
| 1. | Timing of integrating recommendations in ADs | 6 | 6 | 0 | 4 | 2 | 0 | 6 | 0 | 0 |
| 2. | Levodopa carbidopa intestinal gel | 4 | 3 | 1 | 1 | 2 | 0 | 3 | 0 | 0 |
| 3. | Deep brain stimulation | 2 | 2 | 0 | 2 | 0 | 0 | 2 | 0 | 0 |
| 4. | Swallowing disorders | 2 | 2 | 0 | 2 | 0 | 0 | 2 | 0 | 0 |
| 5. | Changes in personality | 4 | 4 | 4 | 1 | 0 | 3 | 1 | 0 | 0 |
| 6. | Neuropsychological symptoms | 4 | ||||||||
| 7. | Bladder and rectal problems | 3 | 2 | 1 | 0 | 1 | 1 | 0 | 0 | 1 |
| Overall | 24 | 19 | 15 | 14 | ||||||
| Recommendation | Consented in Round | Delphi Statement | Agreement Wording | Agreement Relevance | ||
|---|---|---|---|---|---|---|
| % 1–2 | n | % 1–2 | n | |||
| 1st Domain: Timing of integrating recommendations in ADs | ||||||
| R-1.1 | 2 | As part of Advance Care Planning, physicians should discuss disease-specific aspects for an existing or future advance directive with patients suffering from Parkinson’s disease. | 86.3 | 18 | 100 | 22 |
| R-1.2 | 1 | Medical discussions on Parkinson-specific phrases for advance directives should take place at a point in time when the patient is able to grasp the complexity of the decisions, including the consequences. | 93.3 | 28 | 96.7 | 29 |
| R-1.3 | 1 | Physicians should focus on case examples of Parkinson-specific problems to better illustrate the disease specific decisions for advance directives to patients. | 96.7 | 29 | 100 | 30 |
| R-1.4 | 2 | Physicians should provide information about the added medical value of palliative care when explaining or installing a medication pump. Added medical value of palliative care may include help with nutrition or administration of fluids. | 81.8 | 18 | 90.9 | 20 |
| R-1.5 | 1 | At an advanced stage of the disease, at the latest, physicians should provide information about swallowing disorders and treatment options for genitourinary symptoms and functional disorders of the rectum. Options may include catheters and Botox injections. | 90.0 | 27 | 90.0 | 27 |
| R-1.6 | 1 | Physicians should inform about neuropsychiatric symptoms and their treatment early in the course of the disease, but at the latest after primary appearance. | 80.0 | 24 | 83.3 | 25 |
| 2nd Domain: Levodopa carbidopa intestinal gel | ||||||
| R-2.1 | 2 | If swallowing disorders occur in the course of my illness, which make it impossible for me to swallow medication, I:
| 95.5 | 21 | 95.5 | 21 |
| R-2.2 | 2 | Should my decision-making ability be restricted in the course of my illness, I will make a prior decision as to whether or not to take the appropriate action:
| 95.5 | 21 | 95.5 | 21 |
| R-2.3 | 1 | Should I receive Duodopa for Parkinson’s therapy via a gastric tube during the course of my illness, I would like to use this tube to additionally:
| 90.0 | 27 | 90.0 | 27 |
| 3rd Domain: Deep brain stimulation | ||||||
| R-3.1 | 1 | If, in the course of my illness, the deep brain stimulation (DBS) should no longer work according to the assessment of my specialized treating physicians and the battery of the stimulator should be empty, I wish:
| 86.7 | 26 | 90.0 | 27 |
| R-3.2 | 1 | If the deep brain stimulation no longer works well in the course of my illness, I would like (no) further charging of the battery if the stimulator battery is empty. | 80.0 | 24 | 93.3 | 28 |
| 4th Domain: Swallowing disorder | ||||||
| R-4.1 | 1 | If, in the course of my illness, severe swallowing disorders occur that cannot be treated sufficiently with conventional therapies, I agree to a PEG feeding tube (PEG):
| 93.3 | 28 | 96.7 | 29 |
| R-4.2 | 1 | If, in the course of my illness, severe swallowing disorders occur, which also affect my breathing and are not sufficiently treatable with conventional therapies, I wish:
| 83.3 | 25 | 86.7 | 26 |
| 5th Domain: Changes in personality and neuropsychological symptoms | ||||||
| R-5.1 | 1 | In order to assess my behavior, mood, perception, communication skills or mental capacity, please contact my next of kin, XXX. | 96.7 | 29 | 96.7 | 29 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klietz, M.; Berndt, J.M.; Wegner, F.; Schneider, N.; Höglinger, G.U.; Eggers, C.; Stiel, S. Consensus-Based Recommendations for Advance Directives of People with Parkinson’s Disease in Regard to Typical Complications by German Movement Disorder Specialists. J. Clin. Med. 2020, 9, 449. https://doi.org/10.3390/jcm9020449
Klietz M, Berndt JM, Wegner F, Schneider N, Höglinger GU, Eggers C, Stiel S. Consensus-Based Recommendations for Advance Directives of People with Parkinson’s Disease in Regard to Typical Complications by German Movement Disorder Specialists. Journal of Clinical Medicine. 2020; 9(2):449. https://doi.org/10.3390/jcm9020449
Chicago/Turabian StyleKlietz, Martin, Johanna M. Berndt, Florian Wegner, Nils Schneider, Günter U. Höglinger, Carsten Eggers, and Stephanie Stiel. 2020. "Consensus-Based Recommendations for Advance Directives of People with Parkinson’s Disease in Regard to Typical Complications by German Movement Disorder Specialists" Journal of Clinical Medicine 9, no. 2: 449. https://doi.org/10.3390/jcm9020449
APA StyleKlietz, M., Berndt, J. M., Wegner, F., Schneider, N., Höglinger, G. U., Eggers, C., & Stiel, S. (2020). Consensus-Based Recommendations for Advance Directives of People with Parkinson’s Disease in Regard to Typical Complications by German Movement Disorder Specialists. Journal of Clinical Medicine, 9(2), 449. https://doi.org/10.3390/jcm9020449






