Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review
Abstract
:1. Introduction
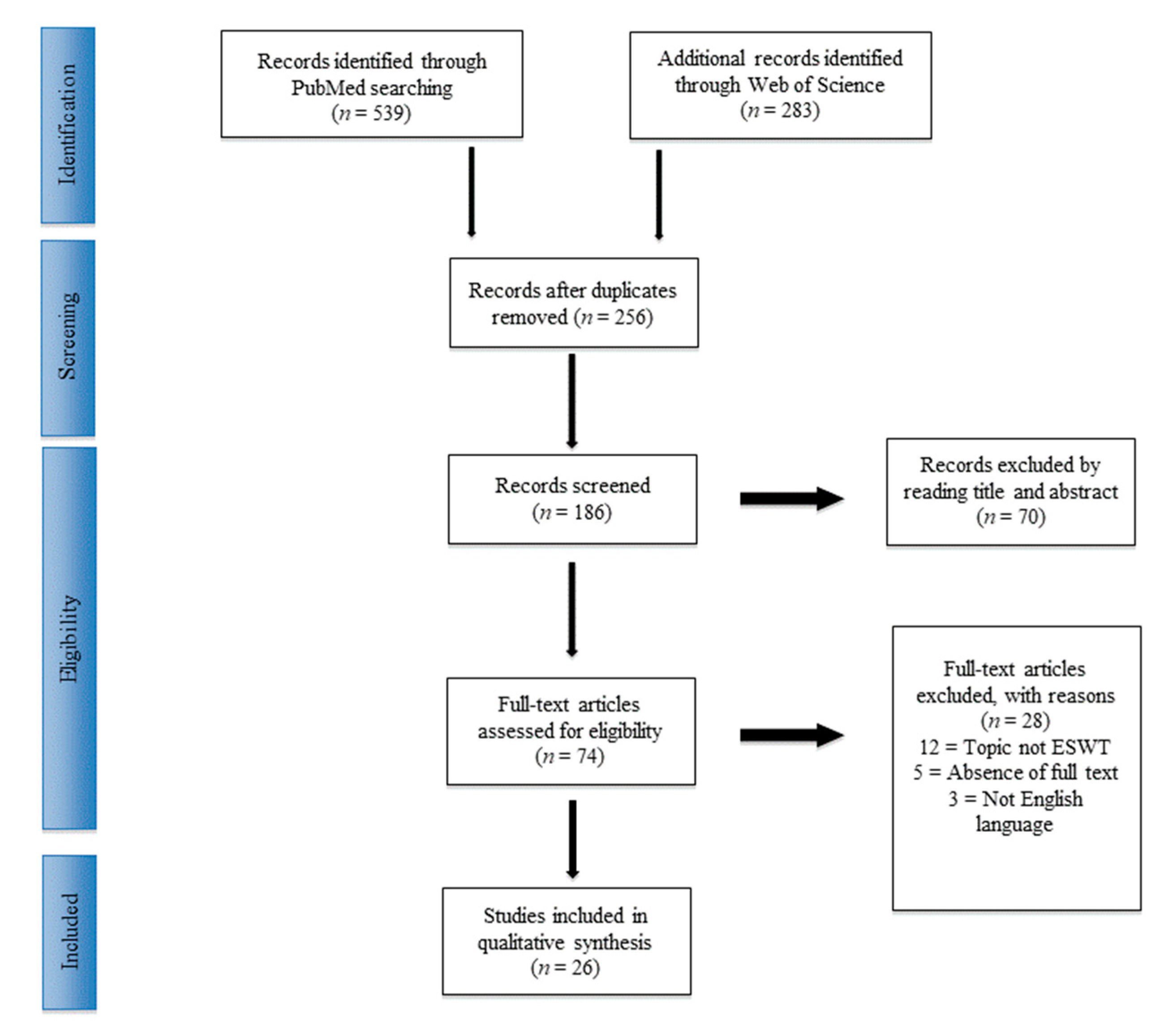
2. Experimental Section
2.1. Study Selection
2.2. Inclusion and Exclusion Criteria
2.3. Risk of Bias Assessment
3. Results
3.1. Included Studies
3.2. Shoulder
3.2.1. Calcific Tendinopathy of the Rotator Cuff (CTRC)
3.2.2. Non-Calcific Tendinopathy of the Rotator Cuff (NTRC)
3.2.3. Subacromial Impingement Syndrome (SAIS)
3.3. Elbow
3.3.1. Lateral Epicondylitis (LEP)
3.3.2. Medial Epicondylitis (MEP)
4. Discussion
4.1. General Consideration
4.2. Shoulder
4.3. Elbow
4.4. Limits of the Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bannuru, R.R.; Flavin, N.E.; Vaysbrot, E.; Harvey, W.; McAlindon, T. High-energy extracorporeal shock-wave therapy for treating chronic calcific tendinitis of the shoulder: A systematic review. Ann. Intern. Med. 2014, 160, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; Singh, S.; Paladini, P.; Porcellini, G. Calcific tendinitis of the rotator cuff: State of the art in diagnosis and treatment. J. Orthop. Traumatol. 2016, 17, 7–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fusini, F.; Bisicchia, S.; Bottegoni, C.; Gigante, A.; Zanchini, F.; Busilacchi, A. Nutraceutical supplement in the management of tendinopathies: A systematic review. Muscles Ligaments Tendons J. 2016, 6, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Fu, S.C.; Chua, E.; Hu, X.; Rolf, C.; Mattila, V.M.; Qin, L.; Yung, P.S.; Chan, K.M. Critical review on the socio-economic impact of tendinopathy. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2016, 4, 9–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, J.S. Subacromial impingement syndrome: A musculoskeletal condition or a clinical illusion? Phys. Ther. Rev. 2011, 16, 388–398. [Google Scholar] [CrossRef]
- Shire, A.R.; Stæhr, T.A.B.; Overby, J.B.; Bastholm Dahl, M.; Sandell Jacobsen, J.; Høyrup Christiansen, D. Specific or general exercise strategy for subacromial impingement syndrome–does it matter? A systematic literature review and meta analysis. BMC Musculoskelet. Disord. 2017, 18, 158. [Google Scholar] [CrossRef]
- Amin, N.H.; Kumar, N.S.; Schickendantz, M.S. Medial epicondylitis: Evaluation and management. J. Am. Acad. Orthop. Surg. 2015, 23, 348–355. [Google Scholar] [CrossRef] [Green Version]
- Vaquero-Picado, A.; Barco, R.; Antuna, R.B.S. Lateral epicondylitis of the elbow. EFORT Open Rev. 2016, 1, 391–397. [Google Scholar] [CrossRef]
- Cardoso, T.B.; Pizzari, T.; Kinsella, R.; Hope, D.; Cook, J.L. Current trends in tendinopathy management. Best Pract. Res. Clin. Rheumatol. 2019. [Google Scholar] [CrossRef]
- Notarnicola, A.; Pesce, V.; Vicenti, G.; Tafuri, S.; Forcignanò, M.; Moretti, B. SWAAT study: Extracorporeal shock wave therapy and arginine supplementation and other nutraceuticals for insertional achilles tendinopathy. Adv. Ther. 2012, 29, 799–814. [Google Scholar] [CrossRef]
- Vitali, M.; Peretti, G.; Mangiavini, L.; Fraschini, G. The treatment with extracorpereal shock wave therapy in some of most frequently musculoskeletal pathologies. Orthop. Proc. 2006, 88-B, 423. [Google Scholar]
- Pavone, V.; Cannavò, L.; Di Stefano, A.; Testa, G.; Costarella, L.; Sessa, G. Low-Energy Extracorporeal Shock-Wave Therapy in the Treatment of Chronic Insertional Achilles Tendinopathy: A Case Series. Biomed. Res. Int. 2016, 2016, 7123769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pavone, V.; Vescio, A.; Mobilia, G.; Dimartino, S.; Di Stefano, G.; Culmone, A.; Testa, G. Conservative Treatment of Chronic Achilles Tendinopathy: A Systematic Review. J. Funct. Morphol. Kinesiol. 2019, 4, 46. [Google Scholar] [CrossRef] [Green Version]
- Yin, M.; Ma, J.; Xu, J.; Li, L.; Chen, G.; Sun, Z.; Liu, Y.; He, S.; Ye, J.; Mo, W. Use of artificial neural networks to identify the predictive factors of extracorporeal shock wave therapy treating patients with chronic plantar fasciitis. Sci. Rep. 2019, 9, 4207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saggini, R.; Di Stefano, A.; Saggini, A.; Bellomo, R.G. Clinical application of shock wave therapy in musculoskeletal disorders: Part II related to myofascial and nerve apparatus. J. Biol. Regul. Homeost. Agents 2015, 29, 771–885. [Google Scholar] [PubMed]
- Visco, V.; Vulpiani, M.C.; Torrisi, M.R.; Ferretti, A.; Pavan, A.; Vetrano, M. Experimental studies on the biological effects of extracorporeal shock wave therapy on tendon models. A review of the literature. Muscles Ligaments Tendons J. 2014, 4, 357–361. [Google Scholar] [CrossRef]
- Wang, C.J.; Cheng, J.H.; Chou, W.Y.; Hsu, S.L.; Chen, J.H.; Huang, C.Y. Changes of articular cartilage and subchondral bone after extracorporeal shockwave therapy in osteoarthritis of the knee. Int. J. Med. Sci. 2017, 14, 213–223. [Google Scholar] [CrossRef] [Green Version]
- Albert, J.D.; Meadeb, J.; Guggenbuhl, P.; Marin, F.; Benkalfate, T.; Thomazeau, H.; Chalès, G. High-energy extracorporeal shockwave therapy for calcifying tendinitis of the rotator cuff: A randomised trial. J. Bone Joint Surg. Br. 2007, 89-B, 335–341. [Google Scholar] [CrossRef]
- Krasny, C.; Enenkel, M.; Aigner, N.; Wlk, M.; Landsiedl, F. Ultrasound-guided needling combined with shock-wave therapy for the treatment of calcifying tendonitis of the shoulder. J. Bone Joint Surg. Br. 2005, 87-B, 501–507. [Google Scholar] [CrossRef]
- Reilly, J.M.; Bluman, E.; Tenforde, A.S. Effect of shockwave treatment for management of upper and lower extremity musculoskeletal conditions: A narrative review. PM&R 2018, 10, 1385–1403. [Google Scholar]
- Fritze, J. Extracorporeal shock wave treatment (ESWT) in orthopaedic indications: A selective review. Versicherungsmedizin 1998, 50, 180–185. [Google Scholar] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, 4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malliaropoulos, N.; Thompson, D.; Meke, M.; Pyne, D.; Alaseirlis, D.; Atkinson, H.; Korakakis, V.; Lohrer, H. Individualised radial extracorporeal shock wave therapy (rESWT) for symptomatic calcific shoulder tendinopathy: A retrospective clinical study. BMC Musculoskelet. Disord. 2017, 18, 513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosentino, R.; De Stefano, R.; Selvi, E.; Frati, E.; Manca, S.; Frediani, B.; Marcolongo, R. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulder: Single blind study. Ann. Rheum. Dis. 2003, 62, 248–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Castillo-González, F.; Ramos-Alvarez, J.J.; Rodríguez-Fabián, G.; González-Pérez, J.; Jiménez-Herranz, E.; Varela, E. Extracorporeal shockwaves versus ultrasound-guided percutaneous lavage for the treatment of rotator cuff calcific tendinopathy: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2016, 52, 145–151. [Google Scholar]
- Gerdesmeyer, L.; Wagenpfeil, S.; Haake, M.; Maier, M.; Loew, M.; Wörtler, K.; Lampe, R.; Seil, R.; Handle, G.; Gassel, S.; et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: A randomized controlled trial. JAMA 2003, 290, 2573–2580. [Google Scholar] [CrossRef]
- Pan, P.J.; Chou, C.L.; Chiou, H.J.; Ma, H.L.; Lee, H.C.; Chan, R.C. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulders: A functional and sonographic study. Arch. Phys. Med. Rehabil. 2003, 84, 988–993. [Google Scholar] [CrossRef]
- Frassanito, P.; Cavalieri, C.; Maestri, R.; Felicetti, G. Effectiveness of Extracorporeal Shock Wave Therapy and kinesio taping in calcific tendinopathy of the shoulder: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 333–340. [Google Scholar]
- Chou, W.Y.; Wang, C.J.; Wu, K.T.; Yang, Y.J.; Ko, J.Y.; Siu, K.K. Prognostic factors for the outcome of extracorporeal shockwave therapy for calcific tendinitis of the shoulder. Bone Joint J. 2017, 99-B, 1643–1650. [Google Scholar] [CrossRef]
- Li, W.; Zhang, S.X.; Yang, Q.; Li, B.L.; Meng, Q.G.; Guo, Z.G. Effect of extracorporeal shock-wave therapy for treating patients with chronic rotator cuff tendonitis. Medicine (Baltimore) 2017, 96, e7940. [Google Scholar] [CrossRef] [PubMed]
- Galasso, O.; Amelio, E.; Riccelli, D.A.; Gasparini, G. Short-term outcomes of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopathy of the supraspinatus: A double-blind, randomized, placebo-controlled trial. BMC Musculoskelet. Disord. 2012, 13, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, K.T.; Chou, W.Y.; Wang, C.J.; Chen, C.Y.; Ko, J.Y.; Chen, P.C.; Cheng, J.H.; Yang, Y.J. Efficacy of Extracorporeal Shockwave Therapy on Calcified and Noncalcified Shoulder Tendinosis: A Propensity Score Matched Analysis. Biomed. Res. Int. 2019, 2019, 2958251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Efe, T.; Felgentreff, M.; Heyse, T.J.; Stein, T.; Timmesfeld, N.; Schmitt, J.; Roessler, P.P. Extracorporeal shock wave therapy for non-calcific supraspinatus tendinitis—10-year follow-up of a randomized placebo-controlled trial. Biomed. Tech. (Berlin) 2014, 59, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Speed, C.A.; Nichols, D.; Richards, C.; Humphreys, H.; Wies, J.T.; Burnet, S.; Hazleman, B.L. Extracorporeal shock wave therapy for lateral epicondylitis—A double blind randomised controlled trial. J. Orthop. Res. 2002, 20, 895–898. [Google Scholar] [CrossRef]
- Circi, E.; Okur, S.C.; Aksu, O.; Mumcuoglu, E.; Tuzuner, T.; Caglar, N. The effectiveness of extracorporeal shockwave treatment in subacromial impingement syndrome and its relation with acromion morphology. Acta Orthop. Traumatol. Turc. 2018, 52, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Kvalvaag, E.; Roe, C.; Engebretsen, K.B. One year results of a randomized controlled trial on radial Extracorporeal Shock Wave Treatment, with predictors of pain, disability and return to work in patients with subacromial pain syndrome. Eur. J. Phys. Rehabil. Med. 2018, 54, 341–350. [Google Scholar]
- Santamato, A.; Panza, F.; Notarnicola, A.; Cassatella, G.; Fortunato, F.; de Sanctis, J.L.; Valeno, G.; Kehoe, P.G.; Seripa, D.; Logroscino, G.; et al. Is Extracorporeal Shockwave Therapy Combined With Isokinetic Exercise More Effective Than Extracorporeal Shockwave Therapy Alone for Subacromial Impingement Syndrome? A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2016, 46, 714–725. [Google Scholar] [CrossRef] [Green Version]
- Park, J.W.; Hwang, J.H.; Choi, Y.S.; Kim, S.J. Comparison of Therapeutic Effect of Extracorporeal Shock Wave in Calcific Versus Noncalcific Lateral Epicondylopathy. Ann. Rehabil. Med. 2016, 40, 294–300. [Google Scholar] [CrossRef] [Green Version]
- Bayram, K.; Yesil, H.; Dogan, E. Efficacy of extracorporeal shock wave therapy in the treatment of lateral epicondylitis. North Clin. Istanb. 2014, 1, 33–38. [Google Scholar] [CrossRef]
- Köksa, İ.; Güler, O.; Mahiroğulları, M.; Mutlu, S.; Çakmak, S.; Akşahin, E. Comparison of extracorporeal shock wave therapy in acute and chronic lateral epicondylitis. Acta Orthop. Traumatol. Turc. 2015, 49, 465–470. [Google Scholar]
- Pettrone, F.A.; McCall, B.R. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J. Bone Joint Surg. Am. 2005, 87, 1297–1304. [Google Scholar]
- Trentini, R.; Mangano, T.; Repetto, I.; Cerruti, P.; Kuqi, E.; Trompetto, C.; Franchin, F. Short- to mid-term follow-up effectiveness of US-guided focal extracorporeal shock wave therapy in the treatment of elbow lateral epicondylitis. Musculoskelet. Surg. 2015, 99 (Suppl. 1), S91–S97. [Google Scholar] [CrossRef]
- Guler, N.S.; Sargin, S.; Sahin, N. Efficacy of extracorporeal shockwave therapy in patients with lateral epicondylitis: A randomized, placebo-controlled, double-blind clinical trial. North Clin. Istanb. 2018, 5, 314–318. [Google Scholar] [PubMed]
- Radwan, Y.A.; ElSobhi, G.; Badawy, W.S.; Reda, A.; Khalid, S. Resistant tennis elbow: Shock-wave therapy versus percutaneous tenotomy. Int. Orthop. 2008, 32, 671–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.S.; Kang, S.; Park, N.K.; Lee, C.W.; Song, H.S.; Sohn, M.K.; Cho, K.H.; Kim, J.H. Effectiveness of initial extracorporeal shock wave therapy on the newly diagnosed lateral or medial epicondylitis. Ann. Rehabil. Med. 2012, 36, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Vulpiani, M.C.; Nusca, S.M.; Vetrano, M.; Ovidi, S.; Baldini, R.; Piermattei, C.; Ferretti, A.; Saraceni, V.M. Extracorporeal shock wave therapy vs cryoultrasound therapy in the treatment of chronic lateral epicondylitis. One year follow up study. Muscles Ligaments Tendons J. 2015, 5, 167–174. [Google Scholar] [CrossRef]
- Wong, C.W.; Ng, E.Y.; Fung, P.W.; Mok, K.M.; Yung, P.S.; Chan, K.M. Comparison of treatment effects on lateral epicondylitis between acupuncture and extracorporeal shockwave therapy. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2016, 7, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Sems, A.; Dimeff, R.; Iannotti, J.P. Extracorporeal shock wave therapy in the treatment of chronic tendinopathies. J. Am. Acad. Orthop. Surg. 2006, 14, 195–204. [Google Scholar] [CrossRef] [Green Version]
- Labelle, H.; Guibert, R.; Joncas, J.; Newman, N.; Fallaha, M.; Rivard, C.H. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. An attempted meta-analysis. J. Bone Joint Surg. Br. 1992, 74, 646–651. [Google Scholar] [CrossRef]
- Kisch, T.; Wuerfel, W.; Forstmeier, V.; Liodaki, E.; Stang, F.H.; Knobloch, K.; Mailaender, P.; Kraemer, R. Repetitive shock wave therapy improves muscular microcirculation. J. Surg. Res. 2016, 201, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Hatanaka, K.; Ito, K.; Shindo, T.; Kagaya, Y.; Ogata, T.; Eguchi, K.; Kurosawa, R.; Shimokawa, H. Molecular mechanisms of the angiogenic effects of low-energy shock wave therapy: Roles of mechanotransduction. Am. J. Physiol. Cell Physiol. 2016, 311, C378–C385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Ref | Authors | No. of Patients | Group | No. of Impulses (Time a Week) | Follow-Up | Results Summery |
|---|---|---|---|---|---|---|
| [11] | Vitali et al. | 30 | ESWT vs ESWT + DS | 1700–2000 (1) | 0, 7, 30 and 60 days | At 2 months follow-up, ESWT+DS group had significant improvement of functional outcome (p value = 0.0002) and pain compared to the only ESWT group. A significant reduction of painkiller was in the ESWT+DS group after one month (p value = 0.0308) and after 2 months (p value = 0.0061). (ESWT+DS (UCLA score = 27 (26–29); VAS = 2 (1–3); NSAIDs = 0%); (ESWT (UCLA score 23(17–25); VAS=5(4–7); NSAIDs = 40%) |
| [24] | Malliaropoulos et al. | 67 | rESWT | 1500 (>3) | 0, 1, 3, 12 months | The study reported the 92% of satisfied patients after 1 year of treatment, 52% of pain decreased after the first treatment, 62% after 30 days, 75% at 3 months and 88% at 1 year follow up. Recurrence rate of the 7%. VAS (baseline = 6.7 ± 1.1; Post-treatment=3.2 ± 0.8; 1st month=2.6 ± 0.9; 3rd month=1.7 ± 1.0; 1 year = 0.8 ± 1.0) |
| [25] | Cosentino et al. | 70 | ESWT vs placebo | 1200 (3) | 0, after the treatment, 1 and 6 months | The pain (p-value < 0.05)was significantly reduced compared to the baseline and improved the functional outcome (p-value < 0.05). Calcium complete reabsorption in the thirty-one to forty per-cent of the patients, and partial in 40% of cases. (ESWT CS( baseline = 45 points (pain 5.2, activities of daily living 9.6, range of motion 23.2, power 7); final follow-up = 71 points (pain 9.8,; activities of daily living 13; range of motion 32; power 16.2))(Placebo Constant Score (baseline = 48 points, final follow-up = 50 points). |
| [26] | Del Castillo-González et al. | 243 | ESWT vs UGPL | 2000 (2) | 0, 3, 6, 12 months | Sixty-five per-cent of pain free patient, 55.6% after 1 year. (VAS (baseline=7.43 ± 0.99; 1 year 2.0 ± 0.4) |
| [27] | Gerdesmeyer et al. | 144 | High ESWT vs low ESWT vs placebo | 1500 (1) | 0, 3, 6, 12 months | High ESWT and low ESWT group recorded the a significant improvement compared to placebo group and baseline. High energy group results were superior the low-energy group results. (CS at 6-month follow-up (High ESWT=31.0 (26.7–35.3); low ESWT = 15.0 (10.2–19.8); placebo = 6.6(1.4–11.8) |
| [28] | Pan et al. | 63 | ESWT vs TENS | 2000 (Nd) | 0, 2, 4, 12 weeks | Significant improvement of the shoulder joint ROM, activities day-livings, and decrease of the pain condition. (ESWT = CS(baseline = 63.77 ± 14.22; final difference =+28.31 ± 13.10); VAS(baseline=6.50±1.81; final difference = -4.08±2.59)); (TENS=CS(baseline=65.66 ± 15.84; final difference = + 11.86 ± 13.32); VAS(baseline = 6.70 ± 1.42; final difference = −1.74 ± 2.20) |
| [29] | Frassinito et al. | 42 | ESWT vs ESWT + KT | 1800 (3) | 0, 1, 4, 12 weeks | At the one-week follow up, the authors recorded a significant reduction in pain and functional enhancement. Baseline(VAS = ESWT+KT =6. 6±1.5(6.0,7.2); ESWT = 6.7 ± 1.1(6.2,7.1) DASH(ESWT+KT = 33.6 ± 12.1(28.4,38.8); ESWT = 31.1 ± 8.9 (27.3, 34.9)); Final difference(ESWT+KT VAS =−5.4; ESWT VAS = −4.3; ESWT+KT DASH = −25.9; ESWT DASH = −17.4) |
| [30] | Chou et al. | 241 | ESWT | 3000 (1−2) | 0, 3, 6, 12 months | After ESWT, improvement of outcome and pain. After the first treatment, 90.5% of complete calcium deposit fragmentation and resorption and the remaining 9.5% after the second. Odds ratio Type I calcification of 24.8 than the other types. Additional one month of symptoms each 1 mm increase of calcific deposit. CS (Baseline = 53.7 ± 10.2(24−37); After treatment 90.0 ± 16.4(33−100)) |
| [31] | Li et al. | 84 | ESWT vs placebo | 3000 (2) | 0, 4, 8 weeks | At the 4(p < 0.05) and 8(p < 0.01) weeks follow-up, significant improvement of pain and functional outcome. CS (Baseline(ESWT = 53.7 ± 14.1; 56.2 ± 14.4) 4-weeks difference(ESWT = 19.4(10.1, 28.5); placebo = 10.3(5.4,17.7)); 8-weeks difference (ESWT = 27.2(18.6, 38.3); placebo = 14.1 (8.8, 20.2)) |
| [32] | Galasso et al. | 20 | ESWT vs placebo | 3000 (1) | 0, 6, 12 weeks and 3 months | Satisfied patients in ESWT group 63.7% and 22.3% of control group. Improvement of pain and functional outcome after shockwaves treatment compare to the other cohort. CS Baseline (ESWT = 42.45 ± 9.83 (29–61) placebo = 41.67 ± 12.53 (20–57)); CS 6 weeks ESWT = 64 ± 16.6 (32–87); placebo = 43.11 ± 19.16 (18–70); CS 3 months ESWT = 74.09 ± 20.56 (39–98) placebo = 48 ± 22.3 (17–79). |
| [33] | Wu et al. | 20 | ESWT | 3000 (1) | 0, 3, 6, 12 months | At one year follow up, decreasing of pain symptomatology and increasing of the shoulder functionality in chronic shoulder tendinosis and type II and type III calcification patients. Similar results in type I calcified and noncalcified tendinitis patients. CS Baseline (No and I Calcified CS = 52.5 ± 14.5(21–74) Calcified CS=49.7 ± 9.03(33–62)); After treatment (No and I Calcified CS = 78.7 ± 18.3(38–98); Calcified CS=71.1 ± 17.8(44–98) |
| [34] | Efe et al. | 29 | ESWT vs placebo | 3000 (Nd) | 0 and 10 years | At 10 years follow-up, increase of functional outcome and decrease of pain differences compare to the baseline in ESWT group but not significant differences compared to placebo group. Eight surgical treated patients between 1- and 10-year follow-ups. The CS at last follow-up placebo = 99 ± 31; ESWT = 105 ± 24) Differences between baseline and 10-year follow-up data were significant (p = 0.02) |
| [35] | Speed et al. | 74 | ESWT vs placebo | 1500 (Nd) | 0, 1 and 3 months |
The 50% improvement of functional score was recorded in the thirty-five per-cent of ESWT group and the 45% of the placebo subjects after 90 days. Significant decrease of pain in both groups. At 6-month follow-up, similar results in the ESWT and placebo cohort. ESWT( baseline = 53.6 ± 20.2(13 to 89); 1 month = 48.7 ± 21.0 (7 to 83); 2 month 46.1 ± 22.4 (9 to 88) 3 month 34.7 ± 26.6 (2 to 90); 6 month = 24.1 ± 22.9 (0 to 82)); placebo( baseline = 59.5 ± 16.1 (16 to 90); 1 month = 58.5 ± 19.7 (13 to 93); 2 month = 48.6 ± 23.8 (3 to 90); 2 month = 39.7 ± 27.7 (5 to 96); 6 month = 34.9 ± 31.7 (0 to 95)) |
| [36] | Circi et al. | 30 | ESWT and Acromion type | 1500 (3) | 0 and post-treatment | Improvement of functional score and pain in all patients, no differences between acromion types subgroups. Acromion type 1 = SPADI(baseline = 47.9 ± 22.4 (16–90);post-treatment = 33.0 ± 19.2(2–60); Acromion type 2 = SPADI(baseline= 57.5 ± 26.3 (14–95); post-treatment = 39.5 ± 24.6 (9–70)); Acromion type 3 = SPADI(baseline = 59.6 ± 27.9 (26–91); post-treatment = 43.6 ± 23.4) |
| [37] | Kvalvaag et al. | 143 | rESWT + FKT vs placebo +FKT | 2000 (4) | 0 and 1 year | Successful result in the 51.4% of ESWT+FKT group and the 53.6% of placebo + FKT group after 12 months. No significant differences between cohorts. rESWT+FKT=SPADI(baseline = 51.9 ± 16.7;post-treatment = 28.3 ± 19.2(2–60); placebo + FKT = SPADI(baseline = 51.8 ± 17.5; post-treatment = 26.9 ± 27.3); |
| [38] | Santamato et al. | 30 | ESWT vs ESWT + FKT | 700 (3) | 0, 10 days and 2 months | Improvement of pain and shoulder functionality in both groups compared to baseline. Better results in ESWT+FKT cohort than ESWT-only group at 10- and 60-days follow-up. Group ESWT CS (Baseline = 49.7 ± 7.9(45.4, 54.1); 10days = 65.1 ± 7.7(60.8, 69.3); 2-month= 75.9 ± 6.7 (72.2, 79.6)) Group ESWT + FKT(Baseline = 45.6 ± 9.8 (40.2, 51.0); 10days = 63.6 ± 8.7 (58.8, 68.4); 2-month = 92.1 ± 6.3 (88.6, 95.6)) |
| Ref | Authors | No. of Patients | Group | No. of Impulses (Time a Week) | Follow-Up | Results Summery |
|---|---|---|---|---|---|---|
| [11] | Vitali et al. | 30 | ESWT vs ESWT + DS | 1700-2000 (1) | 0, 7, 30 and 60 days | In the ESWT, + DS patients were recorded an early significant functional betterment at 7-, 30-, and 60-days follow-up compared to the other group. Reduction of painkiller in 1 and 2 month s(p value = 0.0001 and p value = 0.0053, respectively). (ESWT + DS (Mayo = 27 (26–29); VAS = 2 (1–3); NSAIDs = 7%); |
| [39] | Park et al. | 43 | ESWT | 2000 (1) | 0, 3 and 6 months | Improvement of functional score and pain in all patients. (100-point score (F(df = 1) = 97.801, p < 0.001) and Nirschl Pain Phase scaleF(df = 1) = 63.061, p < 0.0001) |
| [40] | Bayram et al. | 12 | ESWT | 2000 (3) | 0 and 1 month | Decrease of pain at the rest, compression and activities 1-month after the treatment compare to baseline (p < 0.05). Patient’s and physician’s global post treatment self assessment scores were improved comparing the values pre- and post-operatively (p < 0.05). (PRTEE pret = 91.50 ± 11.24; PRTEE postt 1. month 55.83 ± 11.69) |
| [41] | Koskal et al. | 54 | ESWT | 2000 (2) | 0, 2, 12, and 24 weeks | In each evaluation, improvement of pain symptomatology while resting, stretching, working, and nighttime pain compared to the baseline. Pretherapy(VAS resting = 0.79 ± 1.91; VAS stretching = 7.25 ± 1.29; VAS pressed = 8.5 ± 0.98; VAS lifting chair = 6.63 ± 1.21;VAS working = 6.38 ± 1.01; VAS nighttime = 7.04 ± 1.2;); 24 weeks posttherapy VAS resting = 3.67 ± 1.63; VAS stretching = 0.71 ± 1.83; VAS pressed = 5.88 ± 1.9; VAS lifting chair = 4.58 ± 1.61; VAS working = 4.63 ± 1.31; VAS nighttime = 3.38 ± 1.71) |
| [42] | Pettrone et al. | 114 | ESWT vs placebo | 2000 (1) | 0, 2, 4, 8, and 12 weeks | Significant pain reduction (p = 0.001) and improvement of functional scores (p < 0.01) of the ESWT group compared to the placebo at 12 weeks after the therapy. ESWT Pain (baseline = 74 ± 15.8; posttreatment = 37.6 ± 28.7); placebo pain 75.6 ± 16.0 51.3 ± 29.7 32% 0.02 ESWT Functional scale(baseline = 4.7 ± 1.8; posttreatment=2.3 ± 1.6); placebo Functional scale(baseline = 4.6 ± 1.8 posttreatment = 3.2 ± 2.1) |
| [43] | Trentini et al. | 37 | ESWT | 1000 (4) | 0 and last follow-up (Nd) | No positivity to clinical assessment test (p < 0.01) for lateral epicondylitis after the treatment and betterment of outcome and pain (p < 0.001). quickDASH score (baseline = 51.6; posttreatment = 5.5) VAS (pain baseline = 8; posttreatment = 1.1) |
| [44] | Guller et al. | 20 | ESWT vs placebo | 1500 (Nd) | 0, End of treatment and 1 month |
Successful results in ESWT group, compared to the other, in pain and functional outcome, but no significant difference in the grasp and pinching strength between the measurements of the groups (p > 0.05). ESWT VAS(baseline = 5.8 ± 1.8; posttreatment = 4.3 ± 2.1); placebo VAS(baseline = 6.1 ± 1.6;posttreatment=5.3 ± 1.8); ESWT PRTEE(baseline = 79.7 ± 26.4;posttreatment=60.1 ± 33.2); placebo PRTEE(baseline = 76.7 ± 19.7; posttreatment = 64.7 ± 20.2) |
| [45] | Radwan et al. | 56 | ESWT vs Tenotomy | 100+1400 (Nd) | 0, 3, 6, 12 weeks and 1 year | Between the 3th and the 12th weeks, improvement of each assessment in both the treatments. Similar functional results (p > 0.05) were found between the ESWT and operative groups. Success (Roles and Maudsley excellent and good results) = ESWT (3 weeks = 48.3%; 6 weeks = 58.6%; 12 weeks = 65.5%; 1 years = 62.10%); Tenotomy (3 weeks = 59.3%; 6 weeks = 63.0%; 12 weeks = 74.1%; 1 year = 77.80%) |
| [46] | Lee et al. | 22 | ESWT vs steroid local injection | 2000 (1) | 0, 1, 2, 4, 8 weeks | Significant statistical differences were found between pre- and post-therapy in both the groups. Early better outcome was recorded in the local steroid injection group, but similar values were reported in the subsequently follow-ups. 1-week follow up (ESWT Excellent-Good = 41.7%; steroid local injection Excellent-Good = 70.0%; ESWT Acceptable-Poor = 58.3%; steroid local injection Acceptable-Poor = 30.0%); 8-week follow up(ESWT Excellent-Good = 66.7%; steroid local injection Excellent-Good = 40.0%; ESWT Acceptable-Poor = 33.3%; steroid local injection Acceptable-Poor = 60.0%) |
| [47] | Vulpiani et al. | 80 | ESWT vs Cryoultrasound | 2400 (2-3) | 0, 3, 6, 12 months | In the short term, the two treatments results were found similar in pain assessment and patients satisfaction rate. In middle and long-term better result in ESWT group than the other were found. ESWT VAS (baseline = 6.52 ± 1.47; last follow-up = 2.32 ± 2.25) Cryo-US VAS(baseline = 6.60 ± 1.64; last follow-up = 4.70 ± 2.79) |
| [48] | Wong et al. | 34 | ESWT vs Acupuncture | 2000 (Nd) | 0, End of treatment and 2 weeks | Similar results between two treatment groups in all the parameters. At the end of the therapies the no further pain improvements were recorded. Acupunture VAS (baseline = 6.12 ± 2.09; 2weeks follow-up = 4.06 ± 2.41); Acupunture DASH (baseline = 66.88 ± 14.13; 2weeks follow-up = 63.94 ± 15.34); ESWT VAS (baseline = 5.47 ± 1.97; 2weeks follow-up = 3.18 ± 2.13); ESWT DASH( baseline = 64.65 ± 14.56; 2weeks follow-up = 60.12 ± 15.50); |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Testa, G.; Vescio, A.; Perez, S.; Consoli, A.; Costarella, L.; Sessa, G.; Pavone, V. Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review. J. Clin. Med. 2020, 9, 453. https://doi.org/10.3390/jcm9020453
Testa G, Vescio A, Perez S, Consoli A, Costarella L, Sessa G, Pavone V. Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review. Journal of Clinical Medicine. 2020; 9(2):453. https://doi.org/10.3390/jcm9020453
Chicago/Turabian StyleTesta, Gianluca, Andrea Vescio, Stefano Perez, Alberto Consoli, Luciano Costarella, Giuseppe Sessa, and Vito Pavone. 2020. "Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review" Journal of Clinical Medicine 9, no. 2: 453. https://doi.org/10.3390/jcm9020453
APA StyleTesta, G., Vescio, A., Perez, S., Consoli, A., Costarella, L., Sessa, G., & Pavone, V. (2020). Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review. Journal of Clinical Medicine, 9(2), 453. https://doi.org/10.3390/jcm9020453






